Abstract
Since therapeutic endoscopic retrograde cholangiopancreatography replaced surgery as the first approach in cases of choledocolithiasis, a plethora of endoscopic techniques and devices appeared in order to facilitate rapid, safe and effective bile duct stones extraction. Nowadays, endoscopic sphincterotomy combined with balloon catheters and/or baskets is the routine endoscopic technique for stone extraction in the great majority of patients. Large common bile duct stones are treated conventionally with mechanical lithotripsy, while the most serious complication of the procedure is “basket and stone impaction” that is predominately resolved surgically. In cases of difficult, impacted, multiple or intrahepatic stones, more sophisticated procedures have been used. Electrohydraulic lithotripsy and laser lithotripsy are performed using conventional mother-baby scope systems, ultra-thin cholangioscopes, thin endoscopes and ultimately using the novel single use, single operator SpyGlass Direct Visualization System, in order to deliver intracorporeal shock wave energy to fragment the targeted stone, with very good outcomes. Recently, large balloon dilation after endoscopic sphincterotomy confirmed its effectiveness in the extraction of large stones in a plethora of trials. When compared with mechanical lithotripsy or with balloon dilation alone, it proved to be superior. Moreover, dilation is an ideal alternative in cases of altered anatomy where access to the papilla is problematic. Endoscopic sphincterotomy followed by large balloon dilation represents the onset of a new era in large bile duct stone extraction and the management of “impaction” because it seems that is an effective, inexpensive, less traumatic, safe and easy method that does not require sophisticated apparatus and can be performed widely by skillful endoscopists. When complete extraction of large stones is unsuccessful, the drainage of the common bile duct is mandatory either for bridging to the final therapy or as a curative therapy for very elderly patients with short life expectancy. Placing of more than one plastic endoprostheses is better while the administration of Ursodiol is ineffective. The great majority of patients with large stones can be treated endoscopically. In cases of unsuccessful stone extraction using balloons, baskets, mechanical lithotripsy, electrohydraulic or laser lithotripsy and large balloon dilation, the patient should be referred for extracorporeal shock wave lithotripsy or a percutaneous approach and finally surgery.
Keywords: Large bile duct stones, Endoscopic sphincterotomy, Papillary balloon dilation, Large papillary balloon dilation, Mechanical lithotripsy, Electrohydraulic lithotripsy, Laser lithotripsy
INTRODUCTION
Bile duct stone management has changed dramatically in the last two decades when open surgery has been replaced by per-oral endoscopic procedures. Nowadays, therapeutic endoscopic retrograde cholangiopancreatography (ERCP) is performed worldwide as the first approach in the management of extrahepatic bile duct stones and is superior to surgical or percutaneous approaches, although it can be challenging in some cases[1]. Endoscopic therapy involves stone extraction using conventional methods after performing endoscopic biliary sphincterotomy. The routine devices used for stone retrieval are balloon catheters, Dormia baskets and mechanical lithotripters. Alternatively, other therapeutic options such as intra or extracorporeal shock wave lithotripsy may offer adjuvant therapy in selected patients or in particularly challenging cases. In the last thirty years, endoscopic biliary sphincterotomy (EST) is considered the established method for bile duct stone extraction and it is well known that the great majority of the stones can be successfully removed by using conventional techniques. However, stone removal can be difficult and unsuccessful in less than 10% of cases, when managing large, barrel-shaped, piston-like, multiple stones, strictured common bile duct (CBD) or in cases of altered anatomy[2].
In this article, we try to approach the large stone issue, reviewing the current literature and searching for alternatives.
LARGE BILE DUCT STONES
The main problem that has to be solved regarding endoscopic extraction of large bile duct stones is extraction of something larger than the orifice through which access has been achieved. This is obtained by either enlarging the ampulla of vater (cutting, dilation) or reducing the size of the stone that has to be extracted (fragmentation, crushing) using adequate devices[3]. The second problem is the size of the stone itself.
It is not clear and there is no consensus in the literature of the definition of “large stone”. Some authors use the term “difficult stone” when referring to a large stone size, although actually “difficult” could mean multiple, intrahepatic, barrel-shaped, impacted stones or the presence of another comorbidity. Stricture below the stone, stenosis of the intrapancreatic CBD or difficult anatomic access to the papilla caused by duodenal diverticuli are conditions which increase the rate of unsuccessful stone retrieval[3]. Overall, only a small number of “difficult stones” are “large stones”[4]. Regardless of the chosen endoscopic procedure, the large stone issue is still a concern due to high failure rates, even for experienced endoscopists.
Many authors define a stone larger than 10-15 mm in diameter as “large”. Others support that a stone with a diameter equal to the CBD diameter is large[3]. Sharma et al[5], in a recent letter to the Editor of the World Journal of Gastroenterology, tried to redefine the “large stone”, analyzing retrospectively three hundred and four patients with CBD calculi. Patients were enrolled in two groups. The first group comprised of patients with a median stone diameter of 15.5 mm and a median lower CBD diameter of 16 mm, while the second group enrolled patients with a median CBD stone diameter of 8 mm and a median lower CBD diameter of 3 mm. In the second group, the stones were not extracted successfully as the size was disproportionate to the lower CBD diameter. Therefore, definition of a large stone should include the lower CBD diameter so that any stone exceeding that should be called “large”, regardless of the stone size.
ENDOSCOPIC SPHINCTEROTOMY: “FIRST STEP ON THE MOON”
In 1974, Kawai et al[6] first described EST, currently considered worldwide as the established method, as the first step for CBD stone clearance. The size of the EST has to be adapted to the CBD and papilla size. Treated with conventional EST followed by conventional balloons and baskets, up to 90% of CBD stones can be extracted. On the other hand, EST alone for the removal of large stones (over 15 mm in diameter) is usually unsuccessful.
Lauri et al[7] reported successful large stone removal in only 12% of cases using EST alone. Sphincterotomy is a technically complex endoscopic procedure used either in cases of surgically altered anatomy or of a small papilla where there is not enough intraluminal room for a safe complete muscular fiber incision. The current, in combination with mechanical damage, may develop well known complications (bleeding, pancreatitis, cholangitis, perforation). As a consequence, limitation of EST to provide successful removal of large CBD stones and the reported complications ranging from 5% to 10%[8] requires alternative endoscopic options in order to overcome these restrictions.
ENDOSCOPIC PAPILLARY BALLOON DILATION
The original attractive concept was to achieve bile duct clearance while maintaining an intact biliary sphincter. As an alternative to EST, in 1982, Staritz et al[9] published the first trial about the possible role of endoscopic papillary balloon dilation (BD) in the management of CBD stones. BD is easily performed with the wire-guided method using a small diameter balloon catheter (usually 8-10 mm), dilating the papilla while intact for 45-60 s prior to EST. Some authors strongly supported that dilating the papilla without cutting it meant that papillary functions are preserved and complication rates decreased when compared to EST[10,11].
A prospective randomized trial from East Asia tried to determine whether a longer duration of dilation (five minutes vs the conventional one minute) can expand the papilla in order to permit stone extraction and reduce the rates of pancreatitis. Compared with the conventional one minute, five minutes of BD seemed to improve the efficacy of stone extraction and reduce the risk of pancreatitis[12].
BD without prior EST became a popular method of stone extraction, mainly in Asia, and many studies tried to compare the two techniques, supporting the safety and effectiveness of BD without EST and reporting low complication and mortality rates at the same time[13-15].
A current East Asian study analyzed large stone removal (mean stone size 16.4 mm) in a large series of patients that underwent BD from 10 mm to 20 mm (mean size of dilating balloon 13.2 mm), with the duration of the dilation ranging from 2 to 6 min. The authors reported a remarkable success rate of 81.8% of complete retrieval within the first session; however, the stone recurrence rate after six months of follow-up was considerable with the minimum of complications[16].
Previously, a Japanese group published a well designed controlled prospective trial enrolling two hundred and eighty-two patients with choledocolithiasis from eleven national institutions. Patients were randomized in an EST group and a BD without prior EST group. The authors compared the two techniques and reported that they are approximately equal regarding successful stone extraction and complication rate, so they suggest BD without prior EST as an alternative option to EST[17].
Studies from Western countries revealed completely opposite results. In a randomized controlled multicenter trial, Disario et al[18] compared primary BD with EST in patients with choledocolithiasis. The reported outcome was that BD was associated with increased short term morbidity, while two deaths were reported due to severe pancreatitis. This study was stopped at the first analysis, suggesting that BD for stone extraction should be avoided in every day clinical practice.
An American group, searching the Cochrane Library, Medline, Embase and reviewing fifteen randomized trials which included one thousand, seven hundred and sixty-eight patients, reported that primary BD is less successful and more risky, presenting higher rates of pancreatitis when compared with EST[19].
Thus, guidelines for the management of CBD stones published in the “Gut” in 2008 suggested that BD should be avoided due to a high risk of severe pancreatitis. With a lot of skepticism, it could be an alternative in a special group of patients with coagulopathy, altered anatomy or the presence of duodenal diverticuli[20].
ENDOSCOPIC SPHINCTEROTOMY FOLLOWED BY LARGE BALLOON DILATION
In the case of large stones, a promising endoscopic technique is EST followed by large balloon dilation (ESLBD). In patients who underwent a prior sphincterotomy, dilation with large balloons to increase the diameter of the distal CBD opening into the duodenal lumen, instead of extending the already existing sphincterotomy, was found to be very safe. Based on this evidence, some endoscopists tried to do it in the same session and it also proved to be very safe. Ersoz et al[21] first reported the use of ESLBD as an alternative technique for the management of difficult bile duct stones with a very good outcome.
Recently, Maydeo and Bhandari[22] reported their analysis regarding ESLBD for large stone extraction, enrolling sixty patients with large CBD stones (stone diameter from 12 mm to 20 mm). They performed “maximum” ESLBD using a controlled radial expansion (CRE) balloon from Boston Scientific (Natick, MA) with a diameter range of 12 mm to 15 mm, inflated gradually up to 15 mm. The procedure with the fully inflated balloon duration lasted 30 s. After performing ESLBD, three attempts of stone removal were made using balloons or Dormia baskets. In the case of failure after the third attempt, they performed ML with an Olympus BML-3Q or a Microvasive Trapezoid lithotriptor. Post-procedure, the stones were extracted in 95% of the patients. In 5% of the patients, ML was required, while the most common complication was bleeding in 8.3% of the cases. The trial supported the idea of ESLBD in cases of large stones as an effective, technically easy and safe technique.
Heo et al[23] also randomized patients with large stones (over 15 mm in diameter) in an ESLBD group (12 mm to 20 mm balloon diameter, dilation time 60 s) and in an EST group. When EST was performed alone, it was completed to its full length (major EST), whereas combined with dilation it stopped after reaching one third of the full length that could be theoretically reached (minor EST). The reported successful stone removal was 94.4% for the ESLBD group and 96.7% for the EST group, while complication rates were similar between the 2 groups (5% vs 7% respectively). Pancreatitis and cholangitis appeared in the same proportion (4% and 1% respectively). ML for stone extraction after failure of the conventional methods was required in 8% of the ESLBD group and in 9% of the EST group. Based on the similar rates of successful stone removal and complications, the analysis suggested ESLBD as an alternative option in large stone endoscopic treatment.
In another series, Minami et al[24] enrolled eighty-eight patients with large (over 12 mm in diameter) and/or multiple stones that underwent EST “with small incision” combined with large dilation using a 20 mm × 5 cm balloon from Boston Scientific (Watertown, MA). Complete stone removal was achieved in 99% of the patients, while the procedure-related complications were bleeding (1%), pancreatitis (1%) and cholangitis (1%). Moreover, the stone extraction procedure was less time consuming compared to EST and BD alone.
In a multi center retrospective trial involving patients with a median stone size of 13 mm, Attasaranya et al[25] evaluated the efficacy and complications of the method. Five ERCP referral centers and one hundred and three patients were enrolled in that analysis from 1999 to 2007. Complete stone removal was accomplished in 95% of the procedures with the first attempt, while ML was required in 27% of the cases due to failure of stone extraction after ESLBD. Procedure-related complications developed in 5.4% of the patients, with one case of severe bleeding and one case of cystic duct perforation reported.
In a retrospective Indian trial, ESLBD was performed in cases of large (up to 25 mm in diameter) or difficult stones that could not be extracted with routine methods. ML was required in 10% of cases, 32% of the patients presented minor self-limiting bleeding, and mild pancreatitis occurred in 8% of them[26].
Draganov et al[27] evaluated the efficacy and safety of ESLBD in patients with difficult stones who had failed stone extraction with standard techniques after full length EST. Successful complete stone removal was achieved in 95% of the patients, while in 84% the stone clearance was accomplished without additional ML. Mild complications occurred in 6% of the cases.
In another retrospective analysis, Itoi et al[28] randomized one hundred and one patients in an ESLBD group and an EST group, comparing outcome, complications, procedural and fluoroscopy time between the two groups. The successful stone removal in the first session was 96% vs 85% respectively, higher for the ESLBD group but not statistically significant. ML was required more often (statistically significant) in the EST group than in the ESLBD group (25% vs 6%). Total procedure time and total fluoroscopy time in the ESLBD group were significantly shorter (32 min vs 40 min and 13 min vs 22 min respectively).
Investigating a large series of patients, a Korean group tried to manage the question of whether a small EST followed by large balloon dilation can reduce the use of ML in patients with large stones. Complete stone removal from the first session was accomplished in 87.5% of the patients in the ESLBD group vs 74% in the EST group. ML for large stones was required in 17.9% for the ESLBD group and 45.8% for the EST group. The study suggested that ESLBD could reduce the need for ML in the case of large stones[29]. A Korean series analyzing patients with large stones reported similar conclusions for both techniques[30].
The majority of published series regarding ESLBD for large stones report a success rate of 83% to 99% using balloons with a diameter of 12 mm to 20 mm, dilating up to 60 s (Table 1). Although there are plenty of trials in the literature on the dilation issue, few of them are well designed, randomized and prospective.
Table 1.
Endoscopic sphincterotomy plus large balloon dilation in the management of large bile duct stones: outcome, complications
| Author | Nr. | Balloon size (mm) | Success rate (%) | Need of ML (%) | Complications (%) |
| Ersoz et al[21] 2003 | 58 | 12-20 | 83 | 7 | 16 |
| Maydeo et al[22] 2007 | 62 | 12-15 | 92 | 5 | 8 |
| Minami et al[24] 2007 | 88 | Up to 20 | 99 | 1 | 6 |
| Heo et al[23] 2007 | 200 | 12-20 | 97 | 8 | 5 |
| Attasaranya et al[25] 2008 | 107 | 12-18 | 95 | 27 | 6 |
| Misra et al[26] 2008 | 55 | 15-20 | 90 | 10 | 8 |
| Kim et al[30] 2009 | 55 | 15-18 | 85 | 33 | None |
| Draganov et al[27] 2009 | 44 | - | 95 | 11 | 6 |
| Kim et al[29] 2011 | 149 | Up to 20 | 87 | 20 | - |
Our group reported a prospective randomized controlled trial, the first in the literature that compared ESLBD with EST followed by ML, in order to evaluate the therapeutic benefits and complications between the two options in the management of large stones. Ninety patients with large CBD stones (diameter from 12 mm to 20 mm) were randomized in ESLBD and ML groups. Both groups of patients underwent a complete EST. ESLBD was performed with a CRE balloon with diameter from 15 mm to 20 mm and the duration of dilation after disappearance of the waist of the balloon was 10-12 s. For the ML group, an Olympus BML 4Q, Lithocrush 201 or 202Q was used in order to fragment large stones. Complete stone clearance was achieved in 97.7% in the ESLBD group, while it was lower (91.1%) in the ML group. Complications were observed in 4.4% in the ESLBD group compared with 20% in ML group. The major complication when ML was performed was cholangitis. In one patient from the ESLBD group, a tiny perforation occurred that was treated conservatively with a stent placement. None of our patients died. Our analysis concluded that the two techniques are similar in effectiveness but ESLBD is followed by fewer complications compared to ML. A significant observation was that in patients from the ESLBD group to whom a plastic stent was placed due to residual stone fragments, the CBD was found to be completely clean during the second ERCP that was done to retrieve the stent. In patients from ML group, residual stone material had to be extracted after stent retrieval in that second ERCP[31].
Khan et al[32], analyzing eighteen retrospective and prospective studies including more than one thousand, three hundred patients, published a systematic review regarding ESLBD for large stones. The stone size was up to 35 mm; the EST performed was reported as “limited” in nine, “moderate” in four and “large” in four studies. The balloon dilation ranged from 10-20 mm in diameter and the maximum dilation time lasted from 20 s to 60 s. Overall, 0-33% of the patients required complementary ML when successful stone removal with the first ERCP was achieved in 72%-97% of the patients. The complications were pancreatitis (0-9.6%), bleeding (0-12%) and perforation (0-1%).
Recently, a Japanese group reported their first experience with a new prototype large diameter balloon-equipped sphincterotome in a small number of patients. The new device is a combination of a dilating balloon and a sphincterotome and was made by the manufacturers apparently because of the tremendous expansion of this new technique among ERCP units worldwide and the potential commercial need for such a device. In this study, bile duct clearance was accomplished in 94% of the patients when ML was required in 22% of them[33].
MECHANICAL LITHOTRIPSY: “THE CLASSIC”
For more than two decades, ML was the unique endoscopic approach for large stone removal after failure of conventional techniques. ML is a relatively inexpensive option and should be available in all ERCP units. The procedure requires capturing the stone within the lithotripter basket into the strong metallic wire mesh, using the same technique as for conventional stone retrieval. After advancement of the sheath onto the basket with the entrapped stone, the handle of the cranking device should be turned slowly in order to reduce the risk of basket break down, to crush the stone and extract it in smaller fragments[34]. The main complication during ML is “basket and stone impaction” that could occur even during a routine stone extraction or in cases of a small diameter stone and is observed in up to 6% of the cases[35,36]. A usual cause of failure is lack of enough space for the basket to open. That makes capturing of the stone unsuccessful.
Two main types of mechanical lithotripters are commercially available: through-the-scope lithotripsy baskets with a reusable cranking handle (integrated device) and another type that is used after removal of the duodenoscope over the basket wires under fluoroscopy (salvage device).
Emergency lithotripsy over the basket is required when the standard basket with the captured stone is impacted. All ERCP units should have the appropriate devices to perform this procedure because the removal of the impacted basket is essential. Although impaction could be managed surgically, nonsurgical endoscopic maneuvers should be attempted by experienced endoscopists in order to avoid it. A comprehensive retrospective study that involved seven American referral centers showed that impaction was resolved by using alternative options like extending prior EST, performing electrohydraulic lithotripsy, by using a per-oral Soehendra lithotripter, performing intracorporeal or extracorporeal lithotripsy, inserting biliary stents and finally surgery. The study concluded that extension of EST and electrohydraulic lithotripsy was the most popular approaches among endoscopists[37].
The most widely used mechanical lithotripters and some of their characteristics are presented in Table 2. ML was first described by Riemann et al[38] in 1982. In 1988, Schneider et al[36] published one of the first studies referring to ML using self-constructed mechanical lithotripters in a large series of two hundred and nine patients with a median stone diameter of 18 mm, while more than 30% of the enrolled patients had stones over 20 mm in diameter. Authors reported successful lithotripsy in 87.6% of the patients but in cases of very large stones (over 25 mm in diameter), successful lithotripsy decreased to 67.6%.
Table 2.
Mechanical lithotripters-basic characteristics
| Device (integrated) | Assemblyrequired | Contrast injection capability | Minimum accessory channel |
| Microvasive Endoscopy, Boston Scientific Corp | |||
| Monolith | No | Yes | 3.2 mm |
| Trapezoid Rx | Yes | Yes | 3.2 mm |
| Alliance II handle | - | - | - |
| Olympus America Corp,LithoCrush V | |||
| BML-3Q | Yes | Yes | 4.2 mm |
| BML-4Q | Yes | No | 3.2 mm |
| BML – 202Q-204Q | Yes | Yes | 4.2 mm |
| BML – V242QR – 30 | Yes | No | 4.2 mm |
| BML – V237QR – 30 | Yes | No | 3.7 mm |
| BML – V232QR – 30 | Yes | No | 3.2 mm |
| BML – V232QR – 26 | Yes | No | 3.2 mm |
| BML – V442QR – 30 | Yes | No | 4.2 mm |
| Xeon medical | |||
| Xemex crusher catheter | - | No | 2.8-3.2 mm |
| (salvage) | |||
| Olympus | |||
| BML – 110A-1 | Yes | No | 3.2-4.2 mm |
| MAJ – 403 (sheath) | Yes | No | Remove scope |
| Cook Endoscopy | |||
| Conquest TTC Lithotriptor Cable | |||
| TTCL – 1 (sheath) | Yes | No | 3.2 mm |
| TTCL – 10 (sheath) | Yes | No | 3.7 mm |
| SLH – 1 | - | - | - |
In a large series that enrolled three hundred and four patients with large stones (over 15 mm in diameter), ML was performed using the Olympus BML-4Q lithotripter. The reported success rate for the first session was 70% and the overall rate of successful stone removal after multiple sessions of ML was 90%. When ML was unsuccessful, patients were referred for surgery. The reported post-procedure complication rates after the first ML session was 3.3% for pancreatitis and 1.4% for cholangitis, while no perforation was reported[39].
Α previous American multi center prospective trial that enrolled one hundred and sixteen patients from nine medical institutions, reported that stones with a size of less than 20 mm were associated with high rate of successful removal (90%-100%), while for very large stones, the success rate ranged from 68% to 83%.
The complication rates for pancreatitis and bleeding were not greater than that occurring after EST[40].
Garg et al[41] reported the Indian experience of ML using an Olympus mechanical lithotripter and an extraendoscopic lithotripter in cases of impaction in order to remove large stones (over 15 mm in diameter). The overall success rate was 79.3%. Biliary drainage by nasobiliary catheter or stent placement was performed in cases of unsuccessful attempts of stone removal and subsequently the patients were referred for surgical intervention. The study concluded that the impaction, size, shape and composition of the stone could represent some valuable predictive factors for unsuccessful ML.
In another series from Italy, the rate of successful removal of very large stones (over 28 mm in diameter) was 68%, while for smaller stones (less than 10 mm in diameter) it was over 90%. Due to low rates of stone removal in patients with very large stones, surgery or other alternative non-surgical procedures such as extracorporeal shock wave lithotripsy or long term biliary stenting could be a better option[42].
A recent study analyzed five hundred and ninety-two patients with choledocholithiasis. Failure to extract difficult or large stones was reported in about 12% of them, while stone impaction happened in 5% of the patients. The stone extraction rate in patients with impaction was 96% and in patients with non-impacted stones it was 97%. The success rate was 96% for stones smaller than 20 mm and 100% for stones more than 20 mm. The procedure was successful in the first session in 81% of the patients while in 19% of them multiple ERCPs were required in order for CBD clearance to be accomplished. Basket impaction occurred in 5.7% of the patients that underwent ML. The impaction was resolved using a second mechanical lithotriptor. Pancreatitis, cholangitis and bleeding rates were lower compared with the non-ML group[43].
ELECTROHYDRAULIC LITHOTRIPSY-LASER LITHOTRIPSY: “THE ALTERNATIVES”
Electrohydraulic lithotripsy (EHL) is a not a widely available technique because it is a second line method of stone therapy. When available, it is used in cases of large stones, in cases of stones above a strictured CBD segment or in cases of stones impacted within the cystic duct, but it can be applied in cases of failure of the conventional techniques. Initially it was used by urologists for the treatment of urinary tract lithiasis. An EHL probe consists of a coaxial bipolar probe and a separate charge unit. A shock wave is generated and an electric spark created, causing an explosive formation of plasma channel and vaporization of the water surrounding the electrode. Continuous saline irrigation is required to provide a media for shock wave energy transmission, to ensure visualization and to clear the debris. Therefore, a nasobiliary catheter is sometimes necessary to irrigate alongside the probe. EHL is usually performed under direct cholangioscopy with the aid of an EHL probe that is inserted in the common bile duct through the working channel of a cholangioscope. The best option is for the procedure to be performed under direct cholangioscopy in order to avoid application of shock waves directly on the duct wall, causing bleeding or perforation.
When direct cholangioscopic control is not available, an EHL probe can be inserted through a modified balloon catheter that centers the probe onto the stone under fluoroscopic guidance. The tip of the EHL probe looks directly at the stone and is positioned 5 mm from the tip of the scope and 1-2 mm from the stone[44]. Shock waves can be delivered in brief pulses that range from a single discharge to continuous discharging by a foot switch device according to manufacturers’ recommendations, until the stone is fragmented[45].
In a retrospective multicenter Canadian study, efficacy and safety of EHL was assessed in ninety-four patients with difficult stones, eighty-one of them presenting with large ones (over 20 mm in diameter) referred for endoscopic therapy. EHL was performed under direct cholangioscopy using a “mother-baby” system with the Nortech probe and a Northgate SD-100 generator. Overall, successful stone fragmentation was achieved in 96% of the patients. In 66% of the patients, the fragmentation was complete while in 30% it was partial. The great majority of the patients required one session only for successful stone fragmentation while a small amount of patients underwent additional ML or Extracorporeal Shock Wave Lithotripsy (ESWL). Overall, 18% of the patients presented with post-procedural complications, the most common being recurrent jaundice and/or cholangitis. Rare complications were hemobilia and pancreatitis, while one patient developed a biliary leak that was resolved with stent placement[46].
The currently available mother-baby cholangioscopes are not widely used nowadays due to several disadvantages (high cost, requirement of two skillful endoscopists, difficult maneuverability and fragility, as a baby scope can be easily damaged at the level of the duodenoscope elevator). However, several new choledocoscopes offer therapeutic options for interventions for large stones. One of the novel ultra-slim choledocoscopes with a 2 mm working channel dedicated to EHL and laser lithotripsy is under research. One of the limitations of the ultra slim cholangioscopes is that direct insertion through the ampulla is technically difficult and not always successful[47,48].
SpyGlass Direct Visualization System (DVS) (Boston Scientific, Natick, MA) is a new tool that enables direct examination of bile ducts, optically-guided tissue sampling and therapeutic interventions. It is a novel single-operator endoscope. The system uses the SpyScope, a 10Fr single-use catheter-cholangioscope that offers four-way maneuverability, one channel for an optical probe and separate irrigation channels and one working channel that permits direct biopsy and EHL or Holmium Laser probes to pass through into the bile ducts. It is reported that is a safe and effective method of lithotripsy for large stone fragmentation[49].
Chen and Pleskow[50] first published the initial experience, evaluating the use of SpyGlass DVS for diagnostic and therapeutic reasons. They reported EHL in a few cases with very good results.
Recently it has been reported that complete stone therapy was achieved in 68% of patients with difficult stones, while the complication rate was comparable to that of conventional ERCP, with cholangitis being the most common adverse event[51].
An American group performed SpyGlass and EHL in twenty-six patients with large CBD stones. EHL was used in thirty-eight patients, while in five cases the probe could not be advanced up to the tip of the SpyScope and in seven cases it could not target the stone. However, it is reported that EHL was effective and most of the patients did not require complementary sessions of therapy[52].
Laser lithotripsy (LL) works with the same principle as EHL and the two methods share the same indications. LL focuses a laser light of a high power density onto the stone and a plasma of a gaseous collection of ions and free electrons is created. This plasma bubble induces cavitation with tensile and compressive waves that conduces stone fragmentation. The laser light wavelength is in the near-infrared spectrum and delivers high energy pulses of about 500 to 1000 mJ[53]. The procedure is usually performed under direct visualization of the stone. The ideal procedure is performed under direct visualization of the stone in order to prevent ductal trauma or perforation. However, when direct cholangioscopy is not available, the LL fiber probe can be inserted through centering balloons under fluoroscopic guidance. The LL units are portable and smaller than a classic endoscope processor tower. The main LL systems are the Holmium:YAG and the frequency-double pulse neodymium:YAG (FREDDY). Subsequently, other “smart” lasers have been designed in order to limit ductal injury, recognizing the difference between soft tissue and stone. Flashlamp Pulse Dye Laser uses Coumarin dye to produce selectively absorbable pigments by 504 nm light. Another system uses Rhodamine 6G dye in order to create a 595 nm wavelength that delivers energy strictly to the targeted stone[54].
The LL probe passes through the working channel of several choledocoscopes. The classic “mother-baby” endoscopic system, the newer ultra-slim upper endoscopes (nasal endoscopes with a 4.9-5 mm diameter and a working channel of 2 mm) and ultimately the SpyGlass DVS are compatible with laser fiber probes.
The disadvantages of LL could be the multiple sessions that are usually required, the fragility of the probe, the expensive equipment and the requirement of two skillful endoscopists.
More than two hundred patients were enrolled in an analysis of the effective fragmentation of difficult stones with pulsed Dye Laser. In 92% of the patients, the procedure was successful and in the majority fragmentation was achieved in one session[55]. Complications of LL include bleeding and cholangitis and are reported in 7% of the patients[56].
Compared with LL, the stone fragments resulting after EHL are usually larger and occasionally have sharp edges. The main advantage of the LL compared with EHL is that the ultra thin laser probe can be inserted through working channels of mini scopes or 5Fr catheters. Both techniques have been reported to be safe and effective[57,58] but they are not widely used in every day clinical practice.
In a recent prospective international cohort from fifteen centers in Europe and the United States, authors evaluated the efficacy and safety of SpyGlass DVS in the treatment of large or difficult stones by performing EHL and LL. All patients had one month of follow-up after cholangioscopy. The mean diameter of the largest stone was 18 mm and in 63% of cases, the stones were impacted. EHL and LL was performed in 69% and conventional methods in 31% of cases. The reported procedural success for the EHL and LL group was 91% and 93% in the conventional group. The adverse events were minimum and resolved without sequel[59].
BILE DUCT STONE DISSOLUTION
Stone dissolution was investigated in the 1980s as an alternative option in elderly patients with co-morbidities, in poor candidates for stone extraction or in cases of failure of stone clearance with other traumatic techniques. We refer herein to the dissolution option, although it does not represent an endoscopic technique of large stone extraction because the placement of a nasobiliary tube via ERCP is required. The tip of the nasobiliary catheter has to be placed above the stone in order to provide continuous infusion of adequate chemical agents. Several dissolution agents have been proposed but no particular agent has shown its efficacy. Mono-octanoin with an infusion rate of 3-5lt/h is the most studied agent. It is reported that it can dissolve cholesterol stones “in vitro” and “in vivo”. With Methyl tert-butyl ether (MTBE), there is less experience and data for bile duct stones is limited, while EDTA/bile acid solution can dissolve calcium-containing stones. Dissolution agents rarely lead to complete stone disappearance, even although they can shorten and change the stone form, volume and consistency in order to be extracted by routine techniques[60]. The results of these particular studies were disappointing, with low success rates. Data regarding the use of Mono-octanoin infusion for 4-7 d in a large series of patients indicated complete or partial stone dissolution in 46% of patients, with the major side effect of diarrhea[61]. MTBE in a limited number of patients had a poor outcome and caused side effects such as duodenitis and altered hepatic biochemistry[62].
Therefore, the dissolution option is a rather abandoned method of CBD stone clearance with no application in every day clinical practice.
ENDOPROSTHESES: “ALWAYS DRAIN”
Biliary endoprosthesis (stenting) has been proposed as an alternative for bridging or curative therapy, in the elderly or in cases of co-morbidities in patients who are unlikely to tolerate prolonged endoscopic attempts or surgery[63]. In every day clinical practice, biliary stenting is required on a temporary basis in cases of large, difficult to retrieve stones in order to establish continuous bile drainage, to “keep the route open”, to prevent stone enlargement or impaction and, finally, to avoid complete ductal occlusion. The proximal end of the stent has to be placed above the stone and the distal end protrudes through the papilla into the duodenum. Usually 7Fr double pig-tail polyethylene stents are used, while 10-11.5Fr straight stents are usually preferred in cases of large stones associated with CBD stricture. Routine replacement is not required since it appears to obstruct the stent and cause cholangitis[34]. Stent insertion usually is safe and easy, although can be challenging in cases of stenosis of the distal CBD or in altered anatomy where there is no straight access to the papilla.
Some authors support that after biliary stenting for 3-6 mo, some large stones disappear and some other decrease in size or may fragment. That could be an effective adjuvant method to clear large or difficult stones[64].
Jain et al[65], in a prospective trial, studied patients with large or difficult to extract stones after the placement of a 7Fr pig-tail stent, repeating ERCP after six months. In 20% of the patients, the stones fragmented spontaneously and the stone clearance was achieved with balloon, while in 35% of patients, the duct was found without stones.
Hong et al[66], in a recent trial, reported that EST plus biliary stent placement without performing stone extraction as primary therapy in the treatment of large or multiple stones is a safe and effective method. Following the patients for a median of 120 d after the stent placement, the mean CBD diameter and the stone diameter decreased significantly since pancreatitis occurred in 1.9%. Although it is not sufficiently studied thus far, the procedure when performed using one plastic stent is associated with high rates of stent occlusion and cholangitis within the first 6-36 mo[67,68]. Therefore, multiple double pig-tail stents seem to contribute to a reduction in stone size, especially in cases of large CBD diameter[69].
In another Japanese series, patients with large and/or multiple stones had placement of a 7Fr double pig-tail plastic stent without stone extraction at the initial ERCP. Two months later in the follow-up ERCP, it was seen that larger stones decreased and smaller ones disappeared; however, complication rates after the second ERCP were 13% for cholangitis and 5% for pancreatitis[70].
ALTERED ANATOMY: “THE CHALLENGE”
Therapeutic ERCP for large stone extraction in patients with Billroth II gastrectomy, Roux-en-Y reconstruction or Mirizzi syndrome is very challenging and in some cases unsuccessful.
Namely, for the Billroth II anastomosis, the crucial part of the procedure is to reach the papilla positioned in the afferent loop. Another problem is what type of endoscope to chose. According to patient’s anatomy status, availability and group experience, side-viewing, forward-viewing, single/double balloon or spiral endoscopes can be used.
In most of Billroth II patients, the papilla can be easily found in the afferent loop by side-viewing regular duodenoscopes, but in patients with Roux-en-Y it is really difficult and time-consuming[63]. Many endoscopists prefer to use forward-viewing endoscopes in patients with a prior surgery[71]. The main disadvantage of the forward-viewing scopes is the lack of elevator that makes cannulation of an intact papilla difficult as advanced maneuvers are limited due to lack of steerability. Moreover, the working channels of the conventional forward-viewing endoscopes do not permit the use of ML.
EST in patients who underwent gastrectomy is more challenging and difficult. The most popular sphincterotomy technique in Billroth II gastrectomy is cutting with a needle-knife over a plastic stent that has been placed beforehand for this reason and is removed immediately after the completion of the sphincterotomy[72].
Although EST or ESLBD have been performed for removal of bile duct stones in patients with Billroth II gastrectomy, the reported results are not completely satisfactory. In a recent trial, a Korean group performed stone extraction after limited EST followed by dilation up to 15 mm. ML was required in 11.5% of the cases, while in all cases stones were successfully removed in a maximum of three consecutive sessions without significant complications (bleeding, pancreatitis or perforation). The authors consider ESLBD as an effective and safe method of stone removal in patients with Billroth II gastrectomy[73].
Similar outcomes were reported in a Japanese study. The median stone diameter was 13.5 mm, while in 18% of the cases, complementary ML was needed with no serious complications[74].
BD without a prior EST has also been investigated as an easy method with a theoretically lower risk of bleeding. However, the technique showed limited outcomes because dilating the opening of the biliary sphincter up to 10 mm is not large enough to provide stone extraction, especially in cases of large stones[75].
Mirizzi syndrome (MS) is a serious complication of gallstone disease. Open surgery remains the classic therapy, while a laparoscopic approach is contraindicated in selected patients due to increased rates of mortality[76]. MS is defined as a chronic extrinsic compression of the common hepatic duct due to cholecystitis and large or impacted gallstones in Hartman’s pouch with or without formation of a fistula. It seems that capturing large stones in the common hepatic duct with conventional baskets is difficult. Thus, intracorporeal shock wave techniques for stone fragmentation are needed in order to provide stone bile duct clearance[63].
Per-oral cholangioscopy-guided lithotripsy has been successfully performed in patients with Mirizzi syndrome[77].
In an older large series of patients who underwent endoscopic therapy for Mirizzi syndrome using ML, long-term stenting and extracorporeal shock wave lithotripsy, stone clearance was achieved in 56% of the patients[78].
CONCLUSION
Endoscopic extraction of large stones can be problematic, even for experienced endoscopists in selected cases. In such cases, after failure to provide stone therapy with conventional balloons and baskets, the ERCP team has to choose a “Plan B” that has to be effective, not time-consuming and less damaging for the patient’s biliary tree.
The reports regarding ESLBD are promising because it seems to be a safe and effective alternative technique for large stone therapy. A prior competent sphincterotomy is the first step before large balloon dilation and it is an absolute requirement since many authors reported lower complication rates when compared with dilation alone. Moreover, it could be an effective alternative option in cases of “basket and stone impaction”. We believe that the effectiveness of this technique to extract biliary stones is attributed, not only to the radial dilation, but to the straightening of the distal CBD as well, thus the term “sphincteroplasty” is more appropriate and precise.
To date, there are many trials supporting ESLBD but it has not yet become a part of the everyday practice in ERCP units worldwide. More comparative studies with bigger numbers of patients are probably needed. Katsinelos et al, in a letter to the Editor of Endoscopy in 2008, approached the stone impaction issue under the prism of dilation when strategies in case of impaction were the use of a salvage mechanical lithotripter, EHL, LL and a percutaneous or surgical approach.
One of the limitations of ESLBD is the lack of a completely established technique yet. The usual queries are whether we perform “limited” or “maximum” ESΤ, how long we dilate and what balloon size is required. Especially in case of periampullary diverticulum, altered anatomy (Billroth II gastrectomy) or small papilla, our impression is that “minor” EST should be performed prior to large balloon dilation due to lower rates of bleeding and perforation. That hypothesis has to be proved by randomized, comparative, well-designed trials.
The duration of the dilation ranges in some trials from 10 s to 60 s to 2 min to 6 min. Our opinion from our analysis is “less dilation time, lower complication rates”[31]. Keeping the balloon inflated for a longer time (60 s) is common practice when dilating bile duct strictures of fibrotic nature[79]. However, in the setting of post-EST dilation where we are dilating a dissected sphincter and not a fibrotic tissue, theoretically a prolonged dilation time should not be needed and probably would provoke side effects.
Regarding the size of the dilating balloon, it has to be proportionate to the CBD and stone diameter and potential comorbidity has to be considered.
In an animal experiment, researchers studied the histological consequence of ESLBD that was performed using balloons up to 15 mm and up to 20 mm in porcine specimens and tissue sections were assessed for morphological changes. Macroscopic disruption and perforation of the ductal wall increased proportionally to the balloon diameter. Thus, large balloon dilation caused a potential impairment of sphincter function[80].
Primary BD remains unpopular in Western countries[3,19] and is not a routine technique worldwide. David Carr-Locke believes that, for unclear reasons, there are considerable differences in the post-procedure complications comparing ESLBD and BD among East and West. In China, Korea or Japan, primary BD of the papilla for the removal of stones has success and complication rates similar to those of EST, with the exception of bleeding, although there is an increased need for ML[4,81]. When balloon dilation is performed in the West, it presents a high risk of pancreatitis that makes it rather an abandoned technique in everyday clinical practice.
Pancreatitis resulting after BD alone could be explained theoretically by the edematous change of the papilla due to forced sphincter rupture, trauma and finally, the resulting obstruction of the pancreatic duct that discharges the inflammatory cascade leading to acute inflammation of the pancreas. The risk of pancreatitis after ESLBD is less than after BD alone, probably because after EST, the mechanical trauma caused by balloon expansion is directed predominantly towards the biliary part of the sphincter that is already dissected than towards the pancreatic duct[82].
The majority of endoscopists remove conventionally large stones by performing EST followed by ML. To date, there are no trials in the literature analyzing the efficacy of ESLBD after failure of ML to provide large CBD stone retrieval. However, ML is an established but quite challenging technique[83,84], since capturing the stone inside the lithotripter is difficult, time consuming and traumatic. ML seems to be effective in very large stones (over 20-25 mm in diameter). Thus, very large stones should be treated with ML by default, since balloon dilators of a diameter greater than 20 mm are not commercially available.
In cases of failure, we have to think about alternative non-operable options. LL or EHL could be the ideal alternative for elderly patients with an increased surgical risk.
EHL and LL yield similar success rates and may be used complementarily in referral centers. LL using smart laser systems that recognize the stone and protect the ductal tissue seems to be the best option. Dye Laser and the FREDDY system can simplify the large stone fragmentation whereas EHL is rarely used nowadays because of its higher potential of complications (bleeding, perforation)[53]. On the other hand, EHL under direct cholangioscopy or under fluoroscopy presents high rates of successful clearance in large stones (over 90%) when performed by skilled endoscopists. Smaller cohorts reported similar outcomes for EHL, reporting stone fragmentation rates ranging from 77%-100%[4,85,86].
In conclusion, ESLBD could be used as the first line therapy when balloons and baskets are unable to provide stone therapy and before ML[31], with an acceptable complication profile and good outcome[32]. Its role in patients with coagulopathy or other risks for bleeding remains to be evaluated[25,26,30,31,87]. When the stone diameter exceeds 20 mm, the most convenient technique seems to be ML. Alternatively, intracorporeal lithotripsy techniques should be attempted locally if expertise is available or in a referral center[2,20].
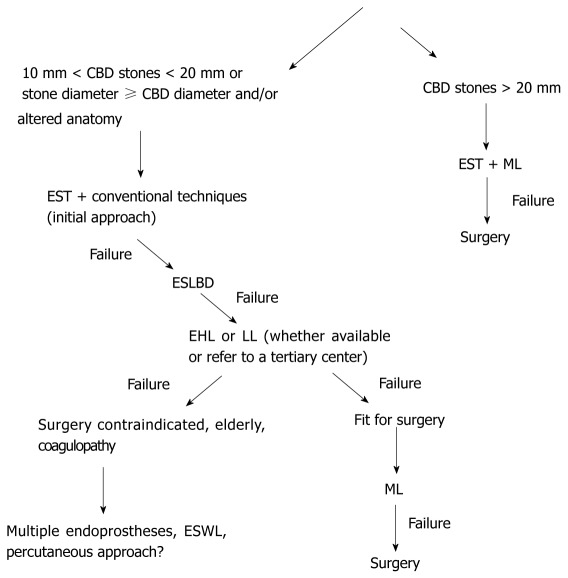
Biliary stenting is a short-term therapy, gaining some time since a permanent treatment is applied. In contrast, stenting as a long-term therapy can be accepted only in cases of very elderly patients with limited life expectancy as it represents the most conservative option[20]. Schematically, a management model or a strategy for endoscopic extraction of large bile duct stones is proposed in Figure 1. However, the availability of each method, the cost-effectiveness, the experience of the team, the appraisal of comorbidities and probably the patient’s preference should be considered.
Figure 1.
Strategy for endoscopic extraction of large bile duct stones. CBD: Common bile duct; EST: Endoscopic biliary sphincterotomy; ESLBD: Endoscopic sphincterotomy plus large balloon dilation; EHL: Electrohydraulic lithotripsy; ESWL: Extracorporeal Shock Wave Lithotripsy.
By using all these alternatives, almost all patients with large stones could be treated endoscopically. In cases of failure despite using advanced technology, the patient should be referred for extracorporeal shock wave lithotripsy or a percutaneous approach or surgery. The advantages and disadvantages of the therapeutic options need to be discussed with the patient and his family in order to proceed with the appropriate therapeutic option for the best outcome.
Footnotes
Peer reviewer: Hirokazu Takahashi, MD, PhD, Assistant Professor, Gastroenterology Division, Yokohama City University Graduate School of Medicine, 3-9 Fuku-ura, Kanazawa-ku, Yokohama 236-0004, Japan
S- Editor Yang XC L- Editor Roemmele A E- Editor Yang XC
References
- 1.Yoo KS, Lehman GA. Endoscopic management of biliary ductal stones. Gastroenterol Clin North Am. 2010;39:209–27, viii. doi: 10.1016/j.gtc.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 2.McHenry L, Lehman G. Difficult bile duct stones. Curr Treat Options Gastroenterol. 2006;9:123–132. doi: 10.1007/s11938-006-0031-6. [DOI] [PubMed] [Google Scholar]
- 3.Carr-Locke DL. Difficult bile-duct stones: cut, dilate, or both? Gastrointest Endosc. 2008;67:1053–1055. doi: 10.1016/j.gie.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Binmoeller KF, Brückner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy. 1993;25:201–206. doi: 10.1055/s-2007-1010293. [DOI] [PubMed] [Google Scholar]
- 5.Sharma SS, Jain P. Should we redefine large common bile duct stone? World J Gastroenterol. 2008;14:651–652. doi: 10.3748/wjg.14.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148–151. doi: 10.1016/s0016-5107(74)73914-1. [DOI] [PubMed] [Google Scholar]
- 7.Lauri A, Horton RC, Davidson BR, Burroughs AK, Dooley JS. Endoscopic extraction of bile duct stones: management related to stone size. Gut. 1993;34:1718–1721. doi: 10.1136/gut.34.12.1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheth SG, Howell DA. What are really the true late complications of endoscopic biliary sphincterotomy? Am J Gastroenterol. 2002;97:2699–2701. doi: 10.1111/j.1572-0241.2002.07051.x. [DOI] [PubMed] [Google Scholar]
- 9.Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilatation, a possible alternative to endoscopic papillotomy. Lancet. 1982;1:1306–1307. doi: 10.1016/s0140-6736(82)92873-2. [DOI] [PubMed] [Google Scholar]
- 10.Komatsu Y, Kawabe T, Toda N, Ohashi M, Isayama M, Tateishi K, Sato S, Koike Y, Yamagata M, Tada M, et al. Endoscopic papillary balloon dilation for the management of common bile duct stones: experience of 226 cases. Endoscopy. 1998;30:12–17. doi: 10.1055/s-2007-993721. [DOI] [PubMed] [Google Scholar]
- 11.Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468–474. doi: 10.1016/s0016-5107(95)70052-8. [DOI] [PubMed] [Google Scholar]
- 12.Liao WC, Lee CT, Chang CY, Leung JW, Chen JH, Tsai MC, Lin JT, Wu MS, Wang HP. Randomized trial of 1-minute versus 5-minute endoscopic balloon dilation for extraction of bile duct stones. Gastrointest Endosc. 2010;72:1154–1162. doi: 10.1016/j.gie.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Minami A, Nakatsu T, Uchida N, Hirabayashi S, Fukuma H, Morshed SA, Nishioka M. Papillary dilation vs sphincterotomy in endoscopic removal of bile duct stones. A randomized trial with manometric function. Dig Dis Sci. 1995;40:2550–2554. doi: 10.1007/BF02220440. [DOI] [PubMed] [Google Scholar]
- 14.Ochi Y, Mukawa K, Kiyosawa K, Akamatsu T. Comparing the treatment outcomes of endoscopic papillary dilation and endoscopic sphincterotomy for removal of bile duct stones. J Gastroenterol Hepatol. 1999;14:90–96. doi: 10.1046/j.1440-1746.1999.01798.x. [DOI] [PubMed] [Google Scholar]
- 15.Arnold JC, Benz C, Martin WR, Adamek HE, Riemann JF. Endoscopic papillary balloon dilation vs. sphincterotomy for removal of common bile duct stones: a prospective randomized pilot study. Endoscopy. 2001;33:563–567. doi: 10.1055/s-2001-15307. [DOI] [PubMed] [Google Scholar]
- 16.Chan HH, Lai KH, Lin CK, Tsai WL, Wang EM, Hsu PI, Chen WC, Yu HC, Wang HM, Tsay FW, et al. Endoscopic papillary large balloon dilation alone without sphincterotomy for the treatment of large common bile duct stones. BMC Gastroenterol. 2011;11:69. doi: 10.1186/1471-230X-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fujita N, Maguchi H, Komatsu Y, Yasuda I, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K, et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: A prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151–155. doi: 10.1067/mge.2003.56. [DOI] [PubMed] [Google Scholar]
- 18.Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–1299. doi: 10.1053/j.gastro.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 19.Weinberg BM, Shindy W, Lo S. Endoscopic balloon sphincter dilation (sphincteroplasty) versus sphincterotomy for common bile duct stones. Cochrane Database Syst Rev. 2006;18:CD004890. doi: 10.1002/14651858.CD004890.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the management of common bile duct stones (CBDS) Gut. 2008;57:1004–1021. doi: 10.1136/gut.2007.121657. [DOI] [PubMed] [Google Scholar]
- 21.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 22.Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958–961. doi: 10.1055/s-2007-966784. [DOI] [PubMed] [Google Scholar]
- 23.Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–76; quiz 768, 771. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 24.Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179–2182. doi: 10.3748/wjg.v13.i15.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, Ajmere N, Ste Marie RW, Bhattacharya K, Gupta K, et al. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67:1046–1052. doi: 10.1016/j.gie.2007.08.047. [DOI] [PubMed] [Google Scholar]
- 26.Misra SP, Dwivedi M. Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy. 2008;40:209–213. doi: 10.1055/s-2007-967040. [DOI] [PubMed] [Google Scholar]
- 27.Draganov PV, Evans W, Fazel A, Forsmark CE. Large size balloon dilation of the ampulla after biliary sphincterotomy can facilitate endoscopic extraction of difficult bile duct stones. J Clin Gastroenterol. 2009;43:782–786. doi: 10.1097/MCG.0b013e31818f50a2. [DOI] [PubMed] [Google Scholar]
- 28.Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560–565. doi: 10.1038/ajg.2008.67. [DOI] [PubMed] [Google Scholar]
- 29.Kim TH, Oh HJ, Lee JY, Sohn YW. Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg Endosc. 2011;25:3330–3337. doi: 10.1007/s00464-011-1720-3. [DOI] [PubMed] [Google Scholar]
- 30.Kim HG, Cheon YK, Cho YD, Moon JH, Park do H, Lee TH, Choi HJ, Park SH, Lee JS, Lee MS. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15:4298–4304. doi: 10.3748/wjg.15.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M, et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278–285. doi: 10.1038/ajg.2010.421. [DOI] [PubMed] [Google Scholar]
- 32.Khan AS, Tiwari P, Nass JP, Romero RV, Rivera RE, Antillon M. R, Roy PK. Large balloon dilation with sphincterotomy for large bile duct stones: a systematic review. Gastrointest Endosc. 2011;73:193. [Google Scholar]
- 33.Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. New large-diameter balloon-equipped sphincterotome for removal of large bile duct stones (with videos) Gastrointest Endosc. 2010;72:825–830. doi: 10.1016/j.gie.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 34.Neuhaus H. Endoscopic and percutaneous treatment of difficult bile duct stones. Endoscopy. 2003;35:S31–S34. doi: 10.1055/s-2003-41534. [DOI] [PubMed] [Google Scholar]
- 35.Sauter G, Sackmann M, Holl J, Pauletzki J, Sauerbruch T, Paumgartner G. Dormia baskets impacted in the bile duct: release by extracorporeal shock-wave lithotripsy. Endoscopy. 1995;27:384–387. doi: 10.1055/s-2007-1005718. [DOI] [PubMed] [Google Scholar]
- 36.Schneider MU, Matek W, Bauer R, Domschke W. Mechanical lithotripsy of bile duct stones in 209 patients--effect of technical advances. Endoscopy. 1988;20:248–253. doi: 10.1055/s-2007-1018186. [DOI] [PubMed] [Google Scholar]
- 37.Thomas M, Howell DA, Carr-Locke D, Mel Wilcox C, Chak A, Raijman I, Watkins JL, Schmalz MJ, Geenen JE, Catalano MF. Mechanical lithotripsy of pancreatic and biliary stones: complications and available treatment options collected from expert centers. Am J Gastroenterol. 2007;102:1896–1902. doi: 10.1111/j.1572-0241.2007.01350.x. [DOI] [PubMed] [Google Scholar]
- 38.Riemann JF, Seuberth K, Demling L. Clinical application of a new mechanical lithotripter for smashing common bile duct stones. Endoscopy. 1982;14:226–230. doi: 10.1055/s-2007-1021626. [DOI] [PubMed] [Google Scholar]
- 39.Chang WH, Chu CH, Wang TE, Chen MJ, Lin CC. Outcome of simple use of mechanical lithotripsy of difficult common bile duct stones. World J Gastroenterol. 2005;11:593–596. doi: 10.3748/wjg.v11.i4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shaw MJ, Mackie RD, Moore JP, Dorsher PJ, Freeman ML, Meier PB, Potter T, Hutton SW, Vennes JA. Results of a multicenter trial using a mechanical lithotripter for the treatment of large bile duct stones. Am J Gastroenterol. 1993;88:730–733. [PubMed] [Google Scholar]
- 41.Garg PK, Tandon RK, Ahuja V, Makharia GK, Batra Y. Predictors of unsuccessful mechanical lithotripsy and endoscopic clearance of large bile duct stones. Gastrointest Endosc. 2004;59:601–605. doi: 10.1016/s0016-5107(04)00295-0. [DOI] [PubMed] [Google Scholar]
- 42.Cipolletta L, Costamagna G, Bianco MA, Rotondano G, Piscopo R, Mutignani M, Marmo R. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84:1407–1409. [PubMed] [Google Scholar]
- 43.Akcakaya A, Ozkan OV, Bas G, Karakelleoglu A, Kocaman O, Okan I, Sahin M. Mechanical lithotripsy and/or stenting in management of difficult common bile duct stones. Hepatobiliary Pancreat Dis Int. 2009;8:524–528. [PubMed] [Google Scholar]
- 44.Moon JH, Cha SW, Ryu CB, Kim YS, Hong SJ, Cheon YK, Cho YD, Kim YS, Lee JS, Lee MS, et al. Endoscopic treatment of retained bile-duct stones by using a balloon catheter for electrohydraulic lithotripsy without cholangioscopy. Gastrointest Endosc. 2004;60:562–566. doi: 10.1016/s0016-5107(04)02012-7. [DOI] [PubMed] [Google Scholar]
- 45.Blind PJ, Lundmark M. Management of bile duct stones: lithotripsy by laser, electrohydraulic, and ultrasonic techniques. Report of a series and clinical review. Eur J Surg. 1998;164:403–409. doi: 10.1080/110241598750004201. [DOI] [PubMed] [Google Scholar]
- 46.Arya N, Nelles SE, Haber GB, Kim YI, Kortan PK. Electrohydraulic lithotripsy in 111 patients: a safe and effective therapy for difficult bile duct stones. Am J Gastroenterol. 2004;99:2330–2334. doi: 10.1111/j.1572-0241.2004.40251.x. [DOI] [PubMed] [Google Scholar]
- 47.Moon JH, Choi HJ, Ko BM. Therapeutic role of direct peroral cholangioscopy using an ultra-slim upper endoscope. J Hepatobiliary Pancreat Sci. 2011;18:350–356. doi: 10.1007/s00534-010-0353-6. [DOI] [PubMed] [Google Scholar]
- 48.Moon JH, Ko BM, Choi HJ, Koo HC, Hong SJ, Cheon YK, Cho YD, Lee MS, Shim CS. Direct peroral cholangioscopy using an ultra-slim upper endoscope for the treatment of retained bile duct stones. Am J Gastroenterol. 2009;104:2729–2733. doi: 10.1038/ajg.2009.435. [DOI] [PubMed] [Google Scholar]
- 49.Seelhoff A, Schumacher B, Neuhaus H. Single operator peroral cholangioscopic guided therapy of bile duct stones. J Hepatobiliary Pancreat Sci. 2011;18:346–349. doi: 10.1007/s00534-010-0360-7. [DOI] [PubMed] [Google Scholar]
- 50.Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video) Gastrointest Endosc. 2007;65:832–841. doi: 10.1016/j.gie.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 51.Kalaitzakis E, Webster G, Vlavianos P, Burnham R, Kallis Y, Hatfield A, Aljabiri R, Westaby D, Sturgess R. Diagnostic and therapeutic utility of spyglass peroral cholangioscopy for indeterminate biliary lesions and bile duct stones. Gut. 2011;60:191–192. doi: 10.1097/MEG.0b013e3283526fa1. [DOI] [PubMed] [Google Scholar]
- 52.Fishman DS, Tarnasky PR, Patel SN, Raijman I. Management of pancreaticobiliary disease using a new intra-ductal endoscope: the Texas experience. World J Gastroenterol. 2009;15:1353–1358. doi: 10.3748/wjg.15.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hochberger J, Tex S, Maiss J, Hahn EG. Management of difficult common bile duct stones. Gastrointest Endosc Clin N Am. 2003;13:623–634. doi: 10.1016/s1052-5157(03)00102-8. [DOI] [PubMed] [Google Scholar]
- 54.Jakobs R, Maier M, Kohler B, Riemann JF. Peroral laser lithotripsy of difficult intrahepatic and extrahepatic bile duct stones: laser effectiveness using an automatic stone-tissue discrimination system. Am J Gastroenterol. 1996;91:468–473. [PubMed] [Google Scholar]
- 55.Schreiber F, Gurakuqi GC, Trauner M. Endoscopic intracorporeal laser lithotripsy of difficult common bile duct stones with a stone-recognition pulsed dye laser system. Gastrointest Endosc. 1995;42:416–419. doi: 10.1016/s0016-5107(95)70042-0. [DOI] [PubMed] [Google Scholar]
- 56.Jakobs R, Adamek HE, Maier M, Krömer M, Benz C, Martin WR, Riemann JF. Fluoroscopically guided laser lithotripsy versus extracorporeal shock wave lithotripsy for retained bile duct stones: a prospective randomised study. Gut. 1997;40:678–682. doi: 10.1136/gut.40.5.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Piraka C, Shah RJ, Awadallah NS, Langer DA, Chen YK. Transpapillary cholangioscopy-directed lithotripsy in patients with difficult bile duct stones. Clin Gastroenterol Hepatol. 2007;5:1333–1338. doi: 10.1016/j.cgh.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 58.Bratcher J, Kasmin F. Choledochoscopy-assisted intraductal shock wave lithotripsy. Gastrointest Endosc Clin N Am. 2009;19:587–595. doi: 10.1016/j.giec.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 59.Parsi M, Neuhaus H, Pleskow D, Binmoeller KF, Hawes RH, Petersen BT, Sherman S, Stevens PD, Deviere J, Haluszka O, et al. Peroral cholangioscopy guided stone therapy: report of an international multicenter registry. Gastrointest Endosc. 2008;67:AB102. [Google Scholar]
- 60.Neoptolemos JP, Hofmann AF, Moossa AR. Chemical treatment of stones in the biliary tree. Br J Surg. 1986;73:515–524. doi: 10.1002/bjs.1800730703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Palmer KR, Hofmann AF. Intraductal mono-octanoin for the direct dissolution of bile duct stones: experience in 343 patients. Gut. 1986;27:196–202. doi: 10.1136/gut.27.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Diaz D, Bories P, Ampelas M, Larrey D, Michel H. Methyl tert-butyl ether in the endoscopic treatment of common bile duct radiolucent stones in elderly patients with nasobiliary tube. Dig Dis Sci. 1992;37:97–100. doi: 10.1007/BF01308349. [DOI] [PubMed] [Google Scholar]
- 63.Katanuma A, Maguchi H, Osanai M. Endoscopic treatment of difficult common bile duct stones. Dig Endoscopy. 2010;22:90–97. doi: 10.1111/j.1443-1661.2010.00979.x. [DOI] [PubMed] [Google Scholar]
- 64.Fan Z, Hawes R, Lawrence C, Zhang X, Zhang X, Lv W. Analysis of plastic stents in the treatment of large common bile duct stones in 45 patients. Dig Endosc. 2011;23:86–90. doi: 10.1111/j.1443-1661.2010.01065.x. [DOI] [PubMed] [Google Scholar]
- 65.Jain SK, Stein R, Bhuva M, Goldberg MJ. Pigtail stents: an alternative in the treatment of difficult bile duct stones. Gastrointest Endosc. 2000;52:490–493. doi: 10.1067/mge.2000.108409. [DOI] [PubMed] [Google Scholar]
- 66.Hong WD, Zhu QH, Huang QK. Endoscopic sphincterotomy plus endoprostheses in the treatment of large or multiple common bile duct stones. Dig Endosc. 2011;23:240–243. doi: 10.1111/j.1443-1661.2010.01100.x. [DOI] [PubMed] [Google Scholar]
- 67.Cotton PB. Stents for stones: short-term good, long-term uncertain. Gastrointest Endosc. 1995;42:272–273. doi: 10.1016/s0016-5107(95)70107-9. [DOI] [PubMed] [Google Scholar]
- 68.Bergman JJ, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. Biliary endoprostheses in elderly patients with endoscopically irretrievable common bile duct stones: report on 117 patients. Gastrointest Endosc. 1995;42:195–201. doi: 10.1016/s0016-5107(95)70091-9. [DOI] [PubMed] [Google Scholar]
- 69.Lee TH, Han JH, Kim HJ, Park SM, Park SH, Kim SJ. Is the addition of choleretic agents in multiple double-pigtail biliary stents effective for difficult common bile duct stones in elderly patients? A prospective, multicenter study. Gastrointest Endosc. 2011;74:96–102. doi: 10.1016/j.gie.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 70.Horiuchi A, Nakayama Y, Kajiyama M, Kato N, Kamijima T, Graham DY, Tanaka N. Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest Endosc. 2010;71:1200–1203.e2. doi: 10.1016/j.gie.2009.12.055. [DOI] [PubMed] [Google Scholar]
- 71.Stellato TA, Crouse C, Hallowell PT. Bariatric surgery: Creating new challenges for the endoscopist. Gastrointest Endosc. 2003;57:86–94. doi: 10.1067/mge.2003.24. [DOI] [PubMed] [Google Scholar]
- 72.van Buuren HR, Boender J, Nix GA, van Blankenstein M. Needle-knife sphincterotomy guided by a biliary endoprosthesis in Billroth II gastrectomy patients. Endoscopy. 1995;27:229–232. doi: 10.1055/s-2007-1005676. [DOI] [PubMed] [Google Scholar]
- 73.Choi CW, Choi JS, Kang DH, Kim BG, Kim HW, Park SB, Yoon KT, Cho M. Endoscopic papillary large balloon dilation in Billroth II gastrectomy patients with bile duct stones. J Gastroenterol Hepatol. 2012;27:256–260. doi: 10.1111/j.1440-1746.2011.06863.x. [DOI] [PubMed] [Google Scholar]
- 74.Itoi T, Ishii K, Itokawa F, Kurihara T, Sofuni A. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth ii gastrectomy. Dig Endosc. 2010;22 Suppl 1:S98–S102. doi: 10.1111/j.1443-1661.2010.00955.x. [DOI] [PubMed] [Google Scholar]
- 75.Prat F, Fritsch J, Choury AD, Meduri B, Pelletier G, Buffet C. Endoscopic sphincteroclasy: a useful therapeutic tool for biliary endoscopy in Billroth II gastrectomy patients. Endoscopy. 1997;29:79–81. doi: 10.1055/s-2007-1004079. [DOI] [PubMed] [Google Scholar]
- 76.Ahlawat SK, Singhania R, Al-Kawas FH. Mirizzi syndrome. Curr Treat Options Gastroenterol. 2007;10:102–110. doi: 10.1007/s11938-007-0062-7. [DOI] [PubMed] [Google Scholar]
- 77.Tsuyuguchi T, Sakai Y, Sugiyama H, Ishihara T, Yokosuka O. Long-term follow-up after peroral cholangioscopy-directed lithotripsy in patients with difficult bile duct stones, including Mirizzi syndrome: an analysis of risk factors predicting stone recurrence. Surg Endosc. 2011;25:2179–2185. doi: 10.1007/s00464-010-1520-1. [DOI] [PubMed] [Google Scholar]
- 78.England RE, Martin DF. Endoscopic management of Mirizzi's syndrome. Gut. 1997;40:272–276. doi: 10.1136/gut.40.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Farah M, McLoughlin M, Byrne MF. Endoscopic retrograde cholangiopancreatography in the management of benign biliary strictures. Curr Gastroenterol Rep. 2008;10:150–156. doi: 10.1007/s11894-008-0036-5. [DOI] [PubMed] [Google Scholar]
- 80.Hisatomi K, Ohno A, Tabei K, Kubota K, Matsuhashi N. Effects of large-balloon dilation on the major duodenal papilla and the lower bile duct: histological evaluation by using an ex vivo adult porcine model. Gastrointest Endosc. 2010;72:366–372. doi: 10.1016/j.gie.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 81.David L Carr-Locke. Ask the expert. Management of bile duct stones. ASGE Publications 2011. [Google Scholar]
- 82.Shim CS. How Should Biliary Stones be Managed? Gut Liver. 2010;4:161–172. doi: 10.5009/gnl.2010.4.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Leung JW, Tu R. Mechanical lithotripsy for large bile duct stones. Gastrointest Endosc. 2004;59:688–690. doi: 10.1016/s0016-5107(04)00174-9. [DOI] [PubMed] [Google Scholar]
- 84.Hintze RE, Adler A, Veltzke W. Outcome of mechanical lithotripsy of bile duct stones in an unselected series of 704 patients. Hepatogastroenterology. 1996;43:473–476. [PubMed] [Google Scholar]
- 85.Adamek HE, Buttmann A, Wessbecher R, Kohler B, Riemann JF. Clinical comparison of extracorporeal piezoelectric lithotripsy (EPL) and intracorporeal electrohydraulic lithotripsy (EHL) in difficult bile duct stones. A prospective randomized trial. Dig Dis Sci. 1995;40:1185–1192. doi: 10.1007/BF02065522. [DOI] [PubMed] [Google Scholar]
- 86.Leung JW, Chung SS. Electrohydraulic lithotripsy with peroral choledochoscopy. BMJ. 1989;299:595–598. doi: 10.1136/bmj.299.6699.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Attam R, Freeman ML. Endoscopic papillary large balloon dilation for large common bile duct stones. J Hepatobiliary Pancreat Surg. 2009;16:618–623. doi: 10.1007/s00534-009-0134-2. [DOI] [PubMed] [Google Scholar]