Abstract
Recent studies have shown that rates of depression and anxiety symptoms are elevated among individuals with autism spectrum disorders (ASDs) of various ages and IQs and that depression/anxiety symptoms are associated with higher IQ and fewer ASD symptoms. In this study which examined correlates of depression and anxiety symptoms in the full school-age range of children and adolescents (age 6-18) with ASDs and IQs ≥ 70 (n=95), we also observed elevated rates of depression/anxiety symptoms, but we did not find higher IQ or fewer ASD symptoms among individuals with ASDs and depression or anxiety symptoms. These findings indicate an increased risk for depression/anxiety symptoms in children and adolescents with ASDs without intellectual disability, regardless of age, IQ, or ASD symptoms.
Keywords: autism, children, adolescents, depression, anxiety, IQ
1. Introduction
Children with autism spectrum disorders (ASDs) have weaknesses in social reciprocity, communication, and repetitive behaviors (American Psychiatric Association, 2000). Psychiatric co-morbidities are prevalent, with secondary psychopathology occurring in as many as 72% of children with ASDs (Leyfer et al., 2006). Depression and anxiety are among the most common ASD co-morbidities (e.g., Siminoff et al., 2008), and have been shown to relate to significantly poorer life functioning (Mattila et al., 2010). Emotional co-morbidities may also increase the core symptoms of ASDs (Matson & Nebel-Schwalm, 2006; Perry, Martson, Hinder, Munden & Roy., 2001). There is growing interest in understanding the nature of depression and anxiety in ASDs (e.g., White, Oswald Ollendick & Scahill, 2009; Whitehouse, Durkin, Jaquet & Ziatas, 2009), including exploring potential profiles of vulnerability and contributory factors.
Several studies have reported associations between age and emotional symptoms in children with ASDs. For example, Ghaziuddin, Weidmer-Mikhail & Ghaziuddin (1998) reported clinical observations of increased rates of depression for young people with ASDs as they entered adolescence. In a study of young people with ASDs, without intellectual disability, higher age related to lower self-perceived social competence, which in turn related to increased self-reported depression symptoms (Vickerstaff, Heriot, Wong, Lopes & Dossetor, 2007). Higher age also correlated with elevated parent-ratings of anxiety for children and adolescents with ASDs and a broad range of IQs (Lecavalier, 2006).
Several studies have specifically investigated the relationship between IQ, autism symptoms, and depression and/or anxiety in ASDs (Bellini, 2004; Burnette et al., 2005; Cederlund, Hagberg & Gillberg, 2010; Mazurek & Kanne, 2010; Sterling, Dawson, Estes & Greenson, 2008; Sukhodolsky et al., 2008; Vickerstaff et al., 2007; Weisbrot, Gadow, DeVincent & Pomeroy, 2005). A large study of children and adolescents with ASDs and a broad range of intellectual functioning showed higher IQ and fewer autism symptoms related to greater parent report of anxiety and depression (Mazurek & Kanne, 2010). This same pattern was observed in adults with ASDs and a broad range of IQ regarding depression assessed by a clinician, and the relationship remained when participants with intellectual disability were removed from the analyses (Sterling et al., 2008). A second study of young adults, ages 16-36, without intellectual disability did not duplicate the relationship (Cederlund et al., 2010); the authors considered whether the high level of parent support might have skewed their findings.
A potential link between greater self-awareness of one's social difficulties and depression was first suggested by Wing (1992), who noted that young people with ASDs who are sufficiently self-aware to realize their social struggles are likely to experience increased emotional pain over their social failures. One study reported higher IQ and fewer autism symptoms to relate to increased self-awareness in adolescents with ASDs; the authors suggested that findings of relationships between IQ, autism symptoms, and emotional difficulties might reflect the impact of self-awareness on emotional functioning (Sterling et al., 2008). Self-awareness deficits may also skew self-report of emotional symptoms, as seen when parents endorse significantly greater emotional symptoms than their children report (e.g., Vickerstaff et al., 2007). In one study comparing parent ratings and child self-report of emotional symptoms, self-ratings were in the non-clinical (normal) range, while parent report was significantly elevated (Nicpon, Doobay, Assouline, 2010), although this finding is not universal (e.g., Hurtig et al., 2009).
To fully understand the relationship of age to emotional symptoms in higher functioning ASD it is helpful to study a group with an adequate number of children across a wide age range. While providing important insight into the relationship of intelligence and age to emotional symptoms in ASDs, previous studies have not yet investigated the role of age in a sample that spans from childhood through adolescence in children with ASD and IQ over 69. The present study examines reported relationships between age, IQ, autism symptoms and parent-rated depression and anxiety symptoms, previously unexamined in the full school-age range of children and adolescents with ASDs (ages 6-18) and IQs ≥ 70. Building on previous research findings, we hypothesized:
Levels of depression and anxiety symptoms in our sample will exceed those found in the normative standardization sample.
Higher age will relate to increased emotional symptoms.
Higher IQ will relate to increased emotional symptoms. As increased age and IQ have been suggested to relate to greater self-awareness of social difficulties and greater depression, we further hypothesized that as age increases, the relationship between higher IQ and increased emotional symptoms will increase.
Fewer autism symptoms will relate to increased emotional symptoms. As with IQ, we hypothesized that with higher age, the relationship between fewer autism symptoms and increased emotional symptoms will increase.
2. Methods and Measures
1.1 Methods
Participants consisted of 95 children and adolescents with IQ ≥ 70 (age 6-12, n = 54; age 13-18, n = 41), who were diagnosed with an autism spectrum disorder based on expert clinical impression using the DSM-IV (APA, 1994). These children were drawn from a pool of individuals who were sequentially referred for clinical services through a multidisciplinary autism clinic in Washington, DC. All participants also met criteria for a ‘broad ASD’ on the ADI or ADI-R (Le Couteur et al., 1989; Lord, Rutter & Couteur, 1994) and/or the ADOS (Lord, Rutter & DiLavore, 2000) according to the criteria established by the NICHD/NIDCD Collaborative Programs for Excellence in Autism (see Lainhart et al., 2006). The group's mean full scale IQ was in the average range (M = 105, SD = 17, range = 71-144) as measured by the Wechsler Intelligence Scale for Children-4th Edition (WISC-IV) or the Wechsler Abbreviated Scale of Intelligence (WASI) (Wechsler, 1999, 2003). Trained research-reliable staff administered all in-vivo measures. Participants with evidence of a neurological or a known genetic disorder were excluded. Participant characteristics (i.e., age, gender ratio, IQ, and autism symptomatology) for depression, non-depression, anxiety, and non-anxiety symptom groups (see details on determination of groupings below) are presented in Table 1. Data were obtained as part of an IRB approved protocol.
Table 1. Comparing characteristics of depression versus non-depression groups and anxiety versus non-anxiety groups.
| Total Sample Mean (SD) | Depression CBCL T>64 (n=42) | Depression CBCL T<65 (n=53) | t-value | P | Anxiety CBCL T>64 (n=53) | Anxiety CBCL T<65 (n=42) | t-value | P | |
|---|---|---|---|---|---|---|---|---|---|
| Age | 11.67 (3.4) | 11.78 (3.27) | 11.58 (3.53) | -.28 | .25 | 11.65 (3.47) | 11.70 (3.36) | .06 | .95 |
| Gender (%M %F) | 86%M 14%F | 90%M 10%F | 83%M 17%F | -- | -- | 96%M 4%F | 75%M 25%F | -- | -- |
| Verbal Ability | 10.71 (3.91) | 10.95 (3.03) | 10.51 (4.51) | -.55 | .59 | 10.68 (3.46) | 10.74 (4.46) | .07 | .94 |
| Nonverbal Ability | 10.97 (3.05) | 10.86 (2.44) | 11.06 (3.48) | .32 | .75 | 10.62 (3.07) | 11.40 (3.0) | 1.25 | .22 |
| Full Scale IQ | 104.87 (16.97) | 105.31 (13.67) | 104.53 (19.31) | -.22 | .83 | 103.79 (15.07) | 106.23 (19.20) | .70 | .49 |
| ADOS Comm. | 3.68 (2.15) | 3.39 (2.16) | 3.95 (2.14) | 1.13 | .26 | 3.93 (2.11) | 3.35 (2.20) | -1.17 | .25 |
| ADOS Social | 8.21 (3.28) | 7.74 (3.33) | 8.67 (3.20) | 1.25 | .22 | 8.37 (3.48) | 8.00 (3.04) | -.49 | .62 |
| ADOS Soc.+ Comm. | 11.88 (4.99) | 11.13 (5.01) | 12.62 (4.93) | 1.31 | .19 | 12.30 (5.12) | 11.35 (4.85) | -.83 | .41 |
| ADOS Stereotyped | 1.77 (1.67) | 1.45 (1.64) | 2.08 (1.66) | 1.67 | .10 | 1.91 (1.90) | 1.59 (1.33) | -.83 | .41 |
1.2 Measures
Emotional Symptoms Measure
Depression and anxiety symptoms were assessed with the Child Behavior Checklist (CBCL) for ages 6-18 (Achenbach & Rescorla, 2001). The CBCL is a standardized parent report questionnaire of child/adolescent behavioral and emotional functioning. Scores are provided for DSM-IV-oriented categories, including affective problems and anxiety problems. Items making up the affective problems domain overlap with DSM-IV diagnostic criteria for depressive disorder. Scores are presented as standardized T scores (M=50, SD=10), with cutoffs for borderline clinical range (64<T<70) and clinical range (T>69). Higher scores are indicative of greater problems. For group analyses, individuals without significant depression symptoms were defined as T<65 and individuals with elevated depression symptoms were T>64. The same cutoffs were used to differentiate those without significant anxiety symptoms (T<65) from those with elevated anxiety symptoms (T>64). All group analyses were repeated using the CBCL clinical range cut point with groups of individuals falling below clinical depression or anxiety symptom levels (T<70) and groups with clinical range depression or anxiety symptoms (T>69).
Verbal and Nonverbal Ability Measures
Full Scale IQ (FSIQ), Verbal Ability, and Nonverbal Ability were assessed using subtests from one of two intelligence scales, the WISC-IV (n = 54) or the WASI (n = 41). To create comparable cross test domain scores, Verbal ability was estimated using the Vocabulary subtest and Nonverbal Ability was estimated using the Block Design subtest. According to Sattler and Dumont (2004), the Vocabulary subtest contributes significantly to the verbal scale with an average loading of .80. Similarly, the Block Design subtest contributes substantially to the perceptual scale, with an average loading of .65. FSIQ estimate was created by averaging the Vocabulary and Block Design subtests. FSIQ, Verbal Ability, and Nonverbal Ability are presented for elevated depression symptom, non-elevated depression symptom, elevated anxiety symptom, and non-elevated anxiety symptom groups in norm-referenced standardized scores (FSIQ M = 100, SD = 15; Verbal Ability and Nonverbal Ability M = 10, SD = 3; Table 1).
Autism Diagnostic Measures
Autism symptoms were assessed through the Autism Diagnostic Interview and the Autism Diagnostic Observation Schedule (ADI/ADI-R; ADOS). The ADI/ADI-R (LeCouteur et al., 1989; Lord et al., 1994) is a detailed parent or primary caregiver interview of developmental history and autism symptoms. Scores are aggregated into symptom clusters that correspond to DSM-IV criteria for a diagnosis of autism. The ADOS (Lord et al., 2000) is a structured play and conversational interview that includes a series of social presses and other opportunities to elicit symptoms of an ASD. Scores for each domain are tallied and presented as non-standardized raw scores. Higher scores are indicative of more autism symptoms. The ADOS is the most widely-used gold-standard measure of in vivo autism symptomotology.
3. Results
3.1 Hypothesis I: Rates of Emotional Symptoms
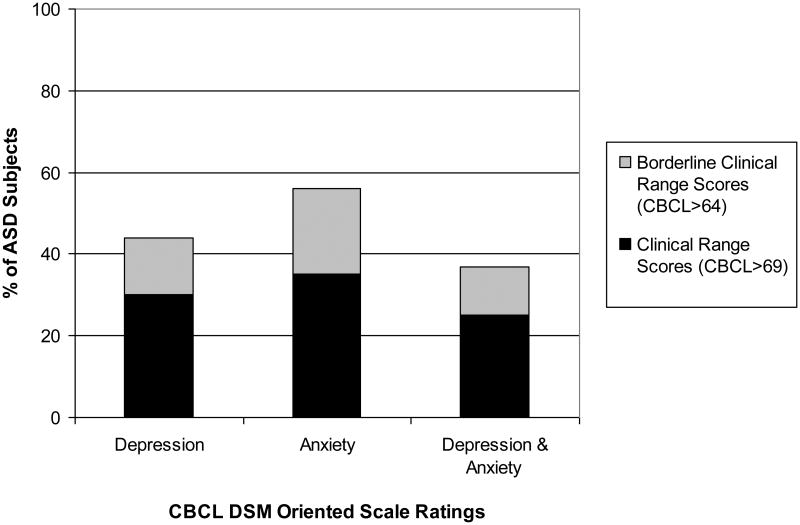
The percentages of subjects with ASDs who met CBCL cut-offs for elevated depression or anxiety symptoms are indicated in Table 1. The data confirmed our hypothesis that rates of depression and anxiety symptoms in our sample would exceed those in the general population. Standard scores (T scores) were used to compare levels of this ASD group's depression and anxiety symptoms with the CBCL standardization sample (T=50) using a one-sample t-test. As depicted in Figure 1, 44% of our sample was in the borderline or clinical range for depression symptoms and 56% in the borderline or clinical range for anxiety symptoms. Thirty percent of our sample was in the clinical range for depression symptoms and 35% was in the clinical range for anxiety symptoms. Thirty seven percent of our sample was in the borderline or clinical range for both anxiety and depression symptoms. Twenty percent of our sample was in the clinical range for both depression and anxiety symptoms, revealing that more than half of those subjects who were in the clinical range for either type of emotional symptom (depression or anxiety) were also in the clinical range for the other type of emotional symptom. Groups for independent sample t-test analyses below were well-balanced, with nearly half of the sample in the borderline/clinical range depression symptoms group and slightly more than half in the borderline/clinical range anxiety symptoms.
Figure 1. Percentage of Subjects with Depression and Anxiety Symptoms.
3.2 Hypothesis II: Emotional Symptoms and Age
The data did not confirm our hypothesis that levels of depression and anxiety symptoms would be greater in adolescence. No differences were found when comparing the mean age of the elevated depression symptoms subjects versus the non-elevated depression symptoms subjects and the elevated anxiety symptoms subjects and the non-elevated anxiety symptoms subjects using independent samples t-tests (Table 1). These tests were repeated with more stringent inclusion criteria for the clinical-range depression/anxiety symptoms groups (CBCL T<70 = subjects without clinical range depression/anxiety symptoms; CBCL T>69 = subjects with clinical range depression/anxiety symptoms), with no change in results. Pearson correlations were conducted in order to investigate the hypothesized relationship between age and emotional symptoms continuously. No significant relationships between age and emotional symptoms were observed for depression or anxiety symptoms (Table 2).
Table 2.
Correlations between age or age interactions and depression and anxiety symptoms.
| Depression | Anxiety | |
|---|---|---|
| Age1 | .03 | -.05 |
| Age × Verbal Ability1 | -.00 | -.09 |
| Age × Nonverbal Ability1 | -.03 | -.14 |
| Age × FSIQ estimate1 | .03 | -.11 |
| Age × ADOS Comm.2 | -.00 | .04 |
| Age × ADOS Soc.2 | -.05 | .01 |
| Age × ADOS Soc.+ Comm.2 | -.05 | .01 |
| Age × ADOS Stereotyped2 | -.17 | -.02 |
Note: n=95 for IQ scores; n=77 for autism symptoms.
= Pearson correlation;
= Spearman correlation.
3.3 Hypothesis III: Emotional Symptoms and Cognitive Ability
No significant relationship between cognitive ability and emotional symptoms was observed for the sample as a whole. Independent samples t-tests comparing elevated depression symptoms subjects versus non-elevated depression symptoms subjects and elevated anxiety symptoms subjects versus non-elevated anxiety symptoms subjects revealed no differences in Full Scale IQ, Verbal Ability, or Nonverbal Ability (Table 1). As before, the tests were repeated with more stringent inclusion criteria for the clinical-range depression/anxiety symptoms groups with no change in results.
The data also did not support our hypothesis that a relationship between IQ and emotional symptoms would increase during development. Pearson correlations were conducted between the interaction of age and cognitive ability (Age × IQ) and emotional symptoms, with no significant relationships observed for Age × FSIQ, Age × Verbal Ability, or Age × Nonverbal Ability with emotional symptoms (Table 2).
3.4 Hypothesis IV: Emotional Symptoms and Autism Symptoms
The length of time between ADOS and CBCL administration for 18 subjects exceeded one year. These subjects did not differ from other subjects in age, IQ, autism symptoms, or emotional symptoms and were removed from all comparisons between ADOS and CBCL variables. No significant relationship between levels of autism symptoms and emotional symptoms was observed (Table 1). Independent samples t-tests comparing elevated depression symptoms subjects versus non-elevated depression symptoms subjects and elevated anxiety symptoms subjects versus non-elevated anxiety symptoms subjects found no differences in scores for the four ADOS domains. As before, the tests were repeated with more stringent inclusion criteria for the depression/anxiety symptoms groups with no change in results.
The data did not support the hypothesis that a relationship between autism symptoms and emotional symptoms would increase during development. Spearman correlations conducted between the interaction of age and autism symptoms (Age × ADOS Domains) with emotional symptoms showed no significant relationship between Age × Communication and Depression, Age × Social and Depression, Age × Comm.+Soc. and Depression, Age × Stereotyped and Depression, Age × Communication and Anxiety, Age × Social and Anxiety, Age × Comm.+Soc. and Anxiety, or Age × Stereotyped and Anxiety (Table 2).
3.5 Psychopharmacology
Twenty percent of our subjects were on medications targeting emotional functioning (anti-depressant, anti-anxiety medication, and/or mood stabilizer). Of those who were on such medications, 40% showed clinical range depression symptoms (CBCL T>69) and 40% showed clinical range anxiety symptoms (CBCL T>69). So as to explore the potential impact of psychopharmacological interventions on the analyses, all subjects taking anti-depressants, anti-anxiety medications, and/or mood stabilizers were removed and the analyses were repeated. No changes in findings were observed.
4. Discussion
The current study examined the relationships between age, IQ, autism symptoms and parent-reported depression and anxiety symptoms, relationships which have previously been unexamined in the full school-age range of children and adolescents with ASDs and IQs ≥ 70. As in previous studies of children and adolescents with ASDs, our sample of subjects showed highly elevated rates of depression and anxiety symptoms as reported by parents. Forty four percent of our sample had borderline or clinical levels of depression symptoms and 30% had symptom levels in the clinical range. This parallels findings in the psychiatric literature in which rates of depression in ASD exceed rates of the general population. It has been estimated that 6% of the general population of children and adolescents has depression (Shaffer et al., 1996), compared to 37% of children with ASDs, as reported by one author (Ghaziuddin et al., 1998). Even more common in our sample was parent report of anxiety symptoms, with 56% in the borderline or clinical range and 35% in the clinical range. As with depression symptoms, levels of anxiety symptoms far exceeded estimates of anxiety occurring in the general population (approximately 24%) (Schaffer et al., 1996). With almost half of our sample at risk for depression and more than half at risk for anxiety, our findings add to a growing literature marking emotional problems as primary assessment and intervention targets for children and adolescents with ASDs and IQs greater than 69. Untreated emotional problems in childhood often persist into adulthood (Bruce et al., 2005; Pine, Cohen, Gurley, Brook & Ma, 1998), and studies report high rates of emotional difficulties among adults with ASDs (Hofvander et al., 2009; Sterling et al., 2008).
We did not find, as previously suggested by some authors, emotional difficulties increasing with age (Ghaziuddin et al., 1998; Lecavalier, 2006). It is notable that our sample spanned a wide range of ages (6-18), with an even distribution of children and adolescents. We would have expected such a broad age span to reveal an age effect if one had been present. Ours is not the first study to find no significant relationship between age and emotional symptoms (e.g., Sukhodolsky et al., 2008). In one study, higher age was shown to relate to more negative (and probably realistic) self-rating of social competence, which in turn related to greater self-reported emotional symptoms (Vickerstaff et al., 2007). It has been suggested that whereas adolescents with ASDs may be able to report some of their difficulties, children with ASDs often cannot do so (Ehlers & Gillberg, 1996, as cited by Kuusikoo et al., 2008). Our parents reported that their pre-adolescent children had as many emotional problems as adolescents. This makes sense clinically, as although children with ASDs may not talk about depression or anxiety symptoms as much as ASD teens, they certainly struggle emotionally. Our use of parent report of emotional symptoms, as opposed to self-report, may have avoided a potentially false age effect and captured emotional symptoms more accurately across the age span.
We also did not find increased IQ or fewer autism symptoms relating to more emotional symptoms, as reported in some prior studies (Sterling et al., 2008; Lecavalier 2006; Mazurek & Kanne, 2010; Sukhodolsky et al., 2008), but not all (Cederlund et al., 2010). In contrast to the current study, the Mazurek and Kanne and the Lecavalier samples consisted of children and adolescents with a broad range of intellectual abilities. It is possible that including children with intellectual disability is responsible for the discrepancy in findings, as differences in emotional functioning between children with and without intellectual disability have been observed, where children with IQs ≤ 70 present with less parent reported anxiety symptoms than those with IQs > 70 (Sukhodolsky et al., 2008). However, Sukhodolsky et al. controlled for differences in intellectual functioning in their analyses of subjects with a broad range of IQ, and their finding of higher IQ relating to increased anxiety remained. It is notable, however, that the Sukhodolsky et al. sample consisted of children with ASDs and severe behavioral issues (tantrums, aggression, and self-injurious behaviors). Sterling et al. found higher IQ and fewer autism symptoms relating to self-report of depression in adults with ASDs, even when removing those subjects with lower than average IQ. Notably, their sample was significantly older than ours and relied on self-report of symptoms, which may have been impacted by the level of functioning/self-awareness of the participants.
This study had several limitations. Although parent report may be our best quick means of quantifying the emotional functioning of children and adolescents with ASDs, and was useful for side stepping impaired self-report abilities in children with ASD, parents may have difficulty differentiating emotional and autism symptoms. Future studies should include self-reports and teacher reports. Additionally, the factor structure and validity of CBCL domains in ASD populations have yet to be articulated for school age children. Another limitation was the use of standardization sample norms instead of a control group. We were not able to match subjects to controls on IQ and other parameters. When addressing age effects we relied on cross-sectional correlations with age rather than the more powerful within subject, longitudinal design. Future longitudinal studies are needed to definitively answer the questions surrounding changes in emotional symptoms across development in ASDs. Finally, although the study considered the potential impact of psychopharmacological medications on the analyses, we did not explore other interventions the children might have received or the impact of comorbid symptomology (e.g. attention/impulsivity symptoms). As remediation of comorbid psychopathology is the ultimate goal, future studies should account for the impact of intervention on emotional functioning.
In spite of the limitations, the current study provides several important findings from a well-characterized group of 95 children and adolescents with ASDs and IQs ≥ 70. This study extends previous studies, as our sample contained the full school-age range of ASD children and adolescents with IQs ≥ 70. High rates of both depression and anxiety symptoms replicate previous findings. A lack of relationship between age and parent reported emotional problems calls into question the suggestion that younger children with ASDs have fewer emotional difficulties. Similarly, a lack of observed relationship between IQ or level of autism symptoms and emotional problems suggests that all ASD children without intellectual disability are at risk for emotional difficulties. The findings of this paper indicate that it is important to screen all higher functioning children and adolescents with ASD for symptoms of anxiety and depression, regardless of age or intelligence level.
Research Highlights.
We assessed the relationships between age, IQ, and autism symptoms and emotional symptoms in children and adolescents with autism spectrum disorders and no intellectual disability. Elevated rates of depression and anxiety were observed, independent of age, IQ, and autism symptoms.
Acknowledgments
This work was supported in part by the Intramural Research Program of the NIH, National Institute of Mental Health, the Isadore and Bertha Gudelsky Family Foundation, The Singer Family Foundation, The Intellectual and Developmental Disabilities Research Center at Children’s National Medical Center (NIH IDDRC P30HD406H), The General Clinical Research Center (NIH GCRCM01-RR13297), and the Studies to Advance Autism Research and Treatment Network (NIMHU54MH066417). We thank the children and families that provided data for the current study. We thank the entire Center for Autism Spectrum Disorders research team at Children's National Medical Center for their feedback on data analysis and interpretation. There are no conflicts of interest, financial or otherwise, for the authors involved directly or indirectly with this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research center for Children, Youth, & Families; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th text rev. ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorder. Focus on Autism and Other Developmental Disabilities. 2004;19:78–86. [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, et al. Keller MB. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. American Journal of Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette CP, Mundy PC, Meyer JA, Sutton SK, Vaughan AE, Charak D. Weak central coherence and its relations to theory of min and anxiety in autism. Journal of Autism and Developmental Disorders. 2005;35:63–73. doi: 10.1007/s10803-004-1035-5. [DOI] [PubMed] [Google Scholar]
- Cederlund M, Hagberg B, Gillberg C. Asperger syndrome in adolescent and young adult males: Interview, self-and parent assessment of social, emotional, and cognitive problems. Research in Developmental Disabilities. 2010;31:287–298. doi: 10.1016/j.ridd.2009.09.006. [DOI] [PubMed] [Google Scholar]
- Ehlers S, Gillberg C. Aspergerin syndrooma-yleiskatsaus l painos. Helsinki: Suomen Autismiyhdistys, Yliopistopaino; 1996. [Google Scholar]
- Ghaziuddin M, Weidmer-Mikhail E, Ghaziuddin N. Comorbidity of Asperger syndrome: a preliminary report. Journal of Intellectual Disability and Research. 1998;42:279–283. doi: 10.1111/j.1365-2788.1998.tb01647.x. [DOI] [PubMed] [Google Scholar]
- Hofvander B, Delorme R, Chaste P, Nydén A, Wentz E, Ståhlberg O, et al. Leboyer M. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry. 2009 doi: 10.1186/1471-244X-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurtig T, Kuusikko S, Mattila M, Haapsamo H, Ebeling H, Jussila K, et al. Moilanen I. Multi-informant reports of psychiatric symptoms among high-functioning adolescents with Asperger syndrome or autism. Autism. 2009;13:583–598. doi: 10.1177/1362361309335719. [DOI] [PubMed] [Google Scholar]
- Kuusikko S, Pollock-Wurman R, Jussila K, Carter AS, Mattila M, Ebeling H, et al. Moilanen I, et al. Social anxiety in high-functioning children and adolescents with autism and Asperger syndrome. Journal of Autism and Developmental Disorders. 2008;38:1697–1709. doi: 10.1007/s10803-008-0555-9. [DOI] [PubMed] [Google Scholar]
- Lainhart JE, Bigler ED, Bocian M, Coon H, Dinh E, Dawson G, et al. Volkmar F. Head circumference and height in autism: a study by the Collaborative Program of Excellence in Autism. American Journal of Medical Genetics Part A. 2006;140:2257–2274. doi: 10.1002/ajmg.a.31465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: relative prevalence, effects of subject characteristics, and empirical classification. Journal of Autism and Developmental Disorders. 2006;36:1101–1114. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- Le Couteur A, Rutter M, Lord C, Rios P. Autism diagnostic interview: A standardized investigator-based instrument. Journal of Autism and Developmental Disorders. 1989;19:363–387. doi: 10.1007/BF02212936. [DOI] [PubMed] [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Lainhart JE. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. Journal of Autism and Developmental Disorders. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule (ADOS) Los Angeles: Western Psychological Services; 2000. [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: A revised version of the autism diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Matson JL, Nebel-Schwalm MS. Comorbid psychopathology with autism spectrum disorder in children: An overview. Research in Developmental Disabilities. 2006;28:341–352. doi: 10.1016/j.ridd.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Mattila M, Hurtig T, Haapsamo H, Jussila K, Kuusikko-Gauffin S, Kielinen M, et al. Moilanen I. Comorbid psychiatric disorders associated with Asperger syndrome/high-functioning autism: a community and clinic-based study. Journal of Autism and Developmental Disorders. 2010 doi: 10.1007/s10803-010-0958-2. [DOI] [PubMed] [Google Scholar]
- Mazurek MO, Kanne SM. Friendship and internalizing symptoms among children and adolescents with ASD. Journal of Autism and Developmental Disabilities. 2010 doi: 10.1007/s10803-010-1014-y. [DOI] [PubMed] [Google Scholar]
- Nicpon MF, Doobay AF, Assouline SG. Parent, teacher, and self perceptions of psychosocial functioning in intellectually gifted children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2010 doi: 10.1007/s10803-010-0952-8. [DOI] [PubMed] [Google Scholar]
- Perry DW, Marston GM, Hinder SA, Munden AC, Roy A. The phenomenology of depressive illness in people with a learning disability and autism. Autism. 2001;5:265–275. doi: 10.1177/1362361301005003004. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Gurley O, Brook J, Ma Y. The risk for early adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Sattler JM, Dumont R. Assessment of Children: WISC-IV and WPPSI-III Supplement. San Diego, CA: Jerome M. Sattler; 2004. [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davies M. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the epidemiology of child and adolescent mental disorders study. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(7):865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Siminoff EM, Pickles AP, Charman TP, Chandler SP, Loucas TOMP, Baird GF. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Sterling L, Dawson G, Estes A, Greenson J. Characteristics associated with presence of depressive symptoms in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2008;38:1011–1018. doi: 10.1007/s10803-007-0477-y. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Gadow KD, Arnold L, Aman MG, McDougle CJ, et al. Vitiello B. Parent-rated anxiety symptoms in children with pervasive developmental disorders: frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology. 2008;36:117–128. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- Vickerstaff S, Heriot S, Wong M, Lopes A, Dossetor D. Intellectual ability, self-perceived social competence and depressive symptomatology in children with high-functioning autistic spectrum disorders. Journal of Autism and Development Disorders. 2007;37:1647–1644. doi: 10.1007/s10803-006-0292-x. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children IV. San Antonio, TX: The Psychological Corporation; 2003. [Google Scholar]
- Weisbrot DM, Gadow KD, DeVincent CJ, Pomeroy J. The presentation of anxiety in children with pervasive developmental disorders. Journal of Child and Adolescent Psychopharmacology. 2005;15:477–496. doi: 10.1089/cap.2005.15.477. [DOI] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009;29:216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehouse AJO, Durkin K, Jaquet E, Ziatas K. Friendship, loneliness and depression in adolescents with Asperger's Syndrome. Journal of Adolescence. 2009;32:309–322. doi: 10.1016/j.adolescence.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Wing L. Manifestations of social problems in high-functioning autistic people. In: Schopler E, Mesibov G, editors. High-functioning individuals with autism. New York: Plenum; 1992. pp. 129–142. [Google Scholar]