Abstract
There are very few cases in the literature in which refractory persistent hypothyroidism responded only to parenteral doses of levothyroxine and no evidence of any malabsorptive disorder could be identified. Here, we present a rare case of a 35-year-old woman with refractory hypothyroidism who responded only to intravenous doses of levothyroxine. We also discuss possible causes for the same.
Keywords: Refractory hypothyroidism, selective malabsorption, thyroxine
INTRODUCTION
Oral levothyroxine sodium (LT4) remains the mainstay of treatment of hypothyroidism to achieve physiological thyroid hormone levels. The mean treatment dosage is 1.6 μg/kg bodyweight per day.[1] Intestinal absorption ranges from 70% to 80% of the administered dose and it differs from patient to patient.[2] In addition, absorption is higher in the fasting state. However, hypothyroidism persists and euthyroid state cannot be achieved in a few cases even after supplementing adequate or excessive doses of oral thyroxine. In such cases of refractory hypothyroidism, the main differentials to be considered are (a) poor patient compliance to oral thyroxine, (b) deiodinase deficiency, and (c) various malabsorption disorders. Of these poor compliance is very commonly seen in refractory hypothyroidism.[3–5] There are very few cases in the literature in which refractory persistent hypothyroidism responded only to parenteral doses of levothyroxine and no evidence of any malabsorptive disorder could be identified.
Here, we present a rare case of a 35-year-old woman with refractory hypothyroidism who responded only to intravenous doses of levothyroxine. We also discuss possible causes for the same.
CASE REPORT
A 35-year-old female presented to the physician with complaints of gradual increase in weight, loss of appetite, lethargy, and weakness over the past 4 years. On examination, she had dry scaly skin, peripheral edema, and a blood pressure of 140/100 mm Hg. She was incidentally diagnosed to be hypothyroid during her third pregnancy and treatment started on 100 μg thyroxine 4 years ago. The delivery was uneventful and the baby also had normal thyroid profile. Her symptoms gradually worsened and her thyroid-stimulating hormone (TSH) levels reached 651.4 μIU/ml 1 year ago. The dose of thyroxine was gradually increased upto 400 μg/day. Patient was compliant to the intake of thyroxine. Repeated thyroid profiles on thyroxine doses between 100 and 400 μg showed TSH ranging from 270 to 360 μIU/ml. Her free T3 and free T4 were also very low. Oral intake under physician supervision did not help. Her serum cholesterol was elevated upto 338 mg/dl. The patient was additionally administered 25 μg of tri-iodothyronine twice daily. Even after such a high dose of T4 and addition of oral T3, her serum T3, T4, and TSH did not normalize. She was thoroughly investigated for refractory primary hypothyroidism. Her antithyroglobulin antibody level was 261 IU/ml and anti-TPO antibody was 974 IU/ml. Family history of hypothyroidism was present. 99mTc pertechnetate thyroid scan showed normally located thyroid gland with normal homogenous tracer uptake in both the lobes of thyroid gland.
As a next step, malabsorption of oral thyroxine was kept as one of the differential diagnosis. Although there was no history of diarrhea/steatorrhea or other clinical findings of malabsorption, further investigations to rule out malabsorption as a cause were done. Hemogram did not reveal anemia and peripheral smear was normal. Stool examination was normal. Upper gastrointestinal (GI) endoscopy was done which was also normal. Duodenal biopsy was taken and it did not show pathological abnormalities consistent with malabsorptive disorder [Figure 1]. Antibodies to gliadin and transglutaminase were in normal range. Her D-xylose test was done which was also within normal limits, i.e., 4 mmol/L. We tried supplementation of thyroxine by intravenous route. Injection levothyroxine (LT4) 200 g once in 3 days was started. After five doses of Levothyroxine, her TSH levels started improving and reached 68 μIU/ml. We continued with the doses of intravenous levothyroxine and after five more doses her TSH levels reached 28 μIU/ml with normalization of T3 and T4 levels. On stopping, the intravenous thyroxine and maintaining the patient on oral medication, the TSH started rising again with fall in T3 and T4 levels within 7 days. This provided us with evidence of oral malabsorption of thyroxine.
Figure 1.
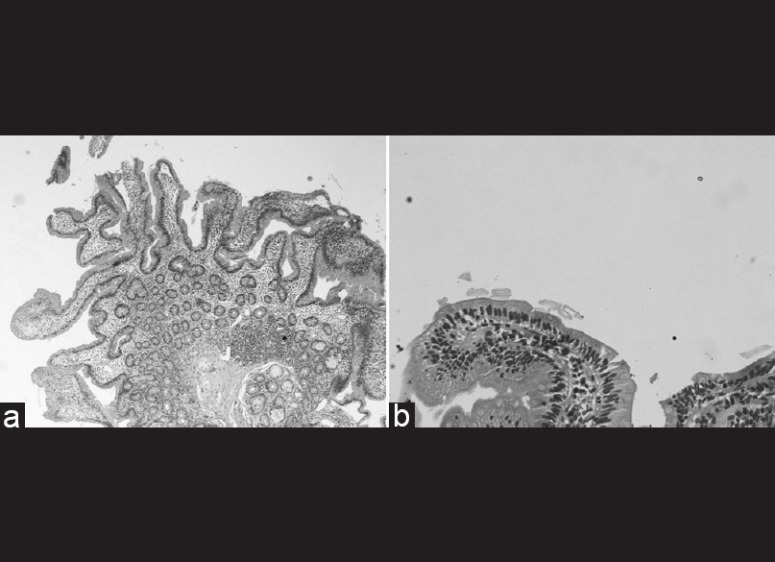
(a) Giemsa stained duodenal biopsy (×4) shows villus to crypt ratio of 3:1,intraepithelial lymphocytes are not increased,no luminal parasite identifed,there is mild chronic inlammatory cell infiltrate in the lamina propria features are non specific. (b) Giemsa stained duodenal biopsy (×20) - one villus with same features as desribed
DISCUSSION
Primary hypothyroidism can be clearly demonstrated by elevation of TSH and decrease in serum free T4 caused due to dysfunction of thyroid gland itself. But the same biochemical picture in spite of adequate or excessive supplementation of oral thyroxine might be due to poor compliance of the patient which is the most frequent cause.[3–5] The other important cause is malabsorption that could be due to GI diseases, pancreatic and liver diseases, dietary interference, or interference due to medications such as antacids, sucralfate, antiepiletics, calcium carbonate amongst others, previous GI surgeries, congestive cardiac failure, and pregnancy.[6]
In the above case, the patient was very much compliant with oral therapy, and it was also tried under medical supervision and hence poor compliance with the drug was excluded. Defect in the conversion of LT4 to triiodothyronine (T3) because of deiodinase-3 deficiency was also suspected which was disproved by her reduced free T4 levels, unresponsiveness even to oral T3, and normalization of T3 also after intravenous T4 supplementation. Her duodenal biopsy was strikingly normal and not consistent with malabsorptive disease. All other investigations relevant for ruling out intestinal malabsorption were done and all turned out to be normal.
Parenteral levothyroxine (LT4) is commercially available in 10 ml flip flop single use in 100 μg, 200 μg or 500 μg vials in lyophilized powder form and it is to be stored at 15–30°C. After injection, the synthetic levothyroxine is no way different from endogenous thyroxine. Its distribution, metabolism, and elimination properties are similar to endogenous thyroxine. Replacement or supplemental therapy by intravenous levothyroxine may be done in congenital or acquired hypothyroidism of any etiology when even high doses of oral thyroxine, given for long enough time, fail to achieve euthyroidism and the possibility of deiodinase deficiency and patient noncompliance has been ruled out. Another indication is when rapid repletion of thyroxine is needed, except in cases of transient hypothyroidism. Another important indication is management of myxedema coma using IV levothyroxine.
After enquiry in numerous pharmacies, only one pharmacy could provide the injection levothyroxine at a cost of Rs. 4700 per vial of 200 μg and that was also not routinely available with them. The patient needs to get it by prior intimation. Thus, we see that in our Indian setup the drug is difficult to procure and expensive.
Our patient responded to 10 doses of parenteral T4, i.e., TSH levels decreased from 370 to 28 μIU/ml and she improved symptomatically. In our Indian setup, where most patients are not covered by insurance, it is highly important to assess the efficacy of such a costly therapeutic regimen, so we repeated the measurement of TSH after five doses of levothyroxine (15 days) to have an early idea about the response.
To find the cause of this unusual selective malabsorption of oral thyroxine, various ideas can be hypothesized. First is the variation which is observed in the absorption of oral thyroxine.[7] Second, thyroid hormone is also important for differentiation and growth of intestinal mucosal cells, and hence the altered states of thyroid hormone also might influence the oral hormonal absorption.[8] The third possible cause could be some specific thyroid hormone uptake defect in the intestinal mucosal cell which can explain the cause for selective malabsorption of thyroid hormone, but this is speculative and not proven so far.
Tönjes et al. in 2006 reported a case of refractory hypothyroidism after total thyroidectomy and radioiodine therapy for papillary thyroid cancer, who benefitted by intravenous LT4administration five times a week. They also suggested the possibility of a specific intestinal uptake deficit, which became apparent in the case of previous thyroid ablation.[9] Jauk et al. in 2000 reported an unusual case of LT4 malabsorption in a patient with papillary thyroid cancer after total thyroidectomy and only parenteral therapy led to clinical and biochemical euthyroidism.[10]
Still the cause of hypothyroidism remains unclear in our patient. But in such cases of refractory hypothyroidism after verifying the compliance with oral therapy and after ruling out all other causes for malabsorption, selective malabsorption of oral thyroxine can be considered and such patients may be treated with parenteral doses of levothyroxine.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ain KB, Refetoff S, Fein HG, Weintraub BD. Pseudomalabsorption of levothyroxine. JAMA. 1991;266:2118–20. [PubMed] [Google Scholar]
- 2.Choe W, Hays MT. Absorption of oral thyroxine. Endocrinologist. 1995;5:222–8. [Google Scholar]
- 3.Eledrisi MS, Szymajda A, Alshanti M, Urban RJ. Noncompliance with medical treatment: Pseudomalabsorption of levothyroxine. South Med J. 2001;94:833–6. [PubMed] [Google Scholar]
- 4.Kubota S, Fukata S, Matsuzuka F, Kuma K, Miyauchi A. Successful management of a patient with pseudomalabsorption of levothyroxine. Int J Psychiatry Med. 2003;33:183–8. doi: 10.2190/0YWR-8DRV-HHP4-UE2E. [DOI] [PubMed] [Google Scholar]
- 5.Ogawa D, Otsuka F, Mimura U, Ueno A, Hashimoto H, Kishida M, et al. Pseudomalabsorption of levothyroxine: A case report. Endocr J. 2000;47:45–50. doi: 10.1507/endocrj.47.45. [DOI] [PubMed] [Google Scholar]
- 6.Lips DJ, Van Reisen MT, Voigt V, Venekamp W. Diagnosis and treatment of levothyroxine Pseudomalabsorption. Neth J Med. 2004;62:115. [PubMed] [Google Scholar]
- 7.Hays MT. Localization of human thyroxine absorption. Thyroid. 1991;1:241–8. doi: 10.1089/thy.1991.1.241. [DOI] [PubMed] [Google Scholar]
- 8.Hodin RA, Shei A, Morin M, Meng S. Thyroid hormone and the gut. Selective transcriptional activation of a villeus enterocyte marker. Surgery. 1996;120:138–43. doi: 10.1016/s0039-6060(96)80280-7. [DOI] [PubMed] [Google Scholar]
- 9.Tönjes A, Karger S, Koch CA, Paschke R, Tannapfel A, Stumvoll M, et al. Impaired enteral levothyroxine absorption in hypothyroidism refractory to oral therapy after thyroid ablation for papillary thyroid cancer: Case report and kinetic studies. Thyroid. 2006;16:1047–51. doi: 10.1089/thy.2006.16.1047. [DOI] [PubMed] [Google Scholar]
- 10.Jauk B, Mikosch P, Gallowitsch HJ, Kresnik E, Molnar M, Gomez I, et al. Case history Unusual Malabsorption of Levothyroxine. Thyroid. 2000;10:93–5. doi: 10.1089/thy.2000.10.93. [DOI] [PubMed] [Google Scholar]


