Abstract
William's syndrome is a chromosomal disorder characterized by multisystem, congenital and panethnic occurrence, characterized by a number of developmental and physical abnormalities. This case report describes the dental management of a 10-year-old male patient with William's syndrome who had multiple dental problems such as caries, periodontal disease and malocclusion.
Keywords: Dentofacial characteristics, dental management, special considerations, William's syndrome
Introduction
William's syndrome, also known as William's-Beuren syndrome or Elfin-facies syndrome, was first described in 1961 as an association of supravalvular aortic stenosis and mental retardation in four children with characteristic facies by J.C.P William. Beuren et al. described the syndrome independently and expanded the phenotype to include peripheral pulmonary artery stenosis and dental malformations.[1]
The Mendelian Inheritance in Man (MIM) number for William's syndrome is #194050.[2] The incidence is around 1 in 10,000 live births. In most individuals, the disorder appears to occur sporadically. However, familial cases have also been reported. Cases are thought to result from deletion of genetic material from adjacent genes (contiguous genes) within a specific region of chromosome 7 (7q11.23).[3]
Clinical diagnosis is based on physical and developmental characteristics. Medical diagnosis shows a deletion of genetic material including the elastin gene on chromosome #7.[3]
There is no cure for William's syndrome. Treatment is symptomatic and supportive. Individuals with William's syndrome need regular monitoring for potential medical problems by a physician familiar with the disorder. The pediatric dentist can act in dental rehabilitation procedures and also behavior modification.
Case Report
A male patient of age 10 years reported to the Department of Pedodontics and Preventive Dentistry, with a chief complaint of pain in the lower right back tooth region. Medical history revealed that he had been diagnosed of William's syndrome 6 months after birth. His parents gave a history of swallowing problem and failure to thrive as an infant.
He had mild mental retardation, hyperacusis and increased anxiety. General examination revealed abnormal gait, sloping shoulders, relatively short limbs, clubbed finger nails, hallus valgus and soft skin [Figure 1,2]. Classic facial features were broad forehead, spiked hair, broad eyebrows, bitemporal narrowness, periorbital fullness, short palpebral fissures, epicanthal folds, short nose, depressed nasal bridge, long philtrum, broad flattened thick lips, and wide mouth [Figure 3].
Figure 1.
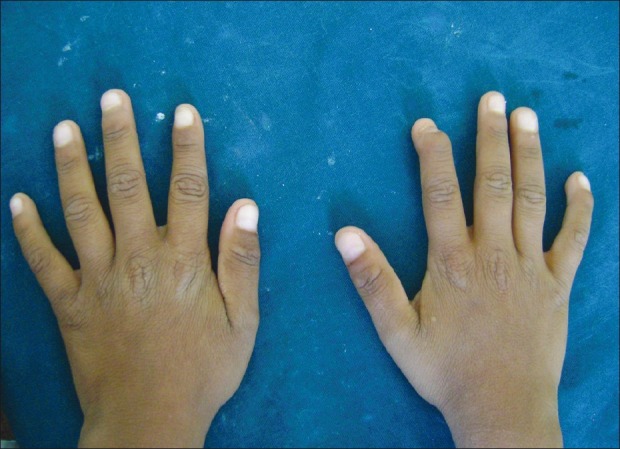
Clubbed finger nails
Figure 2.

Hallus valgus(great toe)
Figure 3.

Craniofacial features
Intraoral examination revealed class I molar relation bilaterally with anterior open bite and widely spaced dentition. Deep proximal caries was seen in A, B, J, K, L and S (Universal system). Deep caries with pulpal involvement was seen in T. Smooth surface caries were seen in the labial aspect of C, M and R. Chronic generalized gingivitis was seen because of poor oral hygiene. The patient presented with excessive salivation and tongue thrusting [Figures 4,5,6].
Figure 4.

Intraoral findings-teeth in occlusion
Figure 5.

Intraoral findings-maxillary arch
Figure 6.

Intraoral findings-mandibular arch
Radiographic examination revealed mild taurodontism of both primary and permanent dentition [Figure 7].
Figure 7.

Radiographic findings
The patient required a complete oral rehabilitation. Consultation was taken from a pediatrician for the dental procedures to be carried out. The following tests were carried out to rule out any systemic condition: transdermal skin test for allergy to lignocaine, cardiovascular evaluations for cardiovascular abnormalities and hypertension, eye test for vision and strabismus and blood investigation. All the reports were normal.
Although the patient presented with cooperative behavior and was able to follow instructions, he was unable to sit for a longer duration and would become irritable. Hence, it was decided to treat the patient in an outpatient surgery setting with a short duration of appointments utilizing behavior management technique – tell-show-do.
Oral prophylaxis, pulpectomy in relation to A, B, J, T, pulpotomy in relation to K followed by stainless steel crown and restoration with glass ionomer cement in relation to C, M and, R was carried out. No complications presented during the treatment and the patient returned for follow-up visits after the next 6 months [Figures 8,9,10].
Figure 8.

Follow-up photographs- teeth in occlusion
Figure 9.

Follow-up photographs- maxillary arch
Figure 10.

Follow-up photographs-mandibular arch
Discussion
William's syndrome (idiopathic hypercalcemia–supravalvular aortic stenosis syndrome) consists of a constellation of manifestations that overlap with hypercalcemia with or without mental retardation and supravalvular aortic stenosis with or without mental retardation.
Diagnosis is usually made in mid-childhood when characteristic features, cognitive profiles and cardiac findings become more apparent. One of the first indications that a neonate may have William's syndrome is “prolonged gestation” (>42 weeks), with birth weight and length in the 5th–50th percentile. Other manifestations are feeding difficulties, profuse vomiting and failure to thrive. Owing to variability in the clinical findings, diagnosis is usually confirmed by chromosomal fluorescent in situ hybridization analysis or polymerase chain reaction. Prenatal diagnosis of the deletion of 7q11.23 is available for families at high risk, using chorionic villous sampling or amniocentesis. There is no screening test for the general population.[3]
Craniofacial and dental findings
Facial dysmorphology is considered to be a diagnostic feature in patients with William's syndrome, and is composed of soft tissue and skeletal components. The gene GTF2IRD1 part of the TFII-1 transcription family has been implicated in the craniofacial features of William's syndrome.[2,4]
According to Mass and Belostoky,[3] four skeletal features contribute to the facial appearance of children with William's syndrome: a short cranial base, the steep angle of the mandibular plane, an unusual proportion of upper to lower anterior facial height and posterior to anterior facial height, and a deficient chin, although the mandible could not be classified as retrognathic. Patients demonstrated a higher than normal prevalence of class II and class III occlusions, open and deep bites, and anterior cross-bites. Mild micrognathia, osteosclerotic changes in the lamina dura (particularly in the premolar–molar region), folding and thickening of the buccal mucous membranes, and prominent accessory labial frenula are observed. Hypoplasia of teeth, high prevalence of tooth agenesis, severe dental decay, oligodontia, pulp stones, microdontia, and abnormally small roots, tapered or screwdriver-shaped incisors, bud-shaped maxillary primary second molars, and mandibular permanent molars have been observed. Abnormal tooth morphology was noted in 12.5% of the primary dentitions and in 40.7% of the permanent dentitions. Malocclusion was noted in 85% of the cases, tongue thrusting in 67.7%, while more than 50% of the patients had excessive interdental spacing.[1,5–7] The craniofacial findings present in the present case were similar to the features described by Moti Moskovitz.[3]
Medical considerations in treating these patients include:[1,3,7,9] (i) cardiovascular and renal defects, which require general anesthetic and dosage of drugs modification. The major cause of morbidity is narrowing of arteries due to stenosis, hypoplasia, or coarctation. Renal defects lead to hypercalcemia, impaired renal function, elevated blood urea, and creatine levels. Cardiovascular and renal defects progress with age. Patients require premedication to reduce anxiety and administration of prophylactic antibiotics for subacute bacterial endocarditis. (ii) Neurological defects – mental retardation, impairment in perceptual motor integration and inability to cooperate, and hyperactivity disorder, which may require treatment consideration under sedation. Hyperacusis in 74–95% of the patients has been reported, which leads to easy distraction. This requires treating with caution to avoid mishaps due to sudden involuntary patient movement while treating in an outpatient surgery setting.[2]
Cognitive, motor, and language delay are universal, and mental retardation is ultimately diagnosed. Older children demonstrate a relative strength in language and auditory memory, with a significant weakness in visuospatial cognition. Behavioral problems may include hypersensitivity to sound, sleep problems, attention-deficit/hyperactivity disorder, and anxiety. Overfriendliness and an empathetic nature are commonly observed.
Younger children suffer from anorexia and vomiting, which requires early dental evaluation and dietary counseling.
Dental considerations[1,3,7,9]
Dental anomalies, caries and malocclusion require nutritional counseling, dental restorative treatments, and orthodontic consultations. The caries rate is not more than in the general population. But, in children with hypoplasia, additional preventive measures need to be taken to reduce the occurrence of caries. Sedation and general anesthesia techniques are used in treating uncooperative children.
The AAPD has set guidelines for special considerations for the child diagnosed with William's syndrome.[8] Establishment of medical and dental home with clear emphasis on continuity of care and the role of the family members as partners in the ongoing management and care of the child is required. William's syndrome patients require a multi-disciplinary approach, taking into consideration their medical conditions and modifying treatment options to improve the quality of life of these patients.[9]
Conclusion
With the occurrence of sporadic cases of William's syndrome, knowledge about their diagnosis, general health, and mode of delivering treatment help the dentists to deliver a more appropriate treatment.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Axelsson S, Bjornland T, Kjær I, Heiberg A, Storhaug K. Dental characteristics in William's syndrome: A clinical and radiographic evaluation. Acta Odontologica Scandinavica. 2003;61:129–36. doi: 10.1080/00016350310001451. [DOI] [PubMed] [Google Scholar]
- 2. [Last accessed on 2011 Aug 28]. Available from: http://www.ncbi.nlm.nih.gov/omim/194050 .
- 3.Moskovitz M, Brener D, Faibis S, Peretz B. Medical considerations in dental treatment of children with William's syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:573–80. doi: 10.1016/j.tripleo.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 4.Jones KI. Smith's recognizable patterns of human malformations. Philadelphia: WB Saunders Publication; 1988. pp. 106–7. [Google Scholar]
- 5.Jones KL, Smith DW. The Williams elfin facies syndrome. A new perspective. J Pediatr. 1975;86:718–23. doi: 10.1016/s0022-3476(75)80356-8. [DOI] [PubMed] [Google Scholar]
- 6.Kelly JR, Barr ES. The elfin facies syndrome. Oral Surg Oral Med Oral Pathol. 1975;40:205–18. doi: 10.1016/0030-4220(75)90153-x. [DOI] [PubMed] [Google Scholar]
- 7.Hertzberg J, Nakisbendi L, Needleman HL, Pober B. Williams's syndrome- oral presentation of 45 cases. Pediatr Dent. 1994;16:262–7. [PubMed] [Google Scholar]
- 8.American Academy Of Pediatrics: Health Care Supervision for Children With Williams Syndrome. Committee on Genetics. Pediatrics. 2001;107:1192–204. [PubMed] [Google Scholar]
- 9.Boraz RA. Williams (Elfin facies) syndrome: Review of literature and report of a rare case. ASDC J Dent Child. 1991;58:57–9. [PubMed] [Google Scholar]


