Abstract
This study assessed effectiveness of an educational community intervention taught by promotoras de salud in reducing cardiovascular disease (CVD) risk among Hispanics using a structural equation modeling approach (SEM). Model development was guided by a social ecological framework proposing CVD risk reduction through improvement of protective health behaviors, health beliefs, contextual and social factors. Participants were 328 Hispanic adults with at least one CVD risk factor. SEM analyses assessed direct and indirect effects of intervention participation on CVD risk (Framingham score) and latent variables nutrition intake and health beliefs. The model fit was adequate (root mean square error approximation =.056 [90% confidence interval = .040, .072], comparative fit index =.967, normed fit index=.938, nonnormed fit index =.947). Intervention participation was associated with improved nutritional consumption, but not lower CVD risk. Stronger health beliefs predicted healthier nutritional habits. This project provided evidence for the adequacy of a conceptual framework that can be used to elicit new pathways towards CVD risk reduction among at-risk Hispanic populations.
Keywords: Path Analysis, structural equation model, conceptual framework, Promotora, Community Health Worker, cardiovascular disease, Hispanic, Border, community, education, nutrition, promotoras de salud
The Hispanic population in the United States has increased from approximately 20 million in 1990 to approximately 44.3 million in July of 2006, and is estimated to consist of over 100 million people by the year 2050 (U.S. Bureau of the Census, 2007). As in other ethnic groups, cardiovascular disease (CVD) is the leading cause of death and disability among Hispanic populations and among the largest Hispanic subgroup: Mexican Americans (Sorlie, Backlund, Johnson, & Rogot, 1993). Higher prevalence of CVD risk factors of diabetes, obesity, and being overweight have been described among Hispanic populations (Centers for Disease Control and Prevention, 2009; National Institute of Diabetes and Digestive and Kidney Diseases, 2008). Furthermore, Hispanics are less likely to have access to and to utilize preventive health care services, and they are less aware of their blood cholesterol level and blood pressure (Center for Border Health Research, 2005; Perez-Stable, Marin & Marin, 1994; Treviño, Treviño, Medina, Ramirez, & Ramirez, 1996). The combination of rapid population growth, a high CVD risk profile and limited access to care suggest major public health challenges related to CVD in the near future among Hispanic populations.
The HEART Project
In response to the high risk for CVD among Hispanics, the Salud Para Su Corazon (SPSC; Health For Your Heart) health education curriculum was developed in 1994 by the National Heart Lung and Blood Institute (NHLBI). The SPSC includes Su Corazon Su Vida (Your Heart Your Life) modules in English and Spanish that aim to address lifestyle risk factors associated with CVD, obesity and diabetes. The SPSC intervention is tailored to be culturally relevant for members of the Hispanic culture. Constructs from the Health Belief Model were first identified for incorporation into the SPSC program development to introduce a theoretical foundation to the intervention (Balcazar, Alvarado, Luna Hollen, Gonzalez-Cruz & Pedregon, 2006). Several studies (e.g. Medina, Balcazar, Luna Hollen, Nkoma & Soto Mas, 2007) have evaluated the success of the SPSC including a project called HEART (Health Education Awareness Research Team) conducted in 2007 in El Paso, Texas (Balcazar et al., 2010; Balcazar, Rosenthal, et al., 2009).
The HEART study consisted of a randomized controlled trial of a health education intervention for Hispanic adults who were at risk for CVD. In project HEART, bilingual promotoras de salud employed by a local clinic provided health education focused on prevention of CVD. Promotoras de salud (or community health workers) are outreach health workers who are members of the community in which they work. Through their contact with the community, they often serve as a liaison between health care providers and patients, providing various forms of health related services, such as community advocacy, social support and cultural mediation (Rosenthal, 1998).
Data from the HEART project were analyzed using conventional multiple regression approaches (see Balcazar et al., 2010) to examine the impact of the intervention on a variety of behavioral and clinical outcomes. In the present article, we take a different approach by examining the role of the promotores de salud intervention in the context of a conceptual framework that postulates that the initiation of risk reduction is triggered by a combination of contextual, psychological responses and behavioral pathways. Within the framework, we hypothesize a set of direct and indirect effects of the intervention on a number of clinical and behavioral health outcomes. To achieve this aim, the current study analyzed the HEART project data using a structural equation modeling (SEM) methodology.
SEM methodologies are rarely used in public health intervention research, although a small number of applications of SEM methods describing associations among health behaviors and aspects of Hispanic culture have been published (e.g. Cobas, Balcazar, Benin, Keith & Chong, 1996; Larkey, Hecht, Miller & Alatorre, 2001; Pichon et al., 2007). SEM methodology affords a greater capacity for modeling the relations between several independent and dependent variables (and among several dependent variables; see Hoyle & Smith, 1994), thus allowing for the analysis of the various factors that influence the development of common complex diseases such as CVD.
In comparison with conventional regression model analyses, SEM methodology offers several important advantages: (a) SEM methodology corrects for unreliability in measurement, explicitly recognizing measurement error in part via the use of latent constructs; (b) SEM methodology allows for the inclusion of multiple equations and can assess direct and indirect effects simultaneously; (c) SEM allows the testing of hypotheses regarding directional effects that may occur between dependent variables, and (d) SEM methodology allows for estimating overall model fit, which (for the current study) indicated how well the empirical data described a previously developed conceptual framework of CVD risk reduction.
Model construction was guided by the SPSC framework (Anders, Balcazar, & Paez, 2006), which was based on an ecological model that was adapted from the work of Stokols (1996). The conceptual framework by Anders et al. (2006) describes how pathways of behavior change can lead towards healthier lifestyles and CVD risk reduction among Mexican Americans. In the proposed model, participation in risk-reducing interventions is hypothesized to be associated with changes in psychosocial responses such as changes in health beliefs and to predict behavioral pathways such as nutrition intake, resulting in the initiation (and maintenance) of risk reduction, directly and indirectly (through specific behavioral pathways). Several important contextual factors such as age, gender, educational attainment and birthplace were included in this model as well. Finally, prior literature (e.g. Pasick & Burke, 2008) has emphasized the importance of social context and resources as determinants of health behaviors among minority populations. Only family cohesion was available as an indicator of social support for the current study. However, Sabogal, Marin, Otero-Sabogal, Marin and Perez-Stable (1987) identified familial support to be the most essential dimension of Hispanic ‘familism.’ Furthermore, recent research has illustrated the importance of family support and cohesion for mental and physical health among Latino populations (Mulvaney-Day, Alegría & Sribney, 2007; Rivera et al., 2008) and therefore it was decided to include family cohesion as an indicator of social resources in our model.
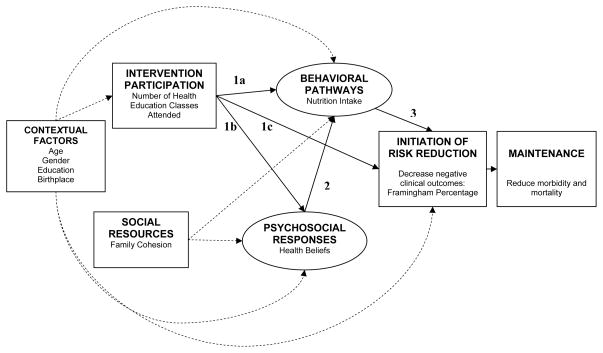
For the current study, the original conceptual framework by Anders et al. (2006) was expanded and described with specific paths that served as hypothesized relationships between the key variables, including specified directions of effect that could be tested in a structural equations model analysis. Figure 1 graphically depicts the intervention model as it was operationalized for the current study. Specific hypotheses are indicated in the model.
Figure 1. The Conceptual model of cardiovascular disease prevention and reduction among Mexican Americans.
Note: 1a = Hypothesis 1a; 1b= Hypothesis 1b. Circles represent latent variables, boxes represent observed variables. Dashed lines are paths that are not associated with a specific hypothesis. No indicators of maintenance were available for the current study.
Hypotheses
Generally, it was expected that the SPSC conceptual framework would provide a viable description of effects that could be modeled and tested with empirical data, with model adequacy assessed with specific indicators of goodness of fit. Three specific hypotheses examined the effectiveness of the promotores de salud SPSC intervention on specific outcome variables, after controlling for pre test values and the effects of contextual factors and social resources. These hypotheses were as follows:
Hypothesis 1a, 1b, 1c: At the follow-up assessment, intervention participation will be associated with Hypothesis 1a; better nutritional habits (lower cholesterol and fat, sodium, and weight-related nutrition intake); Hypothesis 1b: stronger health beliefs (higher perceived susceptibility, severity and benefits) and Hypothesis 1c: lower risk for coronary heart disease.
Hypothesis 2: Stronger health beliefs (higher perceived susceptibility, severity and benefits) will be predictive of healthier nutritional habits (lower cholesterol and fat, sodium and weight-related nutrition intake) at follow-up. Testing this hypothesis in conjunction with Hypothesis 1b would also enable estimating the indirect effect of intervention participation on nutrition intake through health beliefs.
Hypothesis 3: Healthier nutritional intake will be associated with lower risk for coronary heart disease at posttest. Testing this hypothesis in conjunction with Hypothesis 1a will also allow for estimating the indirect effect of intervention participation on the risk for coronary heart disease through nutrition intake.
Method
Study Design and Procedures
The study was a randomized controlled community trial with a baseline and a 4-month follow-up assessment. The intervention group received a series of eight health education classes (once a week for 8 weeks) based on the SPSC curriculum Su Corazon, Su Vida (Your Heart Your Life). This curriculum was taught by a promotora de salud (a community health worker). This educational phase of the intervention was followed by a phase consisting of 8 weeks of continued contact by phone on the part of the community health worker. During the classes, promotoras de salud delivered educational information from the different modules and provided many opportunities for dialogue with participants regarding the usefulness of the information and how they may apply it to begin making positive changes regarding lifestyle behaviors. At the end of every class, participants pledged a change that they would commit to for that week based on the topic of the lesson. At the beginning of each class participants had the opportunity to engage in a dialogue with promotoras and other participants about how well they did with achieving their pledge. The use of personal values or virtues (i.e. perseverance, serenity, openness) was also used to engage participants in a dialogue on how the use of virtues may help them to achieve their weekly pledges. The control group received an informational packet that included the SPSC curriculum. Both groups were assessed at baseline and at 4-month follow-up. Additional details can be found elsewhere (Balcazar et al., 2010; Balcazar, Rosenthal, et al., 2009).
Study Setting
This study was conducted in the lower valley area in El Paso, Texas. The population in El Paso has a lower per capita income and higher poverty rates when compared with other cities in Texas and the United States. El Paso also has the highest proportion of uninsured residents (39.5%) of any major city in the United States. Diabetes prevalence and mortality rates in El Paso are higher when compared with state and national averages (Texas Department of State Health Services [DSHS], 2006). The Lower Valley area is further characterized by a lower median age, lower estimated median household income, and a higher percentage of Hispanic Mexican American residents when compared with the rest of El Paso (Texas DSHS, 2006).
Recruitment
A total of 3,959 households were approached in the selected zip code area. The total number of participants who completed baseline assessments was 328 (232 females). Inclusionary criteria were that the participant had to be between the ages of 30 and 75, be of Hispanic descent, and have at least one risk factor for CVD, including being overweight, having high blood pressure, high cholesterol levels, or diabetes (see also Balcazar et al., 2010; Balcazar, Rosenthal, et al., 2009).
Measures
Data used to specify the model in accord with the conceptual framework included self-report data and data on clinical indicators. Self-report data including demographic characteristics, were collected using a questionnaire that included several validated measures (Balcazar Alvarado, Cantu, Pedregon & Fulwood, 2009; Balcazar et al., 2010). Data on clinical parameters included blood pressure and a lipid profile and were collected following standard procedures described by the American Heart Association.
In the structural equation model, contextual factors included the demographic variables of age, gender, education and birthplace (Mexico vs. United States). Education was indicated by the highest grade in school completed. Social resources were operationalized using the variable Family Cohesiveness which was measured using a three-item scale that included items such as, My family spends a lot of time together which was measured on a 5-point Likert-type scale with a dimension ranging from 1 = never to 5 = always’.
Psychosocial responses were operationalized as health beliefs, which consisted of a latent variable (“health beliefs”) that was defined by three indicator variables based on health belief model constructs: (a) perceived severity, (b) perceived susceptibility, and (c) perceived benefits. All health belief items were rated on a 4-point Likert scale and ranged from 1 = strongly disagree to 4 = strongly agree. Perceived Severity regarding the consequences of CVD was indicated by four items, where an exemplar item was CVD might lead to serious complications. Perceived Susceptibility consisted of a five- item scale, where an exemplar item was: If I am overweight, I am more likely to have CVD. Perceived Benefits of a CVD prevention was measured with four items, where an exemplar item was: Changing my dietary habits will help lower the risk of developing CVD. All health belief scales exhibited adequate reliability (Cronbach’s α > .79).
Behavioral pathways included dietary habits. Dietary habits were assessed as a latent variable (nutrition) that was indicated by three indicator variables, which were cholesterol and fat intake, sodium intake and weight-related dietary intake. Self-reported cholesterol and fat-related nutrition intake was indicated by seven items that were measured on a 4-point Likert-type scale that ranged from: 1 = never to 4 = always. This factor included items similar to the exemplar item of: I read the food label to help in choosing foods lower in fat, saturated fat and cholesterol. Self-reported sodium intake was assessed using a nine- item measure, with an exemplar item being: I add little or no salt to the water when cooking beans, rice, pasta and vegetables, and these items were assessed via a 4-point Likert-type scale that ranged from 1 = strongly disagree, to 4 = strongly agree. The third indicator was weight-related nutrition intake, which consisted of seven items, such as, I eat smaller portions of food and do not go back for seconds, where these items were assessed via the same 4- point Likert-type scale. All scales but one exhibited adequate reliability (Cronbach’s α > .68).
The predictor intervention participation was operationalized in the model as the number of health classes attended by participants (ranging from 0 to 8), as recorded for each class by the promotoras. Control group participants were assigned a “0” for this indicator as they did not attend any classes. This is a different variable than the intent-to-treat design indicator that was reported in the original analyses by Balcazar et al. (2010). This approach was chosen to more accurately obtain an estimate of intervention participation, rather than intervention group assignment. About a quarter of participants (26.3%) did not attend any classes, whereas over 60% attended at least half the classes. The main outcome variable (initiation of risk reduction) consisted of a calculation of the 10-year risk for coronary heart disease development (e.g. myocardial infarction) based on from the following risk factors: LDL and HDL cholesterol, blood pressure, diabetes, smoking status and age. Framingham risk score was computed and converted to percentage risk using standard protocols (Wilson et al., 1998). Although the Framingham risk calculation is based on data from a population-based study that consisted of non-Hispanic Whites, the identified risk factors have been shown to exhibit similar predictive values among Hispanic populations (e.g the San Antonio Heart Study; Wei, Mitchell, Haffner & Stern, 1996).
Structural Equation Modeling Analyses and Modeling
A structural equation model analysis was used to test the proposed conceptual model (Kline, 1998). Model fit was estimated using AMOS 16.0 (SPSS inc.) and using maximum likelihood estimation, under the assumption of multivariate normality, to assess the discrepancy between the sample and a fitted covariance matrix (Hu & Bentler, 1999). Following recommendations by Hu and Bentler (1999), in addition to the χ2 values, the root mean square error of approximation (RMSEA), the nonnormed fit index (NNFI) and comparative fit index and comparative fit index (CFI) were used as fit indices (Hu & Bentler, 1999; McDonald, 1999; MacCallum, Browne, & Sugawara, 1996). Prior to the analyses of the structural model, a measurement model was examined to identify each latent variable for this model, and it was tested for effective identification of each of the latent variables. In this regard the loadings of all indicators variables for each of the latent variables were high (0.72 and higher, ps<.001).
Results
Contextual Factors
The mean age of the participants was 53 ±13 years old; their average educational attainment was 10th grade ±3 grades, and the mean annual household income was between $15,000 and $20,000. About 41% had no health insurance. Overall, 10-year risk for coronary heart disease was higher among both male (21.6 ±14.0 %) and female (10.9 ±8.4%) participants when compared with the national averages for this age group of 14% (men) and 8% (women) respectively (Wilson et al., 1998). Additional demographic characteristics and clinical indicators are described elsewhere (see Balcazar et al., 2010).
Structural Equation Models
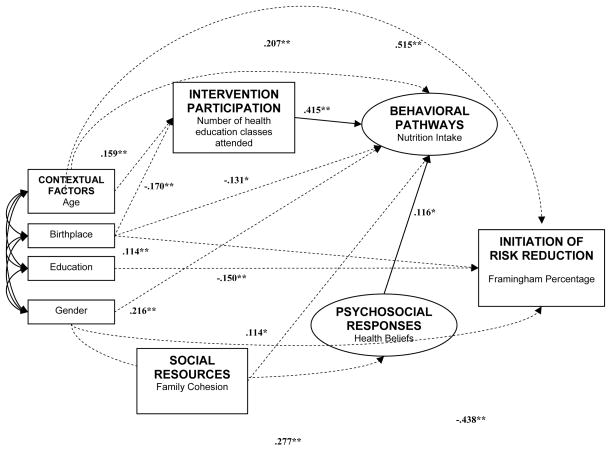
The final assessment of model fit was based on the cross-comparison of several established fit statistics. The final structural model had an adequate goodness of fit value, of 2.04 times the degrees of freedom: χ2 (df=49) = 99.94, p < .01. The other fit statistics indicated good fit as RMSEA = .056 (90% confidence interval [CI] of .040 to .072), CFI =.967, NFI=.938 and NNFI (Tucker-Lewis index) =.947 (see Figure 2). Based on these results, we concluded that the model fit was acceptable.
Figure 2. The final model of cardiovascular disease prevention and reduction among Mexican Americans with significant paths only.
Notes. Regression coefficients are standardized. Circles indicate latent variables, boxes represent observed variables. For clarity, error terms and latent variable indicators are left out. Dashed lines are significant paths not associated with any specified hypotheses.
*p < .05. **p < .01.
Model fit: χ2(df=49)=99.94, RMSEA=0.56 (0.40, 0.72), CFI=.967, NFI=.938, NNFI=.947
Both older age (β =.159, t = 2.940, p =.003) and being born in Mexico ( β= −.170, t = −3.145, p =.002) were associated with greater intervention participation (larger number of classes attended). Females reported stronger health beliefs (β =.277, t = 4.815, p <.001) as indicated by perceived susceptibility, severity and benefits of engaging in protective behaviors. Females also reported better nutritional habits (β =.216, t = 4.039, p < .001) as did older participants (β =.207, t =3.998, p < .001), and participants born in Mexico (β = −.131, t = −2.525, p =.012). Being male, being older, having less education and being born in the United States were associated with higher 10-year Framingham risk. Finally, greater family cohesion was associated with healthier nutrition habits, β = .114, t = 2.277, p =.023 (see Table 1 for all factor loadings).
Table 1.
Standardized and Unstandardized Regression Weights for Final Model
| Model Path | Standardized Estimate | Unstandardized Estimate (SE) | CR | p |
|---|---|---|---|---|
| Hypothesized | ||||
| Hypothesis 1a: Intervention participation ➝ Nutrition | .415 | .405 (.052) | 7.731 | <.001** |
| Hypothesis 1b: Intervention Participation ➝ Health beliefs | .077 | .030 (.022) | 1.367 | .172 |
| Hypothesis 1c: Intervention Participation ➝ Framingham Risk | .049 | .147 (.130) | 1.129 | .259 |
| Hypothesis 2: Health beliefs ➝ Nutrition | .116 | .286 (.137) | 2.079 | .038* |
| Hypothesis 3: Nutrition ➝ Framingham risk | .032 | .097 (.160) | 0.609 | .542 |
| Control | ||||
| Age ➝ Nutrition | .207 | .055 (.014) | 3.998 | <.001** |
| Age ➝ Framingham risk | .515 | .422 (.033) | 12.738 | <.001** |
| Age ➝ Intervention participation | .159 | .043 (.015) | 2.940 | .003** |
| Gender ➝ Health beliefs | .277 | .876 (.182) | 4.815 | <.001** |
| Gender ➝ Nutrition | .216 | 1.685 (.417) | 4.039 | <.001** |
| Gender ➝ Framingham risk | −.438 | −10.526 (.938) | −11.218 | <.001** |
| Birthplace ➝ Nutrition | −.131 | −.923 (.366) | −2.525 | .012* |
| Birthplace ➝ Framingham risk | .114 | 2.477 (.910) | 2.710 | .007** |
| Birthplace ➝ Intervention participation | −.170 | −1.229 (.391) | −3.145 | .002** |
| Education ➝ Framingham risk | −.150 | −.466 (.133) | −3.497 | <.001** |
| Family cohesion ➝ Nutrition | .114 | .161 (.072) | 2.277 | .023* |
| Family cohesion ➝ Health beliefs | .042 | .024 (.032) | .746 | .456 |
| Measurement Models | ||||
| Health beliefs ➝ Susceptibility | .866 | 1.317 (.079) | 16.640 | <.001** |
| Health beliefs ➝ Severity | .893 | 1.113 (.066) | 16.896 | <.001** |
| Health beliefs ➝ Benefits | .787 | 1.000 | ||
| Nutrition ➝ Cholesterol intake | .717 | .927 (.072) | 12.881 | <.001** |
| Nutrition ➝ Weight-related intake | .796 | .933 (.066) | 14.131 | <.001** |
| Nutrition ➝ Sodium intake | .830 | 1.000 | ||
Note. SE= standard error; cr= Critical Ratio.
p<.05,
p<.01.
Hypothesis 1 tested the effect of the intervention on each of three health indicators: health beliefs, nutritional behaviors, and risk of CVD. For hypothesis 1, the model indicated that intervention participation was associated with healthier nutrition intake at post-test, β =.415, t = 7.731, p < .001 (Hypothesis 1a); a one standard deviation higher number of classes attended was associated with a 0.415 standard deviation healthier nutrition intake at posttest. Intervention participation was not associated with significantly more positive health beliefs, β =.077, t = 1.367, p =.172 (Hypothesis 1b) or with a reduced Framingham risk, β = .049, t =1.129, p =.259 (Hypothesis 1c).
Hypothesis 2 examined the effects of health beliefs on nutrition. For hypothesis 2, health beliefs were positively associated with better nutrition intake (β = .116, t = 2.079, p =.038). An increase of one standard deviation in health beliefs was associated with a 0.116 standard deviation healthier nutrition intake.
Hypothesis 3 indicated that healthy nutritional behaviors would exert an effect in reducing Framingham risk. Hypothesis 3 was not supported, as better nutrition intake at follow-up was not associated with lower risk for coronary heart disease (Framingham risk; p=.542).
Discussion
Using SEM methodology, the current study evaluated the data of a controlled community trial of a health education intervention program taught by promotoras de salud (project HEART), an intervention aimed at reduction of risk for CVD among Hispanic adults El Paso, Texas. Based on the HEART study, Balcazar et al. (2010) reported that participants in the intervention group (compared with control group participants) showed greater awareness of CVD risk factors, more confidence in the control of these factors, improved dietary habits and reduced their cholesterol levels. Beyond the findings of Balcazar et al. (2010), the current analysis elicited several new findings. First, the structural equation model based on the conceptual CVD risk reduction framework presented an acceptable fit to the empirical data, providing evidence for the adequacy of the framework by Anders and colleagues (2006) in describing factors associated with CVD risk reduction among Hispanic populations. Second, using a more accurate measure of intervention participation (number of health classes attended, rather than an intent-to-treat design), the current study confirmed the positive association of intervention participation with improved health habits, as indicated by the latent variable of nutrition intake. Third, although we did not find evidence for an effect of intervention participation impacting health beliefs, we did find that stronger health beliefs were associated with healthier nutrition intake at follow-up. Finally, the current analyses elicited new information about the impact of several contextual and social variables and their role in the process of CVD risk reduction in Hispanic populations. For example, being born in Mexico was not only associated with better nutritional habits and lower clinical CVD risk, but also with increased intervention participation.
The conceptual framework of CVD risk reduction among Hispanic populations developed by Anders et al. (2006) provided a meaningful description of the process that influences healthy behavior change in the current study population. Whereas major behavioral theories have focused predominantly on behavior as impacted by cognitive characteristics of an individual, largely uninfluenced by social context (Burke, Joseph, Pasick & Barker, 2009), the framework in the current study was based on a social ecological model (Stokols, 1996), thus recognizing environmental, social and cognitive influences on health behavior. A framework such as this allows for the assessment of complex systemic processes such as the factors that influence CVD development. Knowledge about these factors and the interplay among them can aid in gaining insight into pathways towards CVD risk reduction among Hispanic populations, for example through interventions delivered by promotoras de salud.
Interestingly, we found that intervention participation was associated with improved nutrition intake and that health beliefs predicted nutrition intake at follow-up. However, health beliefs were not directly impacted by intervention participation, which is not consistent with classical behavior theory (such as the Health Belief Model). Recent work (Pérez-Escamilla, Hromi-Fiedler, Vega-López, Bermúdez-Millán & Segura-Pérez, 2008) called for the use of culturally appropriate behavior change theory in future research among Latino populations. For example, several studies (Joseph, Burke, Tuason, Barker and Pasick, 2009; Pasick et al., 2009) have indicated that the associations between constructs frequently described in behavior theory (such as perceived susceptibility, severity and benefits) and health behaviors may not function the same among all populations. Joseph et al. (2009) reported that among participants in their study (immigrant or first-generation Latinas and Filipinas), social context and processes such as acculturation affected behavior directly, rather than exclusively through belief systems. It is possible, that given the similarity of our population of mostly immigrant or first generation U.S.-born Latinas to this recent work (Joseph et al., 2009; Pasick et al., 2009), similar processes may have occurred. For example, among our population, there was a direct effect of birthplace on nutrition intake and intervention participation, suggesting acculturative processes may have played a role in the intervention.
Limitations & Future Directions
Although the model presented in this study exhibited acceptable fit, it can be argued that several important variables are currently omitted from this model. For example, future models could incorporate aspects of culture, such as acculturation (instead of using a proxy measure such as birthplace), family traditionalism, (Castro & Garfinkle, 2003; Castro & Hernández-Alarcón, 2002), socioeconomic factors (Viruell-Fuentes, 2007), and influences of Mexican cultural health beliefs (Castro, Furth & Karlow, 1984). Unfortunately, the current sample size was not sufficient to allow the analysis of more complex models, and thus a smaller and more parsimonious model was presented, which was related to the conceptual framework that describes the health-related determinants of behavior and behavior change.
Furthermore, adequate representation of variables associated with social support and social interactions will be important. There has been some indication that the SPSC curriculum has been successful in improving community referrals, screenings and enhanced information sharing beyond families (Balcazar et al., 2006). Unfortunately, we were only able to include a variable that indicates family cohesion, which is limited as an indicator of the patterns of social support and social influence that exist within Hispanic families. Finally, as reported by Balcazar and colleagues (2010), no evidence for the reduction of clinical risk indicators for CVD was found in the current study, and much work is needed to appropriately evaluate the long-term impact of promotora interventions on clinical outcomes. This research would take steps toward identifying the most important characteristics and type of training that make promotoras effective, as well as what are optimal settings and dosage for interventions using their skills (Pérez-Escamilla et al., 2008). This research may then inform the optimal ways of integrating the promotora model into the health care system.
Implications for Research & Practice
The findings of the current project have several important implications for CVD risk reduction research and practice among Hispanic populations. First, the SEM approach allowed us to confirm the adequacy of an overall framework of CVD risk reduction in describing our population. We believe that future promotora interventions can use this framework to specify hypotheses about potential pathways towards CVD risk reduction.
Second, using traditional behavior theory to elicit pathways towards behavior change may not be an optimal approach among immigrant or first generation U.S.-born populations. As indicated in recent research (Joseph et al., 2009; Pasick et al., 2009), traditional constructs used in behavior theory may not have the same meaning across populations. Eliciting pathways toward CVD risk reduction among Hispanic populations may require going beyond classical behavior theory raising the need to take into account various social and contextual factors. For example, in the current study, we found that higher family cohesion was associated with better nutritional habits. Given that family members often share clinical, cultural, social and behavioral risk factors (Castro, Shaibi, & Boehm-Smith, 2009) and given the importance of family support among Hispanic populations, promotora programs could capitalize on family support networks and provide family-level interventions, rather than solely focusing on individually oriented interventions focused on changing cognitions.
The current study highlights the importance of incorporating context (social, community, behavioral) into the work that promotoras de salud perform when engaging with Hispanic participants involved in CVD risk reduction education and other community and health systems.
Understanding these contextual influences, such as acculturative processes, points to different forms of interventions (Joseph et al., 2009) as delivered in settings where health care providers have a cultural understanding of their clients above and beyond a number of targeted health behaviors. This may be especially important when we take into account that factors associated with acculturation (such as birthplace in the case of the current study) affect not only current behaviors but also participation in promotora interventions.
The promotoras de salud educational model presents an example of an intervention in which the health educator specializes in understanding the client within their social context and therefore presents a tremendous opportunity for engaging participants in a dialogue examining the promotion of healthy behaviors. For this dialogue to be effective, taking into account the context of the environment where participants live, work and interact is essential for fostering opportunities to exchange ideas. The current study provided evidence that promotoras may be able to facilitate the exchange of ideas that can yield heart-healthy practices for CVD risk reduction.
References
- Anders R, Balcazar H, Paez L. Hispanic community-based participatory research using a promotores de salud model. Hispanic Health Care International. 2006;4:71–78. [Google Scholar]
- Balcazar H, Alvarado M, Cantu F, Pedregon V, Fulwood R. A promotora de salud model for addressing cardiovascular disease risk factors in the US-Mexico border region. Preventing Chronic Disease. 2009b;(6):1. Retrieved from http://www.cdc.gov/pcd/issues/2009/jan/08_0020.htm. [PMC free article] [PubMed]
- Balcazar H, Alvarado M, Luna Hollen M, Gonzalez-Cruz Y, Hughes O, Vazquez E, Lykens K. Salud para su Corazon-NCLR: A comprehensive promotora outreach program to promote heart healthy behaviors among Latinos. Health Promotion and Practice. 2006;7:68–77. doi: 10.1177/1524839904266799. [DOI] [PubMed] [Google Scholar]
- Balcazar H, Alvarado M, Luna Hollen M, Gonzalez-Cruz Y, Pedregon V. Evaluation of Salud para su corazon (health for your heart) :NCLR national dissemination promotora outreach projects. Preventing Chronic Disease. 2005;(2):3. Retrieved from: http://www.cdc.gov/pcd/issues/2005/jul/04_0130.htm. [PMC free article] [PubMed]
- Balcazar H, de Heer H, Rosenthal L, Aguirre M, Flores L, Puentes F, Schulz LO. A promotores de salud intervention to reduce cardiovascular disease risk in a high-risk Hispanic border population, 2005–2008. Preventing Chronic Disease. 2010;7(2) Retrieved from: http://www.cdc.gov/pcd/issues/2010/mar/09_0106.htm. [PMC free article] [PubMed] [Google Scholar]
- Balcazar H, Rosenthal L, de Heer H, Aguirre M, Flores L, Vasquez E, Duarte M, Schulz LO. Use of community-based participatory research to disseminate baseline results from a cardiovascular disease randomized community trial for Mexican Americans Living in a U.S.-Mexico Border Community. Education for Health. 2009;22(1):279. [PMC free article] [PubMed] [Google Scholar]
- Burke NJ, Joseph G, Pasick RJ, Barker JC. Theorizing social context: Rethinking behavioral theory. Health Education and Behavior. 2009;36:55S–70S. doi: 10.1177/1090198109335338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro FG, Furth P, Karlow H. The health beliefs of Mexican, Mexican American, and Anglo American women. Hispanic Journal of Behavioral Sciences. 1984;6:365–383. [Google Scholar]
- Castro FG, Garfinkle J. Critical issues in the development of culturally relevant substance abuse treatments for specific minority groups. Alcoholism: Clinical and Experimental Research. 2003;27:1–8. doi: 10.1097/01.ALC.0000080207.99057.03. [DOI] [PubMed] [Google Scholar]
- Castro FG, Hernández-Alarcón E. Integrating cultural variables into drug abuse prevention and treatment with racial/ethnic minorities. Journal of Drug Issues. 2002;32:783–810. [Google Scholar]
- Castro FG, Shaibi GQ, Boehm-Smith E. Ecodevelopmental contexts for preventing type 2 diabetes in Latino and other racial/ethnic minority populations. Journal of Behavioral Medicine. 2009;32:89–105. doi: 10.1007/s10865-008-9194-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Border Health Research. A status report on the health of people in El Paso County, Texas and Doña Ana County, New Mexico. 2005 Retrievedfrom http://www.borderhealth.org/files/res_694.pdf.
- Centers for Disease Control and Prevention. (CDC) Differences in prevalence of obesity among Black, White, and Hispanic Adults--United States, 2006–2008. MMWR Morbidity and Mortality Weekly Report. 2009;58:740–744. Retrieved from http://www.cdc.gov/mmwr/PDF/wk/mm5827.pdf. [PubMed] [Google Scholar]
- Cobas JA, Balcazar H, Benin MB, Keith VM, Chong Y. Acculturation and low-birthweight infants among Latino women: a reanalysis of HHANES data with structural equation models. American Journal of Public Health. 1996;86:394–396. doi: 10.2105/ajph.86.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle RH, Smith GT. Formulating clinical research hypotheses as structural equation models: A conceptual overview. Journal of Consulting and Clinical Psychology. 1994;62:429–440. doi: 10.1037//0022-006x.62.3.429. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Joseph G, Burke NJ, Tuason N, Barker JC, Pasick RJ. Perceived susceptibility to illness and perceived benefits of preventive care: An exploration of behavioral theory constructs in a transcultural context. Health Education and Behavior. 2009;36(5 Suppl):71S–90S. doi: 10.1177/1090198109338915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford Press; 1998. [Google Scholar]
- Larkey LK, Hecht ML, Miller K, Alatorre C. Hispanic cultural norms for health-seeking behaviors in the face of symptoms. Health Education &Behavior. 2001;28:65–80. doi: 10.1177/109019810102800107. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HW. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;7:130–149. [Google Scholar]
- McDonald RP. Test Theory: A Unified Treatment. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- Medina A, Balcazar H, Luna Hollen M, Nkoma E, Soto Mas F. Promotores de salud educating Hispanic communities on heart-health living. American Journal of Health Education. 2007;38:194–202. [Google Scholar]
- Mulvaney-Day NE, Alegría M, Sribney W. Social cohesion, social support, and health among Latinos in the United States. Social Science and Medicine. 2007;64(2):477–495. doi: 10.1016/j.socscimed.2006.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Diabetes and Digestive and Kidney Diseases. National diabetes statistics, 2007 fact sheet. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health; 2008. Retrieved from: http://diabetes.niddk.nih.gov/dm/pubs/statistics/#race. [Google Scholar]
- Pasick RJ, Burke NJ. A critical review of theory in breast cancer screening promotion across cultures. Annual Reviews in Public Health. 2008;29:351–68. doi: 10.1146/annurev.publhealth.29.020907.143420. [DOI] [PubMed] [Google Scholar]
- Pasick RJ, Burke NJ, Barker JC, Joseph G, Bird JA, Otero-Sabogal R, Guerra C. Behavioral theory in a diverse society: Like a compass on Mars. Health Education &Behavior. 2009;36(5 Suppl):11S–35S. doi: 10.1177/1090198109338917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Escamilla R, Hromi-Fiedler A, Vega-López S, Bermúdez-Millán A, Segura-Pérez S. Impact of peer nutrition education on dietary behaviors and health outcomes hmong Latinos: A systematic literature review. Journal of Nutrition Education and Behavior. 2008;40:208–225. doi: 10.1016/j.jneb.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Stable EJ, Marín G, Marín BV. Behavioral risk factors: a comparison of Latinos and non-Latino whites in San Francisco. American Journal of Public Health. 1994;84:971–976. doi: 10.2105/ajph.84.6.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pichon LC, Arredondo EM, Roesch S, Sallis JF, Ayala GX, Elder JP. The relation of acculturation to Latinas’ perceived neighborhood safety and physical activity: A structural equation analysis. Annals of Behavioral Medicine. 2007;34:295–303. doi: 10.1007/BF02874554. [DOI] [PubMed] [Google Scholar]
- Rivera FI, Guarnaccia PJ, Mulvaney-Day N, Lin JY, Torres M, Alegria M. Family cohesion and its relationship to psychological distress among Latino Groups. Hispanic Journal of Behavioral Sciences. 2008;30:357–378. doi: 10.1177/0739986308318713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal EL. A summary of the National Community Health Advisor Study. Baltimore, MD: Annie E. Casey Foundation; 1998. [Google Scholar]
- Sabogal F, Marin G, Otero-Sabogal R, Marin BV, Perez-Stable EJ. Hispanic familism and acculturation: what changes and what doesn’t? Hispanic Journal of Behavioral Sciences. 1987;9:397–412. [Google Scholar]
- Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. Journal of the American Medical Association. 1993;270:2464–2468. [PubMed] [Google Scholar]
- Stokols D. Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion. 1996;10:282–98. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- Texas Department of State Health Services. Texas health facts (state,regions and counties) 2004. 2006 Retrieved from: http://www.dshs.state.tx.us/chs/cfs/
- Treviño RP, Treviño FM, Medina R, Ramirez G, Ramirez RR. Health care access among Mexican Americans with different health insurance coverage. Journal of Health Care for the Poor and Underserved. 1996;7:112–121. doi: 10.1353/hpu.2010.0022. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of the Census. Facts for Features: Hispanics Heritage month 2007: Sept 15-Oct 15. 2007 Retrieved from: http://www.nlatinoaddiction.org/Documents/cb07ff-14.pdf.
- Viruell-Fuentes EA. Beyond acculturation: Immigration, discrimination, and health research among Mexicans in the United States. Social Science &Medicine. 2007;65:1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Wei M, Mitchell BD, Haffner SM, Stern MP. Effects of cigarette smoking, diabetes, high cholesterol and hypertension on all-cause mortality and cardiovascular disease mortality in Mexican Americans. The San Antonio Heart Study. American Journal of Epidemiology. 1996;144:1058–1065. doi: 10.1093/oxfordjournals.aje.a008878. [DOI] [PubMed] [Google Scholar]
- Wilson PWF, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]