Abstract
Purpose:
The aim of the study was to evaluate the minimal invasive approach and endourological techniques in managing the iatrogenic ureterovaginal fistula. The etiology and the diagnostic tools were also looked at.
Patients and Methods:
A retrospective study was conducted on 20 patients with ureterovaginal fistulas. The main causes for these were gynecological and obstetrical procedures. In all cases, the diagnosis was based on clinical presentation, intravenous pyelography, and cystoscopy. Various therapeutic methods were used. Eleven patients were treated by the endoscopic placement of a ureteral stent and 13 patients (including four with failed initial ureteral stent insertion) received ureteral reimplantation. Of these, two patients were treated by the Boari flap method, six by Psoas hitch, four by simple ureteric reimplant, and one by transureteroureterostomy.
Results:
Of the 11 patients treated by the endoscopic placement of a ureteral stent, 7 (64%) were successfully managed with this treatment alone. The remaining 4 (36%) also had open surgery. A total of 13 patients (including the 4 initially treated with endoscopic placement) underwent successful ureteric reimplantation. Routine cystoscopy revealed that 2 of the 20 patients (10%) had a concurrent vesicovaginal fistula.
Conclusion:
A ureterovaginal fistula is a rare but a relatively frequent complication of pelvic surgery. We recommend a minimal invasive approach including ureteric stent insertion as primary management and routine cystoscopy to rule out an association of a vesicovaginal fistula.
Keywords: Percutaneous ureteral stenting, vesicovaginal fistula, endoscopic ureteral stenting, ureterovaginal fistula
INTRODUCTION
The ureter is especially susceptible to injury during vascular, gynecologic, urologic and colonic operations. Gynecological surgery remains the most common cause of ureterovaginal fistulas; total abdominal hysterectomy is the operation most responsible for a ureteral injury.[1]
Loss of continuity of the ureter may result fromdivision or laceration, or from ischemic necrosis related to clamping, ligation, or damage to the blood supply of the ureter.[2] Traditionally, most ureterovaginal fistulas have been repaired by ureteroneocystostomy.[3] Endourological techniques are highly successful in treating ureterovaginal fistulas and ureteral stricture does not appear to be a common complication.[4]
PATIENTS AND METHODS
A retrospective analysis was done of 20 patients with a ureterovaginal fistula the majority of the cases were secondary to gynecological surgery. The mean age was 48 years (26–70 years old). The procedures performed were total abdominal hysterectomy for benign lesions in 12 patients, radical abdominal hysterectomy for malignancy in 7 patients, and repair of the ruptured uterus in 1 patient.
All 20 patients presented with vaginal drainage within 3–4 weeks of the original operation. Seventy percent presented with flank pain and CVA tenderness and 40% with fever and chills.
The medical and surgical history of all the patients was determined, and physical examination, urine analysis and culture, IVP and/or a CT urogram/cystogram, and cystoscopy were performed on all.
RESULTS
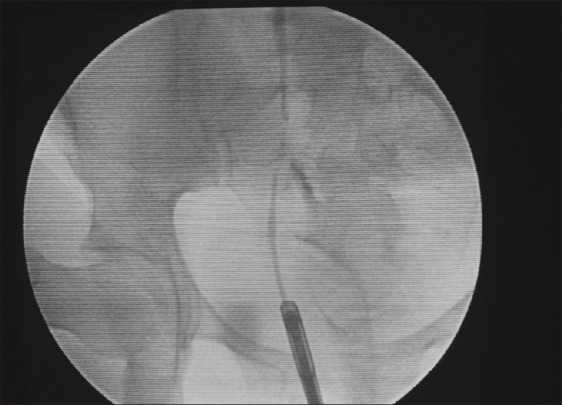
The excretory urogram (IVP) and a CT urogram were abnormal in all 20 patients, with obstruction, extravasation, or both as the findings [Figures 1–4]. Routine cystoscopy revealed a concurrent vesicovaginal fistula in 2 of the 20 patients. Ureteral stent insertion for 6–8 weeks [Figure 5] was the initial treatment in 11 patients (3 of whom had failed initial management with the placement of a percutaneous nephrostomy tube alone). Thirteen patients were treated with ureteric reimplant (including four who had failed initial ureteral stent insertion). Methods for the reimplant were as follows: Boari flap in two patients, Psoas hitch in six, simple ureteric reimplant in four, and transureteroureterostomy in one patient. An additional procedure, the excision of the vesicovaginal fistula and repair with an omintal flap was performed in two of the patients with a concurrent vesicovaginal fistula.
Figure 1.

CT urogram shows the obstructed ureter
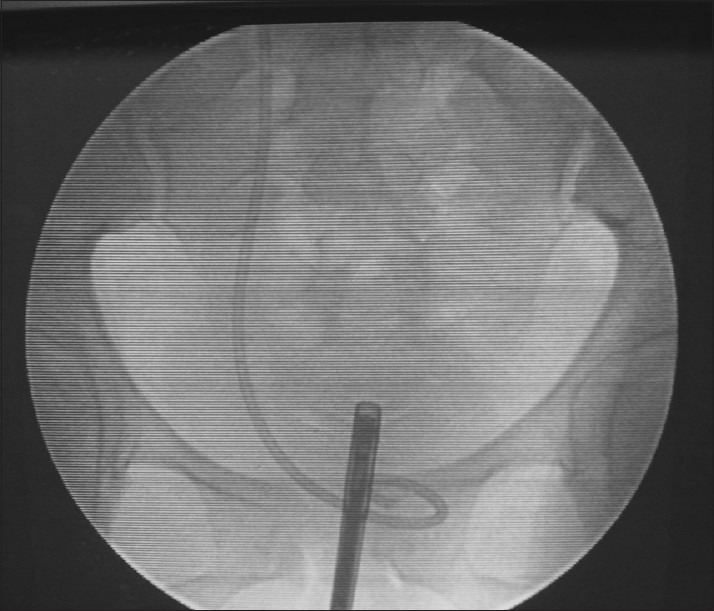
Figure 4.

Retrograde ureterogram reveals complete ureteral obstruction with ureterovaginal fistula
Figure 5.
Insertion of the double J stent
Figure 2.

CT urogram shows the ureterovaginal fistula
Figure 3.

IVP shows the obstructed ureter and the ureterovaginal fistula
None of the patients managed solely with percutaneous nephrostomy tube drainage had a good outcome. There was a 63% success rate with ureteral stent insertion only. All patients treated with ureteral reimplant were dry immediately after the operation. One patient underwent transureteroureterostomy after failed ureteral stent twice (the patient had pelvic radiation for ranulomatous vasculitis).
DISCUSSION
The most common presenting symptom of an iatrogenic genitourinary fistula is continuous urinary drainage from the vagina after gynecologic or other pelvic surgical intervention. A fistula may become apparent either immediately or, much more commonly, in a delayed fashion several days to weeks after surgery. In developed countries, 75% of genitourinary fistulas are subsequent to routine abdominal or vaginal hysterectomy.[5] However, in developing countries, birth trauma still accounts for a majority of fistulas.[6]
The ureterovaginal fistula is a complication of iatrogenic ureteral injuries. Gynecological surgery is considered to be the major cause for the ureterovaginal fistula. Although most women with urinary vaginal fistulas have vesicovaginal fistulas, it is fairly common to have both vesicovaginal and ureterovaginal fistulas. The incidence has been reported to be in 12–25% of all patients.[7,8]
The ureterovaginal fistula is the most serious of the urovaginal fistulas because of its potential to cause incontinence, sepsis, and renal loss.[9]
An excretory urogram or a CT urogram should be performed if the ureterovaginal fistula is suspected. The presence of normal upper tracts essentially rules out a ureteral injury; however, the finding of partial ureteral obstruction associated with urinary drainage from the vagina strongly suggests the presence of an ureterovaginal fistula.[10]
A retrograde pyelogram is helpful to diagnose ureteral injury and the placement of ureteral stent could be attempted at the same time [Figure 4].[11]
Ureteroneocystostomy has been the traditional treatment for the ureterovaginal fistula. Recently, conservative noninvasive treatment has been followed. Primary treatment with percutaneous nephrostomy has been reported to be less effective in the treatment of a ureterovaginal fistula. Schmeller et al. reported on 11 patients with ureterovaginal fistulas treated only by percutaneous nephrostomy, with 6 (55%) having persistent fistulas, while 2 (18%) having strictures.[12]
In our series, of the three patients treated initially by percutaneous nephrostomy alone, all had persistent fistulas.
Conservative management with a percutaneous nephrostomy tube and/or ureteral stent could be successful in allowing the fistula to heal (48% of patients with a ureteral injury discovered postoperatively were successfully managed by these measures alone). Immediate ureteral stent and or nephrostomy tube placement should be attempted when the diagnosis of the ureterovaginal fistula is established. Even if a surgical repair is eventually needed, prompt urinary drainage is essential to preserve the renal function.[13,14]
The diversion of the urine with an internal ureteral stent has been reported to allow spontaneous healing with varying success, in 5–15% of ureterovaginal fistulas.[15]
Selzman reported that ureterovaginal fistulas resolved in all seven patients treated with an internal ureteral stent.[16] In our series, we had a 64% success rate with the internal ureteral stent which was left in situ for 6–8 weeks (in 7 of 11 patients) and 4 patients had a persistent ureterovaginal fistula (including 2 patients who had the stent for 6 months; Figure 6).
Figure 6.
Retrograde pyelogram shows the persistence of the ureterovaginal fistul
Lingeman has reported that endoureterotomy was performed in nine patients for total ureteral occlusion. Simultaneous antegrade and retrograde ureteroscopy was also performed in all nine patients. The “cut-to-the-light” technique was utilized in six patients and a new technique employing a fascial incising needle was used in five patients. With a mean follow-up of 22 months, all nine patients had a successful outcome.[17]
A combined ureteroscopic and fluoroscopic technique to reestablish ureteral integrity has been reported to be a successful treatment.[18] Early intervention is recommended in the treatment of the iatrogenic ureterovaginal fistula, causing minimal morbidity and discomfort, and being less expensive.[19]
In cases of persistent urinary leakage from the vagina postsurgical repair of the vesicovaginal fistula, a ureterovaginal fistula should be suspected. We found that 2 out of the 20 patients (10%) had concurrent vesicovaginal fistulas. UVF was associated with a vesicovaginal fistula in 11 of 45 patients.[20]
CONCLUSION
Our current approach to the patients with symptoms of ureteral obstruction, or fistula, includes an IVP and/or a CT urogram to establish a diagnosis. Cystoscopy and retrograde pyelograms are essential to rule out the associated vesicovaginal fistula and to confirm the diagnosis. The minimal invasive approach is our first choice. Ureteric stent insertion is a primary management for the ureterovaginal fistula. When the retrograde approach is impossible, percutaneous nephrostomy and antegrade stent insertion are the second step. At least 6 weeks of stenting is allowed for healing. In the case of failure, an open surgical repair is necessarily.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.McVary KT, Marshall FF. Urinary fistulae. In: Gillenwater JY, editor. Adult and pediatric urology. 4th ed. Philadelphia: Lippincott, Williams and Wilkins; 2002. pp. 1271–95. [Google Scholar]
- 2.Ross G., Jr . Ureterovaginal fistula. In: Seidman EJ, Hannon PM, editors. Current Urologic Therapy. 3rd ed. Philadelphia: W.B. Saunders; 1994. pp. 242–5. [Google Scholar]
- 3.Mandal AK, Sharma SK, Vaidyanathan S, Goswami AK. Ureterovaginal fistula: Summary of 18 years’ experience. Br J Urol. 1990;65:453–6. doi: 10.1111/j.1464-410x.1990.tb14785.x. [DOI] [PubMed] [Google Scholar]
- 4.Selzman AA, Spirnak JP, Kursh ED. The changing management of ureterovaginal fistulas. J Urol. 1995;153:626–8. doi: 10.1097/00005392-199503000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Tancer ML. Observations on prevention and management of vesicovaginal fistula after total hysterectomy. Surg Gynecol Obstet. 1992;175:501–6. [PubMed] [Google Scholar]
- 6.Arrowsmith S, Hamlin EC, Wall LL. Obstructed labor injury complex: Obstetric fistula formation and the multifaceted morbidity of maternal birth trauma in the developing world. Obstet Gynecol Surv. 1996;51:568–74. doi: 10.1097/00006254-199609000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Fichtner J, Voges G, Steinbach F, Hohenfellner R. Ureterovesicovaginal Fistulas. Surg Gynecol Obstet. 1993;176:571–4. [PubMed] [Google Scholar]
- 8.Goodwin WE, Scardino PT. Vesicovaginal and ureterovaginal fistulas: A summary of 25 years of experience. J Urol. 1980;123:370–4. doi: 10.1016/s0022-5347(17)55941-8. [DOI] [PubMed] [Google Scholar]
- 9.Labasky RF, Leach GE. Prevention and management of urovaginal fistulas. Clin Obstet Gynecol. 1990;33:382–91. doi: 10.1097/00003081-199006000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Gerber GS, Schoenberg HW. Female urinary tract fistulas. J Urol. 1993;149:229–36. doi: 10.1016/s0022-5347(17)36045-7. [DOI] [PubMed] [Google Scholar]
- 11.Flynn JT, Tiptaft RC, Woodhouse CR, Paris AM, Blandy JP. The early and aggressive repair of iatrogenic ureteric injuries. Br J Urol. 1979;51:454–7. doi: 10.1111/j.1464-410x.1979.tb03577.x. [DOI] [PubMed] [Google Scholar]
- 12.Schmeller NT, Gottinger H, Schuller J, Marx FJ. Percutaneous nephrostomy as primary therapy of ureterovaginal fistula. Urologe A. 1983;22:108–12. [PubMed] [Google Scholar]
- 13.Dowling RA, Corriere JN, Jr, Sandler CM. Iatrogenic ureteral injury. J Urol. 1986;135:912–5. doi: 10.1016/s0022-5347(17)45921-0. [DOI] [PubMed] [Google Scholar]
- 14.Gerber GS, Schoenberg HW. Female urinary tract fistulas. J Urol. 1993;149:229–36. doi: 10.1016/s0022-5347(17)36045-7. [DOI] [PubMed] [Google Scholar]
- 15.Labasky RF, Leach GE. Prevention and management of urovaginal fistulas. Clin Obstet Gynecol. 1990;33:382–91. doi: 10.1097/00003081-199006000-00023. [DOI] [PubMed] [Google Scholar]
- 16.Selzman AA, Spirnak JP, Kursh ED. The changing management of ureterovaginal fistulas. J Urol. 1995;153:626–8. doi: 10.1097/00005392-199503000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Lingeman JE, Wong MY, Newmark JR. Endoscopic management of total ureteral occlusion and ureterovaginal fistula. J Endourol. 1995;9:391–6. doi: 10.1089/end.1995.9.391. [DOI] [PubMed] [Google Scholar]
- 18.Beaghler MA, Taylor FC, McLaughlin KP. A combined antegrade and retrograde technique for reestablishing ureteral continuity. Tech Urol. 1997;3:44–8. [PubMed] [Google Scholar]
- 19.Elabd S, Ghoniem G, Elsharaby M, Emran M, Elgamasy A, Felfela T, et al. Use of endoscopy in the management of postoperative ureterovaginal fistula. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:185–90. doi: 10.1007/BF02765810. [DOI] [PubMed] [Google Scholar]
- 20.Tazi K, Moudouni S, Koutani A, Ibn Attya A, Hachimi M, Lakrissa A. Uretero-vaginal fistula.Therapeutic alternatives concerning 10 cases. Prog Urol. 2000;10:83–8. [PubMed] [Google Scholar]


