Abstract
Project Accept is a RCT designed to test the efficacy of community mobilization (CM), mobile voluntary counseling and testing (MVCT), and post-test support services (PTSS) in reducing HIV incidence in three African countries and Thailand. The intervention started in rural areas, northern Thailand in January 2006. CM initially included door-to-door visits during the daytime, small group discussions and joining organized meetings and followed by MVCT. In February 2007, CM strategy using HIV/AIDS “edutainment” (education and entertainment) during evening hours was introduced. After edutainment was initiated, the number of participants increased substantially. VCT uptake increased from 18 to 28 persons/day on average (t test; t = 7.87 P < 0.0001). Edutainment especially motivated younger people, as the median age of VCT clients decreased from 38 to 35 years old (median test; z = 6.74, P < 0.0001). Providing free MVCT in community settings along with edutainment during evening hours increased VCT uptake and was particularly attractive to younger adults.
Keywords: HIV, Community mobilization, Mobile VCT, Thailand
Introduction
In 2008, an estimated 33.4 million people in the world were living with HIV/AIDS and 2.7 million people were newly infected [1]. Ninety-four percent of cases were working age adults who will become sick and die within 10 years with no access to treatment and care. Unfortunately, roughly 80% live in low and middle-income countries where access to the treatment and care remains limited, and they remain unaware of their HIV infection status [2]. This has led to major crises with consequences for human, social and economic progress unless access to treatment and care, particularly ARV, is addressed. For HIV infected individuals to receive necessary treatment and care, they need to know their HIV infection status through HIV testing. HIV testing provided on a voluntary basis should be accompanied by pre- and post-test counseling (VCT). This has major public health benefits by not only linking infected individuals to treatment and care but also in reducing further HIV transmission [3]. Quality VCT has been demonstrated to reduce HIV risk behaviors [4]. UNAIDS and WHO have supported expanding VCT to cover as many individuals as possible by encouraging countries to established national policies (in 1997) [3] andissued their HIV testing policy statement in June 2004 [5] and guidance on provider-initiated VCT in health facilities in 2007 [6]. Promoting “Universal access” at the XVII International AIDS conference in Mexico City cannot be attained without encouraging people to seek VCT; however expanding VCT had been a challenge in low-and-middle income countries.
This manuscript describes the implementation of community mobilization (CM) to promote VCT services using mobile voluntary counseling and testing (MVCT) units in the intervention communities of NIMH Project Accept Thailand site and presents the results. There were some challenges to our approach, and we tested modifications to increase our success. A detailed description of the NIMH Project Accept intervention can be found in the Project Accept (HPTN 043) protocol and manuals at http://www.cbvct.med.ucla [7] and in Khumalo-Sakutukwa et al. [8]. In brief, NIMH Project Accept is the first international multisite study of a phase III community-level randomized controlled trial conducted in 34 communities at 5 sites in 4 countries (South Africa, Zimbabwe, Tanzania and Thailand) to determine the efficacy of a multilevel HIV prevention intervention, where community HIV incidence and stigma reduction are the study end points. Communities were paired within site and randomized to be either control or intervention communities. The control communities received standard VCT (SVCT) which for Thailand site was clinic-based VCT provided at district hospitals. The intervention communities received the project intervention in addition to standard VCT (CBVCT). The project intervention has three components—1) CM—mobilizing the community, stimulating interest and participation, education, stigma reduction and enhancing VCT uptake; 2) MVCT—increasing access to VCT by offering free and same day HIV test results directly in the community, hopefully increasing testing rates and changing HIV testing norms; and 3) post-test support services (PTSS)—to build support and improve the quality of life for HIV positive individuals, reduce social harms, create a support system, as well as assist HIV negative individuals to remain negative. Standard principles were followed in conducting the intervention according to the research protocol by all sites. An intervention working group was established with representatives from the intervention core of each site to address site-specific issues and development of intervention standard operating procedures (SOPs). However, modifications were made to the intervention according to site situations and cultures. The overall utilization out come of the Project Accept trial in three countries (Tanzania, Zimbabwe, and Thailand) presented by Sweat et al. [9] shows that CBVCT captured more first time HIV test cases significantly and four time higher to detect HIV cases (952 vs. 264; P = 0.03) than SVCT, across site.
Project Accept Thailand (PA-Thai) was conducted in partnership with Johns Hopkins University (JHU), Research Institute for Health Sciences, Chiang Mai University (RIHES), and Chiang Mai Public Health Office (CMPHO), Thai Ministry of Public Health. The intervention was launched in January 2006. The operation and data described here are from field notes (counseling chart notes, field notes, staff meeting notes) on conducting the intervention in the intervention communities which was completed up to March 2009. A total of 39 months experience in the field during which the site made local modifications to fit with Thai culture and the local context. In this paper, we present our project CM and MVCT operations overtime and the uptakes in the seven intervention communities as well as the clients’ characteristics and comparing between Thai lowland and ethnic minorities.
Methods
Study Setting and Community Selection
Fourteen communities in six districts (Mae-tang, Chiang Dao, Chaiprakarn, Praow, Mae-Ai, and Fang) of northern Chiang Mai province were selected to be the research communities (Fig. 1).
Fig. 1.
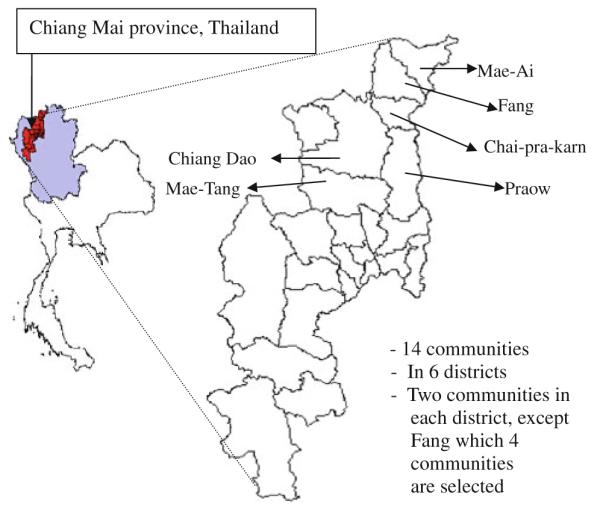
Study setting
The region is mountainous, rural and home to lowland Thais and ethnic minorities including Lahu, Karen, Hmong, Lisu, Yao, and Burmese immigrant (Shan), groups who vary in geographic area of origin and language. Two communities were selected from each district, except Fang where four were selected, paired within each district for randomization to intervention or control, for a total of seven pairs at the Thailand site. Each community wascomprised of 8–23 villages from 1 to 2 sub-districts. Using baseline data, the estimated community size ranged from 5,000 to 9,200. Ethnic minorities made up 40% of residents in the 14 communities [10]. These 14 communities are similar in term of communities’ resident way of life where most of them are famers or being hired for daily working in agriculture farms. Each district has a district hospital to provide health care for the district residents and others. The hospitals provide clinic-based VCT and have opts out VCT policy for pregnant women. Very few if any of an organization, other than our project, provided mobile VCT in these communities.
Community Preparedness and Involvement
Community preparedness and involvement is a main component of NIMH Project Accept. The protocol required sites to undertake a rigorous program of community pre-paredness and involvement, and required establishment of Community Working Groups (CWG) which included community leaders and stakeholders. The Thai site introduced the project to the communities by first meeting with community stakeholders including the district governors, district hospital directors and VCT unit nurses, district public health chiefs and key personnel, and sub-district leaders. In these meetings we introduced the project concepts and procedures, and asked for their opinions and support. The purpose of these meetings was to gain entry to the communities with acceptance, from the top down. After this meeting the CWG in each community was formed, comprised of village leaders, village health volunteers, persons infected with HIV/AIDS (PWHA), housewife leaders, and youth leaders. Meetings with CWGs were conducted several weeks before each research activity was conducted in the community. The meetings were mostly led by the local PI and accompanied by at least one representative from the CMPHO. The primary aim was to inform the CWGs about the activities that were going to occur and to ask for their suggestions on conducting project activities and to seek their assistance.
The intervention protocol required establishing community-based outreach volunteers (CBOVs) in the intervention communities. CBOVs were community members who had the potential to volunteer to work with the project staff to disseminate project information, conduct outreach to community members for HIV/AIDS information, and encourage local participation. CBOVs were trained using a standardized project curriculum.
Religious figures (monks and priests) are influential local leaders and earn much respect from community members; they were invited to join the project in each research community. The team worked with respected monks who were actively working with HIV/AIDS issues in the province to organize HIV/AIDS education for local monks. In turn these monks assisted the study similar to CBOVs. Once understanding the project and local HIV/ AIDS issues, these religious figures could clearly explain the goal of the project to community members and effectively respond to their questions.
Staff Composition
With an estimated 40% ethnic minorities residing in the project communities, we recruited CM staff who did out-reach for community mobilization and HIV/AIDS education who could speak lowland Thai and at least one ethnic minority language. Seven ethnic minorities of 11 CM staff were successfully recruited and later more were added. Qualified nurses were recruited and trained to be HIV VCT counselors and phlebotomists using a scripted risk reduction counseling curriculum, 10–15 in number over the intervention period. Nurses from the 6 district hospitals were also trained as counselors to provide standard VCT (SVCT) for the project. These nurses joined the MVCT team occasionally. Almost all CM staff was trained to be VCT counselors after the first round when we realized the need and importance of counseling in the ethnic minorities languages for those who had limited Thai language capacity. PTSS personnel were comprised of core and local staff as well as staff from the community health centers who were Ministry of Public Health employees working part-time for the project in the evenings and weekends.
Conducting the Intervention (Findings, Challenges and Modifications)
PA-Thai launched the intervention in the seven intervention communities beginning in January 2006. CM and MVCT were conducted by round. This intervention round defined as the conduct of CM and MVCT activities sequentially in all seven communities before starting the next round. Each round took about 3-6 months to complete and by March 2009 we had completed the intervention in the seven intervention communities for a total of seven rounds. Weekly meetings to discuss outcomes, difficulties and strategies were held with the project director and senior staff, with more lengthy meetings following each completed round to address major changes for the next round of intervention. Monthly PI and senior staff meetings were held to discuss issues raised and to problem-solve as needed to adapt the intervention.
For the first three rounds of intervention (Jan-Dec 2006), PA-Thai followed the conventional strategies of delivering services to the communities. The CM teams entered the scheduled villages first, followed by MVCT teams 3–5 days later to deliver VCT. In order to gradually introduce the project, HIV/AIDS education, and mobile VCT to community members the CM strategies used were going door-to-door and holding small group meetings with village members during the day to educate community members about HIV and to alert them to the upcoming availability of MVCT testing during the scheduled time period in their community. Problems encountered included too few people being at home during the day (largely being elderly women), many of whom had difficulty understanding Thai. CM staff tried joining community leader organized meetings that were already planned for the purpose of discussing village issues. During these meetings important community members were in attendance. Since these meetings had their own lengthy agendas, HIV education and mobilization activities occurred only at the end of very long meetings with members demonstrating fatigue and lack of interest. Meeting attendees also did not seem motivated to disseminate information to their community. Day-time CM organized meetings remained the CM strategy as a result, occasionally incentivized by small gifts for participation. Adjustments were made to include setting CM activities according to the dates and times suggested by community leaders, providing MVCT services during evening hours, and splitting staff into smaller teams in order to stay at each service venue for a longer period of time. However, the overall number of people who utilized the MVCT service showed a decreasing trend in rounds 2 and 3.
In the middle of the third round of the intervention in November 2006, a special CWG meeting with the Chai Prakan intervention community leaders was organized. The community was selected because they experienced the greatest decrease in MVCT utilization. At the meeting, there was agreement that the community and PA-Thai project would co-host a large community event called “PA-Thai concert for World AIDS Day” on the evening of November 25, 2006. The activities included entertainment shows by well known local singers and artists, traditional shows by community youth, a PA-Thai HIV knowledge booth, donations for the community AIDS fund, World AIDS Day awareness activities, and the sale of lottery tickets for prizes. The event was a major success in raising HIV/AIDS awareness as well as increasing people’s recognition of the PA-Thai project. Thousands of villagers joined the activities that night and many asked for HIV VCT.
Lessons learned from the PA-Thai concert World AIDS Day is that offering VCT at events can attract large numbers of people to participate. The PA-Thai team decided to adopt similar approaches for CM and VCT strategies for the upcoming fourth round, starting in February 2007, but on a reduced scale providing events and services during evening hours, using a strategy referred to as “edutainment”. All MVCT and CM staff was combined into one team to work together at the same venue for edutainment activities.
The “edutainment” events were divided into several tents, with activities including VCT, HIV education sessions, blood pressure check-up, karaoke, movie projection, sport games, and prize give-always for active participants. Villagers could choose to join activities voluntarily in no particular order. There are three main CM activities which included: HIV/AIDS related games in order to raise HIV transmission awareness, interactive group HIV/AIDS education include VCT, and interactive group education about HIV prevention and condom use. To encourage participation in the three CM activities, a card was given to individual participants and a check mark was added when s/he participated in each activity. Participants who attended all three CM activities were eligible for lottery ticket drawing. Prizes included a small carton of pasteurized milk, cooking oil, soap, detergent, a bag of snacks, etc. Typically, the facilities were set up and ready by 5 pm and activities were finished around 10-11 pm. Loudspeaker announcement vans and door-to-door strategies just before the event were still used as needed. After three rounds of edutainment, in round seven the team attempted to enroll community members who have not yet opted to receive services and a semi opt-out strategy was adapted in addition to “edutainment”. Village health volunteers and CBOVs joined forces for the opt-out strategy. These people went from house to house to collect lists of people interested in getting VCT and to give them an appointment date and time to schedule VCT services. On the scheduled date, volunteers reminded villagers again about the services. The volunteers were given a t-shirt or a jacket for their participation in the program according to the success of their recruitment. The voluntary nature of VCT was enforced during pre-test counseling. Community public venues including schools, churches, temples, and community centers were used as venues to set up MVCT units and the “edutainment” events.
MVCT Process
After setting up VCT at a selected venue, cards with unique numbers were given to individuals who desired VCT. Each individual client was assigned to a counselor for pre-test counseling. After consent for VCT and pre-test counseling were completed, the counselor led the client for a finger prick for rapid HIV testing. Two HIV rapid test kits were used in parallel, Bioline HIV-1/2 (Pacific Biotech CO., LTD., Thailand) and Determine HIV-1/2 (Abbott Laboratory, Japan). When both test kits gave the same result, the HIV infection status of the client was judged according to the results. If the results were discordant, a third kit(ACON HIV-1/2 (Acon Biotech CO., LTD., Hangzhou, and P.R. China) or Clearview HIV1/2 STAT-PAK (Inverness Medical Professional Diagnostics)) was used as a confirmation. Clients were asked to keep his/her card while waiting for test results. While waiting many VCT participants joined CM activities. The result was usually available within 30 min, and the same counselor provided the client with post-test counseling. An anonymous VCT and client centered risk reduction counseling approach was used for Project Accept. Only the unique number on the card was recorded on data collection forms and counseling chart notes. The counselor kept the card after completing post-test counseling. With this approach it was not possible to identify the client. Clients were provided a certificate of test results if requested or were referred for additional medical attention and support as needed.
Data Collection, Management and Analysis
Pre- and post-test counseling chart notes were created for the purpose of counseling individuals as well as collecting data which include demographic characteristics, history of prior VCT, and HIV risk behaviors. The data were entered into an excel spreadsheet and exported for data management and analysis in SAS 9.1 and Stata 9. As each intervention community received the same intervention strategy in each round and is similar in term of the residents’ characteristics and VCT access, thus the seven communities are combined for data analysis. Frequency tabulation, percentage, and χ2 test are used for data presentation and analysis. Meeting and field notes were also used.
Ethical Review
PA-Thai underwent ethical review at each of the three institutions involved, the Johns Hopkins Bloomberg School of Public Health, Chiang Mai University Research Institute for Health Sciences (RIHES), and Ministry of Public Health (MOPH).
Results
From Jan 6th, 2006 to March 25th, 2009, we completed seven rounds of CM and MVCT activities in the seven intervention communities with 574 days of field activities. A total of 57,007 community residents aged 16 years or older participated in CM activities, of whom 31,813 (55.8%) were female. Persons could attend CM activities repeatedly. During the first three rounds using conventional strategies, mostly door-to-door outreach and group discussion without setting up MVCT concurrently in the same day, were conducted. In round 4 we shifted to the edutainment strategy where MVCT concurrently setting up near by. The numbers of clients reached increased with the change in strategy, as well as numbers of days spent each round. When calculating number of CM participants/10 staff hours invested, theses are 53, 39, and 18 persons respectively/10 staff hour for door-to-door outreach, group discussion without MVCT concurrently setting up near by in the same day, and edutainment with MVCT setting up concurrently near by. In CM activities, which were conducted at night, persons aged younger than 16 years attended the edutainment sessions many more than persons aged 16 years and older.
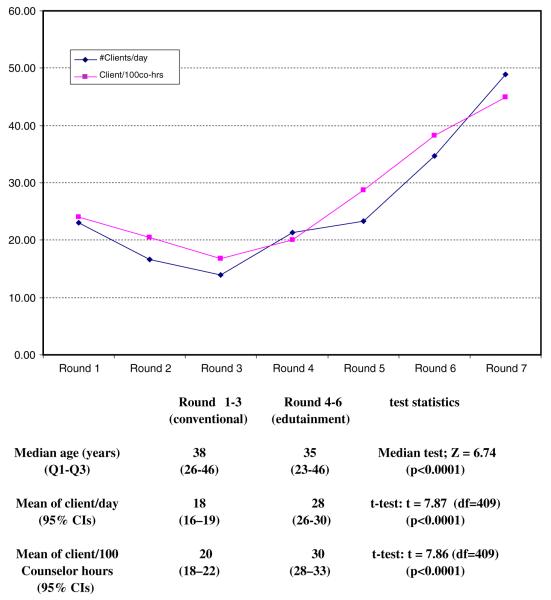
There were 17,785 persons aged 16 years and over who participated in VCT services: 8,503 (48%) men and 9,282 (52%) women. Of the participants 7,093 (39.9%) reported a history of prior HIV testing and 632 (3.6%) declined to have an HIV test from the project. Median age of clients was 36 years old. With same day results, higher proportions of clients received their test results (98.7%). The numbers of VCT clients show a decreasing trend in the second to third round which led to the shift of CM and MVCT approaches to edutainment from the 4th round onward. The numbers of MVCT clients then increased through the 7th round. The trends of MVCT clients are reflect in both absolute numbers but also by clients/day and clients/counselor hours available in each round (Fig. 2; Table 1).
Fig. 2.
Number of MVCT clients/day and 100 counselor hours by round, northern Thailand 2006–2009
Table 1.
CM and MVCT operational provision, northern Thailand 2006–2009
| Descriptions | Round # and dates (dd/mm/yy) of conducting the activities |
||||||
|---|---|---|---|---|---|---|---|
| Conventional CM strategies |
Edutainment strategy |
Edutainment and semi opt-out |
|||||
| 1 03/01/06– 02/04/06 |
2 4/05/06– 5/08/06 |
3 2/09/06– 8/12/06 |
4 1/02/07– 6/06/07 |
5 21/06/07– 31/10/07 |
6 5/11/07– 4/06/08 |
7 13/06/08– 25/03/09 |
|
| # of activities days | 48 | 56 | 56 | 67 | 73 | 111 | 163 |
| # of CM clients aged 16 years and older |
7,513 | 5,796 | 7,513 | 8,306 | 6,903 | 10,934 | 10,042 |
| # of VCT clients | 1,107 | 932 | 781 | 1,427 | 1,705 | 3,852 | 7,980 |
| Median age of clients | 39 | 37 | 36 | 36 | 30 | 35 | 38 |
| Counselor field hours | 4,608 | 4,541 | 4,666 | 7,108 | 5934 | 10,067 | 17,788 |
| #clients/day | 23 | 17 | 14 | 21 | 23 | 35 | 49 |
| #clients/100 co-hours | 24 | 20 | 17 | 20 | 29 | 38 | 45 |
| # of clients have repeat testing after previously test with PA-Thai (% of VCT clients) |
0 | 37 (4.0) | 56 (7.2) | 116 (8.1) | 161 (9.4) | 461 (11.9) | 1611 (20.2) |
| Number clients (aged ≥ 15 years old) by CM activities and by 100 h of each activities |
Total # session performed |
# clients | # client/session | Total working hours |
# clients/10 working hours |
|---|---|---|---|---|---|
| Activities with MVCT conducted concurrently near by (mostly edutainment) |
499 | 30,512 | 61 | 16,512 | 18 |
| Group discussion without MVCT conducted concurrently |
472 | 18,674 | 39 | 4,745 | 39 |
| Door-to-door out reach | 381 | 7,708 | 20 | 1,443 | 53 |
Counselor hours available were rarely oversubscribed at each MVCT event, so few clients were turned away due to lack of counselors. The average number of clients per day between 1–3rd and 4–6th rounds were significantly different (18 vs. 28; t test: t = 7.87 (df = 409), P < 0.0001). The average age of clients were younger in 4-6th compared to 1-3rd round with the medians of 35 and 38, respectively (median test: z = 6.74, P < 0.0001). The seventh round is not considered as the semi opt-out strategy was used along with other strategies. The percentages of repeat testers also increased over time as forecasted.
Comparisons of characteristics of the 17,153 who decided to get an HIV test for Thai lowlanders and ethnic minorities are shown in Table 2. As of December 2009, there were 44,477 persons aged 16 years and over in the intervention communities, 19,054 ethnic minorities and 25,423 Thai lowlanders. Of the population age 16 and over, 8,786 cases (34%) of lowland Thai and 8,386 cases (44%) of the ethnic minorities came for HIV test with the project (χ2 = 410.5 (df = 1), P = 0.000). When compared to Thai lowlanders, ethnic minorities had a higher proportion of persons aged 30 years or younger (53.7 vs. 21.9%; χ2 = 1849.4 (df = 1), P = 0.000) had no formal education (4.6 vs. 54.2%; χ2 = 513.0 (df = 1), P = 0.000), had a higher proportion being first time testers (64.9 vs. 54.3%; χ2 = 200.1 (df = 1), P = 0.000), and had a higherproportion with a history of drug use (6.9 vs. 5.8%; χ2 = 8.3(df = 1), P = 0.004). Injecting drug users was similar among the two ethnic groups (9.6 vs. 9.4% χ2 = 0.02 (df = 1), P = 0.901)). Approximately 6% of these two populations had more than one sexual partner in the prior 6 months.
Table 2.
Characteristics of MVCT clients by total number and ethnicity, northern Thailand 2006–2009
| # MVCT clients and % by characteristics |
||||
|---|---|---|---|---|
| Total | Thai lowland | Ethnic minorities | χ2; P value | |
| # Test at the project MVCT | 17,153 (100%) | 8767 (100%) | 8386 (100%) | 0.40 (df = 1); P = 0.53 |
| Male | 8168 (47.6) | 4154 (47.4) | 4014 (47.9) | |
| Female | 8985 (52.4) | 4613 (52.6) | 4372 (52.1) | |
| Age | ||||
| 16–20 | 2808 (16.4) | 858 (9.8) | 1950 (23.3) | 2.6 × 103 (df = 4); P = 0.000 |
| 21–30 | 3621 (21.1) | 1065 (12.1) | 2556 (30.6) | |
| 31–40 | 3770 (22.0) | 1776 (20.3) | 1994 (23.9) | |
| 41–50 | 4310 (25.2) | 2996 (34.2) | 1314 (15.7) | |
| >50 | 2614 (15.3) | 2072 (23.6) | 542 (6.5) | |
| Occupation | ||||
| Unemployed | 504 (2.9) | 239 (2.7) | 265 (3.2) | 488.9 (df = 7); P = 0.000 |
| Hired for daily work | 6290 (36.7) | 3428 (39.1) | 2862 (34.1) | |
| Farmer/gardener | 7214 (42.1) | 3166 (36.1) | 4048 (48.3) | |
| Trader/vender | 620 (3.6) | 463 (5.3) | 157 (1.9) | |
| Housewife/househusband | 569 (3.3) | 285 (3.3) | 284 (3.4) | |
| Government/state employee | 207 (1.2) | 187 (2.1) | 20 (0.2) | |
| Student | 1017 (5.9) | 539 (6.2) | 478 (5.7) | |
| Other | 728 (4.2) | 457 (5.2) | 271 (3.2) | |
| Marital status | ||||
| Single | 3234 (18.9) | 1412 (16.1) | 1822 (21.7) | 178.6 (df = 4); P = 0.000 |
| Married living together | 11499 (67.0) | 5998 (68.4) | 5501 (65.6) | |
| Married living separate | 811 (4.7) | 361 (4.1) | 450 (5.4) | |
| Widowed | 548 (3.2) | 373 (4.3) | 175 (2.1) | |
| Divorced | 1061 (6.2) | 623 (7.1) | 438 (5.2) | |
| Education | ||||
| No formal education | 4954 (28.9) | 405 (4.6) | 4549 (54.2) | 5.3 9 103 (df = 3); P = 0.000 |
| Primary school | 8082 (47.1) | 5819 (66.4) | 2263 (27.0) | |
| Secondary school or higher | 3539 (20.6) | 2119 (24.2) | 1420 (16.9) | |
| Other | 578 (3.4) | 424 (4.8) | 154 (1.8) | |
| # sex partner last 6 months | ||||
| None | 2192 (13.8) | 1356 (16.3) | 836 (11.1) | 94.0 (df = 2); P = 0.000 |
| One | 12679 (79.9) | 6425 (77.3) | 6254 (82.8) | |
| More than one | 994 (6.3) | 528 (6.4) | 466 (6.2) | |
| Any illicit drug use | ||||
| Ever | 1037 (6.4) | 457 (5.8) | 580 (6.9) | 8.3 (df = 1); P = 0.004 |
| Never | 15213 (93.6) | 7408 (94.2) | 7805 (93.1) | |
| Ever injected drug | ||||
| Ever | 99 (9.5) | 43 (9.4) | 56 (9.6) | 0.02 (df = 1); P = 0.901 |
| Never | 939 (90.5) | 414 (90.6) | 525 (90.4) | |
| Last risk behavior | ||||
| None | 9821 (57.3) | 5142 (58.7) | 4679 (55.8) | 24.6 (df = 3); P = 0.000 |
| Sexual intercourse | 6090 (35.5) | 3037 (34.6) | 3053 (36.4) | |
| Share syringe & needle | 25 (0.1) | 5 (0.1) | 20 (0.2) | |
| Others | 1216 (7.1) | 582 (6.6) | 634 (7.6) | |
| Missing = 1 | ||||
| Ever had STI | ||||
| Ever | 1251 (7.3) | 1023 (11.7) | 228 (2.7) | 507.1 (df = 1); P = 0.000 |
| Never | 15877 (92.6) | 7735 (88.2) | 8142 (97.1) | |
| Not sure | 25 (0.1) | 9 (0.1) | 16 (0.2) | |
| Had HIV test before | ||||
| Ever | 6956 (40.6) | 4010 (45.7) | 2946 (35.1) | 200.1 (df = 1); P = 0.000 |
| Never | 10197 (59.4) | 4757 (54.3) | 5440 (64.9) | |
| Time since last HIV test (among confirm negative result of the previous test) | ||||
| Less than 6 months | 438 (7.0) | 233 (6.3) | 205 (8.0) | 85.1 (df = 3); P = 0.000 |
| 6–12 months | 713 (11.4) | 361 (9.8) | 352 (13.7) | |
| 12–24 months | 1805 (29.0) | 971 (26.4) | 834 (32.6) | |
| More than 24 months | 3278 (52.6) | 2108 (57.4) | 1170 (45.7) | |
| HIV prevalence | 164 (1.0) | 76 (0.9) | 88 (1.1) | 1.5 (df = 1); P = 0.220 |
Of the 17,153 who decided to get an HIV test with Project Accept, 164 (1%) were HIV antibody positive, similar for Thai lowlanders and ethnic minorities (0.9 vs. 1.1%). Overall, 161 (98.1%) of the HIV positive cases received their test result (Table 3), 136 (84.5%) were newly detected cases, more commonly among ethnic minorities compared to Thais (86.4 vs. 78.9%). The majority, 109 (67.7%), had no signs and symptoms of AIDS and were healthy. Ethnic minorities were more often seen to have signs and symptoms of AIDS as compared to Thai lowlanders (35.2 vs. 27.6%), including among those new detected cases (34.2 vs. 25.0%). These comparisons are not statistically significant (see Table 3 for statistics and P value).
Table 3.
HIV/AIDS symptomatic status among 161 HIV infected cases who received HIV results
| Overall cases |
Thai Lowland |
Ethnic minorities |
χ2 (df = 1); P value |
||||
|---|---|---|---|---|---|---|---|
| # | Had signs and symptoms |
# | Had signs and symptoms |
# | Had signs and symptoms |
||
| HIV+ cases | 161 | 52 (32.3) | 76 | 21 (27.6) | 88 | 31 (35.2) | 1.09; P = 0.297 |
| Had no history of HIV test |
91 | 28 (30.7) | 35 | 8 (22.8) | 56 | 20 (35.7) | 1.67; P = 0.196 |
| Had history of HIV test Previous test result |
70 | 24 (34.2) | 41 | 13 (31.7) | 29 | 11 (37.9) | 0.29; P = 0.589 |
| Negative | 34 | 9 (26.5) | 21 | 6 (28.6) | 13 | 3 (23.1) | Fisher’s exact = 1.00 (two tails) |
| Positive | 25 | 11 | 16 | 6 | 9 | 5 | |
| Don’t know | 11 | 4 | 4 | 1 | 7 | 3 | |
| New HIV+ detected cases |
136 | 41 (30.2) | 60 | 15 (25.0) | 76 | 26 (34.2) | 1.35; P = 0.245 |
| % of new case/total HIV+ |
84.5 | 78.9 | 86.4 | 1.58; P = 0.208 | |||
New case definition: Never test for HIV or had history of HIV test and reported negative result or don’t know
Discussion
Of the team experiences in conducting CM, MVCT, and PTSS in the field for over 3 years we have adapted CM strategies to better support promoting VCT uptake. We did not encounter major problems in the initial community approach to MVCT. Stake holders raised some concerned that community members would not come forward to get HIV tested because HIV/AIDS has stigmatization issues associated with it. They thought that the openness of the VCT operations in public venues would scare people away and that community members may be afraid of being labeled as HIV positive or having risk behaviors if they came forward for the test. We have demonstrated that with more knowledge and understanding of the subjects, mobile community-based VCT is a successful avenue to promote VCT. Kawichai et al. [12] and Morin et al. [11] provided surprising results that demonstrate minimal HIV testing stigma, and that stigma is not a factor influencing whether people come forward for HIV testing at mobile VCT units.
The CM strategy of door-to-door solicitation had limited reach as most of the target population was usually at work. Few people attended the initial group sessions, many left during the sessions, and many made excuses to leave to return to their daytime activities or household chores. Even though more persons could be reached with the same staff effort (50/10 staff/hours) compared to daytime CM organized meeting and edutainment, the effort did not yield as many persons.
Day-time CM organized meetings, include joining community leader established meetings could increase the numbers/session compared to door-to-door canvassing, with most attendees being adults. Joining organized meetings created a sense of formality and required taking time from daily work to participate.
The nighttime edutainment required greater staff hours/ eligible participants for VCT. This is expected as running the event required more staff for activities and at least six staff members for each of the three tents for HIV/AIDS education, prevention, and awareness games. The activities also lasted longer than the prior approach. We found that the edutainment approach to CM was more attractive to younger people and generated more attendees/session, most often more than a hundred, sometime reaching 300 if we included those younger than 16 years. This was viewed as a benefit for educating teens and youngsters who may soon be at risk. Young adults also came forward more often for VCT using the edutainment approach. Concurrently providing HIV/AIDS knowledge along with availability of VCT assists decision-making for clients. Often the project young adults (aged 18-25 years old) VCT clients gave reasons for receiving VCT such as the following quotes “I came to cheer on my friend for the Karaoke contest but I am early, my other friends are not here yet. So I am decided to get VCT while waiting”. Or “My intention for coming here is not for VCT at first but to play the games and get a prize. However, I am here anyway and it (VCT) is free, so I decided to get it”. These quotes suggest that these young adults may use of “being early for CM” or “have nothing to do while waiting for playing game” be a reasons for getting VCT to avoid being stigmatized such as labeled to have HIV risk.
Among the ethnic minority communities, particularly those in very remote areas, movies that were related to HIV/AIDS education in their own language were an effective means to educate them about HIV/AIDS. Thevillagers would ask for movies almost every time we visited the villages, although the same movie was often repeated. Discussion would follow after the movies to respond to questions and concerns. We assessed participant’s knowledge of HIV/AIDS after the movie and found that their understanding of the issues were generally correct and accurately demonstrated HIV awareness. However, movies were less attractive to lowland Thais who had easy access to modern technology; however, karaoke singing contests were attractive to them. Lottery tickets for prizes after completing the three core CM activities was also an effective method to encourage individuals to learn about HIV/AIDS and VCT in all ethnic groups.
Mobile VCT was effective for outreach and promoting VCT among hard to reach populations [9, 11, 12] when accompanied with appropriate CM strategies; those who lag behind can also be encouraged. In 574 VCT field days, we tested 17,153 cases (31 cases/day), and identified 136 new infected cases of whom 95 (70%) were had no signs or symptoms of AIDS. This case finding has implications not only for infected individuals but also for the community at large. All identified new cases received comprehensive post-test risk reduction counseling and were offered referral to care and support. Early detection of infection status will help to limit the spread of HIV by those otherwise unaware of their HIV infection. Having large numbers of people in the community (34% lowland Thai and 44% ethnic minorities of persons aged 16 years and over tested with PA-Thai) going through risk reduction counseling and learning their HIV status may also help to limit the spread of the virus, particularly among these low-education communities. In our case, almost 50% of our VCT clients were ethnic minorities of whom 54% had no formal education. A common scenario for young adultsfrom remote areas is to migrate to big cities to seek work, becoming at risk for HIV infection. Knowledge will empower them to prevent themselves from infection which should lead to reducing the further spread of the virus.
There are some limitations to the study. Our results may not generalize to other populations. First, the study was conducted in northern Thailand rural areas and participants voluntarily came forward for VCT. These individuals could be biased to be either the “worried well” or to be at higher risk for HIV infection. However, the information came from a sizable sample where the bias from both groups could be balanced. Second, the data are based on self-reports which are subjected to some bias. Participants may tend to report socially desirable data to the counselors. Risk behaviors may be under-reported, and some low-risk behaviors may be over-reported by participants.
In conclusion, this study suggests that VCT can be successfully promoted in populations with appropriate strategies that fit the local context. Entertainment is of human interest and can be a useful tool for drawing attention to public health issues. Integrated entertainment with HIV/AIDS community mobilization is one strategy recommended to increase HIV/AIDS knowledge in populations which lead to VCT promotion and ultimately to stigma reduction.
Acknowledgments
This research was sponsored by the U.S. National Institute of Mental Health as a cooperative agreement, through contracts U01MH066687 (Johns Hopkins University—David Celentano, PI); U01MH066688 (Medical University of South Carolina—Michael Sweat, PI); U01MH066701 (University of California, Los Angeles—Thomas J. Coates, PI); and U01MH066702 (University of California, San Francisco—Stephen F. Morin, PI). In addition, this work was supported as HPTN Protocol 043 through contracts U01AI068613 (HPTN Network Laboratory—Susan Eshleman, PI); U01AI068617 (SCHARP—Deborah Donnell, PI); and U01AI068619 (HIV Prevention Trials Network—Sten Vermund, PI) of the Division of AIDS of the U.S. National Institute of Allergy and Infectious Diseases; and by the Office of AIDS Research of the U.S. National Institutes of Health. Views expressed are those of the authors, and not necessarily those of sponsoring agencies. We thank the communities that partnered with us in conducting this research, and all study participants for their contributions. We also thank study staff and volunteers at all participating institutions for their work and dedication.
Appendix
NIMH Project Accept Study Group (Voting Steering Committee members are indicated with an asterisk).
Laurie Abler, MPH (University of North Carolina at Chapel Hill), Christopher Bamanyisa, MA, AD (2004–2006) (Muhimbili University of Health and Allied Sciences), Chris Beyrer, MD, MPH (Johns Hopkins University) Adam W. Carrico, PhD (University of California, San Francisco), *David Celentano, ScD, MHS, Principal Investigator (Johns Hopkins University), *Suwat Chariyalertsak, MD, DrPH, Principal Investigator (Chiang Mai University, Research Institute for Health Sciences), *Alfred Chingono, MSc, Principal Investigator (University of Zimbabwe), Lillianne Chovenye, MA (2004–2008) (Muhimbili University of Health and Allied Sciences), *Thomas J. Coates, PhD, Principal Investigator (Chair, Steering Committee) (University of California, Los Angeles), Kathryn Curran, MHS (2007–2009) (Medical University of South Carolina), *Deborah Donnell, PhD (Statistical Center for HIV/AIDS Research & Prevention, Fred Hutchinson Cancer Research Center), Susan Eshleman MD, PhD (Johns Hopkins University), Agnès Fiamma, MIPH (University of California, Los Angeles), Katherine Fritz, PhD, MPH (International Center for Research on Women), Janet Frohlich, Dcur (Human Sciences Research Council), Becky Genberg, MPH (2003–2008) (Johns Hopkins University), *Glenda Gray, MBBCH, FCPaeds(SA), Principal Investigator (University of the Witwatersrand/Chris Hani Baragwanath Hospital), Amy Gregowski, MHS (International Center for Research on Women), Harry Hausler, MD, MPH (2003–2007) (London School of Hygiene and Tropical Medicine), Zdenek Hlavka, PhD (Charles University, Department of Probability and Statistics), Daniel Hlubinka, PhD (Charles University, Department of Probability and Statistics), Nora Margaret Hogan, PsyD (2003–2005) (Muhimbili University of Health and Allied Sciences), Philip Joseph (Human Sciences Research Council), Tendayi Jubenkanda BSs Hons, Registered Nurse, Registered Midwife, MBA (University of Zimbabwe), Salim Abdool Karim, MBChB, PhD (Human Sciences Research Council), Surinda Kawichai, PhD, MSc (Johns Hopkins University, Chiang Mai University, Research Institute for Health Sciences), Sebastian Kevany, MPH (University of California, San Francisco), Gertrude Khumalo-Sakutukwa, MSW, MMS (University of California, San Francisco), G.P. Kilonzo, MD, FRCP, Mmed, MBChB, BA, Co-Principal Investigator (Muhimbili University of Health and Allied Sciences), *Michal Kulich, PhD (Charles University, Department of Probability and Statistics), Oliver Laeyen-decker, MS, MBA (National Institute of Allergy and Infectious Diseases, Johns Hopkins University), Tim Lane, PhD, MPH (University of California, San Francisco), Florence P. Lema, MSc, MPH (Muhimbili University of Health and Allied Sciences), Benjamin Link, MPH, MSW (2003–2005) (Johns Hopkins University), Tserayi Machinda, BSC Admin ACCA, MBA(wip) (2005–2006) (University of Zimbabwe), Suzanne Maman, PhD (University of North Carolina at Chapel Hill), *Jessie Mbwambo, MD, Principal Investigator (Muhimbili University of Health and Allied Sciences), Nuala McGrath, ScD, MSc, BSc (London School of Hygiene and Tropical Medicine), James McIntyre, MBChB, MRCOG,Co-Principal Investigator (University of the Witwaters-rand/Chris Hani Baragwanath Hospital), Joanne Mickalian, MA (2003–2006) (University of California, San Francisco), Precious Modiba, MA(SW) (University of the Witwatersrand/Chris Hani Baragwanath Hospital), Simon Morfit, MPH, BA (2005–2006) (University of California, San Francisco), *Stephen F. Morin, PhD, Principal Investigator (University of California, San Francisco), Khalifa M. Mrumbi, MSc. PhD, Co-Principal Investigator (Muhimbili University of Health and Allied Sciences), Marta I. Mulawa, MHS (Medical University of South Carolina), Oliver Murima, MSc (University of Zimbabwe), Thulani Ngubani, BTh, Hons (Human Sciences Research Council), Audrey Pettifor, PhD, MPH (University of North Carolina at Chapel Hill), Estelle Piwowar-Manning, BS MT(ASCP)SI (Johns Hopkins University), *Linda Richter, PhD, Principal Investigator (Human Sciences Research Council), Gavin Robertson, MEd (University of the Witwatersrand/Chris Hani Baragwanath Hospital), Andrew M. Sadowski (Medical University of South Carolina), Memory Sendah, MSc (2003–2006) (University of Zimbabwe), Basant Singh, PhD, Bsc, Msc (University of Zimbabwe), *Michael Sweat, PhD, Principal Investigator (Medical University of South Carolina), Greg Szekeres (University of California, Los Angeles), Andrew Timbe, Med (University of Zimbabwe), Heidi Van Rooyen, PhD (Human Sciences Research Council), Surasing Visrutaratna, PhD, Co-Principal Investigator (Chiang Mai University, Research Institute for Health Sciences), Godfrey Woelk, PhD, MCOMMH, BSc (University of Zimbabwe), Carla E. Zelaya, PhD, MSc (Johns Hopkins University).
Footnotes
The members of the Project Accept Study Team are given in the appendix.
Contributor Information
Surinda Kawichai, Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA; Research Institute for Health Sciences, Chiang Mai University, 110 Intavaroros Rd. Muang, Chiang Mai 50200, Thailand.
David Celentano, Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA.
Kriengkrai Srithanaviboonchai, Research Institute for Health Sciences, Chiang Mai University, 110 Intavaroros Rd. Muang, Chiang Mai 50200, Thailand.
Monjun Wichajarn, Research Institute for Health Sciences, Chiang Mai University, 110 Intavaroros Rd. Muang, Chiang Mai 50200, Thailand.
Kanokporn Pancharoen, Research Institute for Health Sciences, Chiang Mai University, 110 Intavaroros Rd. Muang, Chiang Mai 50200, Thailand.
Chonlisa Chariyalertsak, Chiang Mai Public Health Office, Thai Ministry of Public Health, Chiang Mai, Thailand.
Surasing Visrutaratana, Chiang Mai Public Health Office, Thai Ministry of Public Health, Chiang Mai, Thailand.
Gertrude Khumalo-Sakutukwa, Department of Medicine, School of Medicine, University of California, San Francisco, San Francisco, CA, USA.
Michael Sweat, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC, USA.
Suwat Chariyalertsak, Research Institute for Health Sciences, Chiang Mai University, 110 Intavaroros Rd. Muang, Chiang Mai 50200, Thailand.
References
- 1.UNAIDS/WHO [Access June 20, 2010];AIDS Epidemic update. 2009 Available at http://data.unaids.org.
- 2.WHO media center [Access June 15, 2010];WHO and UNAIDS issue new guidance on HIV testing and counseling in health facilities. Available at http://www.who.int/mediacenter/news/releases/2007/pr24/en/index.html.
- 3.UNAIDS . UNAIDS Policy on HIV testing and counseling. UNAIDS; Geneva: 1997. [Google Scholar]
- 4.The Voluntary HIV-1 Counseling and Testing Efficacy Study Group Efficacy of voluntary HIV-1 counseling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: a randomized trail. Lancet. 2000;356:103–112. [PubMed] [Google Scholar]
- 5.UNAIDS, WHO . UNAIDS/WHO policy statement on HIV testing. Joint United Nations Program on AIDS and World Health Organization; Geneva: 2004. [Google Scholar]
- 6.WHO and UNAIDS . Guidance on provider initiated HIV testing and counseling in health facilities. WHO; Geneva: 2007. [Google Scholar]
- 7.Project Accept Study group [Accessed June 10, 2010];Project accept: a phase III randomized controlled trial of community mobilization, mobile testing, same-day results, and post-test support for HIV in Sub-Saharan Africa and Thailand. Project protocol. 2007 doi: 10.1371/journal.pone.0149335. version 2.3. Available at http://www.cbvct.med.ucla.edu. [DOI] [PMC free article] [PubMed]
- 8.Khumalo-Sakutukwa G, Morin SF, Fritz K, Charlebois ED, van Rooyen H, Chingono A, et al. Project accept (HPTN 043): a community-based intervention to reduce HIV incidence in populations at risk for HIV in sub-Saharan Africa and Thailand. J Acquir Immune Defic Syndr. 2008;49(4):422–31. doi: 10.1097/QAI.0b013e31818a6cb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sweat M, Morin SF, Celentano DD, et al. [Access May 6, 2011];Community-based intervention to increases HIV testing and case detection in people aged 16-32 years in Tanzania, Zimbabwe, and Thailand (NIMH Project Accept, HPTN 043): a randomised study. doi: 10.1016/S1473-3099(11)70060-3. Available at www.thelancet.com/infection. [DOI] [PMC free article] [PubMed]
- 10.Genberg BL, Kulich M, Kawichai S, Modiba P, Chingono A, Kilonzo GP, et al. HIV risk behaviors in sub-Saharan Africa and Northern Thailand: baseline behavioral data from Project Accept. J Acquir Immune Defic Syndr. 2008;49(3):309–19. doi: 10.1097/QAI.0b013e3181893ed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morin SF, Khumalo-Sakutukwa G, Charlebois ED, Routh J, Fritz K, Lane T, Vaki T, Fiamma A, Coates TJ. Removing barriers to knowing HIV status, same-day mobile HIV testing in Zimbabwe. J Acquir Immune Defic Syndr. 2006;41:218–24. doi: 10.1097/01.qai.0000179455.01068.ab. [DOI] [PubMed] [Google Scholar]
- 12.Kawichai S, Celentano DD, Chariyalertsak S, et al. Community-based voluntary counseling and testing services in rural communities of Chiang Mai Province, northern Thailand. AIDS Behav. 2007;11:770–7. doi: 10.1007/s10461-007-9242-7. [DOI] [PubMed] [Google Scholar]