Abstract
Objective. To assess the effect of high-fidelity simulation on pharmacy students’ attitudes and perceived competencies in providing end-of-life care in an interdisciplinary palliative care course.
Design. Thirty pharmacy students participated in a high-fidelity simulation of the 15 minutes before and 15 minutes after the death of a patient with end-stage renal disease.
Assessment. Students completed the Attitudes Toward Death Survey and the End of Life Competency Survey prior to and after experiencing the simulation. A reflections journal exercise was used to capture post-simulation subjective reactions, and a course evaluation was used to assess students’ satisfaction with the simulation experience. Students’ post-simulation attitudes toward death significantly improved compared to pre-simulation attitudes and they felt significantly more competent to take care of dying patients. Students were satisfied with this teaching method.
Conclusion. High-fidelity simulation is an innovative way to challenge pharmacy students’ attitudes and help them with knowledge acquisition about end-of-life care.
Keywords: high-fidelity simulation, end-of-life care, pharmacy education
INTRODUCTION
The Accreditation Council for Pharmacy Education’s standards and guidelines address the concept of educating future pharmacists to be competent and valuable members of the interprofessional team.1 These standards guide pharmacy faculty members to use novel and effective educational methods such as simulations and case studies.
A high-fidelity simulator is a lifelike mannequin that simulates most bodily functions and can be programmed to speak, move, and have physiologic responses. Few studies in the literature describe the effect of high-fidelity simulation on learning outcomes in the area of end-of-life care. Evidence-based approaches are needed to improve pharmacy students’ skills, which are critical to their ability to provide optimal palliative care.
Interdisciplinary education also addresses the Institute of Medicine’s mandate for health professions education aimed at teaching students to deliver patient-centered care across the continuum of care (including end-of-life care) using interdisciplinary approaches and evidence-based practice.2 Traditionally, end-of-life care has not been taught in health professions programs, yet practicing health care professionals frequently encounter dying patients in a variety of settings.
High-fidelity simulations are not commonplace within pharmacy education. A review of pharmacy literature revealed a relative paucity of studies examining high-fidelity simulation as a method of instruction. A search of MEDLINE through September 1, 2010, was conducted using the following terms: assessment, role playing, patient simulation, active learning, and pharmacy student.
Only 3 studies were found that used this innovative learning technique and they included some common elements.3-5 Mieure and colleagues used high-fidelity simulation in addition to traditional classroom teaching methods to asses students’ perceived competency with advanced cardiac life support4 Fernandez and colleagues used debriefing sessions and a pre- and post-simulation survey to assess students’ attitudes toward a high-fidelity simulation experience.3 Students rated the relevance, realism, and application of the simulation high as well as the value of the debriefing. Over 90% said they would like to participate in high-fidelity simulation in the future. Seybert and colleagues used a standardized rubric and a 4-question survey to assess pharmacy students’ competence and attitudes before and after a simulation experience involving blood pressure assessment.5 The percentage of students who were able to obtain an accurate blood pressure reading significantly improved from pre- to post-simulation (21% vs. 97.6%).5 Pharmacy students in all 3 studies reported that the simulation experience enhanced their learning and ability to care for patients.
There have been several studies of the use of simulation in nursing education. A National League of Nursing study (N = 403), comparing paper/pencil case studies, static manikins, and high-fidelity simulations indicated that high-fidelity simulations provided more opportunities for problem solving and improved self-confidence in students participating in postoperative care. Furthermore, there were no significant differences in scores on a standardized national examination among the 3 groups. Smith-Stoner described the use of simulation to introduce nursing students to the “silver hour” (30 minutes before and after death) to develop skills in death-related care.7
In a study by the National Council of State Boards of Nursing, no significant differences were found in knowledge, clinical performance, or self-confidence among 58 nursing students randomized to 1 of 3 groups in a critical care course: simulation instruction only (30 hours), traditional clinical instruction only (30 hours), and simulation plus clinical instruction (15 hours/15 hours).
Few studies have been published on the use of simulation to foster interdisciplinary collaboration.9 In one study, participation of 14 medical students and 68 nursing students in a mock code scenario followed by a debriefing resulted in significant improvement in scores on collaboration for both groups.9 In another study, 19 medical students and 41 nursing students, were grouped into teams to participate in either a high-fidelity simulation of a mock code or a roundtable discussion of the same scenario. Both groups of students agreed that the experience broadened their understanding of interprofessional communication skills and better defined their roles on a team. Additionally, the high-fidelity simulation group reported significantly more stress during the scenario.10
These previous studies on the use of simulation, specifically those related to pharmacy and nursing education, guided the development of the current study. The purpose of this study was to assess the effect of a high-fidelity simulation end-of-life experience on pharmacy students’ attitudes and perceived competencies in care of the dying. A second purpose was to evaluate the effectiveness of high-fidelity simulation in fostering interdisciplinary awareness and collaboration.
DESIGN
A mixed methods design was used to examine students’ perceptions of a simulated death experience and its effect on students’ attitudes regarding end of life and their perceived competencies in providing end-of-life care. This study was approved by the Institutional Review Board at the University of the Incarnate Word, federally designated as a Hispanic serving institution.
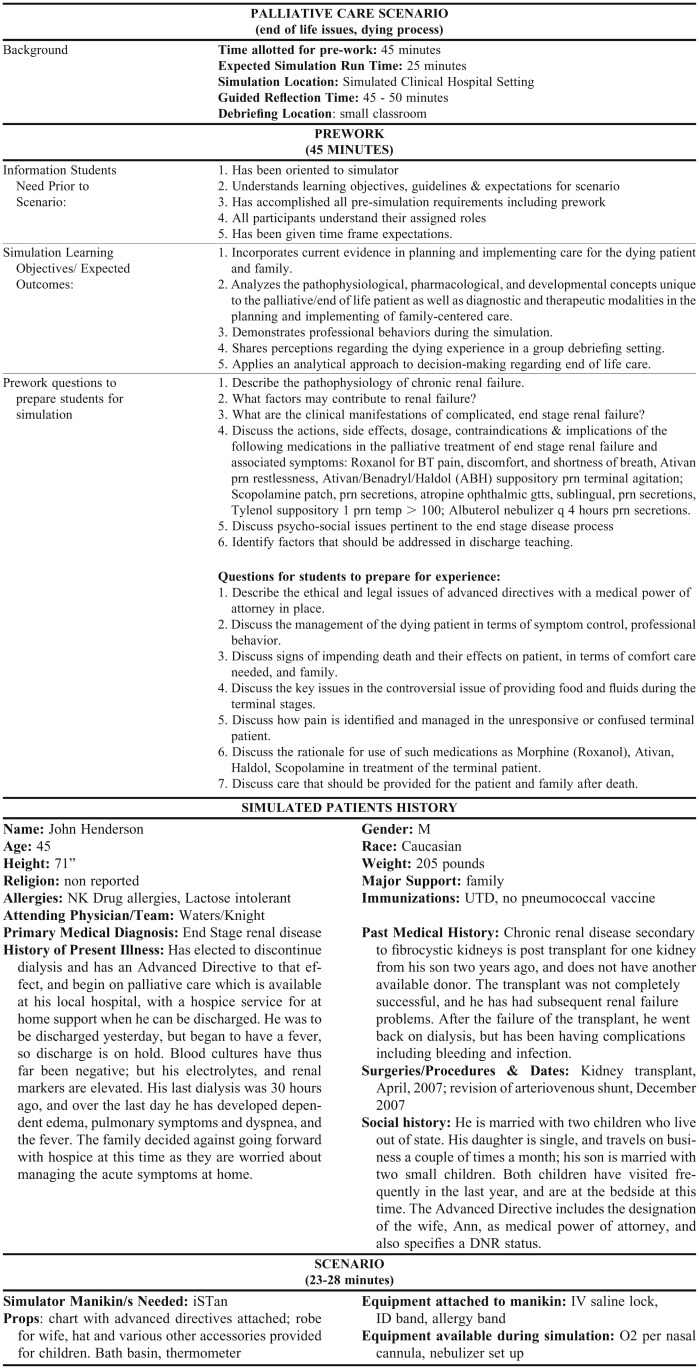
The simulation, which involved the death of a patient with end-stage renal disease, focused on the 15 minutes premortem and 15 minutes postmortem, and used a high-fidelity simulator. Best practices were followed to design, develop, implement, and evaluate the entire simulation experience.11 According to Jeffries, aspects that should be present in a simulation scenario include: having specific objective(s); indicating the level of fidelity for all components, including problem-solving activities; assigning roles in the scenario; and providing debriefing activities. Specific course objectives were written for the simulation scenario, as well as a script for the various roles that students would play during the scenario. Also, a debriefing activity that included both verbal and written components was designed.
Students enrolled in a 3-hour elective entitled Interdisciplinary Approaches to Palliative and End of Life Care were eligible to participate in the simulation. The palliative care elective course is offered only in the fall semester so the simulations were conducted in fall 2009 (n = 20) and fall 2010 (n = 13). The course was taught by faculty members from the school of nursing and the school of pharmacy. Though open to both nursing and pharmacy students, only pharmacy students elected to take the course.
Prior to the simulation, students attended lectures in their palliative care course that addressed social, spiritual, medical, pharmacological, and physiological issues at the time of death. Student-centered learning was encouraged through pre-assigned readings. The students were also provided with the objectives for the simulation experience and questions to answer to prepare them for the simulation. Informed consent was obtained from all participants. Study purpose and methods were disclosed to the students and students were assured that participation was voluntary. Students were not compensated in any form for participating.
The exercise was conducted in a simulation laboratory in the school of nursing, where a highly realistic simulated hospital environment was created for the simulation. A high-fidelity computer-controlled mannequin with human-like features and physiologic functions served as the patient. Participants followed the prewritten scenario (Appendix 1) for the simulation. Students were randomly divided into groups of 4 and each group member was indiscriminately assigned a simulation role: observer, pharmacist, or 1 of 2 of the patient’s family members. The roles of nurse, chaplain, and physician were played by course faculty members.
The pharmacist role was played by a pharmacy student who was expected to suggest other routes of administration for medication if the patient was unable to swallow or suggest medications more effective at relieving the symptoms the patient was experiencing. The scenario focused on the 30 minutes surrounding the patient’s death and involved learners responding to and acting upon experiences typically encountered during an actual end-of-life event.
Immediately following the simulation, each student was given 30 minutes of individual reflective journaling time to focus on their perceptions and attitudes about the experience. A debriefing was then held in which a trained high-fidelity simulation facilitator, who was not directly involved with the course, guided a self-discovery process with the aim of reviewing the events that occurred, focusing on things that could have been done differently or more effectively, appropriate actions taken, and the roles of the team members. This included review of the simulation objectives provided to students before the scenario (Table 1).
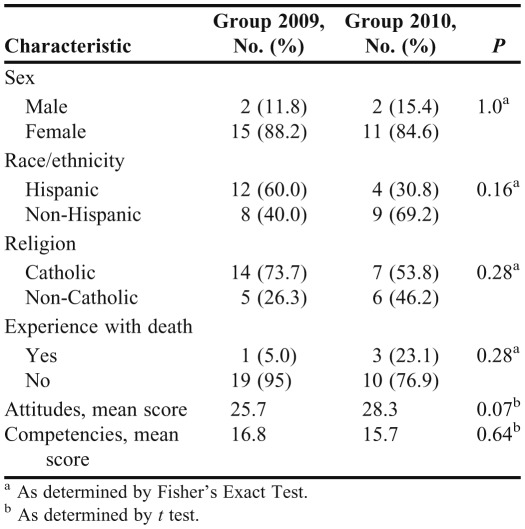
Table 1.
Demographic Data of Pharmacy Students Who Participated in a High-Fidelity Simulation Involving the Death of a Patient With End-Stage Renal Disease, N = 33
EVALUATION AND ASSESSMENT
Two self-administered survey instruments, a student satisfaction questionnaire, and student comments from reflections and debriefings were used for assessment. The 2 survey instruments, the Attitudes Toward Death Survey and the End of Life Competency Survey, were administered before and after the simulation experience.
The Attitudes Toward Death Survey is a 28-item questionnaire with responses based on a 5-point Likert scale ranging from strongly agree (5) to strongly disagree (1).12 The survey instrument is divided into 3 subscales with one 10-item subscale measuring attitudes and the other 2 subscales measuring problems in end-of-life care and improvements needed in end-of-life education. Questions in the attitude subscale include “I am not comfortable caring for the dying patients” and “When a patient dies, I feel something went wrong.” The responses to the 10 items in the first subscale are summed for an overall score. A lower score indicates a more positive attitude.
The End of Life Competencies survey was developed as part of the End of Life Nursing Education Consortium project.13 This tool consists of 6 items referring to student demographic data and 14 items concerning perceived competency, each with Likert-scale responses ranging from not at all effective (1) to very effective (5). Responses to the 14 questions were summed for an overall score; a higher score indicates a higher self-perceived level of competency. Questions include “How effective do you believe you are in pain management?” and “How effective do you believe you are in communication with terminally ill patients?”
A student satisfaction questionnaire, established for course evaluations at the university, was used to assess student satisfaction with the course, faculty members, teaching approaches, and other factors. The survey tool consists of 12 standard questions regarding student satisfaction, and 3 questions that were specific to the use of simulation in the course. Responses were based on a Likert scale ranging from strongly disagree (1) to strongly agree (5). Questions included in this questionnaire were “the simulation scenarios used in this course resembled real-life situations” and “the simulation allowed me to analyze my own behavior and actions regarding symptom management and end of life situations.” Finally, student comments during the debriefing and from individual reflections were analyzed.
Quantitative data were analyzed using descriptive statistics, and a paired t test was used to assess differences in pre and post-simulation scores using IBM SPSS 19 (Chicago, IL). Qualitative data were analyzed for themes and patterns among respondents. Although 33 pharmacy students participated in the simulation, only 30 completed the pre- and post-simulation survey tools (19 students in fall 2009, 11 students in fall 2010). An independent samples t test was used to determine that there were no significant differences between the 2009 and 2010 groups in the pre-simulation mean scores in attitudes (p = 0.07) or competencies (p = 0.64) or demographic characteristics of age, gender, religion, or experience with death, indicating the groups were equivalent at the beginning of the study period. Because there were no significant differences in demographics or mean scores on pre-simulation tests between the 2 groups, analysis proceeded as if participants were from a single group. The demographic data reflected a homogenous group with most participants being Hispanic, female, and Catholic (Table 1). All participants were 21 to 40 years of age.
Mean pre- and post-simulation score differences in attitudes toward death and end-of-life competencies were analyzed using a paired t test. There was a significant decrease in mean attitude scores from pre-simulation (26.5 ± 3.8) to post-simulation (24.0 ± 5.9; p = 0.011) indicating significant improvement in attitude towards death. Mean scores on competency also showed significant changes from pre-simulation (mean = 26.52, SD = 3.7616.5 ± 6.5) to post-simulation (23.0 ± 5.7 ; p < 0.001) indicating significantly improved self-perceived competency in providing end-of-life care. The reliability coefficient for the attitudes instrument was 0.75 and the reliability coefficient for the competency instrument was 0.90.
In the debriefing, students stated that they found the simulation to be realistic enough to provoke feelings of difficulty in coping and memories of past death experiences. Comments such as “It was difficult to find the right words to say” and this “process was very intense” indicated that students recognized active involvement in the simulation scenario to the point of feeling distressed and helpless. Finally, students remarked that the simulated death experience should be used for health professionals who had not themselves experienced a death to help them prepare.
In the course evaluation, students reported high satisfaction with the course in terms of overall teaching methods (mean score 4.6 on a 5-point Likert scale with 5 being the highest satisfaction or agreement), realism in the simulated scenario (4.3), and ability to analyze their own behavior regarding end-of-life situations (4.4). They reported that they had achieved course objectives having to do with improved knowledge regarding pharmacological and other approaches to symptom management, communication about end-of-life issues, and overall end-of-life care.
Interdisciplinary collaboration was the most difficult area to measure because all of the students were pharmacy students and the roles of patient care providers from other disciplines were played by faculty members. Comments in the reflections indicated an appreciation of the various roles depicted in the scenario. For example, comments about the nurse role included “provided valuable information” and “was very supportive to the family”. Other comments related to interdisciplinary roles described how other health care professionals (chaplain, social worker, nurse played by faculty members) were respectful of the patient’s decision not to be resuscitated and were sensitive to the family’s needs. Also, students’ comments referred more to how the simulation affected them on a personal and family level, often using examples of previous death experiences with family members, than its impact on them as a future health care professional.
DISCUSSION
This study describes an innovative use of simulation in the sensitive and often neglected area of death and dying education. The findings suggest that the course, including the simulation, achieved the desired outcomes. The lack of end-of-life education for health professionals has been well documented. In a literature search of end-of-life education specifically for pharmacy students, only 3 articles were found.14-16 Simulation could enable the discussion of death and dying, a subject that health professions students may not encounter in their clinical practice experiences. Other factors that limit discussion of death and dying are lack of comfort on the part of staff or faculty members in letting students provide this specialized care to real patients and student discomfort with or even fear of death-related experiences. However, while nursing students in another study regarding end-of-life care reported feelings of being overwhelmed, they also indicated the value of including experiences focused specifically on death and dying in the nursing curriculum.7
In this study, use of a high-fidelity simulator provided an effective teaching strategy in presenting the dying experience to a group of pharmacy students in a palliative care course. Interestingly, the pharmacy students did not desire to play the role of the pharmacist in these simulations preferring instead to be a family member or an observer. Though the reason for this hesitance is unknown, this could possibly reflect the student pharmacist’s greater comfort level in a family member role than as a practicing pharmacist. High-fidelity simulation could also be used to teach other topics. The advantage of this teaching strategy tool is that it not only can be used to improve students’ knowledge and competence in an area, but also to challenge preconceived attitudes that students have regarding age, ethnicity, religion, and medical diagnoses. Another approach would be to assign the roles of other health care professionals to pharmacy students during the simulation and have a discussion in the debriefing of how the experience affected their perceptions of the physician, nurse, chaplain, or social worker. This would force students to research these roles in advance so they would know how to play the role, ie, their patient care responsibilities. Unfortunately, all participants in this study were pharmacy students and only 2 of the faculty members represented nursing, which limits the analysis of interdisciplinary collaboration. However, faculty members modeled roles of the chaplain, social worker, and nurse in the scenario. Further research is needed to determine whether students’ improved attitudes and competency are sustained over time. Classes with other health professions students are essential in fostering interdisciplinary collaboration.
Limitations of this study are the small, homogenous sample, which makes it difficult to generalize results to the general pharmacy student population. Additional data from larger samples with more diverse student backgrounds are needed. Further study of the effects of high-fidelity simulation on the development of interdisciplinary collaboration is necessary to explore this avenue of research.
Also, while based on student reports at the time and comments on the course evaluation the simulated death experience was a compelling strategy, it was impossible to separate out the effect of other elements of the course on students’ learning of palliative care and end-of-life issues. As a total experience, however, the course, including simulation, significantly improved students’ attitudes and perceived competencies. A short knowledge test before and after the course may have provided a more specific measure of knowledge acquisition regarding palliative and end-of-life care through the simulation and overall course experience.
CONCLUSION
High-fidelity simulation can be used effectively to teach content in health professions programs. This learning tool can be used to teach basic skills and knowledge and allow students to practice what they have learned in a low-risk environment, and to challenge students’ attitudes about situations. Although this study is about application of high-fidelity simulation in end-of-life care, this teaching tool could be used effectively to teach most content. As the emerging role of the pharmacist involves interaction with the public and a variety of interdisciplinary team members, realistic role play exercise using high-fidelity simulation can provide a valuable opportunity for pharmacy students to practice and learn this new role.
Appendix 1. High-Fidelity Simulation Scenario of the Death of a Patient With End-Stage Renal Disease
REFERENCES
- 1.Accreditation Council for Pharmaceutical Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed April 4, 2012.
- 2.Greiner AC, Knebel E. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003. pp. 1–6. [PubMed] [Google Scholar]
- 3.Fernandez R, Parker D, Kalus J, Miller D, Compton S. Using a human simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3):Article 51. doi: 10.5688/aj710351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mieure KD, Vincent WR, III, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2):Article 22. doi: 10.5688/aj740222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeffries P, Rizzolo MA. Designing and implementing models for the innovative use of simulation to teach nursing care of ill adults and children: a national, multi-site, multi-method study. Natl League Nurs. http://www.nln.org/research/LaerdalReport.pdf. 2006. Accessed April 4, 2012. [Google Scholar]
- 7.Smith-Stoner M. Using high fidelity simulation to educate nursing students about end-of-life care. Nurs Educ Perspect. 2009;30(2):115–120. [PubMed] [Google Scholar]
- 8.Hicks FD, Coke L, Li S. Report of findings from the effect of high-fidelity simulation on nursing students’ knowledge and performance: a pilot study. NCSBN Res Brief. 2009;40(June):2–34. [Google Scholar]
- 9.Dillon P, Noble K, Kaplan L. Simulation as a means to foster collaborative interdisciplinary education. Nurs Educ Perspect. 2009;30(2):87–90. [PubMed] [Google Scholar]
- 10.Reising DL, Carr DE, Shea RA, King JM. Comparison of communication outcomes in traditional versus simulation strategies in nursing and medical students. Nurs Educ Perspect. 2011;32(5):323–327. [PubMed] [Google Scholar]
- 11.Jeffries P. A framework for designing, implementing, and evaluation simulations used as teaching strategies in nursing. Nurs Educ Perspect. 2005;26(2):96–103. [PubMed] [Google Scholar]
- 12.Strumpf N. Attitudes towards death survey: promoting excellence in end-of-life care. http://www.promotingexcellence.org/pennsylvania/downloads/up03.pdf. Accessed April 20, 2012.
- 13.ELNEC Core Curriculum, American Association of Colleges of Nursing. http://www.aacn.nche.edu/elnec/curriculum.htm. Accessed April 4, 2012.
- 14.Bealle J, Broesker A. Pharmacy students’ attitudes toward death and end of life care. Am J Pharm Educ. 2010;74(6):Article 104. doi: 10.5688/aj7406104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herndon C, Jackson K, Fike D. End of life care education in United States pharmacy schools. Am J Hosp Palliat Care. 2003;20(5):340–344. doi: 10.1177/104990910302000507. [DOI] [PubMed] [Google Scholar]
- 16.Herndon C, Fike D, Anderson A, Dole E. Pharmacy student training in United States hospices. Am J Hosp Palliat Care. 2001;18(3):181–186. doi: 10.1177/104990910101800309. [DOI] [PubMed] [Google Scholar]