Abstract
Objectives. To assess the effectiveness of human patient simulation to teach patient safety, team-building skills, and the value of interprofessional collaboration to pharmacy students.
Design. Five scenarios simulating semi-urgent situations that required interprofessional collaboration were developed. Groups of 10 to 12 health professions students that included 1 to 2 pharmacy students evaluated patients while addressing patient safety hazards.
Assessment. Pharmacy students’ scores on 8 of 30 items on a post-simulation survey of knowledge, skills, and attitudes improved over pre-simulation scores. Students’ scores on 3 of 10 items on a team building and interprofessional communications survey also improved after participating in the simulation exercise. Over 90% of students reported that simulation increased their understanding of professional roles and the importance of interprofessional communication.
Conclusions. Simulation training provided an opportunity to improve pharmacy students’ ability to recognize and react to patient safety concerns and enhanced their interprofessional collaboration and communication skills.
Keywords: simulation, interprofessional, emergency department, patient safety, team work
INTRODUCTION
The Accreditation Council for Pharmacy Education recognizes the importance of interprofessional education and supports its inclusion within the pharmacy curriculum.1 This inclusion can be partially attributed to the 2001 Institute of Medicine (IOM) report, “Crossing the Quality Chasm,” which stated there were significant deficits in the quality of care provided to patients. Among these deficits were a dearth of interdisciplinary collaboration among healthcare professionals. The report further stated that this deficit could impede effective communication among healthcare providers and significantly compromise patient safety. Additionally, the IOM report identified 10 rules for health systems redesign, one of which was to improve collaboration among all individuals involved in a patient’s care. The report stated that health care providers could no longer operate in segregated units – or “professional silos” – and expect to optimize patient care.2 Kyrkjebo and colleagues wrote that students in various healthcare professions develop a conceptual understanding of other professionals’ roles on the healthcare team but are not afforded the opportunity to apply teamwork skills in a hands-on manner.3 The responsibility of teaching teamwork and collaboration falls to educators. One strategy to teach these skills may be to create a simulated situation where students have the opportunity to learn together in a risk-free environment. This approach was supported in the IOM report “To Err is Human,” which proposed that simulation training might be a strategy to improve patient safety.4 Simulation training has improved students’ technical and clinical skills.5-16 However, there is little focus on teaching patient safety concepts to the novice learner. This paper describes the development and initial experiences of human patient simulation to promote interprofessional teamwork and collaboration while providing novice learners an opportunity to recognize and react to select Joint Commission National Patient Safety Goals.17
DESIGN
Every spring semester since 2003, the University of Missouri offers a once-a-week, 4-week interprofessional curriculum that focuses on teamwork/communication, patient safety, and quality improvement. The University of Missouri-Kansas City (UMKC) School of Pharmacy satellite campus joined this curriculum in 2009 to provide third-year pharmacy students the opportunity to interact with other health professions students. This was an opportunity to provide satellite students more robust opportunities to learn about teamwork and patient safety while developing relationships with students who they would possibly encounter again on clinical practice experiences in the region.
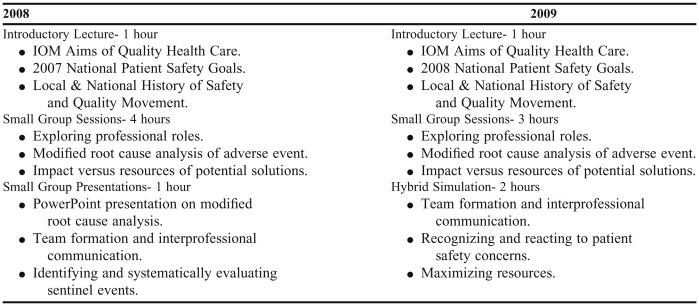
Prior to 2009, the interprofessional curriculum consisted of an introductory lecture followed by a small-group exercise, which entailed completing a root-cause analysis of a sentinel event. The purpose of the class was to encourage teamwork in a collaborative environment where students could apply a systems-based approach to quality improvement. The course underwent several revisions of content and teaching methods including adopting a problem-based learning (PBL) format and the addition of students from other health professions.18,19 The components are presented in Table 1. In 2009, a simulation component was added to the curriculum to provide more hands-on opportunities to work together as part of an interdisciplinary team and potentially increase the curriculum’s perceived relevance to students’ future careers. The course enrolled approximately 210 students from the colleges and schools of pharmacy, medicine, nursing, health professions, and health administration. These students included undergraduate students, graduate students, and students in professional programs. Students varied in clinical experience from no clinical exposure, to participation in several prior clinical practice experiences. The level of experience with high-fidelity simulation also differed among the students, with nursing students having the most experience with simulation. Pharmacy students had no prior experience with simulation. An interprofessional steering committee with a representative from each participating school coordinated the course. Each representative ensured that the curriculum was applicable to the students involved in the course. For all programs, interprofessional curriculum was a required course component. Because of the variation in curricula content among the participating schools, each program determined a course within which to incorporate the interprofessional curriculum. The school of pharmacy opted to incorporate the course into a clinical introductory pharmacy practice experience (IPPE). All schools opted not to provide a grade for the interprofessional curriculum and felt that the formative feedback was more important than a summative grade. The Health Sciences Institutional Review Board at the University of Missouri approved all data collection and analysis.
Table 1.
Comparison of Interprofessional Curriculum in Safety, Quality, and Teamwork Between 2008 and 2009 When a Simulation Exercise Was Added
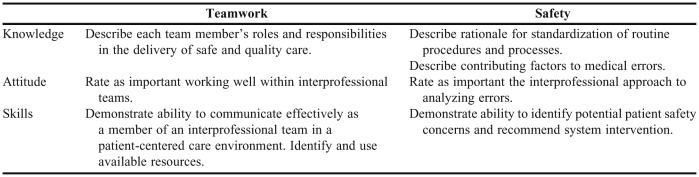
The introductory lecture and small group sessions were reduced from 6 contact hours to 4 to allow time in the curriculum for a 1-hour hybrid simulation experience. The simulation exercises addressed specific educational objectives that complemented the lecture and small-group sessions (Table 2).
Table 2.
Pharmacy Student Objectives for an Interprofessional Simulation Exercise
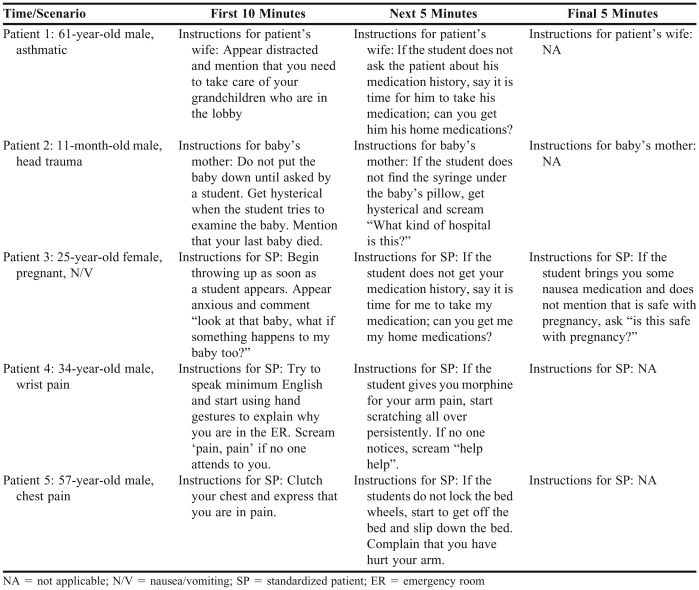
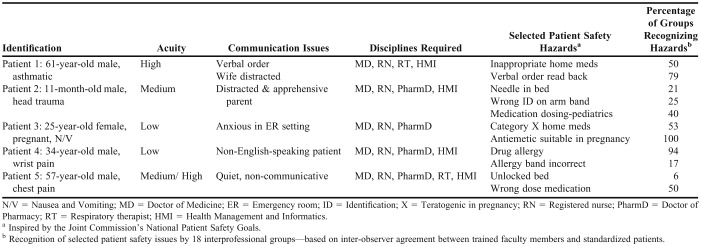
The team chose an acute care setting for the simulation experience, specifically a hospital emergency department receiving an influx of lower-acuity patients after a mass-casualty event. Five patient cases were developed using a combination of standardized patients, high-fidelity simulators, and hospital staff members, including resident physicians. Scenarios integrated specific patient hazards derived from the National Patient Safety Goals. The students were expected to address multicultural and multigenerational barriers to communication with the patient and family members. To optimize opportunities for interprofessional collaboration, the simulation area replicated a real emergency department with supplies and services such as a pharmacy, diagnostic radiology, and a laboratory. Both high-fidelity simulators and standardized patients were used in the simulations. A human adult simulator was used to simulate an asthma case and a pediatric simulator was used to simulate a head trauma case. The simulators were programmed to simulate specific physiologic symptoms, such as wheezing and crying, the latter of which added a realistic environmental distraction. Standardized patients served as either a patient or a family member. These actors received training and instruction regarding specific behaviors and actions to portray during the simulation. These included displaying certain emotional responses during the scenario to add an extra layer of complexity to the experience. Typical standardized patient emotional responses consisted of repeated calls for attention, hysterical crying, and anxiety over the care of children waiting in the lobby of the emergency department. In the training session, each actor was given a script with verbal cues to provide students with subtle guidance regarding the care of the patient (Table 3). Facilitators and observers were trained in the use of the checklists, on the various patient safety hazards that were embedded in the cases (Table 4), and about National Patient Safety Goals.
Table 3.
Verbal Cues Provided to Standardized Patients Participating in an Interprofessional Simulation
Table 4.
Recognition of Selected Patient Safety Issues by Interprofessional Students Participating in Various Emergency Department Simulations (N = 18 Groups)a
Simulation Exercise
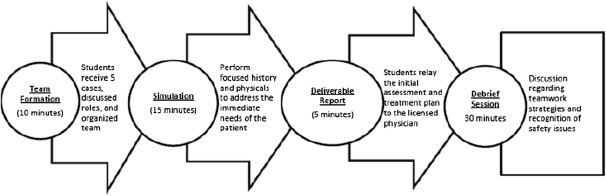
To refine the simulations, 3 plan, do, study, act (PDSA) cycles were conducted to identify any areas of improvement. Once all problems were rectified in the PDSA cycles, students participated in the simulation as outlined (Figure 1). Groups of 10 to 12 students with representatives from all participating schools received the 5 patient cases. Students were instructed to triage, assess, and provide initial evaluation and treatment plans under the supervision of a licensed physician (an intern). Students had to meet the needs of the patient within the scope of their own discipline and to remain within their student role. Each group had 10 minutes to form their team and determine the best course of action to provide safe and effective care to the 5 patients.
Figure 1.
Interprofessional curriculum in quality, safety, and teamwork.
After rapid team formation, the licensed physician briefly made students aware of available resources. During the simulation, the licensed physician provided little assistance with regard to medical decision-making, allowing students to independently create a care plan for each patient. While student roles were not delineated by the facilitators, the pharmacy student on the team was expected to make sure the patient’s therapeutic regimen was appropriate. In the case of the pregnant patient, teratogenic medications were included as part of the patient’s home medications. The pharmacy students were expected to take on the role of the medication-use expert and determine whether these medications should be discontinued. This also applied to the patient who presented with an acute asthma exacerbation. This patient’s home medications consisted of a non-selective beta blocker which could have contributed to the asthma exacerbation. For the head trauma case, the pharmacy student on the team was expected to assist with dosing any medications that the team chose to administer to the patient. The patient who presented with wrist pain had an allergy to morphine and required an alternative analgesic. During the simulation, the intern physician ordered the wrong dose of a medication for the patient who presented with chest pain, and the pharmacy student was expected to intervene on this error.
At the end of the exercise, the team of 5-6 students provided a report summarizing their assessment and plan to the licensed physician. Following the simulation, the students participated in a debriefing session led by an interprofessional team of faculty members. Students reflected on the simulation, focusing on effective areas of teamwork and communications, as well as opportunities for improvement. Students also identified the safety issues embedded in each case, including any patient safety concerns that they did not respond to during the simulation. This provided opportunities for introspection and allowed students to see the importance of having other health professionals on their team who were able to pinpoint profession-specific safety issues. At the end of each debrief session, the facilitator highlighted the National Patient Safety Goals and reinforced the importance of patient safety education.
The resources required to support the 2 days of simulation included 16 faculty raters (1 hour of training; 2 to 6 hours of observation), 5 standardized patients/family members per room, 4 audiovisual staff members, 1 interpreter, 6 to 8 support staff members/session, 6 high-fidelity simulators (2/room), 3 simulation rooms, 6 classrooms, 6 computers, audiovisual equipment, hospital beds, and medical equipment.
EVALUATION AND ASSESSMENT
Two hundred eight students from various disciplines participated in the simulation exercise. Of these, 11% were pharmacy students, 46% were medical students and 26% were nursing students.
Debriefing
Trained faculty observers completed a detailed checklist that highlighted student responses to various teamwork, communication, and safety concerns. Faculty observers documented safety hazards recognized and reacted to by the student teams. Additionally, the licensed physician (intern) and standardized patients completed observation forms. Video and audio recordings were taken from multiple angles throughout the simulation rooms. Unfortunately, the audio-visual equipment did not adequately capture student-patient interaction and was not used for the debrief as originally intended by the committee. Completed forms provided data for summative feedback to students during the debrief session and helped to facilitate a meaningful follow up.
Survey Findings
Faculty members administered a 30-item Likert scale pre- and post-course knowledge, skills, and attitudes (KSA) survey instrument regarding teamwork and quality improvement, previously adapted from Madigosky and colleagues for this curriculum.18-20 Students also completed a 10 item pre- and post-simulation team building and interprofessional communications survey tool adapted from existing literature.8 Finally, students completed a general course evaluation.
Statistical analysis was done using SAS, version 9.2 (Cary, NC) to analyze the data from the KSA survey tool, team building and interprofessional communications survey tool, and the course evaluations. Data from the KSA survey tool were matched by discipline for analysis. Matched pre/post data were analyzed using Bhapkar’s test for marginal homogeneity.21 The Wilcoxon rank sum test was used to compare the distribution of each survey question (the scale of 1 to 10) pre- and post-simulation. In view of these multiple tests, the False Discovery Rate (FDR) was used to control the rate of false discoveries.22 For these multiple tests, FDR adjusted p values of ≤0.05 were considered significant. As subject identifiers were not available, the pre- and post-simulation groups were treated as independent groups for this analysis. The pre- and post-simulation team building and interprofessional communications survey data were analyzed in aggregate without individual or professional discipline analysis. Course evaluation data were matched by de-identified individual and discipline for analysis.
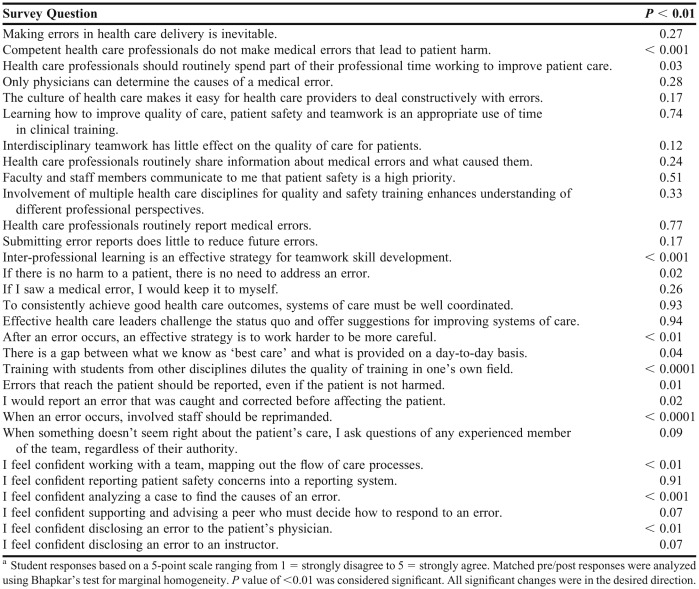
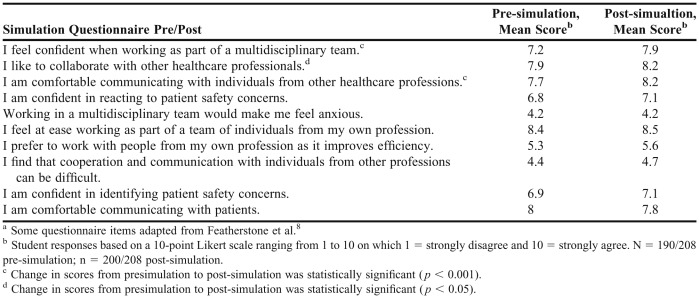
Knowledge, Skills, and Attitudes Survey. Significant positive improvements were seen in students’ responses on the post-course survey of knowledge, skills, and attitudes (Table 5). Fewer students post-course agreed that training with students from other disciplines diluted the quality of training in their own field (p < 0.001), that competent health care professionals do not make medical errors that lead to patient harm (p < 0.001), and that staff members should be reprimanded when an error occurs (p < 0.001). These responses were not significantly different from previous years; however, students’ comfort with disclosing an error to the patient’s physician (p = 0.002) was. Students also responded more positively to questions on interprofessional communication and teamwork pre- and post-simulation. However, students did not report feeling more confident reacting to patient safety concerns after the simulation (Table 6). Of note, only 6 out of 11 safety issues embedded in the cases were identified by greater than 50% of student groups in this pilot simulation (Table 4). Only 50% of the teams noticed that the pregnant patient’s home medications were teratogenic and that the asthmatic patient’s home medications were inappropriate.
Table 5.
Change in Pharmacy Students’ Responses on the Knowledge, Skills, and Attitudes Survey After Participating in an Interprofessional Simulation Exercise (N =110)a
Table 6.
Responses to the Team Building and Interprofessional Communications Survey Pre- and Post-Simulationa
Students provided more positive evaluations of the entire course than did students in the previous 2 years. When asked the question “Should simulation be included in future reiterations of the course?” on a Likert scale of 1 to 5, with 5 being “strongly agree,” the average score was 4.2. Over 90% of all students agreed or strongly agreed with statements that the simulation had increased their understanding of the importance of interprofessional communication, understanding of the roles of other healthcare professionals, and ability to recognize and respond to patient safety issues.
DISCUSSION
This pilot study immersed students in a “real-life, low-risk” experience that encouraged interprofessional teamwork and communication while providing safe patient care. Developing a learning experience simulating real-life healthcare situations requires significant commitment from faculty and staff members and volunteers, as well as extensive equipment and facility resources. This can present a challenge in resource-limited academic settings. One of the strengths of this study was the deliberate likeness to a real emergency department setting and the introduction of the complexities rampant in this healthcare setting. By requiring students to prioritize care and resources for multiple patients with health problems of varying acuity, they experienced some of the chaotic nature of an emergency department.
There is a concern that students’ self-reported confidence in identifying safety concerns did not significantly increase during the simulation exercise. However, this may be because a majority of the student groups only recognized 6 of the 11 safety issues in the cases. Exposing this gap in competence may provide opportunities for educators to better address this topic in subsequent curriculum revisions. From a pharmacy curriculum perspective, more emphasis should be placed on medication safety.
We identified several limitations to this study and the simulation experience. First, the learners involved in the simulation had varied levels of clinical experience (eg, third-year pharmacy students enrolled in IPPE versus second-year/pre-clinical medical students). Students with little or no clinical experience were noted to have the most difficulty and stress during the simulation. Additionally, in facilitated debriefs and post-course faculty evaluations, faculty observers reported there was tremendous apprehension from students who had not been involved in a simulation previously. The level of complexity and inherent chaos generated by creating a realistic, high-acuity setting likely compounded the challenge faced by the most novice learners participating in the experience. An initial, lower-complexity simulation exercise at the beginning of the unit could provide many benefits to students in this case. Specifically, this would orient students to the concept of human patient simulation as well as allow for repeated, interactive exposure to important patient safety concepts. Second, students expressed some confusion about their roles and responsibilities during the simulation, especially the health management students. More instruction prior to the simulation may have prevented some of this confusion, but must be balanced with providing students sufficient autonomy to independently organize themselves. The pre- and post-simulation survey responses were not matched by de-identified individuals, resulting in statistical analysis on group data alone without comparison of changes in individuals’ responses.
The steering committee learned several important concepts as part of the simulation development experience. First, the PDSA cycles were integral in creating a cohesive simulation. They allowed for early feedback to simulation planners and troubleshooting of logistical problems without detrimental impact on the intended learners. Involving all stakeholders when developing objectives and scenarios allowed the planners to create a more well-rounded experience for students of multiple professions and helped add details that made the simulation more true to life.
These lessons reinforce the need for extensive and early involvement of simulation center personnel and for interprofessional collaboration. Additionally, having adequate numbers of observers requires a concerted recruitment effort. Finally, coordinating the diverse schedules of students from multiple professional schools requires extensive planning, as well as flexibility by educators and professional school administrators.
SUMMARY
Simulation-based interprofessional education is an innovative method of teaching novice students communication and teamwork skills while reinforcing patient safety concepts. With varying curricula within the health professions programs, a design such as the one described here that incorporates interprofessional education into existing courses may be a way to circumvent concerns from programs about adding an additional course into their curriculum. This course provided pharmacy students the opportunity to collaborate with other healthcare professionals and sensitized them to patient safety issues that they may not have encountered in their classroom or experiential coursework. For other pharmacy schools considering the addition of interprofessional education to their curriculum, it may be possible to incorporate a short simulation exercise such as this prior to students beginning their advanced pharmacy practice experiences.
ACKNOWLEDGEMENTS
The authors wish to acknowledge Dr. Leslie Hall, Dr. Karen Cox, Dr. Douglas Wakefield, Dr. Richard Madsen, Dr. Linda Headrick, Dr. Youngju Pak, the Interprofessional steering committee, and the staff of the Russell D. and Mary B. Shelden Clinical Simulation Center.
REFERENCES
- 1.Accreditation Council for Pharmaceutical Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed February 29, 2012.
- 2.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 3.Kyrkjebo JM, Brattebo G, Smith-Strom H. Improving patient safety by using interprofessional simulation training in health professional education. J Interprof Care. 2006;20(5):507–516. doi: 10.1080/13561820600918200. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 5.Comer SK. Patient care simulations: role playing to enhance clinical understanding. Nurs Educ Perspect. 2005;26(6):357–361. [PubMed] [Google Scholar]
- 6.Feingold CE, Calaluce M, Kallen MA. Computerized patient model and simulated clinical experiences: evaluation with baccalaureate nursing students. J Nurs Educ. 2004;43(4):156–163. doi: 10.3928/01484834-20040401-03. [DOI] [PubMed] [Google Scholar]
- 7.Henneman EA, Cunningham H. Using clinical simulation to teach patient safety in an acute/critical care nursing course. Nurse Educ. 2005;30(4):172–177. doi: 10.1097/00006223-200507000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Featherstone P, Smith GB, Linnell M, Easton S, Osgood VM. Impact of a one-day inter-professional course (ALERT) on attitudes and confidence in managing critically ill adult patients. Resuscitation. 2005;65(3):329–336. doi: 10.1016/j.resuscitation.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 10.Larew C, Lessans S, Spunt D, Foster D, Covington BG. Innovations in clinical simulation: application of Benner's theory in an interactive patient care simulation. Nurs Educ Perspect. 2006;27(1):16–21. [PubMed] [Google Scholar]
- 11.Lighthall GK, Barr J, Howard SK, et al. Use of a fully simulated intensive care unit environment for critical event management training for internal medicine residents. Crit Care Med. 2003;31(10):2437–2443. doi: 10.1097/01.CCM.0000089645.94121.42. [DOI] [PubMed] [Google Scholar]
- 12.Marshall RL, Smith JS, Gorman PJ, Krummel TM, Haluck RS, Cooney RN. Use of a human patient simulator in the development of resident trauma management skills. J Trauma. 2001;51(1):17–21. doi: 10.1097/00005373-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Peteani LA. Enhancing clinical practice and education with high-fidelity human patient simulators. Nurse Educ. 2004;29(1):25–30. doi: 10.1097/00006223-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Seropian MA, Brown K, Gavilanes JS, Driggers B. An approach to simulation program development. J Nurs Educ. 2004;43(4):170–174. doi: 10.3928/01484834-20040401-02. [DOI] [PubMed] [Google Scholar]
- 15.Small SD, Wuerz RC, Simon R, Shapiro N, Conn A, Setnik G. Demonstration of high-fidelity simulation team training for emergency medicine. Acad Emerg Med. 1999;6(4):312–323. doi: 10.1111/j.1553-2712.1999.tb00395.x. [DOI] [PubMed] [Google Scholar]
- 16.Spunt D, Foster D, Adams K. Mock code: a clinical simulation module. Nurse Educ. 2004;29(5):192–194. doi: 10.1097/00006223-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Joint Commission on the Accreditation of Healthcare Organizations. National Patient Safety Goals. http://www.jointcommission.org/patientsafety/nationalpatientsafetygoals. Accessed February 29, 2012.
- 18.Madigosky WS, Headrick LA, Nelson K, Cox KR, Anderson T. Changing and sustaining medical students' knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006;81(1):94–101. doi: 10.1097/00001888-200601000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Hall LW, Cox KR, Scott SD, et al. Interprofessional teamwork in health care – a successful model that creates “open spaces for learning” about quality and safety. Qual Saf Health Care. 2008;17(3):224–232. [Google Scholar]
- 20.Hall LW, Cox KR, Scott SD, et al. Problem-based quality/safety curriculum enhances interprofessional teamwork. Qual Saf Health Care. 2008;17(3):224–232. [Google Scholar]
- 21.Bhapkar VP. A note on the equivalence of two test criteria for hypotheses in categorical data. J Am Stat Assoc. 1966;61(313):228–235. [Google Scholar]
- 22.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc. 1995;57(1):289–300. [Google Scholar]