Abstract
Traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) is a benign, self-limiting lesion of the oral mucosa with unknown pathogenesis. A 65-year-old male patient presented with an ulcerative palate lesion, which on microscopic examination exhibited an exuberant polymorphic lymphoid proliferation, numerous eosinophils, and extensive vascular destruction. The atypical lymphoid cells infiltrating the medium-sized vessels showed positivity for CD3, CD30, and granzyme B, implicating an activated cytotoxic T-cell phenotype. The lesion diagnosed as TUGSE achieved complete resolution within 3 months. This unusual presentation has expanded the spectrum of oral CD30+ T-cell atypical infiltrates and must be distinguished from lymphomas showing angiocentric/angiodestructive growth pattern.
Keywords: Angiocentric growth pattern, Eosinophilic ulcer, Immunohistochemistry, Malignant lymphoma, Traumatic ulcerative granuloma with stromal eosinophilia
Introduction
Traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) is a benign lesion of the oral mucosa of unclear pathogenesis. Eosinophils and cytotoxic large atypical CD30+ cells may be observed, with some authors considering that a subset of TUGSE could be better classified as the oral counterpart of the primary cutaneous CD30+ lymphoproliferative disorders (LPDs).[1–3] TUGSE with extensive vascular destruction mimicking malignant lymphoma is unusual. This angiocentric/angiodestructive growth pattern is characteristic of natural killer (NK)/T-cell lymphoma, nasal type, being rare in other LPDs.[4,5] Moreover, Baum et al.[6] report an interesting case of a post-traumatic atypical intravascular CD30+ T-cell proliferation, which followed a benign clinical course. Herein, we report a case of TUGSE affecting the palate with angiodestructive features, thus expanding the spectrum of oral reactive lesions with CD30+ T-cell atypical infiltrates.
Case Report
A 65-year-old male patient was referred to Dentistry School, Federal University of Sergipe (UFS), Brazil, presenting a painful ulcerated lesion in the hard palate for 20 days. The medical history was noncontributory and extraoral examination did not show any alterations. Intraoral examination showed an ulcerative lesion of 1.5 cm in diameter in the left hard palate, covered by a yellowish fibrinopurulent membrane encircled by an erythematous halo [Figure 1]. There were neither regional lymphadenopathies nor radiographical alterations. The main clinical differential diagnosis was necrotizing sialometaplasia. The histopathological examination showed extensive areas of superficial necrosis and deeply an exuberant polymorphic lymphoid infiltrate. Most of the lymphocytes were medium-sized and large, presenting clear to pale cytoplasm, irregular nuclei, and conspicuous nucleoli, surrounded by numerous eosinophils. Mitotic figures were common. The atypical lymphoid cells admixed with eosinophils showed a multifocal angiocentric and angiodestructive infiltration. Although some blood vessels exhibited endothelial cells with an epithelioid-like appearance and strongly reduced lumen, others showed complete vascular occlusion. Periodic acid-Schiff (PAS) stain highlighted the internal elastic membrane of medium-sized arteries, which showed atypical large cells, some of them with mitotic figures, infiltrating the muscular layers [Figure 2]. In spite of the worrisome features, an aggressive reactive process was considerate firstly; nevertheless, a malignant lymphoma was not fully discarded. After immunohistochemical (IHC) and in situ hybridization (ISH) analysis, a diagnosis consistent with TUGSE showing angiocentric/angiodestructive features was suggested. The lesion achieved complete resolution within 3 months and no recurrence or alteration was noticed after 3 years of follow-up.
Figure 1.

Clinical view of an ulcerative lesion on the left hard palate, diagnosed as TUGSE showing angiocentric/angiodestructive pattern
Figure 2.
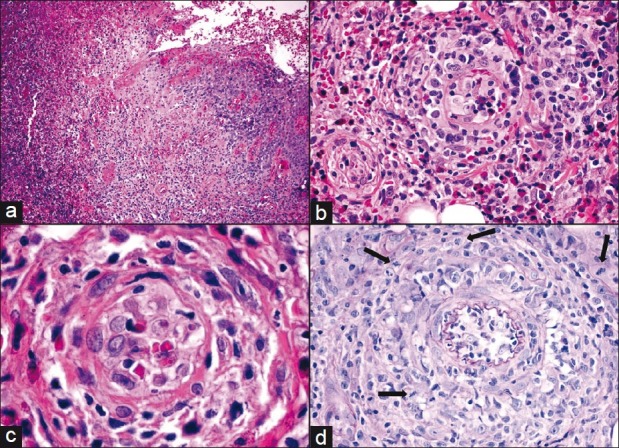
Superficial necrosis and polymorphous infiltrate (a, × 10). Atypical lymphoid cells admixed with eosinophils showing angiocentric infiltration (b, × 40). In high power, cellular details (c, × 100). A medium-sized artery showing angiocentric/ angiodestructive features and atypical large cells with mitotic figures (arrows) (d, PAS × 40)
IHC analysis using CD1a, CD3, CD15, CD20, CD30, CD31, CD34, CD45, CD68 (PG-M1), granzyme B, D2-40, S100, Ki-67 (MIB-1) (DAKO, Carpinteria, CA, USA), CD56 (Novocastra, Newcastle upon Tyne, England), and ISH staining for EBER (Epstein-Barr virus-encoded small nuclear RNA) complementary to EBV EBER1 and EBER2 loci (EBER, PNA probes, DAKO, Denmark) were performed. Both atypical large and medium-sized cells were positive for CD3, CD30, and granzyme B, whereas CD45 and CD56 were negative [Figure 3]. The majority of the benign small lymphocytes were CD3+ T-cells, whereas only rare small CD20+ B-cells were present. ISH staining for EBER1/2 was negative. CD31 and CD34 highlighted the epithelioid-like appearance of the endothelial cells, while D2-40 showed scarce slit-like lymphatic vessels. Moreover, CD68 (PG-M1) evidenced numerous reactive histiocytes and isolated S100-positive interstitial dendritic-like cells were also visualized. The Ki-67 labeling index was 10%.
Figure 3.
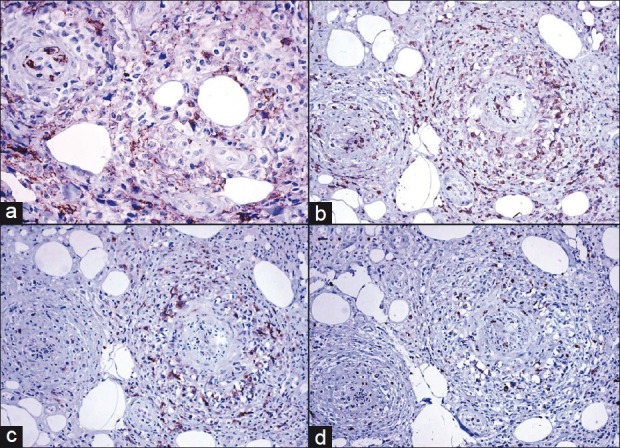
The atypical large- and medium-sized cells were negative for CD45 (a, OM × 40), and positive for CD3 (b), CD3O (c), and granzyme B (d) (OM × 20), showing an activated cytotoxic T-cell immunophenotype
Discussion
TUGSE is a benign, rapidly growing ulcerative nodule of the oral cavity, with self-limited course. The cause of TUGSE is unknown; however, trauma is considered an important contributing factor. The tongue is the most common location and there is a slight female predominance, with a peak of incidence between the sixth and seventh decades of life.[2] The current case had no history of trauma, affected the palate, an unusual location, exhibited vascular damage, and showed spontaneous regression. The unusual multifocal angiocentric and angiodestructive growth pattern were suggestive of NK/T-cell lymphoma, nasal type. Nevertheless, the absence of bone involvement, negativity for CD45, CD56, and EBER1/2, along with the prominent eosinophilic infiltrate, discarded this diagnosis.
The angiocentric and angiodestructive growth pattern observed typically in NK/T-cell lymphoma, nasal type, also can be found in other non-Hodgkin lymphomas such as T-cell-rich large B-cell lymphoma, mycosis fungoides, hydroa-like lymphoma, lymphomatoid granulomatosis, and adult T-cell leukemia/lymphoma.[4] Approximately, 40 cases of intravascular large T-cell or NK-cell lymphoma involving mainly the skin and following an aggressive clinical course have been described, but they are rarely CD30 positive.[5] On the other hand, Baum et al.[6] reported an interesting case of a post-traumatic atypical intravascular CD30+ T-cell proliferation which followed a benign clinical course. These findings, together with the histopathological features of the current case, indicate that there are malignant and reactive/benign lymphoid conditions which can show angiocentric/angiodestructive and intravascular patterns and must be recognized as such to avoid misdiagnosis.
Non-Hodgkin lymphoma with extensive infiltrate of neutrophils or eosinophils is extremely rare, and the diagnosis can be challenging. In these cases, cohesive sheets or small clusters of neoplastic T-cells admixed with large numbers of neutrophils and/or eosinophils are observed. Precise correlation of clinical presentation, morphological features, and phenotypic analysis are necessary in order to establish the correct diagnosis. To date, approximately 19 cases of neutrophil/eosinophil-rich type primary cutaneous anaplastic large cell lymphoma have been reported.[7] To our best knowledge, no case of malignant lymphoma with these features has been described in the oral cavity.
Eosinophil-rich lesions affecting the oral cavity include angiolymphoid hyperplasia with eosinophilia (ALHE), Kimura disease, Langerhans cell histiocytosis, infectious diseases, as well as contact allergy, drug reactions, and immunobullous diseases, all excluded in the current case through a careful clinicopathologic correlation.[8] Interestingly, Cham et al.[9] showed that the ALHE lymphoid component may contain large activated CD30+ cells, suggesting that a subset of it might represent a form of low-grade T-cell LPD.
Conclusion
TUGSE is a benign, self-limited oral lesion, of unknown pathogenesis, showing a polymorphous histological spectrum and that clinically and microscopically can be confused with malignancy. The angiocentric/angiodestructive growth pattern in TUGSE, as shown in the present report, is unusual but it should be recognized to avoid misdiagnosis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Agarwal M, Shenjere P, Blewitt RW, Hall G, Sloan P, Pigadas N, et al. CD30-positive T-cell lymphoproliferative disorder of the oral mucosa--an indolent lesion: Report of 4 cases. Int J Surg Pathol. 2008;16:286–90. doi: 10.1177/1066896907313755. [DOI] [PubMed] [Google Scholar]
- 2.Segura S, Pujol RM. Eosinophilic ulcer of the oral mucosa: A distinct entity or a non-specific reactive pattern? Oral Dis. 2008;14:287–95. doi: 10.1111/j.1601-0825.2008.01444.x. [DOI] [PubMed] [Google Scholar]
- 3.Alobeid B, Pan LX, Milligan L, Budel L, Frizzera G. Eosinophil-rich CD30+ lymphoproliferative disorder of the oral mucosa. A form of “traumatic eosinophilic granuloma”. Am J Clin Pathol. 2004;121:43–50. doi: 10.1309/JQFX-PND6-DBLF-6B9U. [DOI] [PubMed] [Google Scholar]
- 4.Shanti RM, Torres-Cabala CA, Jaffe ES, Wilson WH, Brahim JS. Lymphomatoid granulomatosis with involvement of the hard palate: A case report. J Oral Maxillofac Surg. 2008;66:2161–3. doi: 10.1016/j.joms.2008.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cerroni L, Massone C, Kutzner H, Mentzel T, Umbert P, Kerl H. Intravascular large T-cell or NK-cell lymphoma: A rare variant of intravascular large cell lymphoma with frequent cytotoxic phenotype and association with Epstein-Barr virus infection. Am J Surg Pathol. 2008;32:891–8. doi: 10.1097/PAS.0b013e31815d29c9. [DOI] [PubMed] [Google Scholar]
- 6.Baum CL, Stone MS, Liu V. Atypical intravascular CD30+ T-cell proliferation following trauma in a healthy 17-year-old male: First reported case of a potential diagnostic pitfall and literature review. J Cutan Pathol. 2009;36:350–4. doi: 10.1111/j.1600-0560.2008.01033.x. [DOI] [PubMed] [Google Scholar]
- 7.Kong YY, Dai B, Kong JC, Lu HF, Shi DR. Neutrophil/eosinophil-rich type of primary cutaneous anaplastic large cell lymphoma: A clinicopathological, immunophenotypic and molecular study of nine cases. Histopathology. 2009;55:189–96. doi: 10.1111/j.1365-2559.2009.03359.x. [DOI] [PubMed] [Google Scholar]
- 8.Kempf W, Haeffner AC, Zepter K, Sander CA, Flaig MJ, Mueller B, et al. Angiolymphoid hyperplasia with eosinophilia: Evidence for a T-cell lymphoproliferative origin. Hum Pathol. 2002;33:1023–9. doi: 10.1053/hupa.2002.128247. [DOI] [PubMed] [Google Scholar]
- 9.Cham E, Smoller BR, Lorber DA, Victor TA, Cibull TL. Epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia) arising on the extremities. J Cutan Pathol. 2010;37:1045–52. doi: 10.1111/j.1600-0560.2009.01400.x. [DOI] [PubMed] [Google Scholar]


