Abstract
Noncommunicable diseases and injuries account for 52% of deaths in India. Burden of noncommunicable diseases and resultant mortality is expected to increase unless massive efforts are made to prevent and control NCDs and their risk factors. Based on available evidence, cancer, diabetes, hypertension, cardiovascular diseases, stroke, chronic obstructive pulmonary disease, chronic kidney disease, mental disorders and trauma are the leading causes of morbidity, disability and mortality in India. Government of India had supported the States in prevention and control of NCDs through several vertical programs since 1980s. However, during the 11th plan, there was considerable upsurge to prevent and control NCDs. New programs were started on a low scale in limited number of districts. However, there has not been any considerable change in the burden of NCDs. Based on experiences in the past, there is need to emphasize on health promotion and preventive measures to reduce exposure to risk factors. Facilities and capacity for screening, early diagnosis and effective management are required within the public health care system. Public awareness program, integrated management and strong monitoring system would be required for successful implementation of the program and making services universally accessible in the country.
Keywords: Disease burden, life style diseases, NCD policy and programs, noncommunicable diseases, risk factors
Introduction
Chronic noncommunicable diseases (NCDs) have replaced communicable diseases as the most common causes of morbidity and premature mortality worldwide. About 80% of the burden occurs in low and middle-income countries and 25% is in individuals younger than 60 years. The global economic impact of NCDs is enormous; by 2015, just two diseases (cardiovascular diseases and diabetes) are expected to reduce global GDP by 5%. Approximately half of the total economic burden is reported to account for by CVD including stroke, ischemic heart disease and peripheral vascular disease, which together cause more deaths than HIV/AIDs, malaria and tuberculosis combined.(1) In recognition of the increasing burden and importance of chronic diseases, in 2005, the World Health Organization (WHO) released a plan for NCD prevention and control, which offers the health community a new global goal to reduce death rates from all chronic diseases by 2% per year over and above existing trends during the next 10 years”.(2)
Burden of noncommunicable diseases in India
As of 2004, NCDs contributed half of the total mortality and were the major causes of death.(3) Among the NCDs, cardiovascular diseases are number one cause of mortality (52%). NCDs account for more than two-fifth (43%) of the DALYs and among this group, cardiovascular diseases, diabetes, cancers together account for 40% of the NCD-related DALYs in India. Regional studies have reported that even in rural India the leading cause of death (32%) is NCDs followed by injuries and external cause of deaths (12%).(4) Projection estimates from the WHO have shown that by the year 2030, CVDs will emerge as the main cause of death (36%) in India. Since the majority of deaths are premature, there is a substantial loss of lives during the productive years as compared to other countries.
The salient features of the Causes of Death Survey (2001-03) conducted by the Registrar General of India were:(5)
The overall noncommunicable diseases are the leading causes of death in the country, constituting 42% of all deaths. Injuries and ill-defined causes constitute 10% of deaths each. However, majority of ill-defined causes are at older ages (70 or higher years) and most ill-defined deaths are likely to be from noncommunicable diseases.
Urban areas have a lower number of deaths from communicable, maternal, perinatal and nutritional conditions but a higher proportion from noncommunicable diseases (56%). Their proportion is less in rural areas (40%). Injuries constitute about the same proportion in both rural and urban areas.
Overall, the leading cause of death is cardiovascular disease (19%), followed by respiratory diseases (namely chronic obstructive pulmonary disease or COPD, asthma, other respiratory diseases; 9%), diarrheal diseases (8%), perinatal conditions (6.3%), respiratory infections such as acute pneumonia (6.2%), tuberculosis (6%), malignant and other neoplasms (5.7%), senility (5.1% - which is concentrated at ages 70 and higher), unintentional injuries: other (4.9%), and symptoms, signs and ill-defined conditions (4.8%) [Figure 1].
Figure 1.
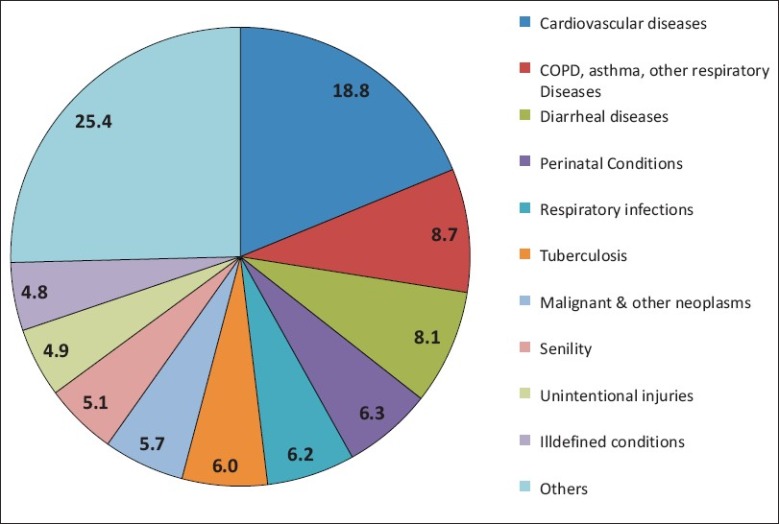
Causes of death survey: 2001-03
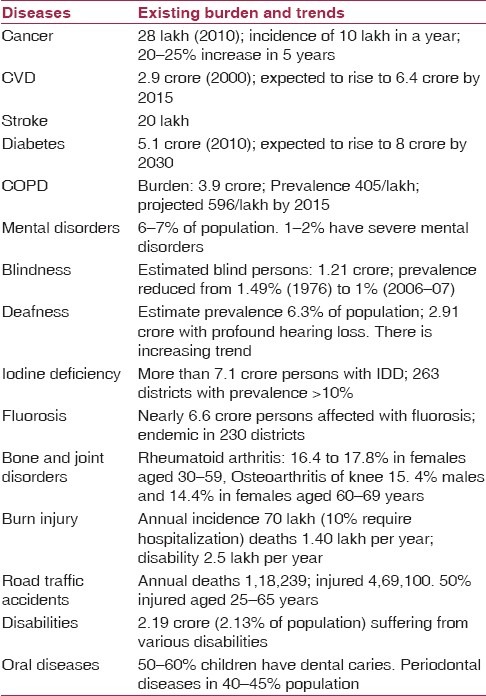
Based on available evidence, cancer, diabetes, hypertension, cardiovascular diseases, stroke, chronic obstructive pulmonary disease, chronic kidney disease, mental disorders and trauma are the leading causes of morbidity, disability and mortality in the country [Table1].
Table 1.
Estimated burden and trends of Noncommunicable diseases in India(6)
National response to NCDs
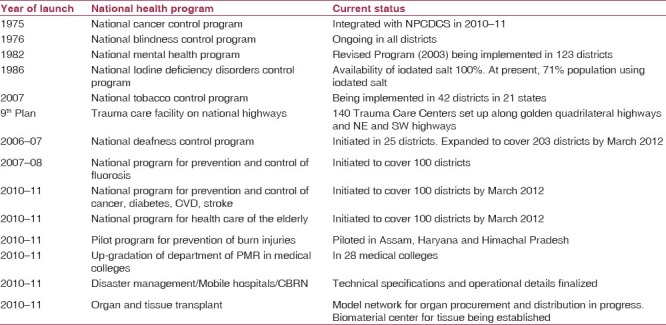
Government of India had supported the States in prevention and control of NCDs through several vertical programs. National Health Programs for Cancer and Blindness were started as early as 1975 and 1976, respectively, followed by program on Mental Health in 1982. However, during the 11th Plan, there was considerable upsurge to prevent and control NCDs. New programs were started on a low scale in limited number of districts. Convergence with public sector health system was a feature of these programs. Some of the programs were within the framework of National Rural Health Mission. New programs focused on CVDs, diabetes, stroke, tobacco control, deafness, trauma, burns, fluorosis and geriatric problems. These programs have given insights of problems and experiences in implementation that would be useful in up-scaling and expanding them across the country. National Health Programs implemented during the 11th Plan and their status is given in Table 2.
Table 2.
Status of national health programs on NCDs in India
Broadly, across programs, following experiences were observed and lessons learnt in implementation of programs, which need to be addressed during the 12th Plan:
Health promotion and prevention need to be given more attention to reduce the incidence of NCDs and their risk factors;
The States need to be given flexibility in implementation of the programs based on their public sector health system, prevalence and distribution of NCDs and socio-cultural context. The flexibility would, however, should be within broad policy framework.
Convergence and integration would be critical in implementation of large number of interventions, which would require unified management structure at various levels.
Integration of cross-cutting components like health promotion, prevention, screening of population, training, referral services, emergency medical services, public awareness program management, monitoring and evaluation etc. would save on costs and make implementation more effective.
Future plan to prevent and control NCDs
There is adequate evidence that NCDs are major contributors to high morbidity and mortality in the country. Risk factors including tobacco and alcohol use, lack of physical activity, unhealthy diet, obesity, stress and environmental factors contribute to high disease burden of NCDs, which are modifiable factors and can be controlled to reduce incidence of NCDs and better outcomes for those having NCDs. Most of the NCDs like cancer, diabetes, cardiovascular diseases (CVD), mental disorders and problems relating to aging are not only chronic in nature but also may have long pre-disease period where effective lifestyle changes can turn around health status of individuals. Costs borne by the affected individuals and families may be catastrophic as treatment is long term and expensive. The economic, physical and social implications of NCDs are significant justifying investment both for prevention and management of NCDs and well-established risk factors.
The efforts made by Government of India and the States have not been able to check rising burden of NCDs. Investments during the 11th Plan and earlier plans have been more on provision of medical services, which have not been adequate in the public sector. Private sector has grown particularly in urban settings but is beyond the reach of the poor and middle sections of the society. There is urgent need for a comprehensive scheme that should focus on health promotion and prevention of NCDs and their risk factors and comprehensive management of NCDs at various levels across the country. While Government of India's role should be policy formulation, population-based multi-sectoral interventions, technical and financial support, the onus of implementation should be with the States. Lessons learnt during the 11th Plan should be addressed and the programs for various NCDs and their risk factors should be integrated and converged with public sector health system. As many programs are either new or expanded after piloting in small number of districts and as NCDs are prevalent in rural as well as urban areas, it would be critical to have a separate implementation and monitoring structure at various levels though as an integral part of the Public Sector Health System.
Policy and approach
There have been some legal measures taken by Government of India aiming at noncommunicable diseases e.g. the Mental Health Act 1987(7) and the Tobacco Control Act 2003(8) which aimed at prohibition on advertisement and regulation on production, supplies and distribution of tobacco products. However, implementation of these acts is a challenge.
The National Health Policy 2002(9) did not spell out any clear directions on prevention and control of NCDs though it did mention (para 1.6) that there is increase in mortality due to lifestyle diseases and trauma. Except for Mental Health Services (para 2.13.1 and 4.13.1.1), there is hardly any policy direction spelt on prevention and control of NCDs and their risk factors. It is expected that revision in National Health Policy is due and should duly emphasize policies and strategies to prevent and control NCDs including population-based interventions that require multi-sectoral approach.
A comprehensive approach would be required for both prevention and management of NCDs in the country through following key strategies:
Health promotion for healthy lifestyles that preclude NCDs and their risk factors
Specific prevention strategies which reduce exposure to risk factors
Early diagnosis through periodic/opportunistic screening of population and better diagnostic facilities
Infrastructure development and facilities required for management of NCDs
Human resources and their capacity building for prevention and treatment of NCDs
Establish emergency medical services with rapid referral systems to reduce disability and mortality due to NCDs
Treatment and care of persons with NCDs including rehabilitation and palliative care
Health legislation and population-based interventions through multi-sectoral approach for prevention of NCDs
Building evidence for action through surveillance, monitoring and research.
Programs
Most of the NCDs are prevalent across the country though there may be regional variations. The plan of action therefore should cover all the districts of the country in a phased manner in the coming years giving high priority to districts with high prevalence and low level of available services. To ensure convergence and integration with public health services, a decentralized approach is recommended with district as the management unit for programs. The country should not limit programs to major NCDs but cover all NCDs in an integrated manner. Diseases to be covered and other interventions recommended for inclusion are summarized below:
-
Programs for lifestyle chronic diseases and risk factors
- Cancer
- Diabetes, cardiovascular diseases (CVD) and stroke
- Chronic obstructive pulmonary diseases
- Chronic kidney diseases
- Organ and tissue transplant
- Mental disorders
- Iodine deficiency disorders
- Fluorosis
- Oro-dental disorders
-
Programs for disability prevention and rehabilitation
- Trauma (including road traffic accidents)
- Burn injuries
- Disaster response
- Emergency medical services
- Musculo-skeletal (Bone and Joint) disorders
- Physical medicine and rehabilitation
- Blindness
- Deafness
- Health care of the elderly (geriatric disorders)
- Neurological disorders (epilepsy, autism)
- Congenital diseases
- Hereditary blood disorders (sickle cell anemia, thalassemia, hemophilia)
-
Health promotion and prevention of NCDs
- Tobacco control
- Prevention and management of nutritional disorders and obesity
- National institute for health promotion and control of chronic diseases
- Patient safety program
- Establishment of air port/port health offices
Implementation
To ensure long-term sustainability of interventions, the programs should be built within existing public sector health system and feasible public-private partnership models. The integrated program should address following levels of care for a comprehensive and sustainable system to prevent and control NCDs:
Primary health care: Health promotion, screening, basic medical care, home-based care and referral system (integration with NRHM)
Strengthening district hospitals for diagnosis and management of NCDs including rehabilitation and palliative care: NCD clinic, intensive care unit, district cancer centre, dialysis facility, geriatric centre, physiotherapy center, mental health unit, trauma and burn unit, strengthening of facilities for orthopedic, oro-dental, eye and ENT departments, tobacco cessation center, obesity guidance clinic.
Tertiary care for advanced management of complicated cases including radiotherapy for cancer, cardiac emergency including cardiac surgery, neurosurgery, organ transplantation etc.
Emergency medical care and rapid referral systemth including highway trauma centers and 108 EMS services.
Health Promotion and Prevention: Legislation, population-based interventions, behavior change communication using mass media, mid-media and interpersonal counseling and public awareness programs in different settings (schools, colleges, work places and industry).
Universal coverage
India should ensure universal coverage and implement the program in all 640 districts. To ensure convergence, common districts should be selected for all interventions. The schemes should be flexible to meet local requirements as there would be variation in prevalence and availability of existing health infrastructure. Districts need to be selected based on selected identified parameters including disease burden and availability of human resources and facilities but in consultation with the states.
Monitoring and Evaluation
Monitoring of the programs for prevention and control of noncommunicable diseases, their risk factors and determinants is essential to provide the evidence for advocacy, policy development, program planning, monitoring and evaluation. Monitoring should not only be limited to tracking data on the magnitude of and trends in noncommunicable diseases, but should also include evaluating quality of services, their effectiveness and impact on disease burden and outcomes.
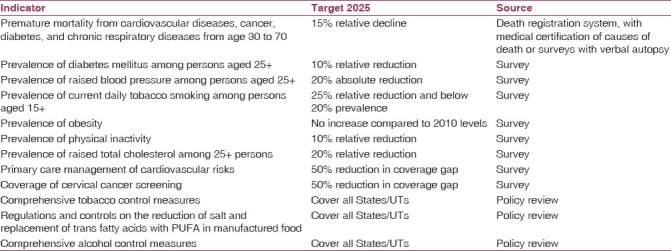
An independent evaluation of the program should be periodically carried out and required corrective measures should be taken based on response, unforeseen challenges and issues. While the programs should set short-term targets for each intervention and monitor progress for each identified indicator (input, process, output), long-term targets need to be set up. Proposed targets for key indicators and their sources of information are given in Table 3.
Table 3.
Proposed long terms targets for prevention and control of NCDs
Conclusion
There is evidence to show that NCDs are leading causes of death, disability and morbidity and their burden is likely to increase if urgent interventions are not initiated on a mass scale throughout the country. Currently implemented programs that address NCDs have not been able to reduce their burden due to limited scale of implementation. The Government should consider a massive investment and effort to prevent and control NCDs and their risk factors in the coming years. An integrated and comprehensive approach is suggested that gives emphasis on health promotion, population-based interventions, prevention of exposure to risk factors, specific measures at individual and family level, early diagnosis through screening and better diagnostic facilities, improved capacity for management and universal access to health services.
Acknowledgments
The paper is based on Plan of Action for Prevention and Control of NCDs in India during the 12th Plan. The authors acknowledge contribution of all members of the Working Group on Disease Burden (sub-group NCD) for their contribution.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Anderson GF, Chu E. Expanding priorities-confronting chronic disease in countries with low income. N Engl J Med. 2007;356:209–11. doi: 10.1056/NEJMp068182. [DOI] [PubMed] [Google Scholar]
- 2.2008-2013 action plan for the global strategy for the prevention and control of noncommunicable diseases: prevent and control cardiovascular diseases, cancers, chronic respiratory diseases and diabetes. Geneva: WHO; 2008. World Health Organization. [Google Scholar]
- 3.World Health Organization. Mortality and Burden of Disease Estimates for WHO Member States in 2004. [Last accessed on 2011 Nov 30]. Available from: http://www.who int/entity/healthinfo/global_burden_disease/gbddeathdalycountryestimates2004 xls 2009 .
- 4.Joshi R, Cardona M, Iyengar S, Sukumar A, Raju CR, Raju KR, et al. Chronic diseases now a leading cause of death in rural India-mortality data from the Andhra Pradesh Rural Health Initiative. Int J Epidemiol. 2006;35:1522–9. doi: 10.1093/ije/dyl168. [DOI] [PubMed] [Google Scholar]
- 5.Office of the Registrar General of India. New Delhi: Government of India; 2010. Report on causes of deaths in India 2001-2003. [Google Scholar]
- 6.Plan of Action for Prevention and Control of NCDs in India during the 12th Plan, Directorate General of Health Services, Ministry of Health and Family Welfare. Report Submitted to Planning Commission. 2011 Sep [Google Scholar]
- 7.The Mental Health Act, 1987. The Gazette of India Extraordinary. Ministry of Law and Justice (Legislative Department) Government of India, New Delhi. (22) 1987 [Google Scholar]
- 8.2003. New Delhi: Government of India; The Cigarettes and other Tobacco Products (Prohibition of Advertisement and Regulation of Trade and Commerce, Production, Supply and Distribution) Act, 2003 (COTPA) [Google Scholar]
- 9.National Health Policy-2002. [Last accessed on 2011 Nov 30]. Available from: http://www.mohfw.nic.in.


