Abstract
Background
National initiatives to prevent and/or manage sickness absence require a database from which trends can be monitored.
Aims
To evaluate the information provided by surveillance schemes and publicly available datasets on sickness absence nationally from musculoskeletal disorders (MSDs).
Methods
A grey literature search was undertaken using the search engine Google, supplemented by leads from consultees from academia, industry, employers, lay interest groups and government. We abstracted data on the outcomes and populations covered, and made quantitative estimates of MSD-related sickness absence, overall and, where distinguishable, by sub-diagnosis. The coverage and limitations of each source were evaluated.
Results
Sources included the Labour Force Survey (LFS) and its Self-reported Work-related Illness survey module; the THOR-GP surveillance scheme; surveys by national and local government; surveys by employers’ organisations; and a database of benefit statistics. Each highlighted MSDs as a leading cause of sickness absence. Data limitations varied by source, but typically included lack of diagnostic detail and restriction of focus to selected subgroups (e.g. work-ascribed or benefit-awarded cases, specific employment sectors). Additionally, some surveys had very low response rates, were completed only by proxy respondents, or ranked only the perceived importance of MSD-related sickness absence, rather than measuring it.
Conclusions
National statistics on MSD-related sickness absence are piecemeal and incomplete. This limits capacity to plan and monitor national policies in an important area of public health. Simple low-cost additions to the LFS would improve the situation.
Introduction
Several prominent reviews have highlighted the benefits of work for health and the major costs of sickness absence and job loss [1-3]. Musculoskeletal disorders (MSDs) are a leading cause of these adverse vocational outcomes [4], and there is a need for reliable national statistics on their impact on work so that interventions can be planned, evaluated and optimised.
Here we outline the sources of publicly accessible data on MSD-related sickness absence nationally, describe their coverage and limitations, summarise recent findings, and evaluate the consistency of observations between sources. We also consider potential benefits from improved methods of data collection, and whether they would justify the extra costs of implementation.
Methods
To explore which national surveillance schemes and publicly available, population-based datasets provide information on MSD-related sickness absence, we combined web searching (using Google) with information from personal contacts. Relevant websites of government departments and employers’ organisations were investigated, along with other sources of data in the “grey” literature. Publications examined included: reports of the Office for National Statistics (ONS); website statistics compiled by the Department for Work and Pensions (DWP) and the Health and Safety Executive (HSE); and sickness absence surveys by the Confederation of British Industries (CBI) and the Chartered Institute of Personnel and Development (CIPD). Also, staff at ONS, HSE and DWP were contacted to explore the availability of other datasets. All searches were completed in June 2010. We shared findings with 11 European researchers and nine non-research stakeholders (occupational physicians and representatives of HSE, trades unions, employers, relevant charities and lay interest groups). Consultees completed a questionnaire concerning additional data sources, international comparisons and the perceived value of such information.
From each identifiable source one of us (KTP) abstracted the outcomes recorded, the populations to which statistics applied, and quantitative estimates of MSD-related sickness absence, overall and, where distinguishable, by subcategories of MSD. Data abstraction was checked independently and in full by ECH. The coverage and limitations of each source were assessed.
Results
Sources could be subdivided into those supplying whole-population statistics, data from selected public sector employments, and employers’ views (rather than numerical absence data).
The Labour Force Survey (LFS), which is managed by the ONS, collects information quarterly from samples of 50-60,000 private households in Great Britain. In the two-year period ending June 2006, the household-specific response rate approached two-thirds. Interviewers can accept proxy responses if the respondent is unavailable (empirical evidence suggests the approach is robust).
Questions are posed about the days that an individual has been absent from work because of illness or injury in the week of inquiry. MSDs are classified as affecting arms or hands, legs or feet, and back or neck. Respondents absent at the start or end of the reference week may have an unknown preceding or subsequent spell of absence. Thus, while providing an indication of period prevalence (MSD-related sickness absence in an index week) and the percentage of working days lost because of MSDs, the data are uninformative as regards the duration of spells of absence.
Table 1 shows that, amongst a nationally representative population sample who took sickness absence in the previous week, about 30% cited musculoskeletal problems as the main reason [6].
Table 1. Proportion of sickness absence in the reference week attributed to musculoskeletal problems: Analysis by main health problem and site(s) affected, Oct – Dec 2009 (from the Labour Force Survey [6]).
| Total days absent from work |
Proportion (%) of absence attributed to: |
|||
|---|---|---|---|---|
| Arms, hands | Legs, feet | Back or neck |
Any/all of these sites |
|
| 1 | 6.1 | 14.0 | 14.0 | 34 |
| 2 | 4.7 | 9.4 | 8.2 | 22 |
| 3 | 7.5 | 14.9 | 13.4 | 36 |
| 4 | 5.0 | 7.5 | 25.0 | 38 |
| 5 | 6.1 | 7.3 | 14.6 | 28 |
| 6 | 0.0 | 0.0 | 50.0 | 50 |
| 7 | 0.0 | 20.0 | 0.0 | 20 |
| 1-7 | 5.8% | 11.5% | 13.9% | 31% |
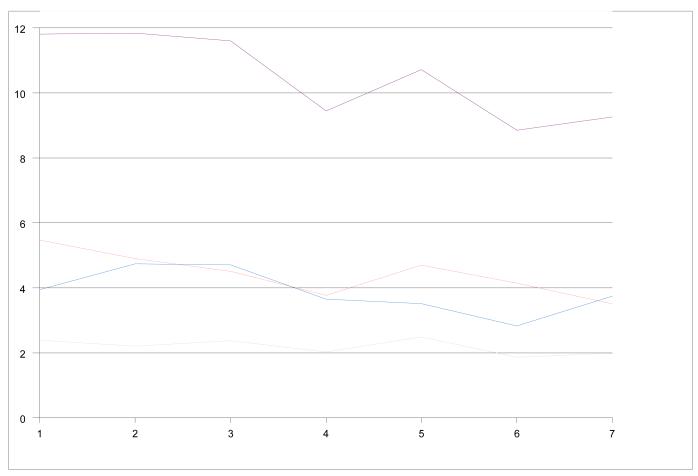
Since 1990, HSE has commissioned supplementary questions in the LFS, to track work-related illness and injury. The Workplace Injury survey module, added in 1990, was supplanted in 2003/4 by the Self-reported Work-related Illness (SWI) survey module – with broader coverage of health. The SWI module is administered annually to adults from the LFS who are or have been employed. Individuals answer a screening question: “Within the last 12 months have you suffered from any illness, disability or other physical or mental problem that was caused or made worse by your job or work done in the past?” Those responding positively are asked how many work-related illnesses they have had. Subsequent inquiries focus on the most serious work-ascribed illness, and respondents who have worked in the past 12 months are asked how much time they have taken off work during that period because of their illness. Thus, assuming that respondents accurately recall sickness absence and the underlying health problem, the data provide a lower limit on the burden of all sickness absence from MSDs, statistics being published for sickness absence attributed to MSDs of back; neck or upper limb; lower limb, and all sites combined (Figure 1 [7]).
Figure 1. Trends in sickness absence in the Labour Force SWI Survey [7].
The SWI estimated that an annual 9.26 million working days were lost in 2008/9 from self-reported work-ascribed MSDs, with back pain contributing 3.51 million lost days, neck or upper limb pain 3.75 million days, and lower limb pain 1.99 million days. Relative to 2001-2, this represents a decline of 22% overall, the fall being greatest for back pain (36%) and least for arm or neck pain (5%). The average days lost per case also declined – from 19.3 days/year in 2001-2 to 17.2 days/year in 2008-9, a fall of 11%, with a greater reduction (17%) for back pain. Numbers of cases and spells per case are not reported routinely, but the steeper decline in total days of absence than in days lost/case implies a fall in the number of cases, as well as briefer illness episodes.
In 1995/6, HSE estimated that the 9.5 million working days lost to work-related musculoskeletal disorders cost society £5.7 billion (£8 billion adjusted to 2009 prices). In principle, such costs can be estimated for other periods, but no serial index of costs is routinely published.
The Health Occupation Reporting network, general practitioner extension (THOR-GP) is an HSE-sponsored surveillance scheme, initiated in 2005, and administered by the Centre for Occupational and Environmental Health at the University of Manchester. A panel of volunteers (some 270 general practitioners with supplementary training in occupational medicine) identifies new cases of work-related ill health from their clinical practice. Reporters classify cases into disease categories and record their age, sex, job, industry, exposure, and sickness absence.
Data are available on MSD-related sickness absence which, in the reporter’s judgement, are caused or exacerbated by work [8]. An audit has revealed “a considerable level of underreporting” of sickness absence [9]: THOR-GP documents an individual’s initial spell of absence, but not routinely their subsequent spells. Detailed follow-up in a sample of cases has suggested that only about 40% of the total duration of absence is captured (J Hodgson, personal communication). In 2009, absence data were not published by diagnostic subcategory of MSD.
During 2006-08, the annual incidence of new GP consultations for work-related MSDs was estimated as 830 per 100,000 working population, with 43% of the consultations resulting in sickness certification – a rate of 357 spells per 100,000 workers per year. As each certificate was issued for an average of 9.7 days, the estimated annual loss from certified absence for work-related MSDs (not allowing for underreporting) was 3,462 days per 100,000 workers, or 2.26 million lost days across Great Britain.
The annual estimate of days lost from SWI −9.67 million for 2005/6 to 2007/8 [7] – is >4 times that from THOR-GP, in part because of the under-reporting mentioned and in part because SWI counts total sickness absence, including uncertified spells. Other factors might also contribute to the discrepancy, such as differences in attribution between doctor and patient.
The Department for Work and Pensions (DWP) collates national statistics on social security benefit, and sponsors internet tabulation tools and a Work and Pensions Longitudinal Study (WPLS), based on all benefit recipients, with further detail published for a 5% sub-sample.
Data on caseload of Incapacity Benefit (IB) are available from 1999 for the WPLS and from 1995 for the 5% sub-sample [10]. These identify cases arising from MSDs but do not distinguish sub-diagnoses. To be counted, recipients must be below state pension age when they fell ill, and most need to have paid qualifying national insurance contributions and been off sick or unable to work for ≥ 28 weeks. In 2008, 430,000 adults were in receipt of IB for a musculoskeletal reason, 59% of whom had received benefits for ≥5 years (Table 2). The caseload has fallen over the past decade and was 23% lower in 2008 than 2004, in accord with time trends in MSD-related absence estimated by the SWI.
Table 2. Caseload on Incapacity Benefit because of “diseases of the musculoskeletal system and connective tissues”, by duration of current claim [10].
| Date | 0-3 months |
3-6 months |
6-12 months |
1-2 years | 2-5 years | >5 years | All |
|---|---|---|---|---|---|---|---|
| August 2000 |
27,730 | 24,090 | 37,150 | 63,060 | 156,670 | 250,080 | 558,790 |
| August 2004 |
21,770 | 19,650 | 29,070 | 47,320 | 114,950 | 281,860 | 514,620 |
| August 2008 |
19,190 | 15,530 | 23,320 | 37,680 | 81,930 | 251,910 | 429,570 |
In October 2008, Incapacity Benefit was replaced by Employment Support Allowance, making later figures only partially comparable
The DWP also commissions ad hoc research based on its client populations. One example concerned structured interviews with 1,843 people who had claimed IB in the previous three months (47% response) [11]. Among respondents reporting a disability, the leading sites affected included the legs or feet (29%), the neck, shoulders or back (27%), and the arms or hands (19%). These problems ranked third, fourth and fifth among 17 non-mutually exclusive categories of disability.
The Cabinet Office collected data on total sickness absence, classified by ICD-9 diagnosis, across the Civil Service during 2004, 2005, 2005/6 and 2006/7. In 2006/7, 115 departments participated (almost all) [12]. Some 4.1 million working days were lost from sickness absence of all causes (in 685,000 spells at an average of 6.01 days/spell). MSDs caused 492,000 lost days, 12% of the total (in 51,000 spells). The proportion of lost days attributed to MSDs in large government departments was almost double that in small and ‘micro’ departments (Table 3). The total cost of absence was estimated at £393 million, the MSD-related contribution being £47 million.
Table 3. Working days lost across the Civil Service in the 2006/7 financial year, overall and because of musculoskeletal-related diagnoses [12].
| Departmental size (no, of departments) |
Total days lost | Days lost from MSDs |
|
|---|---|---|---|
| No. | % | ||
| >25,000 (3) | 1,870,661 | 261,641 | 14 |
| >10,000-25,000 (6) | 842,313 | 103,542 | 12 |
| >1000-10,000 (44) | 1,256,153 | 114,960 | 9 |
| 250-1000 (30) | 121,197 | 9,809 | 8 |
| <250 (32) | 27,651 | 2,068 | 7 |
| All departments (115) | 4,117,975 | 492,020 | 12% |
The Local Government Employers Association (LGE) has issued several reports on sickness absence in local government and social services [13,14]. Its 2004/2005 survey covered 107 unitary and county authorities across England and Wales (62% response), and that in 2006/2007 covered 143 local authorities (35% response). The surveys collected data on days lost per employee and converted this to an absence rate reflecting the proportion of working time lost. Similar methods were used in a survey of social service departments in 105 authorities (61% response).
MSDs were categorised into back and other musculoskeletal problems, with data supplied on the median proportion (across authorities) of all days lost and the median proportions of short- and long-term absence spells attributed to MSDs (Table 4). These indicate the relative importance of MSDs among other causes of absence but do not quantify lost work time.
Table 4. Proportion of sickness absence days and spells attributed to musculoskeletal causes across local government and social services [13,14].
| Median % (Rank§) | ||||
|---|---|---|---|---|
|
|
||||
| Local government | Social services |
|||
|
|
|
|||
| 2003/4 | 2004/5 | 2006/7 | 2004/5 | |
| All sick leave days | ||||
| Back | 8.8 (4) | 9.2 (4) | 8.7 (4) | 9.2* (4) |
| Other MSDs | 12.8 (3) | 13.3 (2) | 13.8 (2) | 12.2* (2) |
| All short-term spells | ||||
| Back | 7.6 (5) | 7.3 (5) | 7.5 (6) | - |
| Other MSDs | 8.7 (3) | 8.6 (4) | 10.9 (4) | - |
| All long-term spells | ||||
| Back | 10.1 (3) | 10.1 (3) | 9.2 (3) | - |
| Other MSDs | 19.2 (2) | 18.2 (2) | 16.7 (2) | - |
Rank across 11 potential causes
excluding figures from authorities where “other causes” of absence accounted for >25% of the total
Across local government and social services, about 9% of all sick leave days were attributed to back pain and another 12-14% to other MSDs. Thus, in both local and in central government, MSDs are leading causes of sickness absence.
The CIPD conducts an annual survey of absence management, polling human resources (HR) professionals across a range of industrial sectors. Sampling methods are not described. In 2009, 642 replies (5% response) were received from organisations employing >1.9 million people [15]. Information was obtained on causes of short-term and long-term sickness absence, with findings presented overall and by industrial sector for 13 causes of sick leave.
Absence data, separately distinguishable for back pain and other MSDs, are shown in Table 5. Information is limited to proportions of respondents citing these as major contributory causes of absence. The survey highlights the relative importance of back pain as a contributory factor as judged by HR professionals; but offers no quantitative data on the number or duration of absence spells, or working time lost. Many respondents cited MSDs amongst the leading causes of sickness absence, both in manual and in non-manual workers.
Table 5. Proportions of respondents citing musculoskeletal disorders as a major factor in sickness absence (CIPD Annual Survey Report, 2009 - Absence Management [15]).
| All (Rank§) | Manufacture | Private services |
Non-profit organisations |
Public services |
|
|---|---|---|---|---|---|
|
Back pain (short-
term) | |||||
| Manual | 55 (2*) | 60 | 51 | 42 | 65 |
| Non-manual | 40 (5) | 35 | 44 | 40 | 41 |
| Back pain (long-term) | |||||
| Manual | 53 (2) | 58 | 49 | 41 | 62 |
| Non-manual | 36 (5) | 39 | 32 | 31 | 46 |
|
Other MSDs (short-
term) | |||||
| Manual | 55 (2*) | 57 | 42 | 52 | 73 |
| Non-manual | 45 (3) | 36 | 39 | 56 | 58 |
|
Other MSDs (long-
term) | |||||
| Manual | 49 (3) | 47 | 35 | 48 | 76 |
| Non-manual | 42 (4) | 39 | 31 | 51 | 65 |
Rank across 13 potential causes
jointly. (As more than one cause may be contributory, %s total to more than 100%)
MSD - musculoskeletal disorder
The CBI (now CBI/AXA) Absence and Labour Turnover Survey has been conducted annually since 1987. In 2008, the survey was completed by managers and HR professionals from 503 private and public sector organisations, employing >1 million workers [16]. The sampling process is not described. Response rates have run at about 5% in recent times.
In 2008, information was presented on 10 leading causes of short-term and long-term sickness absence, which included the categories “back pain” and “other MSDs” (Table 6). Again, details were limited to the proportions of managers citing these as leading causes of short or long-term sickness, and no quantitative data were provided on number or duration of absence spells, or work time lost. The survey estimated an average direct cost to the employer of all sickness absence of £517 per employee/year (salary costs, replacement costs such as agency staff) or 3.1% of payroll; indirect costs, like reduced customer satisfaction, were put at £263 per employee/year. MSD-related absences were not costed separately.
Table 6. Proportions of respondents citing musculoskeletal disorders as a causal factor in sickness absence (CBI/AXA Absence and Labour Turnover Survey, 2008 [16]).
| Short term (Rank§) | Long term (Rank§) | |||
|---|---|---|---|---|
| Manual | Non- manual |
Manual | Non-manual | |
| Back pain | 67 (2) | 47 (3) | 60 (1) | 45 (4) |
| Other musculoskeletal | 50 (3) | 40 (4) | 51 (3) | 48 (3) |
Rank across 10 potential causes. (As more than one cause may be contributory, %s total to more than 100%).
EEF The manufacturers’ organisation, whose members are drawn from manufacturing, engineering and technology-based companies, conducts annual surveys on sickness absence and labour turnover. In its 2010 report, responses were analysed from 498 member organisations with 99,591 employees (20% response) [17]. Most respondents (79%) came from small or medium-sized organisations.
Absence rates and total days lost were estimated by industry, social class and size of employer. Information on absence by cause, however, was restricted to questions seeking the three main causes of short-term and long-term absence. “Back pain and other joint/muscular problems” was cited as the second most common cause of both short- and long-term absence.
The CIPD (Table 5), CBI/AXA (Table 6), and EEF surveys have different sampling frames, but have generated similar rankings by managers, a perspective shared with managers from local government and social services (Table 4).
Recent EEF surveys have recorded a downward trend in companies citing back pain as a leading cause, but no similar trend for other MSDs – perhaps in part because medical guidance from the 1990s has improved the management of back pain.
Discussion
Our study found differences in the recording of sickness absence by different organisations. Surveys collected data by different methods with differing timeframes of inquiry and suffered differing limitations. Our findings support the comments by Bevan et al (2007) [18], for the Work Foundation, that: “the recording of sickness absence is rarely accurate”. In some surveys, the data came from employees or their physicians, but in others from proxy respondents. Surveys that relied on workers’ recall may not have been accurate in the days lost or their attribution, while employer surveys were limited by the poor quality of data held. In surveys that quantified lost working time, differences may have arisen in how non-working and partially lost work days were counted – no detail was given. Very poor response rates in employer surveys will have rendered them prone to response bias (perhaps with returns completed only by those with good recording systems), while the sampling frames in some surveys are unlikely to have been nationally representative. Some sources ranked the importance of MSDs as a cause of absence without enumerating days lost, and some restricted interest only to work-attributed instances or to narrow sectors of employment. Noteworthy shortcomings included sparse information on time trends and a want of diagnostic detail (e.g. no data on absence rates for osteoarthritis, rheumatoid arthritis, inflammatory arthritis, upper limb disorders etc).
In sum, the UK national statistics on musculoskeletal sickness absence are fragmentary and incomplete; there is no one-stop comprehensive data source. Our findings suggest a problem that is huge in scale, costly, and dominated by back pain, and offer several pointers on time trends; but they lack detail and flexibility to address specific research and policy questions.
Our grey literature search may not have been fully comprehensive. However, Holmes, in conducting a similar exercise in 2008, noted similar limitations [19]; and our consultees were unable to identify additional UK-based national datasets that we had overlooked.
It seems that the situation is not dissimilar in other countries. Responses from contacts identified through our stakeholder consultation, in Denmark, the Netherlands, Australia, Canada, New Zealand and France, were consistent with this view, which was supported also by a comprehensive report of the European Agency for Safety and Health at Work [20] and contact with its author (Elke Schneider, personal communication). Common limitations internationally include restriction of focus to compensable or occupationally-caused cases, and inability to discriminate by diagnosis.
The benefits of collecting more detail need to be weighed against costs, with a view as to purpose. Consultees of our review saw the main purposes as to plan and monitor national policies in an economically important area of public health. Thus, want of such information makes it difficult to target preventive interventions optimally, to monitor their impact, to judge the required scale of treatment and rehabilitation services, and to follow trends arising from changing demography. Stakeholders’ concerns were amplified by the context of MSDs as major causes of lost work productivity, of unemployment and claims for incapacity benefits, and of pain and disability.
However, as one consultee observed, although better statistics inform national policy, they do not necessarily lead to better interventions. Proposals for improved data collection need to be evaluated carefully to ensure that the costs entailed will be justified by the benefits from the additional information.
In the current economic climate, improvement of existing datasets is more attractive than development of a new national system of data collection. The improvement that might give best value for money would be to augment the LFS with a question about when the participant last attended work, giving various response options ranging, say, from “within the past week” to “not within the past six months”. This would allow sickness absence rates to be broken down by duration, a useful refinement because the management of long-term absence differs from that of short absences. In addition, data on absences of >6 months could be compared with those on benefit awards, by way of triangulation.
In addition, DWP’s planned electronic fit-note [20] should allow rapid collation of national data on certified sickness absence by cause. Its value, however, will depend on the accuracy and completeness with which information is entered: an early priority will be to assess this, and if necessary to improve the quality of record-keeping.
Beyond this, we do not envisage any changes to routine data systems that could readily be justified. In particular, it seems unlikely that detailed diagnostic information on spells of sickness absence could be routinely obtained with sufficient accuracy to be useful, other than at prohibitive cost. However, consideration should be given to one-off targeted research projects to address specific policy questions. For example, if there were a need to estimate the economic impact of sickness absence from severe hip osteoarthritis or rheumatoid arthritis, this could be accomplished by surveying representative samples of patients.
Key messages.
National statistics on MSD-related sickness absence are fragmentary, with many gaps and limitations.
This limits capacity to plan and monitor national policies on prevention and case management
Simple low-cost additions to the Labour Force Survey can improve the situation.
Acknowledgements
This study was funded by the research charity Arthritis Research UK. We thank the following for their comments: Kim Burton, Peter Buckle, Peter Croft, Gary Macfarlane, Ira Madan, Chris Main, Eira Viikari-Juntura, Alex Burdorf, Sigurd Mikkelsen, Jos Verbeek, Bart Koes, Karen Walker-Bone (research active consultees); John Osman and David Lewis (HSE); Hugh Robertson (TUC); Cynthia Atwell (RCN); Margaret Barrett (NHS Confederation); Siobbain McCurrach (Arthritis Care); Olivia Carlton (Transport for London); Su Wang (independent practitioner); and Alan Silman (Arthritis Research UK).
References
- 1.National Institute for Health and Clinical Excellence . Managing Long-Term Sickness Absence and Incapacity for Work. NICE publications; London: [accessed 3/2/11]. 2009. NICE public health guidance 19. http://www.nice.org.uk/nicemedia/pdf/PH19Guidance.pdf. [Google Scholar]
- 2.Black C. Working for a healthier tomorrow. The Stationery Office; London: [accessed 3/2/11]. 2008. Dame Carol Black’s Review of the health of Britain’s working age population. ISBN 978011702513 4. http://www.dwp.gov.uk/docs/hwwb-working-for-a-healthier-tomorrow.pdf. [Google Scholar]
- 3.Boorman S. NHS Health and Well-being. Final Report. COI for Department of Health; London: [3/2/11]. Nov, 2009. 2009 http://www.nhshealthandwellbeing.org/pdfs/NHS%20Staff%20H&WB%20Review%20Final%20Report%20VFinal%2020-11-09.pdf. [Google Scholar]
- 4.Waddell G, Aylward M, Sawney P. Economic and Social Data Service Nesstar Catalogue. Royal Society of Medicine Press; London: [accessed 3/2/11]. 2002. Back pain, incapacity for work and social security benefits: an international literature review and analysis. http://nesstar.esds.ac.uk/webview/ [Google Scholar]
- 5. [3 February 201, date last accessed];Economic and Social Data Service Nesstar Catalogue. http://nesstar.esds.ac.uk/webview/
- 6.Health and Safety Executive [accessed 3/2/11];Self-reported work-related illness (SWI) and workplace injuries: Results from the Labour Force Survey (LFS) Index of tables. http://www.hse.gov.uk/statistics/lfs/0809/swit1.htm.
- 7.Health and Safety Executive [accessed 3/2/11];THOR - Voluntary reporting of occupational diseases by specialist doctors: Index of THOR tables. http://www.hse.gov.uk/statistics/tables/index.htm#thor.
- 8.Health and Safety Executive [accessed 23/3/11];Voluntary reporting of occupational diseases by General Practitioners (THOR GP) http://www.hse.gov.uk/statistics/sources.htm#odin.
- 9.Department for Work and Pensions [accessed 3/2/11];Tabulation Tool. http://83.244.183.180/100pc/tabtool.html.
- 10.Kemp P, Davidson J. [accessed 08/10/10];Routes onto Incapacity Benefit: Findings from a survey of recent claimants. DWP Research Report no 469. 2007 :47–61. chapter 4. http://research.dwp.gov.uk/asd/asd5/rports2007-2008/rrep469.pdf.
- 11.Cabinet Office [accessed 3/2/11];Analysis of Sickness Absence in the Civil Service. 2006-7 http://www.civilservice.gov.uk/Assets/Sickness_Absence_2006to2007_tcm6-2515.pdf.
- 12.Employer’s Organisation for Local Government [accessed 3/2/11];Sickness Absence in Social Services. 2004/2005 http://www.lge.gov.uk/lge/aio/55057.
- 13.Local Government Association [accessed 3/2/11];Local Government Sickness Absence Levels and Causes Survey. 2006-2007 http://www.lga.gov.uk/lga/aio/1098656.
- 14.Chartered Institute of Personnel and Development [accessed 3/2/11];Absence Management Annual Survey Report. 2009 http://www.cipd.co.uk/subjects/hrpract/absence/_absence_management_summary.htm?IsSrchRes=1.
- 15.CBI/AXA [accessed 3/2/11];At work and working well? CBI/AXA Absence and Labour Turnover Survey. 2008 http://www.personneltoday.com/assets/getasset.aspx?ItemID=6457.
- 16.EEF [accessed 3/2/11];Sickness Absence and Rehabilitation Survey. 2010 http://www.eef.org.uk/publications/surveys/Sickness-Absence-and-Rehabilitation-Survey-2010.htm.
- 17.Bevan S, Passmore E, Mahdon M. Fit for Work? Musculoskeletal Disorders and Labour Market Participation. The Work Foundation; London: [accessed 3/2/11]. 2007. http://www.theworkfoundation.com/assets/docs/publications/44_fit_for_work_ small.pdf. [Google Scholar]
- 18.Holmes E. [accessed 3/2/11];The feasibility of comparing sickness absence surveys and the Labour Force Survey. HSE Contract Research Report RR673. 2008 http://www.hse.gov.uk/research/rrpdf/rr673.pdf.
- 19.Schneider E, Irastorza X. European Agency for Safety and Health at Work. OSH in figures: Work-related musculoskeletal disorders in the EU — Facts and figures. Publications Office of the European Union; Luxembourg: [3/2/11]. 2010. ISBN 978-92-9191-261-2. http://osha.europa.eu/en/publications/reports/TERO09009ENC. [Google Scholar]
- 20.Carvel J. [accessed 3/2/11];Government to replace sick notes with ‘fit notes’. Society Guardian. 2008 Nov 26th; http://www.guardian.co.uk/society/2008/nov/26/nhs-health-sick-notes-fit-notes.