Abstract
Adrenal incidentalomas of more than 4 cm size are usually malignant. We describe a 28-year-old woman with a 7-cm, non-functioning, well-demarcated adrenal mass, which was identified as an oncocytoma on histopathological examination. Therefore, a large, non-functioning, unilateral adrenal mass with preserved tumor outline should invoke the suspicion of oncocytoma, which is invariably a benign tumor.
Keywords: Adrenal gland, neoplasm, oncocytoma
INTRODUCTION
Adrenal “incidentaloma” is an adrenal mass, generally one cm or more in diameter, that is discovered serendipitously during a radiologic examination performed for indications other than an evaluation for adrenal disease.[1] The incidence of adrenal incidentaloma based on imaging and autopsy data varies from 4 to 6%.[1] The differential diagnoses of unilateral adrenal incidentaloma include cortical adenoma, pheochromocytoma, adrenocortical carcinoma, granulomas (e.g. tuberculosis and histoplasmosis), adrenal cyst, myelolipoma, ganglioneuroma, metastatic deposits and rarely adrenal oncocytoma.[1]
Oncocytomas are epithelial tumors composed of cells with abundant eosinophilic granular cytoplasm packed with mitochondria.[2] Sites of origin for oncocytoma include kidney, salivary glands, parathyroid, lung, pituitary, and ovary.[2,3] However, the oncocytoma of the adrenal gland is very rare. There are nearly 50 case reports of adrenal oncocytoma in English literature.[4–7] These are usually large and non-functional; however, rarely functional adrenal oncocytomas presenting as Cushing's syndrome and pheochromocytoma have also been reported.[6,8]
We describe a case of large, non-functioning adrenal oncocytoma in a young woman who presented with abdominal pain.
CASE REPORT
A 28-year-old female presented to the out-patient department with history of ill-defined, non-colicky abdominal pain in the right flank region for the past 2 months. She was not a known case of hypertension and diabetes. Her past, personal and family history was unremarkable. General physical examination was essentially normal. She did not have any stigma of Cushing's syndrome. Abdominal examination revealed a non-distended, soft abdomen, which was not tender on palpation. Ultrasound (US) abdomen revealed a large heterogeneous mass between the right kidney and the liver, containing both hyperechoic and hypoechoic areas. Computed tomography (CT) scan showed well-demarcated 7 × 5.5 cm homogenous mass arising from the right adrenal gland with few foci of necrosis [Figure 1]. The mass enhanced (50 HU) after contrast and there was no evidence of calcification or surrounding tissue invasion and adenopathy.
Figure 1.

Computed tomography adrenal showing well-demarcated, 7 × 5.5 cm homogenous mass arising from the right adrenal gland with few foci of necrosis (arrow)
Hemogram, electrolytes, renal and liver function tests were normal. Serum cortisol at 0800 hour was 360 nmol/L (normal 171–536 nmol/L) and was suppressible after overnight 1 mg dexamethasone (30 nmol/L). 24 hours urinary metanephrine was 111.6 μg (normal up to 131 μg/24 hours) and normetanephrine was 157.1 μg (normal up to 177 μg/24 hours). Patient underwent laparoscopic right adrenalectomy. There were no fluctuations in blood pressure during perioperative period. On gross examination, the tumor was well encapsulated with maximum measurement of 7 cm. On cut section, it showed no evidence of hemorrhage or necrosis. Histopathology revealed well-encapsulated tumor [Figure 2a] and the cells were arranged in sheets as well as nests. Individual cells had abundant eosinophilic granular cytoplasm with centrally placed nucleus [Figure 2b]. No evidence of necrosis or mitosis was seen. These features were consistent with the diagnosis of adrenal oncocytoma. Her postoperative period was unremarkable. She continues to remain well till the last follow-up after 1 year of surgery.
Figure 2.
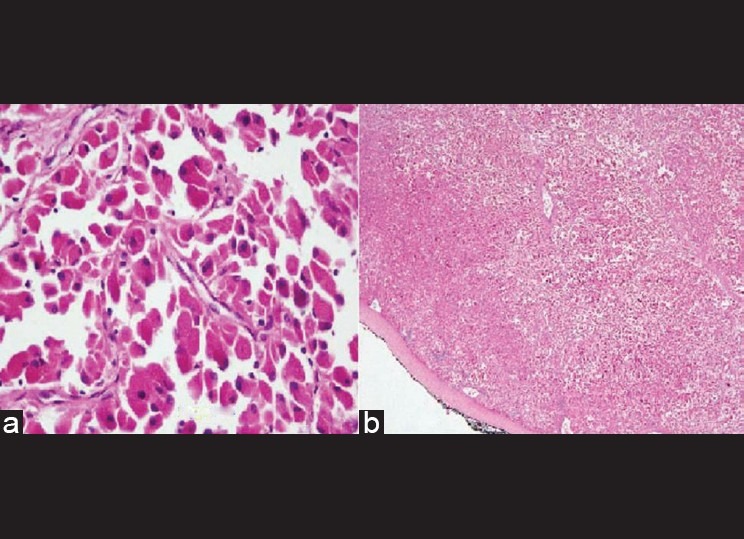
Cells arranged in sheets as well as nests with abundant eosinophilic granular cytoplasm and centrally placed nucleus (a) and Histopathology showing well-encapsulated tumor (b)
DISCUSSION
With the availability and improvement in imaging modalities, adrenal incidentalomas are not uncommon in clinical scenario. Adrenal incidentalomas ≥4 cm in size are likely to be malignant; however, adrenal oncocytoma, a rare cause of adrenal incidentaloma, despite being larger in size, is usually benign.
All the cases of adrenal oncocytoma so far reported in the literature have been diagnosed retrospectively, as there are no clinical and radiological clues to suspect the diagnosis preoperatively.[4–8] Most common site of origin of oncocytoma is kidney; however, the adrenal is affected rarely. Adrenal oncocytoma has been reported in the age group from 27 to 72 years with modest female predilection.[6,8] These tumors vary in size from 3 to 17 cm and are usually larger than 6 cm as seen in our case.[4,5] These tumors do not have a side predilection. Moreover, adrenal oncocytoma dose not follow the rule of four: (a) 4% diagnosed on CT; (b) 4% of these tumors are pheochromocytoma or adrenocortical carcinoma; (c) ≥4 cm in size is an indication for surgery and (d) 4 years of follow-up is required.[9]
They are usually non-functional and benign in nature as was seen in our case. However, few cases of functioning adrenal oncocytomas secreting cortisol and adrenal androgens have been reported.[6,8] Though benign, a few cases of malignant oncocytoma with metastasis to adjacent and distant organs have also been reported.[4,10]
Though imaging characteristics for renal oncocytoma are well described, imaging features of adrenal oncocytoma lack clarity.[11] Fibrous encapsulation visible on US and CT is a characteristic finding for adrenal oncocytomas, though it was not seen in our case.[11,12] Despite being larger in size, the surrounding tissue invasion, particularly fat plane and vascular structure, is characteristically absent, while these features are usually present in adrenocortical carcinoma. The differential diagnoses of other larger but benign adrenal masses include adrenal myelolipoma and adrenal cysts and both can be diagnosed with confidence on imaging. However, the diagnosis of oncocytoma can be secured preoperatively by fine needle aspiration cytology after careful exclusion of functionality of the tumor and particularly in a large mass with preserved tumor outline and without invasion to the surrounding structure.
On gross examination, these tumors are round, well circumscribed and encapsulated. A cut section shows tan brown color with areas of hemorrhage and necrosis. Histologically, these tumors contain cells arranged in solid, tubular, papillary and trabecular pattern. Cells are highly eosinophiilic and granular due to high mitochondrial density.[2]
While the majority of oncocytomas are benign and have an uneventful course, malignant oncocytoma, however, are rare and have a poor prognosis.
CONCLUSION
Adrenal oncocytoma should be included in the differential diagnosis of a unilateral large non-functioning adrenal mass with preserved tumor outline.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Young WF. The Incidentally discovered adrenal mass. N Engl J Med. 2007;356:601–10. doi: 10.1056/NEJMcp065470. [DOI] [PubMed] [Google Scholar]
- 2.Chang A, Harawi SJ. Oncocytes, oncocytosis, and oncocytic tumors. Pathol Annu. 1992;27:263–304. [PubMed] [Google Scholar]
- 3.Smirnova EA, Michailov IG. Electron microscopic characteristic of oncocytoma of the lung, small intestine, and adrenal gland. Arch Pathol. 1968;48:79–81. [PubMed] [Google Scholar]
- 4.Lin BT, Bomsib SM, Mierau GW, Weiss LM, Medeiros LJ. Oncocytic adrenocortical neoplasms: A report of seven cases and review of the literature. Am J Surg Pathol. 1998;22:603–14. doi: 10.1097/00000478-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Waters PR, Haselhuhn GD, Gunning WT, Phillips ER, Selman SH. Adrenocortical oncocytoma: Two case reports and review of literature. Urology. 1997;49:624–8. doi: 10.1016/s0090-4295(96)00543-2. [DOI] [PubMed] [Google Scholar]
- 6.Sharma N, Dogra PN, Mathur S. Functional adrenal oncocytoma: A rare neoplasm. Indian J Pathol Microbiol. 2008;51:531–3. doi: 10.4103/0377-4929.43751. [DOI] [PubMed] [Google Scholar]
- 7.Goel T, Thomas J, Garg S, Rao AC, Reddy S. Adrenal oncocytoma masquerading as functional tumor. Indian J Urol. 2007;23:77–8. doi: 10.4103/0970-1591.30275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander A, Paulose KP. Oncocytic variant of adrenal carcinoma presenting as Cushing's syndrome. J Assoc Physicians India. 1998;46:235–7. [PubMed] [Google Scholar]
- 9.Alexandrakia KI, Gross AB. Adrenal incidentalomas: ‘The rule of four’. Clin Med. 2008;8:201–4. doi: 10.7861/clinmedicine.8-2-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El-Naggar AK, Evans DB, Mackay B. Oncocytic adrenal cortical carcinoma. Ultrastruct Pathol. 1991;15:549–56. doi: 10.3109/01913129109016262. [DOI] [PubMed] [Google Scholar]
- 11.Shah RK, Oto A, Ozkan OS, Ernst RD, Hernandez JA, Chaudhary HB, et al. Adrenal oncocytoma: US and CT findings. JBR-BTR. 2004;87:180–2. [PubMed] [Google Scholar]
- 12.Gandras EJ, Schwartz LH, Panicek DM, Levi G. Case report: Adrenocortical oncocytoma: CT and MRI findings. J Comput Assist Tomogr. 1996;20:407–9. doi: 10.1097/00004728-199605000-00016. [DOI] [PubMed] [Google Scholar]


