Abstract
Objectives
To describe diagnoses and factors associated with hospital transfer among nursing home (NH) residents with advanced dementia.
Design
Prospective cohort study.
Setting
22 Boston-area NHs.
Participants
323 NH residents with advanced dementia.
Measurements
Data were collected quarterly for up to 18 months. Data regarding transfers included: hospitalization or emergency department (ED) visit, diagnosis and duration of inpatient admission. The occurrence of any acute medical event (pneumonia, febrile episode or other acute illness) in the prior 90 days was obtained quarterly. Logistic regression conducted at the level of the acute medical event identified characteristics associated with hospital transfer.
Results
The entire cohort experienced74 hospitalizations and 60 ED visits. Suspected infections were the most common reason for hospitalization (44/74, [59%]), most frequently attributable to a respiratory source (30/74, [41%]). Feeding tube-related complications accounted for 47% of ED visits. In adjusted analysis conducted among acute medical events, younger resident age, the event type (pneumonia or other event vs. febrile episode), chronic obstructive pulmonary disease and the lack of a DNH order (adjusted odds ratio 5.22, 95% CI 2.31-11.79) were associated with hospital transfer.
Conclusion
The majority of hospitalizations among NH residents with advanced dementia were due to infections, and thus, were potentially avoidable, as infections are often treatable in the NH setting. Feeding tube-related complications accounted for almost half of all ED visits, representing a common but under-recognized burden of this intervention. Advance care planning in the form of a DNH order was the only identified modifiable factor associated with avoiding hospitalization.
Keywords: dementia, hospitalization, nursing home
Introduction
The majority of end-of-life care for patients with dementia is provided in the nursing home (NH).1 NH residents with advanced dementia are at high risk of hospital transfer due to the frequency of acute illness, particularly infections.2 The benefit of hospital transfers among patients with advanced dementia is unclear, due to the fact that hospitalizations are costly,3-5 associated with burdensome interventions,6-7 and may impair family member well-being.8 Furthermore, many hospitalizations for NH residents with dementia may be avoidable, since NH care is as effective as hospital care for the treatment of many common conditions such as pneumonia.9 Lastly, for the majority of patients with advanced dementia, comfort is the goal of care,2 which is seldom consistent with hospitalization.
Approximately 25% of NH residents with advanced dementia will have a hospital transfer in the last six months of life.10 In this population, hospitalizations account for 30% of Medicare expenditures, with an additional 10% attributable to skilled nursing facility care post-hospitalization.5 Due to pressures from health care reform to reduce both overall expenditures and hospital readmissions among Medicare beneficiaries, it is important to understand the diagnoses and factors associated with hospital transfers in this population, which are currently not well described.
This study utilizes a prospective cohort of NH residents with advanced dementia to examine the primary diagnoses associated with hospital transfer (hospitalization or emergency department [ED] visit), and the frequency and predictors of hospital transfer in the setting of acute illness.
Methods
Study Population
Participants were from the Choices, Attitudes and Strategies for Care of Advanced Dementia at the End-of-Life (CASCADE) study, a prospective cohort study of NH residents with advanced dementia and their health care proxies (HCPs).2 Residents were from 22 NHs within 60 miles of Boston having at least 60 beds. Eligibility criteria were: 1) age > 60; 2) dementia (any type); and 3) Global Deterioration Scale (GDS)11 score of 7 (cannot recognize family, minimal verbal communication, total functional dependence, incontinence of urine and stool, inability to ambulate independently). Residents in skilled nursing facilities or subacute care were not eligible for the study. Residents had to have a HCP who could provide informed consent and communicate in English. The institutional review board of Hebrew SeniorLife approved this study.
Data Collection
Resident assessments were conducted at baseline and quarterly using medical record reviews, nurse interviews and clinical examinations. HCP data were obtained at baseline and quarterly by telephone interviews. Resident and HCPs were followed for 18 months or until resident death. After a resident died, a chart review and a nurse interview were conducted within 14 days.
Hospital Transfers and Acute Medical Events
At each quarterly assessment, the occurrence of any hospital transfer (hospitalization or emergency department [ED] visit) in the prior 90 days was ascertained. For these analyses, ED visits and hospitalizations were mutually exclusive, with ED visits defined as those not resulting in hospitalization. Any ED transfer resulting in hospital admission was defined as a hospitalization. Hospitalization data included the length of stay and the primary diagnosis leading to admission (abstracted from the hospital discharge summary by research assistants). ED visit data included the primary diagnosis for the visit.
At each quarterly assessment, the occurrence of an acute medical event since the last assessment was also obtained from the medical chart. These events were categorized as pneumonia, febrile episode or other acute illnesses. Other acute illnesses included any new medical condition that had the potential to lead to a clinically significant change in health status (e.g., seizure, bone fracture, myocardial infarction, stroke, or gastrointestinal bleed). For each acute medical event, information was obtained as to whether a treatment discussion with the HCP was documented in the medical record and whether the event resulted in a hospital transfer.
Resident and HCP Characteristics
Resident variables ascertained at baseline included age, gender, race (white vs. other), length of NH stay, residence on a special care dementia unit, and any chronic illness likely to cause hospital transfer (coronary artery disease, congestive heart failure or chronic obstructive pulmonary disease). Resident variables obtained at quarterly assessments included: functional status as measured by the Bedford Alzheimer's Nursing Severity Subscale12 (BANS-S) (range 7-28, higher scores indicate greater disability); presence of a feeding tube; presence of a do not hospitalize (DNH) order; and whether or not the resident was receiving hospice care.
Baseline HCP variables included age, gender, relationship to resident (child vs. other), whether the HCP's stated goal of care was comfort (versus life prolongation) and whether the HCP felt they understood the complications of advanced dementia. All continuous variables were dichotomized at their median values for ease of presentation.
Analysis
Descriptive statistics of all variables were conducted using frequencies to describe categorical variables and mean with standard deviations to describe continuous variables. Hospital transfers were described using data from the entire sample of 323 residents. Next, logistic regression was used to examine the unadjusted and adjusted associations between resident, HCP and event characteristics (independent variables) with whether or not a hospital transfer occurred for that event (i.e., the event was the unit of the analysis). This analysis was conducted only among those assessments where an acute medical event occurred, and thus, the opportunity for a hospital transfer arose. For time-varying independent variables (DNH order, BANS score, hospice referral and presence of a feeding tube), values were used from the quarterly assessment prior to that during which the acute medical event occurred. Static independent variables (e.g., age, gender) were brought forward from the baseline assessment. Independent variables associated at the level of p<0.1 with hospital transfer in unadjusted analyses were included in the multivariable model, which was adjusted for repeated measures at the individual level using robust standard error estimates.13-14 Odds ratios (ORs) and 95% confidence intervals (CIs) were generated from the logistic regression models. Statistical analyses were performed using STATA SE version 10.0 (STATA Corporation, College Station, TX).
Results
Characteristics of residents and hospital transfers
There were 323 NH residents followed in the CASCADE study. The mean age was 85.3 years, 85.4% were female and 89.5% were white (the distribution of resident characteristics presented in Table 1 differ slightly as the unit of analysis was the acute medical event). Among these 323 residents, 52/323 (16%) were hospitalized at least once and 32/323 (10%) had at least one ED visit (previously reported15). Overall there were 74 hospitalizations and 60 ED visits during the follow-up period. The diagnoses associated with hospital transfers are displayed in the Figure. Suspected infections were the most common reason for hospitalization (44/74, [59%]), most frequently attributable to a respiratory source (30/74, [41%]). Gastrointestinal bleeds were the second most common cause of hospitalization (6/74, [8%]), followed by respiratory distress (5/74, [7%]), fracture (4/74, [5%]), congestive heart failure (2/74, [3%]), and other single occurrence diagnoses (13/74, [18%]). The median hospital length of stay was 4.5 days (range 1- 25). Feeding tube-related complications (e.g., dislodgement, blockages) were the most common cause of ED visits, accounting for 28/60 (47%) of all visits. The second most common cause for an ED visit was evaluation after a fall (8/60, [13%]), followed by urogenital infections (5/60, [8%]), skin infections (4/60, [7%]), gastrointestinal infections (4/60, [7%]), respiratory infections (3/60, [5%]), fractures (2/60, [3%]), and other single occurrence diagnoses (6/60, [10%]).
Table 1. Characteristics of Nursing Home Residents with Advanced Dementia and Health Care Proxies According to Hospital Transfer a among Assessments with an Acute Medical Event (N=610 events).
| N (%) | N (%) with hospital transfer | Unadjusted Odds Ratio (95% CI) | Adjusted Odds Ratio b (95% CI) | ||
|---|---|---|---|---|---|
| With characteristic | Without characteristic | ||||
| Resident characteristics | |||||
| Age above median (85 y) | 294/610 (48.2) | 19/294 (6.5) | 48/316 (15.2) | 0.39 (0.21-0.73) | 0.43 (0.22-0.80) |
| Female | 522/610 (85.6) | 49/522 (9.4) | 18/88 (20.5) | 0.40 (0.19-0.84) | 0.62 (0.29-1.33) |
| Race, white vs. other | 569/610 (93.3) | 57/569 (10.0) | 10/41 (24.4) | 0.35 (0.13-0.89) | 0.47 (0.16-1.42) |
| Length of NH stay above median (1116 days) | 301/610 (49.3) | 29/301 (9.6) | 38/309 (12.3) | 0.76 (0.41-1.42) | N/A |
| Special care dementia unit | 289/610 (47.4) | 23/289 (8.0) | 44/321 (13.7) | 0.54 (0.29-1.03) | 0.74 (0.39-1.41) |
| BANS-Sc score above median (22) | 208/610 (34.1) | 18/208 (8.7) | 49/402 (12.2) | 0.68 (0.39-1.20) | N/A |
| Feeding tube | 76/610 (12.5) | 14/76 (18.4) | 53/534 (9.9) | 2.05 (0.90-4.69) | 1.39 (0.51-3.78) |
| Lack of do-not-hospitalize order | 301/610 (49.3) | 55/301 (18.3) | 12/309 (3.9) | 5.54 (2.70-11.33) | 5.22 (2.31-11.79) |
| Hospice referrald | 41/447 (9.2) | 4/41 (9.8) | 48/406 (11.8) | 0.81 (0.29-2.25) | N/A |
| Coronary artery disease | 118/610 (19.3) | 9/118 (7.6) | 58/492 (11.8) | 0.62 (0.20-1.89) | N/A |
| Congestive heart failure | 130/610 (21.3) | 17/130 (13.1) | 50/480 (10.4) | 1.29 (0.68-2.45) | N/A |
| Chronic obstructive pulmonary disease | 94/610 (15.4) | 17/94 (18.1) | 50/516 (9.7) | 2.06 (1.06-3.98) | 2.11 (1.03-4.31) |
| Health care proxy characteristics | |||||
| Age above median (59 y) | 314/610 (51.5) | 21/314 (6.7) | 46/296 (15.5) | 0.39 (0.21 -0.72) | 0.62 (0.32-1.22) |
| Female | 361/610 (59.2) | 40/361 (11.1) | 27/249 (10.8) | 1.36 (0.33-5.64) | N/A |
| Proxy is child of resident | 412/610 (67.5) | 50/412 (12.1) | 17/198 (8.6) | 1.47 (0.77-2.82) | N/A |
| Primary goal of care is comfort | 405/610 (93.1) | 48/405 (11.9) | 4/30 (13.3) | 0.87 (0.35-2.21) | N/A |
| Understands expected complications of advanced dementia | 497/610 (81.5) | 52/497 (10.5) | 15/113 (13.3) | 0.76 (0.36-1.62) | N/A |
| Acute medical event characteristics | |||||
| Documented proxy care discussion | 153/610 (32.6) | 18/153 (11.8) | 26/316 (8.2) | 1.49 (0.73-1.62) | N/A |
| Type of acute medical event | |||||
| Febrile illness | 343/610 (56.2) | 21/343 (6.1) | 46/267 (15.7) | 1.00 (reference) | N/A |
| Pneumonia | 225/610 (36.9) | 30/225 (13.3) | 37/385 (9.6) | 2.36 (1.34-4.17) | 1.86 (1.07-3.21) |
| Other evente | 42/610 (6.9) | 16/42 (38.1) | 51/608 (8.4) | 9.44 (4.40-20.2) | 11.90 (5.13-27.61) |
Hospitalization or emergency department visit
Includes all covariates associated with outcome at p <0.1 level, also adjusted for clustering due to repeated observations
Bedford Alzheimer's Nursing Severity Subscale (range 7-28, higher scores indicate greater disability)
Data not collected at baseline assessment
seizure, hip fracture, myocardial infarction, stroke, or gastrointestinal bleed
Figure 1.
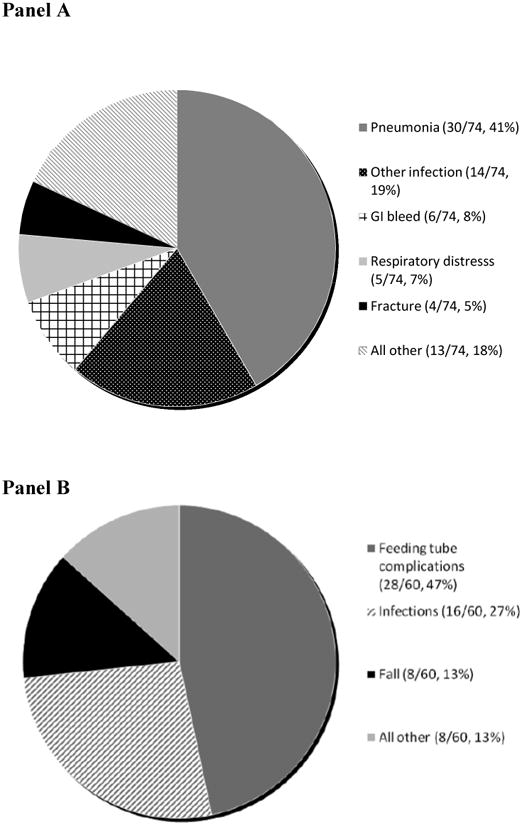
Diagnoses leading to hospital admissions (Panel A, n= 74 hospitalizations) and emergency department visits (Panel B, n = 60 visits) among nursing home residents with advanced dementia
Predictors of hospital transfer after acute medical event
There were 610 acute medical events (225 pneumonias, 343 febrile episodes and 42 other events), which occurred among 237 residents. Seizures accounted for 14 of the 42 other events (33%), gastrointestinal bleeding for 11 (26%), hip fractures for 3 (7%), other bone fractures for 4 (10%), stroke for 3 (7%), pulmonary embolus for 1 (2%), myocardial infarction for 1 (2%), and other events for 5 (12%). Among all assessments where an acute medical event occurred, 67/610 (11%) resulted in a hospital transfer. Table 1 displays the association between resident, HCP and event characteristics and whether or not the resident was transferred to the hospital for the acute medical event. In unadjusted analysis, resident characteristics associated with being transferred to the hospital at a p value <0.1 included: younger age, male gender, non-white race, not being on a special care unit, presence of a feeding tube, lack of DNH order, and having chronic obstructive pulmonary disease. Younger HCP age and event type were also associated with hospital transfer in the unadjusted analysis. Pneumonia and other acute medical events were more likely than febrile episodes to result in hospital transfer. In adjusted analysis, younger resident age, the event type, presence of chronic obstructive pulmonary disease and the lack of a DNH order were associated with a greater likelihood of hospital transfer.
Discussion
This study examines hospital transfers among a cohort of NH residents with advanced dementia. Overall, 16% of residents were hospitalized and 10% visited the ED over the 18 month period. Although the rates of hospital transfer were modest, the majority of hospitalizations were potentially avoidable, as 59% were due to infections that may be treatable in the NH setting. Feeding tube-related complications accounted for almost half of all ED visits, representing a significant but unrecognized burden associated with this intervention. The presence of a DNH order was the only modifiable factor independently associated with a reduced likelihood of hospitalization for an acute illness.
Ideally, the decision to hospitalize a NH resident with advanced dementia should be guided by the overall goals of care. For the majority of patients where the goal is comfort (96%),15 hospitalization is unlikely to be consistent with that goal except for rare events, such as a hip fracture. For the minority of residents where life prolongation is the goal, hospitalization may make sense, although most acute illnesses observed in our cohort can be potentially treated with the same efficacy in the NH setting at lower cost and with less disruption to patients and families. For example, prior research shows that hospitalization for NH residents with pneumonia does not improve functional status or survival when compared to those treated on-site.9, 16
Hospital transfers in this patient population can be anxiety provoking, due to the stress of unfamiliar surroundings and medical personnel, and the likelihood of invasive testing. Hospital transfers have been shown to also be distressing to families,8 and increase the risk of delirium.17 Once hospitalized, patients with dementia are at greater risk than others of receiving burdensome interventions such as intravenous lines and restraints.7 Furthermore, care transitions between hospital and NH place patients at risk of medical errors and adverse drug events.18-20 Finally, hospitals are a key site of medical decision-making although the conditions for decision-making may be suboptimal due to the discontinuity of care, unfamiliar providers and pressures for timely discharge. For example, among patients with advanced dementia, 68% of feeding tubes, which are of questionable benefit in this population,21 are placed during an acute hospitalization.22 It is notable that although only 8% of the CASCADE cohort had a feeding tube, feeding tube complications were the most common reason for ED visits. This observation underscores the need to communicate this previously undescribed burden of tube-feeding to families considering this intervention for their loved ones with advanced dementia.
Our results indicate that DNH orders were the only modifiable factor associated with lower likelihood of hospital transfer. Because decisions regarding hospitalization are common in this population, advance care planning for NH patients with dementia should include periodic discussions that identify the primary goals of care and consideration of whether or not a hospitalization would be consistent with goal for anticipated complications (e.g., pneumonia). As such, avoiding unnecessary or undesired hospitalizations using advance directives such as DNH orders has the potential to prevent a potentially burdensome experience for residents and families, and at the same time lower Medicare expenditures.5
Our results should be interpreted in light of several limitations. The CASCADE study was limited to the Boston area and a mostly white and well-educated cohort, which may limit the generalizability of our findings. However, the facility and resident characteristics are comparable to similar cohorts nationwide.23 Data regarding acute illness and hospital transfers was obtained from chart reviews and may contain inaccuracies, and although we sought to identify factors associated with hospital transfer after acute medical events, our characterization of such events was limited to pneumonia, febrile episode and acute illness. Although the prevalence of DNH orders was high in our population, we expect the relationship between DNH orders and transfers to be generalizable to other populations. Finally, due to limitations of the size of our cohort, we may have been unable to determine associations due to lack of power, and we were unable to account for facility level characteristics which may have affected transfers.
Reducing unnecessary or burdensome hospital transfers is an important goal for patients, their families and for reducing health care expenditures. Our study found that the majority of hospital transfers were for conditions potentially treatable in the NH setting, and that feeding tubes were associated with high rates ED visits. These results highlight the importance of advance care planning, in order to determine overall goals of care and to potentially align these goals with plans for acute care treatment such as DNH orders.
Acknowledgments
Funding: This work was supported by the National Institute on Aging at the National Institutes of Health (R01 AG024091, K24AG033640 to SLM, and K23 AG034967 to JLG)
Footnotes
Conflict of Interests: None of the authors have any financial or conflict of interest to report.
Author Contributions: Concept and design: SLM, JLG, Acquisition of subjects: SLM, Data analysis: JLG, KS, KSG, Interpretation of data: JLG, KS, KSG, SLM, Preparation of manuscript: JLG, KS, KSG, SLM
Sponsor's Role: The sponsor had no role in the design or conduct of this study, data analysis, interpretation of results or preparation of manuscript.
References
- 1.Mitchell SL, Teno JM, Miller SC, et al. A national study of the location of death for older persons with dementia. J Am Geriatr Soc. 2005;53:299–305. doi: 10.1111/j.1532-5415.2005.53118.x. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361:1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fillenbaum G, Heyman A, Peterson BL, et al. Use and cost of hospitalization of patients with AD by stage and living arrangement: CERAD XXI. Neurology. 2001;56:201–206. doi: 10.1212/wnl.56.2.201. [DOI] [PubMed] [Google Scholar]
- 4.Bynum JP, Rabins PV, Weller W, et al. The relationship between a dementia diagnosis, chronic illness, medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52:187–194. doi: 10.1111/j.1532-5415.2004.52054.x. [DOI] [PubMed] [Google Scholar]
- 5.Goldfeld KS, Stevenson DG, Hamel MB, et al. Medicare expenditures among nursing home residents with advanced dementia. Arch Intern Med. 2011;171:824–830. doi: 10.1001/archinternmed.2010.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teno JM, Mitchell SL, Gozalo PL, et al. Hospital characteristics associated with feeding tube placement in nursing home residents with advanced cognitive impairment. JAMA. 2010;303:544–550. doi: 10.1001/jama.2010.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrison RS, Siu AL. Mortality from pneumonia and hip fractures in patients with advanced dementia. JAMA. 2000;284:2447–2448. [PubMed] [Google Scholar]
- 8.Gaugler JE, Mittelman MS, Hepburn K, et al. Predictors of change in caregiver burden and depressive symptoms following nursing home admission. Psychol Aging. 2009;24:385–396. doi: 10.1037/a0016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kruse RL, Mehr DR, Boles KE, et al. Does hospitalization impact survival after lower respiratory infection in nursing home residents? Med Care. 2004;42:860–870. doi: 10.1097/01.mlr.0000135828.95415.b1. [DOI] [PubMed] [Google Scholar]
- 10.Lamberg JL, Person CJ, Kiely DK, et al. Decisions to hospitalize nursing home residents dying with advanced dementia. J Am Geriatr Soc. 2005;53:1396–1401. doi: 10.1111/j.1532-5415.2005.53426.x. [DOI] [PubMed] [Google Scholar]
- 11.Reisberg B, Ferris SH, de Leon MJ, et al. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139:1136–1139. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 12.Volicer L, Hurley AC, Lathi DC, et al. Measurement of severity in advanced Alzheimer's disease. J Gerontol. 1994;49:M223–226. doi: 10.1093/geronj/49.5.m223. [DOI] [PubMed] [Google Scholar]
- 13.Huber P. The behavior of maximum likelihood estimates under nonstandard conditions. Paper presented at: Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability; Berkeley, CA. 1967. [Google Scholar]
- 14.White H. A hereroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–830. [Google Scholar]
- 15.Mitchell SL, Teno JM, Kiely DK, et al. The Clinical Course of Advanced Dementia. N Engl J Med. 2009;361:1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loeb M, Carusone SC, Goeree R, et al. Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: A randomized controlled trial. JAMA. 2006;295:2503–2510. doi: 10.1001/jama.295.21.2503. [DOI] [PubMed] [Google Scholar]
- 17.Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: A systematic review. J Am Geriatr Soc. 2002;50:1723–1732. doi: 10.1046/j.1532-5415.2002.50468.x. [DOI] [PubMed] [Google Scholar]
- 18.Boockvar K, Fishman E, Kyriacou CK, et al. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Intern Med. 2004;164:545–550. doi: 10.1001/archinte.164.5.545. [DOI] [PubMed] [Google Scholar]
- 19.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 20.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: A review of the evidence. JAMA. 1999;282:1365–1370. doi: 10.1001/jama.282.14.1365. [DOI] [PubMed] [Google Scholar]
- 22.Teno JM, Mitchell SL, Skinner J, et al. Churning: the association between health care transitions and feeding tube insertion for nursing home residents with advanced cognitive impairment. J Palliat Med. 2009;12:359–362. doi: 10.1089/jpm.2008.0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell SL, Kiely DK, Jones RN, et al. Advanced dementia research in the nursing home: The CASCADE study. Alzheimer Dis Assoc Disord. 2006;20:166–175. doi: 10.1097/00002093-200607000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]


