Summary
Detachable coils are established as a safe and effective treatment option for some patients with intracranial aneurysms. However this treatment is not useful for the treatment of certain types of complicated aneurysms. Wide-necked or broadbased aneurysms are still complicated to embolize because of the risk of coil migration or coil protrusion into the parent vessel.
The Neuroform stent has recently been introduced for the treatment of complex aneurysms. The stent functions primarily to provide durable parent vessel protection during embolization.
This report demonstrates coil migration occurring as a delayed complication of Neuroform stent-assisedt coil embolization of a small intracranial aneurysm.
Key words: coil migration, Neuroform stent
Introduction
The treatment of intracranial aneurysms with endovascular coils has become an important and well known alternative to microsurgical clip placement 1,2. Detachable coils are established as a safe and effective treatment option for some patients with intracranial aneurysms 3,4. Despite advances in the devices and techniques for endovascular occlusion of intracranial aneurysms, aneurysmal configuration remains a technical limiting factor in coiling 5,6.
The application of stent-assisted coiling in intracranial aneurysms offers significant technical advantages. But stent technology has been limited primarily by the safely negotiating the available stiff unique structure.
The author experienced delayed coil migration under stent-assisted coiling during anterior choroidal artery aneurysm treatment. The case is reported together with a literature review.
Case Report
A 66-year-old man with subarachnoid hemorrhage (SAH) was admitted in Hunt and Hess Grade II. The initial brain computed tomography (CT) scan revealed significant subarachnoid blood around both sylvian fissures (Figure 1). Three dimensional (3D)-CT angiography and diagnostic cerebral angiography showed a small aneurysm of left anterior choroidal artery and another region revealed a negative nonspecific finding (Figure 2). Because of the small size and intolerable dome and neck ratio, we decided to place a stent before placing the coil. Pretreatment with antiplatelet agents was not done. A 3.5 cm x 15 mm Neuroform stent (Boston Scientific/Target Therapeutics, Inc., Natick, MA) was deployed, followed by endovascular occlusion. A single 2 mm x 2 cm Guglielmi detachable ultrasoft coil (Boston Scientific) was introduced into the aneurysm. An unsubtracted image shows the stent and coil in place (Figure 3). The patient was discharged from the hospital 14 days after admission without any neurological deficits. After ten months, follow-up cerebral angiography showed coil migration (Figure 4).
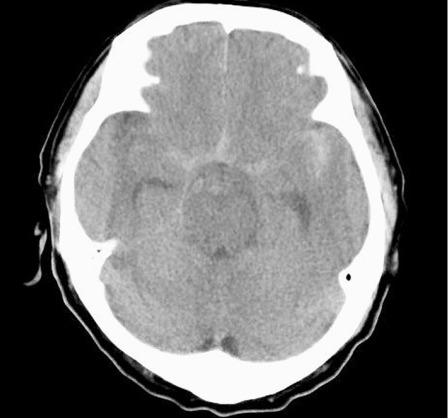
Figure 1.
Initial non-contrast brain CT scan reveals hyperdense subarachnoid hemorrhage in the basal cistern and left sylvian fissure.
Figure 2.
Three dimensional (3D) CT angiography and digital subtraction angiography at admission. A) 3D CT angiography shows a small anterior choroidal artery aneurysm in the left internal carotid artery. B) Oblique view of left ICA angiography shows an aneurysm in the anterior choroidal artery.
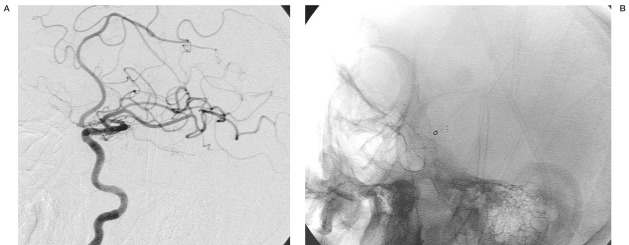
Figure 3.
A) Immediately post treatment, oblique view unsubtracted left ICA angiography demonstrating a residual filling in aneurysm. B) Oblique view demonstrating an optimal stent position.
Figure 4.
Follow-up angiography ten months after treatment. Oblique unsubtracted view of left ICA angiography shows a coil migration into the distal middle cerebral artery.
Discussion
The endovascular treatment of intracranial aneurysms with detachable coils has developed into a widely used and effective technique 3,4. Despite increasing clinical experience and technological improvements, endovascular treatment still has inherent risks of morbidity and mortality 7. In particular, this treatment is not a useful option for the treatment of certain types of complicated aneurysms: wide-necked or broad-based aneurysms are still complicated to embolize because of the risk of coil migration or coil protrusion into the parent vessel 8,9.
The application of an endovascular stent as an adjunctive technique to coil embolization has evolved rapidly in recent times 9. The Neuroform stent, a Nitinol self-expanding stent delivered through a microcatheter, offers several substantial advantages over the preexisting balloon expandable coronary stents primarily related to the increased flexibility of the stent and delivery system, which allows safe negotiation and deployment within even the most tortuous segments of the cerebrovasculature 6,10,11.
The stents come in a variety of diameters and lengths, ranging from 2.5 to 4.5 mm and 10 to 20 mm. The ultrathin property of the stent struts makes the stent essentially radiolucent, and this is offset by four radiopaque platinum marker bands at each end. In addition, it is composed of six to eight cells that are joined to one another 6,9,10. The stent is 'open-cell' with two fusion points between stent elements. The cell size between elements ranges from 2.0 to 2.7 Fr. The open cell design with only two fusion points makes the Neuroform stent system highly flexible and is large enough to allow protrusion and migration of coils 8,10,11.
Stent-assisted coiling provides important technical and theoretical advantages 8,9,11. By providing secure and durable protection of the parent vessel, a broad-necked aneurysm theoretically could be more completely packed with coils with less risk of rupture, coil migration and parent artery obstruction. The stents may produce flow redirection and disruption of the aneurysm inflow and outflow zones resulting in hemodynamic change of the parent vessel-aneurysm complex. This hemodynamic change may help to reduce coil compaction in the region of the inflow zone and prevent subsequent growth of the aneurysm. In addition, the stent potentially provides a physical matrix for endothelial growth and allows appropriate remodelling of the parent vessel along the aneurysm neck 6,9.
Complete isolation of the aneurysm from the circulation is the obvious goal of both open and endovascular treatment. In various endovascular series, complete aneurysm occlusion rates between 21% and 84% when using detachable coils are reported 12-15, the relatively broad range being explained by differences in aneurysm size and morphological composition. In particular, this might be of limited use in small acutely ruptured, wide-necked aneurysms. These small aneurysms are frequently encountered and the endovascular treatment of these lesions can be technically demanding.
Small aneurysms are also associated with an increased incidence of intraprocedural rupture 16-19. Ricolfi et Al 17 observed four procedure related perforations in small aneurysms only (4 mm or smaller diameter). Vinuela et Al 18 reported that two of three perforated aneurysms measured 3-4 mm in diameter. Small aneurysms make for challenging aneurysm catheterization, risk of dome perforation by the microcatheter, the load and jumping phenomenon, and difficulty placing multiple coils 16. In many patients with small aneurysms, it is often not possible to place more than a single coil. Therefore, approximate coil selection is very important.
As stated above, the Neuroform stent has an open-cell structure and the cells are arranged at an interval of about 2 French. In particular, care should be taken that the coil does not prolapse or migrate because the intervals between cells may be widened more than 2 French if a stent is positioned between convexities 5,20. Interventionists should always bear in mind possible coil migration. Additionally, it has been reported that stent malposition, thromboembolism, etc. are included in the complications related to stent-assisted coiling 8,11, but there is no specific report in the literature focusing on coil migration under stent-assisted endovascular treatment.
The stent-assisted coiling method may represent a therapeutic option, especially in the treatment of complex aneurysms, in which direct coiling is not considered feasible or believed to be too dangerous. However, the author did experience coil migration in stent-as-sisted embolization, and therefore thinks that the structural features of the stent should be completely understood and small coils should be used carefully.
Conclusions
The Neuroform stent represents a significantly advanced device in endovascular treatment. however, the long-term durability and safety of the occlusion of aneurysms with stents remains unsettled. Interventionists should always bear in mind possible unexpected coil migration.
Acknowledgement
The present research was conducted using the research fund of Dankook University in 2005.
References
- 1.Guglielmi G, Viñuela F, et al. Electrothrombosis of saccular aneurysms via endovascular approach, I: electrochemical basis, technique and experimental results. J Neurosurg. 1991;75:1–7. doi: 10.3171/jns.1991.75.1.0001. [DOI] [PubMed] [Google Scholar]
- 2.Guglielmi G, Viñuela F, et al. Electrothrombosis of saccular aneurysms via endovascular approach, 2: preliminary clinical experience. J Neurosurg. 1991;75:8–14. doi: 10.3171/jns.1991.75.1.0008. [DOI] [PubMed] [Google Scholar]
- 3.Molyneux A, Kerr R, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet. 2002;360(9342):1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 4.Molyneux A, Kerr RS, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366(9488):809–17. doi: 10.1016/S0140-6736(05)67214-5. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez Zubillaga A, Guglielmi G, et al. Endovascular occlusion of intracranial aneurysms with electrically detachable coils: correlation of aneurysm neck size and treatment results. Am J Neuroradiol. 1994;15:815–20. [PMC free article] [PubMed] [Google Scholar]
- 6.Fiorella D, Albuquerque FC, et al. Preliminary experience using the Neuroform stent for the treatment of cerebral aneurysms. Neurosurgery. 2004;54:6–16. doi: 10.1227/01.neu.0000097194.35781.ea. discussion 16-17. [DOI] [PubMed] [Google Scholar]
- 7.Henkes H, Fisher S, et al. Endovascular coil occlusion of 1811 intracranial aneurysms: early angiographic and clinical results. Neurosurgery. 2004;54:268–80. doi: 10.1227/01.neu.0000103221.16671.f0. discussion 280-285. [DOI] [PubMed] [Google Scholar]
- 8.Benitez RP, Silva MT, et al. Endovascular occlusion of wide-necked aneurysms with a new intracranial microstent (Neuroform) and detachable coils. Neurosurgery. 2004;54:1359–67. doi: 10.1227/01.neu.0000124484.87635.cd. discussion 1368. [DOI] [PubMed] [Google Scholar]
- 9.dos Santos Souza MP, Agid R, et al. Microstent-assisted coiling for wide-necked intracranial aneurysms. Can J Neurol Sci. 2005;32:71–81. doi: 10.1017/s0317167100016917. [DOI] [PubMed] [Google Scholar]
- 10.Henkes H, Kirsch M, et al. Coil treatment of a fusiform upper basilar trunk aneurysm with a combination of "kissing" neuroform stents, TriSpan-, 3D- and fibered coils, and permanent implantation of the microguide-wires. Neuroradiology. 2004;46:464–468. doi: 10.1007/s00234-004-1192-4. [DOI] [PubMed] [Google Scholar]
- 11.Howington JU, Hanel RA, et al. The Neuroform stent, the first microcatheter-delivered stent for use in the intracranial circulation. Neurosurgery. 2004;54:2–5. doi: 10.1227/01.neu.0000099370.05758.4d. [DOI] [PubMed] [Google Scholar]
- 12.McDougall CG, Halbach VV, et al. Endovascular treatment of basilar tip aneurysms using electrolytically detachable coils. J Neurosurg. 1996;84:393–399. doi: 10.3171/jns.1996.84.3.0393. [DOI] [PubMed] [Google Scholar]
- 13.Nichols DA, Brown RD, Jr, et al. Endovascular treatment of ruptured posterior circulation aneurysms using electrolytically detachable coils. J Neurosurg. 1997;87:374–380. doi: 10.3171/jns.1997.87.3.0374. [DOI] [PubMed] [Google Scholar]
- 14.Pierot L, Boulin A, et al. Selective occlusion of basilar artery aneurysms using controlled detachable coils: report of 35 cases. Neurosurgery. 1996;38:948–954. doi: 10.1097/00006123-199605000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Raymond J, Roy D, et al. Endovascular treatment of acutely ruptured and unruptured aneurysms of the basilar bifurcation. J Neurosurg. 1997;86:211–219. doi: 10.3171/jns.1997.86.2.0211. [DOI] [PubMed] [Google Scholar]
- 16.Goddard JK, Moran CJ, et al. Absent relationship between the coil-embolization ratio in small aneurysms treated with a single detachable coil and outcomes. Am J Neuroradiol. 2005;26:1916–1920. [PMC free article] [PubMed] [Google Scholar]
- 17.Ricolfi F, Le Geurinel C, et al. Rupture during treatment of recently embolized aneurysms with Guglielmi electrodetachable coils. Am J Neuroradiol. 1998;19:1653–1658. [PMC free article] [PubMed] [Google Scholar]
- 18.Viñuela F, Duckwiler G, et al. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 1997;86:475–482. doi: 10.3171/jns.1997.86.3.0475. [DOI] [PubMed] [Google Scholar]
- 19.Sluzewski M, Bosch JA, et al. Ruptured of intracranial aneurysms during treatment with Guglielmi detachable coils: incidence, outcome, and risk factors. J Neurosurg. 2001;94:238–240. doi: 10.3171/jns.2001.94.2.0238. [DOI] [PubMed] [Google Scholar]
- 20.Lylyk P, Ferrario A, et al. Buenos Aires experiences with the Neuroform self-expanding stent for the treatment of intracranial aneurysms. J Neurosurg. 2005;102:235–241. doi: 10.3171/jns.2005.102.2.0235. [DOI] [PubMed] [Google Scholar]