A 60-year-old diabetic woman with stage IV chronic kidney disease and a history of lichen planus presented with chronic intermittent solid food dysphagia for seven years that had worsened over the past year. She had associated dyspeptic symptoms with no other gastrointestinal symptoms. She had been treated with lansoprazole and famotidine, with some improvement in her symptoms. She reported no history of allergic rhinitis or asthma.
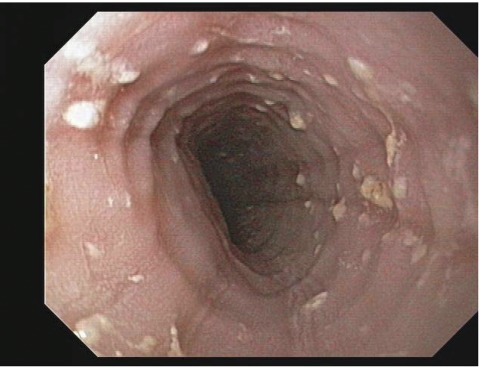
Physical examination was unremarkable. Significant laboratory findings included blood urea nitrogen 58 mg/dL, serum creatinine 5.7 mg/dL (baseline), total calcium 8.9 mg/dL, phosphate 4.9 mg/dL, estimated glomerular filtration rate 8.2 mL/min, thyroid stimulating hormone 2.56 μIU/mL, and hemoglobin 11.1 g/dL. Chest radiograph was normal. Barium swallow showed non-specific rings with normal swallowing, and esophagogastroduodenoscopy (EGD) revealed diffuse full-length esophageal rings and furrows (figure 1). Multiple biopsies were obtained from the proximal and distal esophagus, stomach, and duodenum, and a lower esophageal sphincter dilatation was performed.
Figure 1.
Esophagogastroduodenoscopy showing rings and furrows throughout the length of the esophagus; these are common in lymphocytic esophagitis.
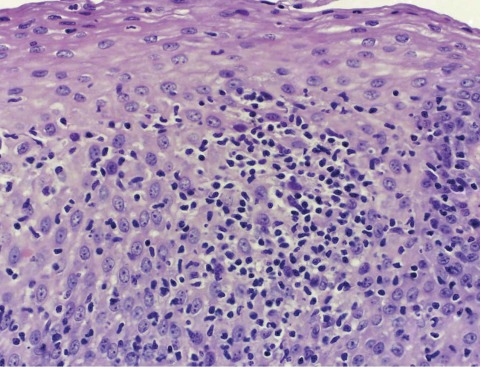
A proximal esophageal biopsy revealed squamous mucosal injury with an intraepithelial lymphocytosis in a peripapillary distribution, characteristic of the entity lymphocytic esophagitis (LE) (figure 2). There was no neutrophilic or eosinophilic component to the inflammatory infiltrate, supporting the latter diagnosis.
Figure 2.
Esophageal mucosa showing peripapillary intraepithelial lymphocytosis with basal zone hyperplasia and intercellular edema. No significant population of eosinophils or neutrophils is identified (hematoxylin and eosin stain).
A therapeutic trial of swallowed fluticasone (two puffs [220 μg/actuation aerosol] t.i.d.) was initiated, to be followed by EGD and biopsy. Follow-up at six months revealed resolution of the solid food dysphagia, but the patient declined the repeat EGD.
A small subset of patients with upper gastrointestinal tract symptoms, in the absence of gastritis, duodenitis, or recognizable cause of esophagitis (eg, gastroesophageal reflux disease [GERD]), have manifested a characteristic esophageal biopsy appearance featuring a prominent intraepithelial infiltrate of T lymphocytes. This recently recognized histological pattern of esophageal mucosal injury, termed “lymphocytic esophagitis,” is poorly understood.1 There is scant demographic data, but 43% of LE patients present with dysphagia.2 While some cases have occurred with another concomitant inflammatory gastrointestinal disease (GERD, gastritis, lichen planus, celiac disease, Crohn’s disease), others have remained of undetermined pathogenesis. Possible causes of LE include a hypersensitivity reaction to an ingestant and an autoimmune phenomenon.1, 2 The relationship of our patient’s previously diagnosed lichen planus to LE remains unclear.
There is no defined strategy for diagnosis or treatment of LE. However, in order to exclude the possibility of an underlying treatable gastrointestinal disorder, esophageal, gastric, and duodenal biopsy, as well as scrutiny of the past medical history are recommended. With an undetermined etiology and ineffective acid suppression therapy, a course of a topical corticosteroid agent (eg, fluticasone) would be appropriate. Corticosteroids have been noted to be beneficial in other gastrointestinal lymphocytic or autoimmune phenomenon.3–5 Swallowed fluticasone in particular has been found to induce histological remission in closely related esophageal autoimmune conditions like eosinophilic esophagitis.5
This case illustrates that the recently recognized, enigmatic entity LE should be considered in the evaluation of chronic dysphagia, even though it remains a diagnosis of exclusion.
References
- 1.Rubio CA, Sjödahl K, Lagergren J. Lymphocytic esophagitis: a histological subset of chronic esophagitis. Am J Clin Pathol 2006;125:432–437 [PubMed] [Google Scholar]
- 2.Purdy JK, Appelman HD, Golembeski CP, McKenna BJ. Lymphocytic esophagitis: a chronic or recurring pattern of esophagitis resembling allergic contact dermatitis. Am J Clin Pathol 2008; 130:508–513 [DOI] [PubMed] [Google Scholar]
- 3.Miehlke S, Madisch A, Karimi D, Wonschik S, Kuhlisch E, Beckmann R, Morgner A, Mueller R, Greinwald R, Seitz G, Baretton G, Stolte M. Budesonide is effective in treating lymphocytic colitis: a randomized double-blind placebo-controlled study. Gastroenterology 2009;136:2092–2100 [DOI] [PubMed] [Google Scholar]
- 4.Chande N, McDonald JW, Macdonald JK. Interventions for treating lymphocytic colitis. Cochrane Database Syst Rev 2008;(2):CD006096. [DOI] [PubMed] [Google Scholar]
- 5.Konikoff MR, Noel RJ, Blanchard C, Kirby C, Jameson SC, Buckmeier BK, Akers R, Cohen MB, Collins MH, Assa’ad AH, Aceves SS, Putnam PE, Rothenberg ME. A randomized, double-blind, placebo-controlled trial of fluticasone propionate for pediatric eosinophilic esophagitis. Gastroenterology 2006;131:1381–191 [DOI] [PubMed] [Google Scholar]