Abstract
Adenomatoid odontogenic tumor (AOT) is a rare odontogenic tumor which is often misdiagnosed as odontogenic cyst and accounts for about 1% until 9% of all odontogenic tumors. It is predominantly found in young and female patients, located more often in the maxilla in most cases associated with an unerupted permanent tooth. It is a benign (hamartomatous), noninvasive lesion with slow but progressive growth. There are three variants of AOT: follicular, extrafollicular, and peripheral. We report a rare case of follicular-type AOT in the mandible of a 14-year-old male patient who presented with right -sided jaw swelling.
Keywords: Adenomatoid odontogenic tumor, benign, hamartoma, odontogenic tumors
Introduction
Adenomatoid odontogenic tumor (AOT) was first reported by Harbitz as cystic adamantoma.[1] Philipsen and Birn proposed the widely accepted and the currently used name adenomatoid odontogenic tumor.[2] In 2005, the histologic typing of World Health Organization (WHO) defined AOT as a tumor composed of odontogenic epithelium, presenting a variety of histoarchitectural patterns, embedded in mature connective tissue stroma, and characterized by slow and progressive growth.[3]
AOT is a benign (hamartomatous), noninvasive lesion. It usually affects young patients, mostly during their second decade of life. There is a tendency to affect females (male : female ratio 1 : 2) and to occur in the anterior maxillary region.[4–7] It often causes expansion of surrounding bone and displacement of adjacent teeth.[8] However, the slow-growing nature of the lesion may cause the patients tolerate the swelling for years until it produces an obvious deformity.[9] The tumor is usually associated with unerupted teeth, frequently canines or lateral incisors.[10] In this report of a case, we presented an AOT causing jaw swelling in the mandible.
Case Report
A 14-ear-old patient reported to the Department of Oral Medicine, Diagnosis and Radiology with complaint of swelling on right side of face since 6 to 7 months. The swelling was initially small in size, gradually increased, more so in last 2 months. The patient revealed no history of pain or pus discharge associated with the swelling. There was no relevant medical history suggestive of any allergy, infections, cardiovascular, respiratory, kidney, liver diseases, and mental illness. Patient was not under any medication.
Clinical examination
On examination, the face appeared asymmetrical with a swelling seen on the right side of the face, approximately 6 × 5 cm in size, extending superiorly to ala tragus line, inferiorly up to the submandibular region, anteroposteriorly from midline to anterior border of ramus [Figure 1]. The overlying skin was tense, normal in color with no draining sinuses. The swelling was nontender, firm to hard in consistency with diffuse margins.
Figure 1.

Extraoral view of the swelling
Intraorally, the patient had retained 83, 84, and 85 [Figure 2]. There was obliteration of mandibular right vestibule in 83-46 region due to swelling, which was hard in consistency. There was little expansion of buccal cortex.
Figure 2.

Intraoral view of the swelling
Radiographic features
Orthopantomogram showed presence of well-defined radiolucency in right mandibular region with flecks of calcification extending from 83-46 region associated with impacted 43, 44, and 45. 43 was displaced to the inferior and medial aspect of the lesion and 44 and 45 were at the superior and lateral aspect of the lesion. Over-retained 83, 84, and 85 were seen. Right mandibular canal could not be traced anterior to 46. Expansion/bowing of the lower border of the mandible was also seen [Figure 3].
Figure 3.

OPG showing impacted teeth and expansion of the lower border of the mandible
CT(Computed tomography) scan revealed the presence of isodense non-enhancing mass in the mandible with expansion of the buccal and lingual cortical plates. The lesion extended from 43-46 region and foci of calcification were seen throughout the lesion. Impacted teeth were seen at the superolateral aspect of the lesion and inferomedial aspect of the lesion [Figures 4 and 5].
Figure 4.
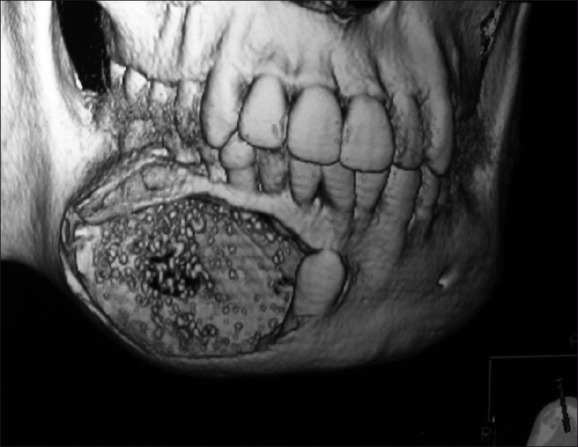
CT scan revealing the presence of isodense non-enhancing mass in the mandible
Figure 5.
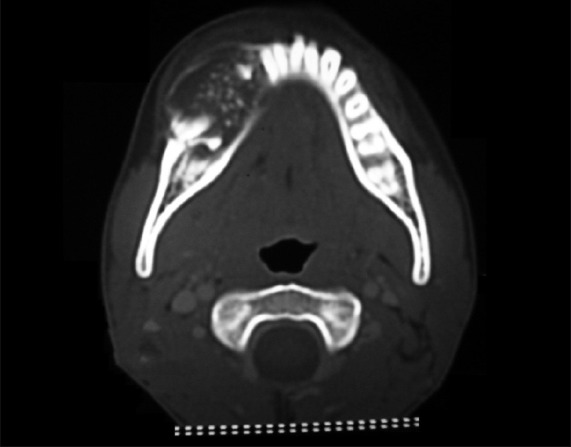
CT scan revealing the expansion of the buccal and lingual cortical plates
A provisional diagnosis of AOT was made. FNAC(Fine needle aspiration cytology) was done following which the lesion was excised under general anesthesia. Separating the lesion from the mandible caused no problems [Figures 6 and 7]. The postoperative course was uneventful [Figure 8].
Figure 6.
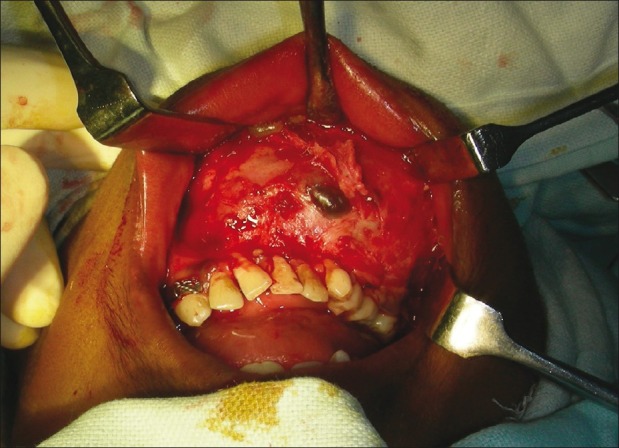
Operative procedure being carried out
Figure 7.
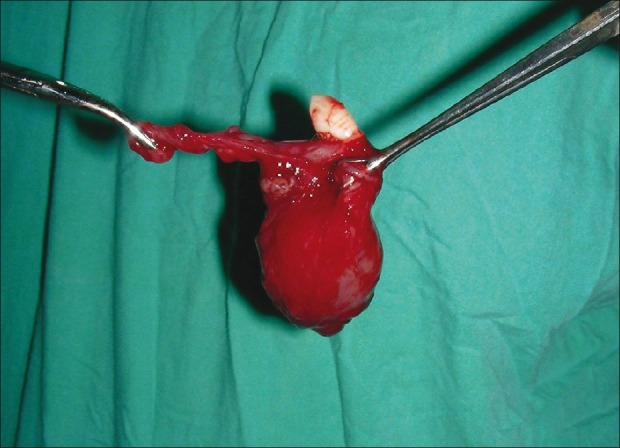
Removal of the lesion
Figure 8.

Postoperative view of the lesion
Microscopic features
FNAC from the lesion showed proteinaceous fluid with few RBCs(red blood cells), polymorphonuclear lymphocytes, and macrophages. No definitive diagnosis could be made.
The excisional biopsy report revealed a duct-like pattern. The central space was surrounded by a layer of columnar or cuboidal epithelial cells. Small foci of calcification were scattered throughout the lesion. The features were suggestive of AOT [Figure 9].
Figure 9.
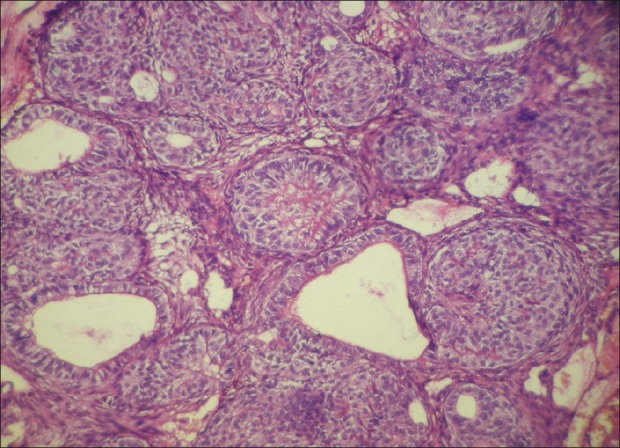
Fine needle aspiration cytology of the lesion
Discussion
There are three clinicopathologic variants of AOT, namely intraosseous follicular, intraosseous extrafollicular, and peripheral, all with identical histology. The follicular type is a central intraosseous lesion associated with an impacted tooth, while extrafollicular intraosseous AOT has no relation with an unerupted tooth. Despite this, it is often located between, above, or superimposed upon the roots of adjacent erupted teeth. The peripheral variant appears as a gingival fibroma or epulis attached to the labial gingiva.[10]
The lesion usually appears unilocular radiologically, although a few multilocular cases have been reported. Radiologically, it should be differentiated from dentigerous cyst, which most frequently occurs as pericoronal radiolucency in the jaws. Dentigerous cyst encloses only the coronal portion of the impacted tooth, whereas AOT shows radiolucency usually surrounding both the coronal and radicular aspects of the involved tooth.[11] Irregular root resorption is seldom reported.[12] Displacement of the neighboring teeth due to tumor expansion is more common than root resorption. Minute, variable-shaped radiopacities are frequently found within the lesion. These calcified deposits are seen in 78% of AOTs. The extraosseous, peripheral, or gingival types of AOT are rarely detected radiographically, but there may be slight erosion of the underlying alveolar bone cortex.[10,13]
Common neoplastic causes, such as ameloblastoma, calcifying epithelial odontogenic tumor (CEOT), ameloblastic fibroma, and ameloblastic fibro-odontoma, which are taken into consideration in the differential diagnosis are easily differentiated on histology. CEOT shows larger and more numerous calcifying spherules within eosinophilic cytoplasm of large cells along with smaller cells with hyperchromatic nuclei. Amyloid-like eosinophilic material is also present. Ameloblastoma has characteristic lining and arrangement with stellate reticulum besides usual location in mandible and posterior maxilla in contrast to AOT that is located in anterior maxilla.[14]
Structurally, AOT is a well-circumscribed lesion, derived from odontogenic epithelium, which, at least in the follicular variety as described here, usually establishes itself around the corona of unerupted, anterior teeth in young patients, being constituted of whorled nests of epithelium together with areas of glandular or ductal patterns intermixed with occasional spherical calcifications.[15,16] Eosinophilic, amorphous, uncalcified material called “tumor droplets” can be found. They may reveal electron-dense plaques or homogenous matrix.[17]
Immunohistochemical and ultrastructural findings have shown that the eosinophilic deposits (amyloid-like material) most probably represent some form of enamel matrix.[8] Immunohistochemically, the classic AOT phenotype is characterized by a cytokeratin profile similar to follicular cyst and/or oral or gingival epithelium based on positive staining with CK5, CK17, and CK19.[18] Classic AOT is negative for CK4, CK10, CK13, and CK18. The detection of CK14 in AOT by Crivelini et al. indicates its origin in reduced dental epithelium.[19] The histogenesis of AOT is still uncertain, although recent findings strongly indicate that AOT is derived from a complex system of dental laminae or its remnants. It is often considered as a hamartomatous lesion rather than a true neoplasm.[20]
All variants of AOT are well encapsulated and show an identical benign behavior. Conservative surgical enucleation or curettage is the treatment of choice with only rare recurrence.[10] For periodontal intrabony defects caused by AOT, guided tissue regeneration with membrane technique is suggested after complete removal of the tumor.[21] The patient we described in this case report is healthy without recurrence and is under follow-up after local excision.
We conclude that although AOT commonly referred to as “Two-third tumor” because of its predominance in maxilla, should also be considered in the differential diagnosis of mandibular lesions, although its incidence is low.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Harbitz F. Cystic tumours of maxilla, and especially on adamantine cystadenomas (adamantomas) Dent Cosmos. 1915;57:1081–93. [Google Scholar]
- 2.Philipsen HP, Brin H. The adenomatoid odontogenic tumour, ameloblastic adenomatoid tumour or adenameloblastoma. Acta Pathol Microbiol Scand. 1969;75:375–98. [PubMed] [Google Scholar]
- 3.Philipsen HP, Nikai H. Adenomatoid odontogenic tumour. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. In: Pathology and genetics of head and neck tumors. Lyon, France: IARC Press; 2005. pp. 304–5. [Google Scholar]
- 4.Arotiba GT, Arotiba JT, Olaitan AA, Ajayi OF. The adenomatoid odontogenic tumor: An analysis of 57 cases in a black African population. J Oral Maxillofac Surg. 1997;55:146–8. doi: 10.1016/s0278-2391(97)90231-7. [DOI] [PubMed] [Google Scholar]
- 5.Philipsen HP, Reichart PA. Adenomatoid odontogenic tumour: Facts and figures. Oral Oncol. 1999;35:125–31. doi: 10.1016/s1368-8375(98)00111-0. [DOI] [PubMed] [Google Scholar]
- 6.Batra P, Prasad S, Parkash H. Adenomatoid odontogenic tumour: Review and case report. J Can Dent Assoc. 2005;71:250–3. [PubMed] [Google Scholar]
- 7.Leon JF, Mata GM, Fregnani ER, Carlos-Bregni R, Almeida OP, Mosqueda A, et al. Clinicopathological and immunohistochemical study of 39 cases of adenomatoid odontogenic tumour. Oral Oncol. 2005;41:835–842. doi: 10.1016/j.oraloncology.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Bravo M, White D, Miles L, Cotton R. Adenomatoid odontogenic tumor mimicking a dentigerous cyst. Int J Pediatr Otorhinolaryngol. 2005;69:1685–8. doi: 10.1016/j.ijporl.2005.03.055. [DOI] [PubMed] [Google Scholar]
- 9.Olgac V, Koseoglu BG, Kasapoglu C. Adenomatoid odontogenic tumor: A report of an unusual maxillary lesion. Quintessence Int. 2003;34:686–8. [PubMed] [Google Scholar]
- 10.Dayi E, Gurbuz G, Bilge OM, Ciftcioglu MA. Adenomatoid odontogenic tumour (adenoameloblastoma).Case report and review of the literature. Aust Dent J. 1997;42:315–8. doi: 10.1111/j.1834-7819.1997.tb00136.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee JK, Lee KB, Hwang BN. Adenomatoid odontogenic tumor: A case report. J Oral Maxillofac Surg. 2000;58:1161–4. doi: 10.1053/joms.2000.9581. [DOI] [PubMed] [Google Scholar]
- 12.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2nd ed. Philadelphia: WB Saunders; 2002. pp. 621–3. [Google Scholar]
- 13.Rick GM. Adenomatoid odontogenic tumor. Oral Maxillofac Surg Clin North Am. 2004;16:333–54. doi: 10.1016/j.coms.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Rosai J. Mandible and Maxilla. In: Rosai J, editor. In: Ackerman's Surgical Pathology. 8th ed. St. Louis: Mosby; 1996. pp. 257–88. [Google Scholar]
- 15.Sempere FJ Vera, Martínez MJ Artes, Sirera B Vera. Bonet Marco Follicular adenomatoid odontogenic tumor: Immunohistochemical study. Med Oral Patol Oral Cir Bucal. 2006;11:E305–8. [PubMed] [Google Scholar]
- 16.Cossío I, Rodríguez-Armijo Sánchez L, García Calderon M, Gutiérrez Pérez JL, González Cámpora R. Tumor odontogénico adenomatoide de maxilar superior. Med Oral. 1997;2:168–71. [Google Scholar]
- 17.Philipsen HP, Reichart PA. The adenomatoid odontogenic tumor: Ultrastructure of tumor cells and non calcified amorphous masses. J Oral Pathol Med. 1996;25:491–6. doi: 10.1111/j.1600-0714.1996.tb00303.x. [DOI] [PubMed] [Google Scholar]
- 18.Larson A, Swartz K, Heikinheimo K. A case of multiple AOT-like jaw bone lesions in a young patient- a new odontogenic entity? J Oral Pathol Med. 2003;32:55–62. doi: 10.1034/j.1600-0714.2003.00046.x. [DOI] [PubMed] [Google Scholar]
- 19.Crivelini MM, de Araujo VC, de Sousa SO, de Araujo NS. Cytokeratins in epithelia of odontogenic neoplasms. Oral Dis. 2003;9:1–6. doi: 10.1034/j.1601-0825.2003.00861.x. [DOI] [PubMed] [Google Scholar]
- 20.Philipsen HP, Samman N, Ormiston IW, Wu PC, Reichart PA. Variants of the adenomatoid odontogenic tumor with a note on tumor origin. J Oral Pathol Med. 1992;21:348–52. doi: 10.1111/j.1600-0714.1992.tb01363.x. [DOI] [PubMed] [Google Scholar]
- 21.Blumenthal NM, Mostofi R. Repair of an intrabony defect from an adenomatoid odontogenic tumor. J Periodontol. 2000;71:1637–40. doi: 10.1902/jop.2000.71.10.1637. [DOI] [PubMed] [Google Scholar]


