Abstract
Objective:
To assess the effect of a comprehensive yogic breathing program on glycemic control and quality of life (QOL) in patients with diabetes.
Materials and Methods:
This is a prospective randomized controlled intervention trial. Patients having HbA1c between 6 and 9% for at least 3 months with lifestyle modification and oral antidiabetic medication were included. They were followed-up and randomized at 6 months into two groups: one group receiving standard treatment of diabetes and the other group receiving standard treatment of diabetes and taught and told to regularly practice the comprehensive yogic breathing program (Sudarshan Kriya Yoga and Pranayam). Change in fasting and post-prandial blood sugars, glycated hemoglobin and QOL as assessed by the World Health Organization QOL WHOQOL BREF questionnaire were assessed.
Results:
There was a trend toward improvement in glycemic control in the group practicing the comprehensive yogic breathing program compared with the group following standard treatment alone, although this was not significant. There was significant improvement in physical, psychological and social domains and total QOL post-intervention in the group practicing the comprehensive yogic breathing program as compared with the group following standard treatment alone.
Conclusion:
There was significant improvement in the QOL and a non-significant trend toward improvement in glycemic control in the group practicing the comprehensive yogic breathing program compared with the group that was following standard treatment alone.
Keywords: Comprehensive yogic breathing program, diabetes mellitus, quality of life
INTRODUCTION
A few studies suggest that yoga can improve glycemic control.[1] There are several hypotheses for the biological mechanisms that link the benefits of yoga to diabetes management. One hypothesis points to the role of stress and relaxation.[2] Sudarshan Kriya Yoga[3] has been found to be useful in stress and anxiety.[4,5] Stress and anxiety effect behavior. Diabetes treatment requires changes in behavior and lifestyle.[6]
With this background, we performed a randomized controlled trial to asses the effect of Sudarshan Kriya Yoga on quality of life (QOL) and glycemic control in patients with diabetes who were and continued to be on oral diabetic medications.
MATERIALS AND METHODS
Patients with type 2 diabetes on treatment with lifestyle modification, i.e. exercise and diet control (according to ADA recommendations) plus oral hypoglycemic agents having HbA1c between 6 and 9%, were included in the study.
Patients with uncontrolled hypertension, glaucoma, schizophrenia, bipolar disorder, pregnancy, patients who did not consent for follow-up, type 1 diabetes, congestive cardiac failure, proliferative diabetic retinopathy or nephropathy with serum creatinine >1.5 mg/dL were excluded from the study.
This study was approved by an Ethics Committee. All patients found to satisfy the inclusion criteria were told about the study. The patients were administered informed consent and those who gave consent were included. Comprehensive diabetic education was imparted to all subjects and they were treated on an outpatient department basis. Patients were on a stable dose of antidiabetic medicines for the initial 6 months, in which they were maintaining an HbA1c level between 6 and 9%. At 6 months, they were randomized into two groups: group non-SKY and group SKY. Randomization was performed by computer-generated numbers using the n Query advisor program. The SKY group patients underwent a comprehensive yogic breathing program for 3 days. This course included yogic movements and postures (asanas), relaxation practices, meditation, group processes and discussion of stress-relieving principles. Patients underwent 1 h of long group breathing technique, which included three stages of Pranayam, three rounds of 20 each of Bhastrika, three times Om chanting and Sudarshan Kriya (long kriya) followed by rest in supine position on the first and second day. On the third day, they were taught the short breathing technique, which included three stages of Pranayam, three rounds of 20 each of Bhastrika, three times Om chanting and Sudarshan Kriya (short kriya) followed by rest in supine position.[2] This process took a total of 25–35 min and was learnt under the guidance of a certified teacher.
Patients in the non-SKY group continued the standard treatment of diabetes while patients in the SKY group continued the standard treatment and practice of short kriya daily at home. To ensure home practice, they were asked to fill a follow-up book in which they marked the days on which they did SKY and got it countersigned by a relative or attendant. They were required to come weekly for group Sudarshan Kriya Yoga and Pranayam (long kriya) to a center in the hospital and get the follow-up book signed by the yoga teacher each time they attended.
Compliance was defined as number of short kriya ≥30 (33% of short kriyas) and number of long kriya ≥3 (25% of long kriyas) or number of long kriya ≥6 (50% of long kriyas). To ensure compliance, telephonic reminders were given to the patients the day after the course was completed for daily practice of short kriya and weekly to come for the group practice of long kriya.
At the time of enrollment, the following tests were carried out: fasting plasma glucose (FBG), plasma glucose postprandial (PPBS), HbA1c, electrocardiogram, ocular tension measurement, blood urea and serum creatinine.
After 3 months, assessment of plasma glucose-fasting and -postprandial, HbA1c and QOL by WHOQOL BREF questionnaire were performed.
HbA1c was measured by the BIO-RAD D-10 Hemoglobin A1c Program.
Statistical methods
Statistical analysis was performed using the Wilcoxon rank-sum (Mann–Whitney) test using STATA/IC 11.1 software.
RESULTS
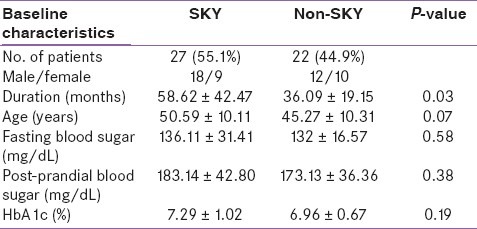
A total of 210 patients were screened. One hundred and four refused to participate. Fifty-four were screen failures. There were three dropouts. The remaining 49 patients were randomized into two groups. There were 27 patients (55.1%) in the SKY group and 22 patients (44.9%) in the non-SKY group. Their baseline characteristics are given in Table 1. Among the 27 patients in the SKY group, only 16 patients were compliant according to the criteria defined.
Table 1.
Baseline characteristics of patients
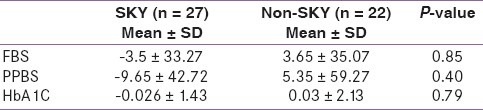
There was a decrease of mean FBS by 3.5 ± 33.27 mg/dL in the SKY group, whereas it increased by 3.65 ± 35.07 mg/dL in the non-SKY group (P = 0.85). The mean post-prandial blood sugar (PPBS) decreased by 9.65 ± 42.72 mg/dL in the SKY group while it increased by 5.35 ± 59.27 mg/dL in the non-SKY group (P = 0.40). There was a decrease of 0.026 ± 1.43% in the mean glycated hemoglobin (HbA1c) in the SKY group whereas in the non-SKY group, there was an increase of 0.03 ± 2.13% (P = 0.79) [Table 2]. This trend of improvement in glycemic control is not statistically significant.
Table 2.
Changes at 9 months compared with 6 months
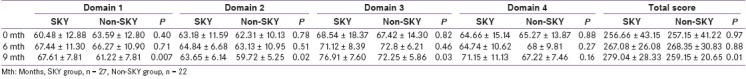
WHOQOL-BREF assesses the QOL in four domains. Domain 1 assesses physical health, domain 2 assesses psychological well being, domain 3 pertains to social relationships and domain 4 pertains to environment.
Post intervention, there was improvement in QOL in the SKY group in domain 1 (P = 0.007), domain 2 (P = 0.02), domain 3 (P = 0.03) and domain 4 (P = 0.16) and in the total mean score (P = 0.01). QOL mean scores at various times are shown in Table 3. This table shows the pattern of improvement in QOL when comparing all subjects (SKY = 27, non-SKY = 22). When we compared the compliant patients in the SKY group with the non-SKY group, the pattern of improvement in QOL was similar to the pattern in Table 3.
Table 3.
WHO BREF QOL mean scores at baseline and follow-up
DISCUSSION
Our study was a randomized controlled trial. There were 27 patients in the SKY group and 22 patients in the non-SKY group. They were similar in baseline characters except for the duration of diabetes. In the SKY group, the mean duration of diabetes was 58.62 ± 42.47 months and in the non-SKY group, it was 36.09 ± 19.15 months (P = 0.03).
There was a decrease in mean FBS by 3.5 ± 33.27 mg/dL in the SKY group, whereas it increased by 3.65 ± 35.07 mg/dL in the non-SKY group (P = 0.85). Mean PPBS decreased by 9.65 ± 42.72 mg/dL in the SKY group while it increased by 5.35 ± 59.27 mg/dL in the non-SKY group (P = 0.40). There was a decrease of 0.026 ± 1.43% in mean HbA1c in the SKY group, whereas in the non-SKY group, there was an increase of 0.03 ± 2.13% (P = 0.79) [Table 2]. Although there was a trend toward improvement in glycemic control in patients practicing SKY and taking standard treatment compared with those taking standard treatment alone, this improvement was not statistically significant.
Yoga is practiced worldwide for its health benefits, including physical fitness, relaxation and awareness of self. It is based on the principle that the mind and body are intimately related. Stress produces a state of physical and mental tension. In yoga, physical postures and breathing exercises improve muscle strength, flexibility, blood circulation and oxygen uptake. While many researchers conceptualize yoga as a form of physical activity, others argue that comprehensive yoga, an approach incorporating body postures (asanas), breathing techniques (pranayamas), meditation, cleansing, nutrition, attitudinal and behavioral modification and mental discipline, is more beneficial and loyal to its ancient tenets.[7]
Previous studies suggested that SKY may be useful for relieving depression,[8,9] improving the antioxidant[10] and immune[11] defenses of the body. In an open preliminary study, there was a significant decrease in fasting blood sugar, cholesterol and triglycerides after the practice of SKY for 4 months.[12] Although this study suggested a promising potential of SKY as complementary therapy in diabetes, it was limited by its sample size and design. Systematic scientific experiments are necessary to establish the efficacy of SKY as a complementary therapy in chronic diseases like diabetes.
There is growing evidence concerning the potent effect of psychosocial factors on physical health outcomes. People with diabetes often feel challenged by their disease and its day to day management demands. This itself can lead to stress. The psychosocial toll of living with diabetes can often affect self-care behavior, long-term glycemic control, QOL and risk of developing long-term complications. There is now good evidence that psychosocial issues are critical to good diabetes care. Psychosocial factors often determine self-management behaviors, and psychosocial variables (such as depression) are often strong predictors of measures such as the presence of complications, body mass index (BMI) and glycated hemoglobin (HbA1c).[13]
Yoga has been studied for its role in the management of several chronic diseases, including obesity, hypertension,[14] asthma,[15] neuromuscular diseases[16] and psychiatric illnesses.[5] Yoga has been studied for controlling both the symptoms and the complications associated with diabetes mellitus type 2.[12]
Yoga can be easily learned and performed. Once learned, yoga can be practiced at any time on an individual basis thus reducing common barriers to physical activity such as time conflicts and poor weather. It is not as simple as swallowing a drug. It needs acceptance, motivation, a will for improvement, time, silent space for practice and active participation on the part of the patient and the patient's family. Also, it does not show immediate effect and, for attitudinal change and health benefits, it needs to be practiced regularly.
A controlled pilot study in healthy volunteers[17] showed that subjects who practice SKY felt that they had gained a tool that can be used in stressful situations that would make it easier to relax and better handle them.
Five studies were included in a review[18] with 10 arms, comparing the intervention of yoga practice alone or combined with other modes of interventions. Five arms (200 participants with the control group in which two arms and 40 participants) received nothing apart from the conventional medical therapy,[16,19] one arm and 72 participants received recommendation on unsupervised training at home,[20] one arm and 30 participants received herbal, diet and exercise[21] and the last arm with 20 participants reviewed recommendation for diet and walking exercise.[22] A total of 362 participants (200 intervention group and 164 in the control group) were analyzed. The mean trial duration was 14 weeks (range from 6 to 24 weeks). These studies were conducted in India and in the USA. Yoga practice alone was used in three studies,[16,19,22] while it was combined with lifestyle modification only in one study.[20] Yoga was accompanied with lifestyle modification, diet and herbal intake in one study.[21] All of the participants received training for yoga practice. The range of frequency of each session of yoga practice was different: e.g. two 20-min sessions per day for one of the trials[21] and three to five 90-min sessions in another.[19] Four studies provided results on FPG. These four studies provided favorable results for the intervention in lowering FPG. The mean differences ranged from 28.8 to 41.1 in lowering the plasma glucose between the intervention and control groups, and they were all significant in three studies;[15,22,23] however, the difference in the Elder study was 3.6, and it was not significant.[24] Three of the included studies reported the value of HbA1c.[19–21] The mean differences indicated that the intervention lowered the level of the HbA1c. However, the results were only statistically significant in one study.[19]
The main objective of treating all chronic diseases like diabetes mellitus is to improve well being and attain a satisfactory QOL. Pooled analysis of population-based surveys in Germany (n = 9579) has shown that type 2 diabetes has negative consequences for health-related QOL.[22] In another study, the mean total score of QOL in physical dimension, mental–emotional and feelings of well being dimensions and behavioral activity dimension were significantly higher in the healthy population than in the diabetes mellitus group.[23] Other studies have also shown that type 2 diabetes adversely affects the QOL[24] and good QOL is significantly related to good compliance.[25]
In our study, there was improvement in all four domains and total mean score of QOL post intervention in the group practicing SKY compared with the group getting standard treatment of diabetes alone [Table 3]. The improvements in domains 1, 2, 3 and total mean score of QOL were significant.
In the previous study of SKY in reducing anxiety, practice of SKY for 2 months was accompanied by a significant reduction in anxiety score (P = 0.039) and stress score (P = 0.017) and by marginal improvement in patience score (P = 0.134).[26] A sense of well being was reported by 67% of the subjects, improved sleep quality was reported by 50% and 33% experienced increased enthusiasm for doing their work.
In another pilot study[17] in healthy volunteers, those practicing a comprehensive yogic breathing program experienced increased wellness, reduced stress, feeling of balance and living in present moment and a new outlook in life compared with a group that was instructed to relax in an arm chair each day during the same period.
Our study is the first randomized controlled trial to determine the effect of SKY on glycemic control and QOL. The major challenge in our study was the compliance in practicing SKY. That is why we selected patients from nearby only. We ensured compliance by providing them a logbook. They had to get the logbook signed daily by a relative after finishing a short yogic breathing exercise at home. Their logbook was reviewed weekly at the yoga center when they came for the weekly group breathing program and signed by the yoga instructor.
Compliance was defined as number of short kriya ≥30 (33% of short kriyas) + number of long kriya ≥3 (25% of long kriyas) or number of long kriya ≥6 (50% of long kriyas).
Reasons for non-compliance were failure to complete the 3-day comprehensive yogic breathing program (engagements at home, sudden illness or demise of relative), lack of motivation, illness, travel, lack of time due to long working hours or household work, all of which led to inability to pursue the home practice and weekly group processes.
Because there was evidence for weekly follow-up and performance of long kriya as the log books had to be signed by the yoga instructor, the number of long kriya was given more weightage. At 3 months (90 days), 33% amounted to 30 short kriyas. As the short kriyas were self-reported, the criteria of 25% of total long kriyas was added (3 months amounts to 12 weekly follow-ups, 25% of which is three long kriyas).
However, this study has limitations. Firstly, patients in the SKY group on an average had longer duration of diabetes compared with those in the non-SKY group. This is a potential contributing factor to the final results. Secondly, the compliance of daily practice was self-reported by patients. Thirdly, because there are no parameters by which we can define compliance, the definition of compliance used in this study was arbitrary. Fourthly, the sample size is limited. Fifthly, the small sample size of compliant versus non-compliant limits a valid statistical comparison between the two groups. Lastly, the study could not be not blinded.
CONCLUSION
This study was a randomized controlled intervention trial to assess the effect of Sudarshan Kriya Yoga and Pranayam on glycemic control and QOL in patients with diabetes in addition to the standard treatment of diabetes.
There was a trend toward improvement in glycemic control, which was only marginal and not statistically significant. At 3 months, there was a significant improvement in QOL in the group practicing Sudarshan Kriya Yoga in addition to standard treatment of diabetes compared with the group that was following standard treatment alone.
Because SKY has been found to improve QOL in a chronic disease like diabetes, it might also help in the long term to adhere to lifestyle measures, which will ultimately help in better diabetes control.
This study is ongoing and is still recruiting patients. To assess the long-term beneficial effect of the comprehensive yogic breathing program on QOL and glycemic control, compliance needs to be ensured and a larger sample size needs to be studied.
ACKNOWLEDGEMENT
This project is funded by the Indian council of Medical Research, New Delhi.
Footnotes
Source of Support: Project is funded by the Indian council of Medical Research, New Delhi.
Conflict of Interest: None declared.
REFERENCES
- 1.Sahay BK. Role of yoga in diabetes. J Assoc Physicians India. 2007;55:121–6. [PubMed] [Google Scholar]
- 2.Surwit RS, Schneider MS. Role of stress in the etiology and treatment of diabetes mellitus. Psychosom Med. 1993;55:380–93. doi: 10.1097/00006842-199307000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety and depression: Part I- Neurophysiological model. J Altern Complement Med. 2005;11:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 4.Miller JJ, Fletcher K, Kabat-Zinn J. Three year follow up and clinical implications of a mindfulness-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- 5.Gupta N, Khera S, Vempati RP, Sharma R, Bijlani RL. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50:41–7. [PubMed] [Google Scholar]
- 6.Dunning T. Complementary therapies and diabetes. Complement Ther Nurs Midwifery. 2003;9:74–80. doi: 10.1016/S1353-6117(02)00143-9. [DOI] [PubMed] [Google Scholar]
- 7.Manyam BV. Diabetes mellitus, Ayurveda, and yoga. J Altern Complement Med. 2004;10:223–5. doi: 10.1089/107555304323062185. [DOI] [PubMed] [Google Scholar]
- 8.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy(ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 9.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ. Therapeutic efficacy of Sudarshan Kriya Yoga (SKY) in dysthymic disorder. NIMHANS J. 1998;17:21–8. [Google Scholar]
- 10.Sharma H, Sen S, Singh A, Bhardwaj NK, Kochupillai V, Singh N. Sudarshan Kriya practitioners exhibit better antioxidant status and lower blood lactate levels. Biol Psychol. 2003;63:281–91. doi: 10.1016/s0301-0511(03)00071-1. [DOI] [PubMed] [Google Scholar]
- 11.Kochupillai V, Kumar P, Singh D, Aggarwal D, Bhardwaj N, Bhutani M, et al. Effect of rhythmic breathing (Sudarshan Kriya and Pranayam) on immune functions and tobacco addiction. Ann N Y Acad Sci. 2005;1056:242–52. doi: 10.1196/annals.1352.039. [DOI] [PubMed] [Google Scholar]
- 12.Agte VV, Tarwadi K. Sudarshan Kriya yoga for treating type 2 diabetes: A preliminary study. Altern Complement Ther. 2004;10:220–2. [Google Scholar]
- 13.Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults: A three-year prospective study. Diabetes Care. 1998;21:231–5. doi: 10.2337/diacare.21.2.231. [DOI] [PubMed] [Google Scholar]
- 14.Guanacino JL, Savino S, Edelstein S. Yoga participation is beneficial to obesity prevention, hypertension control, and positive quality of life. Top Clin Nutr. 2006;21:108–13. [Google Scholar]
- 15.Sabina AB, Williams AL, Wall HK, Bansal S, Chupp G, Katz DL. Yoga intervention for adults with mild-to-moderate asthma: A pilot study. Ann Allergy Asthma Immunol. 2005;94:543–8. doi: 10.1016/s1081-1206(10)61131-3. [DOI] [PubMed] [Google Scholar]
- 16.Ramaratnam S, Sridharan K. The Cochrane Library. Oxford: update software; 2000. Yoga for epilepsy. Issue 1. [Google Scholar]
- 17.Kjellgren A, Bood SA, Axelsson K, Norlander T, Saatcioglu F. Well ness through a comprehensive yogic breathing program – A controlled pilot study. BMC Complement Altern Med. 2007;7:43. doi: 10.1186/1472-6882-7-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aljasir B, Bryson M, Al-Shehri B. Yoga Practice for the management of type II diabetes mellitus in adults: A systematic review. Evid Based Complement Alternat Med. 2010;7:399–408. doi: 10.1093/ecam/nen027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monro R, Power J, Coumar A, Nagarathna R, Dan Dona P. Yoga therapy for NIDDM: a controlled trial. Complement Med Res. 1992;6:66–8. [Google Scholar]
- 20.Agarwal RP, Aradhana , Hussain S, Beniwal R, Sabir M, Kochar DC, Kothari RP. Influence of yogic treatment on quality of life outcomes, glycemic control and risk factors in diabetes mellitus. Int J Diabetes Dev Ctries. 2003;23:130–4. [Google Scholar]
- 21.Elder C, Aickin M, Bauer V, Cairns J, Vuckovic N. Randomized trial of a whole-system ayurvedic protocol for type 2 diabetes. Altern Ther Health Med. 2006;12:24–30. [PubMed] [Google Scholar]
- 22.Malhotra V, Singh S, Tandon OP, Madhu SV, Prasad A, Sharma SB. Effect of Yoga asanas on nerve conduction in type 2 diabetes. Indian J Physiol Pharmacol. 2002;46:298–306. [PubMed] [Google Scholar]
- 23.Schunk M, Reltmeir P, Schipf S, Volzke H, Melsenger C, Thorand B, et al. Health related quality of life in subjects with or without type 2 diabetes: Pooled analysis of five population based surveys in Germany. Diabet Med. 2012;29:646–53. doi: 10.1111/j.1464-5491.2011.03465.x. [DOI] [PubMed] [Google Scholar]
- 24.Hashemi Hefz Abad F, Shabany Hamedan M. Comparison of attitudes regarding quality of life between insulin treated subjects with diabetes mellitus and healthy populations. Diabetes Metab J. 2011;35:397–403. doi: 10.4093/dmj.2011.35.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Urzua MA, Chirino A, Valladares G. Health related QOL among patients with type 2 diabetes mellitus. Rev Med Chil. 2011;139:313–20. [PubMed] [Google Scholar]
- 26.Chaveepojnkamjorn W, Pichainarang N, Schelp FP, Mahaweerawat U. Quality of life and compliance among type 2 diabetic patients. Southeast Asian J Trop Med Public Health. 2008;39:328–34. [PubMed] [Google Scholar]


