Abstract
A case of invasive ductal carcinoma of an ectopic pancreas in the stomach in a 74-year-old woman is presented. A 4.0 cm gastric submucosal tumor (SMT) was resected surgically. Histologically, the tumor showed cystic tissue consisting of an ectopic pancreas with foci of a moderately differentiated tubular adenocarcinoma. In this tumor, small pancreatic tissues, acini, Langerhans islets, and ductular cells were detected in the gastric SMT. The patient has experienced long-term survival. The incidence of pancreatic cancer of an ectopic pancreas is rare, and the etiology of this disease is discussed in the literature.
Key words: Ectopic pancreas, Pancreas cancer, Gastric wall
Introduction
Ectopic pancreas, also called a heterotopic or aberrant pancreas, is defined as pancreatic tissue lying outside its normal location and lacking anatomic or vascular connections with the pancreas. This usually asymptomatic condition is found incidentally at laparotomy or autopsy in the stomach, duodenum, small intestine, Meckel's diverticulum, or biliary tract [1, 2]. It is found in approximately 1 to 2% of autopsy cases. It has also been reported that more than 85% of cases occurred in the gastrointestinal wall. Of them, 30% occurred in the duodenum, 25% in the stomach, 15% in the jejunum, 5% in the ileum, and 5% in Meckel's diverticulum [3].
Neoplasms arising from an ectopic pancreas are extremely rare. Adenocarcinoma originating from an ectopic pancreas has been reported in several cases in the literature [4, 5, 6, 7, 8]. In this report, we describe a case of invasive ductal carcinoma arising from an ectopic pancreas in the stomach.
Case Report
A 75-year-old woman came to our hospital presenting with epigastralgia in February 2000. Physical examination revealed no abnormal findings. Routine blood count and chemistry tests were within normal limits. Serum amylase concentration was also within normal limits. Carcinoembryonic antigen (CEA) was 8.7 ng/ml, and carbohydrate antigen 19–9 (CA19–9) was 287.4 U/ml. Gastrointestinal endoscopy was performed and revealed a gastric submucosal tumor (SMT) at the middle corpus, posterior wall and lesser curvature of her stomach. Biopsy showed only normal gastric mucosa. The SMT had obviously enlarged with a lobular surface from when examined 2 years previously (fig. 1). Computed tomography (CT) revealed an intramural cystic mass, 4.0 cm, located in the lesser curvature of the stomach (fig. 2). No other tumor was observed in the pancreas or liver. Probe laparotomy was conducted in May 2002. At laparotomy, we found a 2.0 · 2.0 · 2.0 cm elastic mass fused to the other tumor. There was no evidence of metastasis or invasion to the surrounding tissue. Since the tumor had no connection with the neighboring gastric wall, it was easily resected with the capsulized tumor. The pancreas was normally located and normal in size.
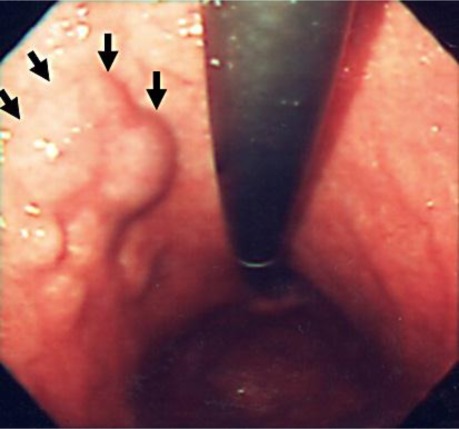
Fig. 1.
Gastrointestinal endoscopy shows multiple fusioned submucosal tumors at the middle corpus, posterior wall and lesser curvature of the stomach.
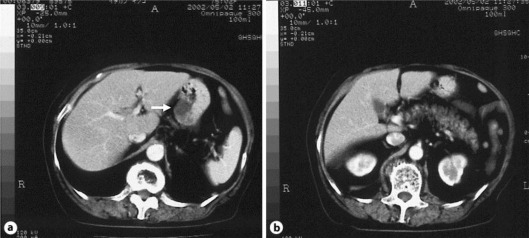
Fig. 2.
a Abdominal CT scan reveals a cystic lesion in the gastric wall. b Morphology of the pancreas is within normal limits.
Histological examination of the submitted material shows the resected part of the stomach with submucosal cystic tissue consisting of an ectopic pancreas with cystic or papillary hyperplasia of ducts, mature clusters of pancreatic acini, Langerhans islets and foci of moderately differentiated tubular adenocarcinoma in fibrous stroma, located in the submucosa and subserosa through the muscle layers of the stomach with no marked mucosa (fig. 3). Microscopically, invasive ductal carcinoma arising from the ectopic pancreas was observed in the stomach.
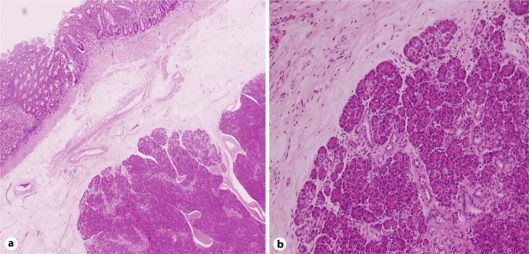
Fig. 3.
a, b Histological examination shows a resected part of the stomach with foci of moderately differentiated tubular adenocarcinoma in fibrous stroma, located in submucosa and subserosa through muscle layers of the stomach. a ·20. b ·100.
The postoperative course was uneventful, and the patient has been healthy without any evidence of disease recurrence for 11 years.
Discussion
Ectopic pancreas tissue in the stomach is most commonly found in the antrum and is also seen relatively frequently along the greater curvature and posterior and anterior walls, whereas it rarely occurs along the lesser curvature [9]. Von Heinrich [10] proposed three types of heterotopic pancreas in 1909; thereafter, his classification was modified by Gaspar Fuentes in 1973 [11], acquiring its final form.
Type I: heterotopia consists of typical pancreatic tissue with acini, ducts, and islet cells similar to those seen in a normal pancreas. Type II: heterotopia is composed of pancreatic ducts only, referred to as canalicular variety. Type III: heterotopia is characterized by acinar tissue only. Type IV: heterotopia is made up of islet cells only [10, 11]. Our case, a type of heterotopic pancreas, seemed to be categorized in type I, because typical pancreas tissue with acini, ducts, and islet cells was seen in the pathological examination. The origin of ectopic pancreas is unknown; it is possible that during rotation of the foregut and fusion of the ventral and dorsal parts of the pancreas in early fetal life, small pieces of tissue become detached from the forming organ, leading to entrapment in different locations [8].
Malignant transformation in an ectopic pancreas has been reported in less than 15 cases in the literature [4, 5, 6, 7, 8, 12, 13]. Criteria have been proposed for the diagnosis of carcinoma from an ectopic pancreas as follows: (1) the tumor must be located within or very close to the ectopic pancreas tissue, (2) transition between pancreas structures and carcinoma must be identified, and (3) the nonneoplastic pancreatic tissue must comprise fully developed acini and ducts [4]. The diagnosis in the present case would fulfill these three criteria.
Preoperative diagnosis of ectopic pancreas malignancy may be difficult with imaging studies such as CT and radiographic study. Endoscopic ultrasound (EUS) is typically used to evaluate submucosal lesions in the upper gastrointestinal tract [14]. EUS also allows the use of targeted fine needle aspiration biopsy (FNAB), particularly helpful for the final diagnosis; however, cytological examinations are inconclusive in about 50% of cases [8].
The prognosis of adenocarcinoma arising from ectopic pancreas is not known. One author reported that adenocarcinoma arising from an ectopic pancreas seemed to have a somewhat better prognosis than those arising from the pancreas itself, probably due to earlier presentation [12]. In the literature, only ten cases have been reported, with a survival time of between six months and ten years, and all with a life expectancy longer than in the case of orthotopic pancreas surgery [15]. In the present case, the patient has survived for more than 11 years.
In summary, we report a rare case of malignant transformation of an ectopic pancreas of the gastric wall in a patient who has survived during long-term follow-up after surgery.
References
- 1.Barbosa De Castro J, Dockerty MB, Waugh JM. Pancreatic heterotopia. Surg Gynecol Obstet. 1946;82:527–542. [PubMed] [Google Scholar]
- 2.Dolan RV, ReMine WH, Dockerty MB. The fate of heterotopic pancreatic tissue: a study of 212 cases. Arch Surg. 1974;109:762–765. doi: 10.1001/archsurg.1974.01360060032010. [DOI] [PubMed] [Google Scholar]
- 3.Seifer G. Congenital anomalies. In: Kloppel G, Heitz PU, editors. Pancreatic Pathology. Churchill-Livingstone: Edinburgh; 1984. pp. 22–26. [Google Scholar]
- 4.Emerson L, Layfield LJ, Rohr LR, Dayton MT. Adenocarcinoma arising in association with gastric heterotopic pancreas: a case report and review of the literature. J Surg Oncol. 2004;87:53–57. doi: 10.1002/jso.20087. [DOI] [PubMed] [Google Scholar]
- 5.Ishikawa O, Ishiguro S, Ohhigashi H, Sasaki Y, Yasuda T, Imaoka S, Iwanaga T, Nakaizumi A, Fujita M, Wada A. Solid and papillary neoplasm arising from an ectopic pancreas in the mesocolon. Am J Gastroenterol. 1990;85:597–601. [PubMed] [Google Scholar]
- 6.Tornóczky T, Kálmán E, Jáksó P, Méhes G, Pajor L, Kajtár GC, Battyány I, Davidovics S, Sohail M, Krausz T. Solid and papillary epithelial neoplasm arising in heterotopic pancreatic tissue of the mesocolon. J Clin Pathol. 2001;54:241–245. doi: 10.1136/jcp.54.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koh HC, Page B, Black C, Brown I, Ballantyne S, Galloway DJ. Ectopic pancreatic-type malignancy presenting in a Meckel's diverticulum: a case report and review of the literature. World J Surg Oncol. 2009;7:54. doi: 10.1186/1477-7819-7-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tolentino LF, Lee H, Maung T, Stabile BE, Li K, French SW. Islet cell tumor arising from a heterotopic pancreas in the duodenal wall with ulceration. Exp Mol Pathol. 2004;76:51–56. doi: 10.1016/j.yexmp.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Yamagiwa H, Ishihara A, Sekoguchi T, Matsuzaki O. Heterotopic pancreas in surgically resected stomach. Gastroenterol Jpn. 1977;12:380–386. doi: 10.1007/BF02774535. [DOI] [PubMed] [Google Scholar]
- 10.Von Heinrich H. Ein Beitrag zur Histologie des sogen. akzessorischen Pankreas. Virchows Arch A Pathol Anat Histopathol. 1909;198:392–401. [Google Scholar]
- 11.Gaspar Fuentes A, Campos Tarrech JM, Fernandez Burgui JL, Castells Tejon E, Ruiz Rossello J, Gomez Perez J, Armengol Miro J. Pancreas ectopias. Rev Esp Enferm Apar Dig. 1973;39:255–268. [PubMed] [Google Scholar]
- 12.Eisenberger CF, Gocht A, Knoefel WT, Busch CB, Peiper M, Kutup A, Yekebas EF, Hosch SB, Lambrecht W, Izbicki JR. Heterotopic pancreas – clinical presentation and pathology with review of the literature. Hepatogastroenterology. 2004;51:854–858. [PubMed] [Google Scholar]
- 13.Mizuno Y, Sumi Y, Nachi S, Ito Y, Marui T, Saji S, Matsumoto H. Acinar cell carcinoma arising from an ectopic pancreas. Surg Today. 2007;37:704–707. doi: 10.1007/s00595-006-3384-5. [DOI] [PubMed] [Google Scholar]
- 14.Yasuda K, Cho E, Nakamura M, Kawai K. Diagnosis of submucosal lesions of the upper gastrointestinal tract by endoscopic ultrasonography. Gastrointest Endosc. 1990;36:S17–S20. doi: 10.1016/s0016-5107(90)71010-3. [DOI] [PubMed] [Google Scholar]
- 15.Jiang LX, Xu J, Wang XW, Zhou FR, Gao W, Yu GH, Lv ZC, Zheng HT. Gastric outlet obstruction caused by heterotopic pancreas: a case report and quick review. World J Gastroenterol. 2008;14:6757–6759. doi: 10.3748/wjg.14.6757. [DOI] [PMC free article] [PubMed] [Google Scholar]