Abstract
Wellness and pre-anesthetic screening of blood and urine of geriatric companion animals are routinely recommended. In addition, there are occasional references to the use of imaging in clinically normal geriatric patients. However, the utility of wellness testing is not known, and there is limited information regarding the value of pre-anesthetic testing. Wellness testing, including complete blood cell count, biochemical profile, urinalysis, and abdominal ultrasound, was performed on 53 clinically normal, mature golden retriever dogs. Laboratory analysis revealed abnormalities in 54.7% (29/53) of the dogs. Abdominal ultrasound screening demonstrated abnormalities in 64.2% (34/53) of the dogs. As only a small number of dogs had follow-up diagnostic testing available, the significance of these abnormalities is unknown. Further study involving a larger cohort of animals and analysis of follow-up data is necessary to determine the utility of laboratory and imaging studies in clinically normal geriatric patients.
Résumé
Dépistage échographique et laboratoire chez des chiens Golden retriever âgés normaux. Des tests de santé et de dépistage sanguin et urinaire pré-anesthésiques des animaux de compagnie gériatriques sont habituellement recommandés. De plus, il y a des mentions occasionnelles de l’usage de l’imagerie chez des patients gériatriques cliniquement normaux. Cependant, l’utilité du test de santé n’est pas connue et il existe des renseignements limités concernant la valeur des tests pré-anesthésiques. Les tests de santé, incluant la numération globulaire complète, le profil biochimique, l’analyse d’urine et une échographie abdominale, ont été réalisés sur 53 chiens Golden retriever âgés cliniquement normaux. L’analyse de laboratoire a révélé des anomalies chez 54,7 % (29/53) des chiens. Un dépistage échographique abdominal a démontré des anomalies chez 64,2 % (34/53) des chiens. Vu que seulement un faible nombre de chiens disposaient de tests diagnostiques de suivi, la signification de ces anomalies est inconnue. De nouvelles études sont nécessaires pour déterminer l’utilité des études de laboratoire et d’imagerie chez les patients gériatriques cliniquement normaux, incluant une plus grande cohorte d’animaux et l’analyse des données de suivi.
(Traduit par Isabelle Vallières)
Introduction
The use of routine laboratory testing and imaging in clinically normal populations are discussed in both human and veterinary medicine. In human medicine, routine laboratory testing and imaging are used to screen at-risk patients for disease. Examples include serum cholesterol levels for hyper-cholesterolemia and mammography for breast cancer. However, there is debate about the use of routine laboratory analysis and imaging in the asymptomatic human population without specific risk factors (1). In veterinary medicine, screening laboratory tests are available for many diseases in at-risk breeds, such as fasting triglyceride levels in miniature schnauzers to assess for hyperlipidemia, and ALT (alanine aminotransferase) levels in Bedlington terriers to assess for copper storage disease. In addition, the use of routine wellness laboratory screening has resulted in the early diagnosis of occult diseases such as protein-losing nephropathy. However, large-scale prospective studies documenting the benefits of screening tests in the clinically normal canine population are lacking.
The purpose of this study was to determine the value of wellness screening, including complete blood (cell) count (CBC), biochemical profile, urinalysis, and abdominal ultrasound, in a small population of clinically normal mature golden retriever dogs.
Materials and methods
Criteria for patient selection
This study was a prospective, blinded clinical trial. Clinically normal golden retriever dogs aged 6 y and older were evaluated at the Mississauga-Oakville Veterinary Emergency Hospital (MOVEH). These dogs were also used as control dogs in a study investigating a biomarker to predict presence or recurrence of hemangiosarcoma. All dogs resided in southern Ontario and ranged in age from 6 to 13 y (median = 9 y). Gender categories included 47.2% (25/53) spayed female, 18.9% (10/53) intact female, 13.2% (7/53) neutered male, and 20.8% (11/53) intact male dogs. Pre-existing disease did not result in exclusion from the study, provided that the disease was stable. Stable pre-existing disease was defined as disease that was unchanged, including no change in measurable parameters and no change in medication, over a minimum of 6 mo. Stable disease was present in 13.2% (7/53) of the dogs, and included hypothyroidism, hypertension, and otitis externa.
Laboratory data
Prior to entrance into the study, a history for each dog was obtained from the owner to confirm that there were no current health concerns and that any disease present was stable and fit the inclusion criteria. A physical examination, CBC, biochemical profile, and urinalysis were performed on each dog. All laboratory testing was performed at the Animal Health Laboratory, University of Guelph. Prior to entry into the study, the owner’s consent and willingness to comply with all study requirements was obtained. The study was approved by the MOVEH Scientific Board and the Animal Care Committee of the University of Guelph, and the care of animals was conducted according to the principles outlined in the Canadian Council on Animal Care.
Abdominal ultrasonography
A complete abdominal ultrasound examination was performed in each dog by a board-certified small animal internal medicine specialist (J.A.W.), utilizing an ATL HDI 5000 SonoCT (ATL Ultrasound, Bothell, Washington, USA). All patients were scanned in dorsal recumbency, with either an 8–5 MHz curvilinear transducer, or a 14 MHz linear array transducer; the right lateral intercostal window was used as necessary. The dog’s abdomen was shaved and acoustic coupling gel was applied. Thorough ultrasonographic examination of the liver, gall bladder, bile duct, kidneys, adrenal glands, spleen, urinary bladder, reproductive organs when present, pancreas, gastrointestinal tract, and lymph nodes was performed. The right dorsal intercostal window was used for evaluation of the liver and, when necessary, the pylorus and proximal duodenum. Still images were digitally recorded for all organs, including images of any abnormalities. The images were reviewed by a blinded board-certified radiologist (S.G.N.). The medical record, including results from the laboratory work and ultrasound interpretation, was reviewed by a board-certified small animal internal medicine specialist (J.A.W.). Review of the laboratory data was performed while blinded from the radiologist’s interpretation of the ultrasound images, and review of the radiologist’s interpretation of the ultrasound images was performed while blinded from results of the laboratory data.
Statistical analysis
A paired t-test was used to determine statistically significant differences between age and the prevalence of laboratory and imaging abnormalities, including a separate analysis for splenic masses, and a paired t-test was also used to determine statistically significant differences between age and the presence of follow-up data. A Fisher’s exact test was used to determine statistically significant differences between gender/intact status in the prevalence of laboratory and imaging abnormalities, including a separate analysis for splenic masses. A Fisher’s exact test was also used to determine statistically significant differences between gender/intact status and the presence of follow-up data. If there was statistical significance then the odds ratio was determined.
Results
Fifty-three dogs were included in this study. Laboratory analysis, including CBC, biochemical profile, and urinalysis, revealed abnormalities indicative of occult but potentially significant disease in 54.7% (29/53) of dogs (Table 1). These abnormalities included hypoalbuminemia, azotemia with inadequately concentrated urine, pyuria with bacteriuria in urine samples obtained via cystocentesis, increased ALT activity, anemia, leukopenia, thrombocytosis, neutropenia, neutrophilia, low urea with microcytosis and isosthenuria, proteinuria, and both struvite and calcium oxalate crystalluria. Abdominal ultrasound demonstrated abnormalities indicative of occult but potentially significant disease in 64.2% (34/53) of the dogs. Abnormalities included renal aplasia, cystic uterine changes, presumptive pyelonephritis, urolithiasis, cholelithiasis, cystic renal change, adrenomegaly, presumptive pancreatitis, and gastric, hepatic, splenic, testicular, and adrenal masses (Table 2).
Table 1.
Abnormalities found on laboratory analysis
| Laboratory abnormality | Number of dogs | % of total |
|---|---|---|
| Bacteriuria in sample collected by cystocentesis | 6 | 11.3% |
| Increased ALT | 5 | 9.4% |
| Proteinuria | 5 | 9.4% |
| Neutropenia | 4 | 7.5% |
| Increased creatinine with dilute urine | 3 | 5.7% |
| Decreased urea | 3 | 5.7% |
| Anemia | 2 | 3.8% |
| Crystalluria | 2 | 3.8% |
| Hypoalbuminemia | 1 | 1.9% |
| Microcytosis | 1 | 1.9% |
| Thrombocytosis (marked) | 1 | 1.9% |
| Neutrophilia (marked) | 1 | 1.9% |
ALT — alanine aminotransferase.
Table 2.
Abnormalities found on ultrasound examination
| Ultrasound abnormality | Number of dogs | % of total |
|---|---|---|
| Splenic mass(es) | 28 | 52.8% |
| Testicular mass(es) | 7 | 63.6%a |
| Cystic uterus | 2 | 20.0%b |
| Pyelectasia | 5 | 9.4% |
| Hepatic mass(es) | 3 | 5.7% |
| Adrenomegaly | 3 | 5.7% |
| Irregular kidney(s) | 3 | 5.7% |
| Prostatomegaly | 1 | 5.6%c |
| Renal cysts | 2 | 3.8% |
| Cholelith(s) | 1 | 1.9% |
| Focal gastric thickening | 1 | 1.9% |
| Urolith(s) | 1 | 1.9% |
| Adrenal mass(es) | 1 | 1.9% |
| Renal aplasia | 1 | 1.9% |
The calculation of percentage of total was based on the 11 intact male dogs imaged for testicular masses,
10 intact female dogs imaged for cystic uterine change, and
18 male dogs imaged for prostatomegaly.
If a laboratory or ultrasonographic abnormality was noted, then appropriate follow-up diagnostic testing or monitoring was recommended to the primary care veterinarian (Tables 1 and 2). The owners of 44.8% (13/29) of the 29 dogs with laboratory abnormalities declined to pursue recommended follow-up testing or monitoring, due to the costs involved. Four owners among owners of 16 dogs that received follow-up testing only pursued portions of the recommended testing. Monitoring or additional testing of 4 dogs revealed normalization of values. However, some cases indicated on-going disease processes or revealed the need for intervention, such as 4 dogs with a positive urine culture, and 1 dog with azotemia with confirmed early morning low urine specific gravity. This resulted in therapy such as an antibiotic for the 4 dogs with confirmed occult urinary tract infection, and initiation of an appropriate diet, supplementation, and monitoring for the dog with confirmed renal failure.
Owners of 20 (58.9%) of the 34 dogs, which had ultrasonographic abnormalities, declined to pursue recommended follow-up testing or monitoring. Owners were not charged for additional ultrasound examinations and in most cases the reason given for not pursuing recommended follow-up monitoring was the distance involved in returning the dogs to MOVEH for ultrasonographic evaluation. Cost and invasiveness were given as reasons for declining additional testing beyond repeat ultrasound examinations. All dogs that had follow-up monitoring had splenic masses; of these dogs, 50% (10/20) also had abnormalities in other organs. As cases were recruited to be control dogs for a study investigating the presence of a biomarker for splenic hemangiosarcoma, owners were more educated as to the possible implication of a splenic mass in an older golden retriever, and therefore more likely to return for ultrasound examination.
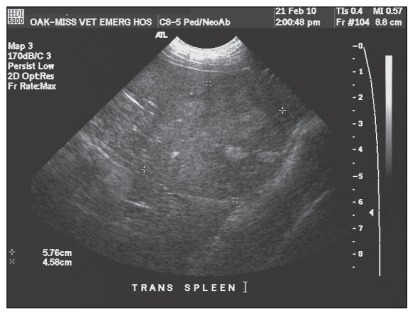
Ultrasound examination revealed occult splenic masses in 52.8% (28/53) of dogs examined (Figure 1). None of the splenic masses contained areas of cavitation, a feature which is often noted in splenic hemangiosarcoma. Of the 28 dogs with splenic masses, 10 dogs had a solitary mass and 18 dogs had multiple splenic masses. Three dogs had splenic masses greater than 3 cm, and 1 dog had a splenic mass that more than doubled in size in a 4-week period. All 4 dogs, therefore, fit the MOVEH criteria for splenectomy. There are no defined parameters in the published veterinary literature; however, 1 source did report similar parameters (2). Fine-needle aspiration was not performed prior to splenectomy due to the lack of consistent correlation of this procedure with histopathology (3). In all 4 dogs for which splenectomy was recommended, the mass was of mixed echogenicity (Figure 1). Although there was a lack of cavitation, this does not rule out hemangiosarcoma. Three of these dogs had splenectomy performed, including the 2 dogs with a splenic mass > 3 cm in diameter, and 1 dog with a splenic mass that more than doubled in diameter in a 4-week period. Thoracic radiographs performed in all 3 dogs prior to splenectomy did not reveal any evidence of metastatic disease. Histopathology of the splenic masses was consistent with benign lymphoid hyperplasia in all 3 dogs. In the dog for which splenectomy was declined, the splenic mass was followed by abdominal ultrasound examination at months 1, 2, 3, and 6, and both the diameter and echotexture remained unchanged.
Figure 1.
Ultrasound imaging of a splenic mass > 3 cm in diameter noted in a clinically normal, mature, golden retriever dog. Histopathology revealed benign lymphoid hyperplasia.
Initial ultrasound examination revealed splenic masses that were < 3 cm in diameter in 47.2% (25/53) of dogs. Sixteen dogs had follow-up splenic ultrasound examinations at months 1, 2, 3, and 6. One dog had a mass that more than doubled in diameter in a 4-week period, as described. In the remainder of the cases, none of the masses increased by more than 15% over the 6-month period, nor did they develop areas of cavitation. None of the masses reached 3 cm in diameter; therefore, splenectomy was not recommended for any of these dogs. Given the lack of progression over a 6-month period, hemangiosarcoma was unlikely but not ruled out.
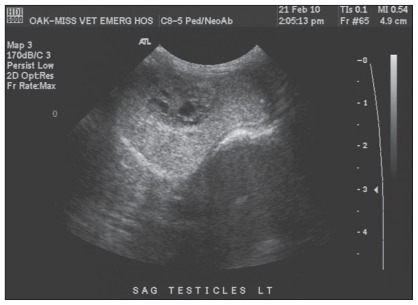
Seven dogs had testicular masses, 2 of which had histopathology of the testicular masses, 1 performed via castration and 1 at postmortem examination. The castrated dog had both Leydig and Sertoli cell tumors present (Figure 2), and castration was considered curative. However, the other dog had metastatic scirrhous carcinoma detected in the testicles; the primary mass was not found on postmortem examination. The splenic mass represented benign lymphoid hyperplasia. Two dogs with pyelectasia were monitored and the changes were stable over 6 mo. One dog with a cholelith had follow-up ultrasound performed which revealed that the cholelith was unchanged in size and location, and 1 dog with hepatic masses had masses that were stable in number, size, and echotexture. One dog had an irregular prostate that was stable on ultrasound examination; no abnormalities were detected in endoscopic prostatic urethral biopsies and prostatic wash cytology. One dog had gastric fundic thickening that was diagnosed as lymphocytic gastritis endoscopically.
Figure 2.
Ultrasound imaging of a testicular mass detected in a clinically normal, mature, golden retriever dog. Histopathology revealed that both Leydig and Sertoli cell tumors were present.
There were no statistically significant differences between age or intact status and the presence of laboratory abnormalities, ultrasonographic abnormalities, presence of splenic mass(es), or the presence of follow-up data. Male dogs were statistically more likely to have follow-up ultrasounds performed (P = 0.008); however, this was based on a population of only 7 male dogs.
Discussion
The objective of this study was to investigate the utility of wellness laboratory and imaging modalities in clinically normal mature golden retriever dogs. A proportion of the dogs had occult but potentially significant disease identified on laboratory and ultrasonographic screening (Tables 1 and 2). There is little information in the veterinary literature on the benefit of preanesthetic or wellness laboratory screening of companion animals. Two recent studies fail to agree on the utility of preanesthetic screening of veterinary patients (4,5). One study concluded that routine hematologic and biochemical screening of dogs was of little clinical relevance and did not tend to alter the anesthetic plan (5). A second study that evaluated dogs that were 7 y or older stated that the value of screening was questionable and needed further evaluation; however, 13% of dogs did not undergo anesthesia as a result of preanesthetic hematologic or biochemical testing (4).
An ideal screening test has a high sensitivity and specificity to minimize the rate of false results. However, as the sensitivity of a test increases the specificity will decrease, resulting in a higher number of false positive results. Additional, unnecessary testing is then indicated. It is, therefore, important to consider the invasiveness and risk of additional testing that would be indicated with a positive result when assessing the utility of a screening test. The number of false positives will also increase as the disease prevalence decreases. Reviews of the benefit of preanesthetic laboratory analysis in humans have generally shown that abnormal results are observed in only a very small proportion of the tested population, typically < 3% (1,6,7). The conclusion of 1 review was that the evidence did not support a policy of routine preanesthetic laboratory testing; however, there was no evidence that a policy of performing preanesthetic laboratory testing would be harmful (6). In human medicine, the financial implications and cost:risk benefit analysis are a large factor in determining the use of screening testing, as is the legal implication of missed diagnoses (1,8). More recent reviews have stressed the importance of a thorough history and physical examination, with targeted preanesthetic laboratory testing (1,8).
Given the inability to detect certain processes, such as protein-losing nephropathy and chronic hepatic disease, until late in the course of disease, there is an arguable benefit to performing routine wellness testing in the older pet population. In the majority of cases, clients are given the option of pursuing preanesthetic and wellness laboratory testing in apparently clinically normal companion animals. However, veterinarians must counsel owners as to the value of this type of testing, and currently there are insufficient data available to aid in this counselling. Veterinarians are also subject to the legal implications that are present in human medicine, and there are no large, prospective studies available to assess the need for wellness or preanesthetic screening by the veterinarian. Indeed, if larger studies were performed, they may also aid in recommending the appropriate age and frequency for performing this testing, which likely will vary with breed.
The present study, although involving only a small group of dogs of a single breed, supports the implementation of routine laboratory wellness testing in older companion animals. However, given the small number of dogs in this study, final recommendations on the use of routine laboratory testing require an evaluation of a larger group of dogs. Over half of the dogs included in this study had laboratory changes that indicated potentially significant disease, and warranted either monitoring or further diagnostic evaluation. Follow-up testing revealed that abnormalities had resolved in some cases, but needed to be addressed in others. In one of the dogs diagnosed with a urinary tract infection, ultrasound examination suggested chronic pyelonephritis, prompting a recommendation for a longer course of antibiotic therapy. Unfortunately, 44.8% (13/29) of owners declined to pursue recommended follow-up testing due to the cost involved. Larger prospective studies are required to determine the benefit of routine wellness and preanesthetic laboratory testing, and the optimum age and frequency of such testing. Ideally, these studies would include follow-up testing and/or monitoring when abnormalities are found.
The routine use of ultrasonography as a screening test for older animals has been suggested only occasionally, and to our knowledge there are no prospective studies evaluating the use of ultrasonography in clinically normal geriatric patients (9,10). One concern about using imaging to screen for occult disease in an apparently healthy population is the large number of incidental abnormalities that may be encountered (1). Moreover, there may be inherent risk associated with additional testing to determine whether an incidentally discovered abnormality is significant and requires intervention. Testing may also place a financial burden on the pet owner for procedures that may not be required. These concerns have been noted in human medicine, in which whole body computed tomography (CT) scanning and magnetic resonance imaging (MRI) have recently been offered directly to the public by the commercial sector (1,11–13). In addition, there is a psychological effect in asymptomatic people with a normal CT or MRI scan; there is a feeling that their results guarantee the absence of disease (13). Extending this scenario to the pet population, an owner might conceivably delay presentation of a pet with clinical signs if an ultrasound examination had previously shown no abnormalities.
In this study, the discovery of splenic masses resulted in the recommendation to perform splenectomy in a small number of cases, arguably an invasive and expensive procedure. However, as larger benign splenic masses can result in rupture with subsequent hemoabdomen and cardiovascular instability, their removal is indicated, even if the mass is benign. Therefore, their discovery prior to rupture would result in a more cardiovascularly stable patient for general anesthesia and splenectomy. Testicular masses in dogs typically are benign and therefore detecting them ultrasonographically would not result in recommended removal or monitoring; however, in 1 case in this study the masses were evidence of metastatic scirrhous carcinoma. One dog had gastric fundic thickening that was diagnosed as lymphocytic gastritis on endoscopic biopsies, which lead to recommendations on additional testing of biopsy samples and therapy.
There appears to be widespread agreement in human medicine to discourage the use of whole body CT and/or MRI scanning in asymptomatic people (1,13). The use of whole body CT and/or MRI scanning in asymptomatic companion animals has not been investigated or recommended, likely in part due to the cost involved along with the lack of studies assessing the benefit. However, ultrasonographic screening of asymptomatic companion animals is more financially feasible, and this may become a procedure requested by some pet owners. In the asymptomatic companion animal, however, there is a requirement for large, prospective studies to evaluate the implementation of any imaging modality before there can be an assessment of benefits or risks regarding its use.
In conclusion, our study indicated that a number of clinically normal mature golden retriever dogs have occult but potentially significant disease based on laboratory and/or ultrasonographic screening. However, due to the small study size, definitive recommendations on timing and type of laboratory wellness screening could not be achieved. The utility of abdominal ultrasound as a screening tool in clinically normal mature golden retriever dogs remains unclear due to the small study size and lack of follow-up testing and/or monitoring in some cases. Large, prospective studies are required to determine the clinical relevance of abnormal results from laboratory analyses and abdominal ultrasound findings in asymptomatic patients. CVJ
Footnotes
This work was supported by a grant from the Pet Trust Fund, Ontario Veterinary College. Preliminary data from this study were presented at the European College of Veterinary Internal Medicine Companion Animal Congress, Toulouse, France, 2010.
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Mayer D. Essential Evidence-Based Medicine. Cambridge, UK: Cambridge University Press; 2010. pp. 310–319. [Google Scholar]
- 2.Page RL. Management considerations for incidental adrenal, splenic and pulmonary nodules. Proc Atlantic Coast Veterinary Conference; Atlantic City, New Jersey. 2001. [Google Scholar]
- 3.Watson AT, Penninck D, Knoll JS, Keating JH, Sutherland-Smith J. Safety and correlation of test results of combined ultrasound-guided fine-needle aspiration and needle core biopsy of the canine spleen. Vet Radiol Ultrasound. 2011;52:317–22. doi: 10.1111/j.1740-8261.2010.01778.x. [DOI] [PubMed] [Google Scholar]
- 4.Joubert KE. Pre-anaesthetic screening of geriatric dogs. J S Afr Vet Assoc. 2007;78:31–35. doi: 10.4102/jsava.v78i1.283. [DOI] [PubMed] [Google Scholar]
- 5.Alef M, von Praun F, Oechtering G. Is routine pre-anaesthetic haematological and biochemical screening justified in dogs? Vet Anaesth Analg. 2008;35:132–140. doi: 10.1111/j.1467-2995.2007.00364.x. [DOI] [PubMed] [Google Scholar]
- 6.Munro J, Booth A, Nicholl J. Routine preoperative testing: A systematic review of the evidence. Health Technol Assess. 1997;1:i–iv. 1–62. [PubMed] [Google Scholar]
- 7.Takemura Y, Ishida H, Inoue Y, et al. Opportunistic discovery of occult disease by use of test panels in new, symptomatic primary care outpatients: Yield and cost of case finding. Clin Chem. 2000;46:1091–1098. [PubMed] [Google Scholar]
- 8.Katz RI, Dexter F, Rosenfeld K, et al. Survey study of anesthesiologists’ and surgeons’ ordering of unnecessary preoperative laboratory tests. Anesth Analg. 2011;112:207–212. doi: 10.1213/ANE.0b013e31820034f0. [DOI] [PubMed] [Google Scholar]
- 9.Villalobos A, Kaplan L. Canine and Feline Geriatric Oncology: Honoring the Human-Animal Bond. Hoboken, New Jersey: Blackwell Publishing; 2007. p. 257. [Google Scholar]
- 10.Page RL. Changing attitudes about cancer: Prevention, screening, and early diagnosis. Proc Atlantic Coast Veterinary Conference; Atlantic City, New Jersey. 2001. [Google Scholar]
- 11.Hillman BJ. CT screening: Who benefits and who pays. Radiology. 2003;228:26–28. doi: 10.1148/radiol.2281021733. [DOI] [PubMed] [Google Scholar]
- 12.Furtado CD, Aguirre DA, Sirlin CB, et al. Whole-body CT screening: Spectrum of findings and recommendations in 1192 patients. Radiology. 2005;237:385–394. doi: 10.1148/radiol.2372041741. [DOI] [PubMed] [Google Scholar]
- 13.Elliott A. Committee on medical aspects of radiation in the environment 12th report. London, England: Health Protection Agency; 2007. [Google Scholar]