Abstract
Background
Smokers' knowledge of the risks of second-hand smoke (SHS) and the role this plays in implementing behaviours to reduce the SHS exposure of others have not been thoroughly explored. Mass media health promotion is used to promote behaviour change partly by providing information on the consequences of behaviour. In England, between 2003 and 2006, frequent mass media campaigns highlighted the toxicity of SHS.
Objectives
To examine peoples' knowledge of SHS-related illnesses in England over time, identify the determinants of good knowledge and to assess its importance in predicting SHS-protective behaviours.
Methods
Statistical analysis of repeat cross-sectional data (1996–2008) from the Omnibus Survey to explore the trends and determinants of knowledge of SHS-related illnesses and the determinants of SHS-protective behaviours.
Results
Only 40% of smokers had ‘good’ knowledge of SHS-related illnesses compared with 65% of never smokers. Knowledge increased markedly when frequent SHS-related mass media campaigns (2003–06) ran, compared with earlier years (1996–2002). Smokers with better knowledge were more likely to have smoke-free homes [odds ratio (OR): 1.10, 1.04–1.16] and abstain from smoking in a room with children (OR: 1.11, 1.09–1.14).
Conclusions
The low levels of knowledge of some SHS-related conditions, especially among smokers, and the relationship between knowledge and SHS-protective behaviours, suggest that greater efforts to educate smokers about the risks associated with SHS are worthwhile.
Keywords: smoking, home
Introduction
Knowledge acquisition is an important step in the process of health behaviour change.1–7 Nevertheless, the relationship between knowledge and behaviour change is complex. There is often a discrepancy between one's beliefs and behaviours known as cognitive dissonance. Dissonance theory proposes that in order to achieve consonance, either the belief or the behaviour must be changed.8,9 Although some smokers change their smoking behaviour by quitting or reducing their smoking,10 other evidence suggests that many smokers choose to understate the scientific evidence or adduce anecdotal evidence to counter risks publicized in the media instead.11,12
There is no safe level of exposure to SHS.13,14 People's knowledge of the impacts of SHS and the role this might play in smoking practices have not been thoroughly explored. It may be the case that smokers' concerns about harming others is a motivating factor in quit attempts.15 Furthermore, for those smokers who are unable or unwilling to quit, concerns about the dangers and decreased social acceptability of smoking may influence smokers to take measures to protect others from their smoke.16 In Queensland, Australia, researchers found that smokers immediately indicated that they would avoid exposing both adults and children to their SHS after they were informed of the risks of SHS to non-smokers.17 Qualitative work in Scotland indicated that concerns about the possible health risks were cited as the main reason for both total and partial smoking restrictions at home.18 Similarly, in the USA, strong belief in the danger that SHS posed to children's health was associated with home smoking bans amongst smokers.19 It may be the case that smokers' unrealistic optimism about their own risk of illness is juxtaposed by their concern about the impact of their smoking on others.20 Indeed, a phenomenon known as the ‘third person effect’ suggests that people often discount the personal effects of harmful environments and at the same time recognize the risks to others.21 However, results from a small-scale US study on children with asthma showed that although many parents were aware that their smoking exacerbated the symptoms of their children's asthma, only 33% of these smokers reported having a smoke-free home.22 Similarly, a UK study found that 85% of parents from smoking households believed that smoking affects children's health, yet only 30% prohibited smoking in the house. However, 65% of these parents did report other measures that they believed protected against SHS exposure, e.g. opening a window or not smoking in the same room with a child.23 Recent qualitative UK research has suggested that smokers are confused about the specific impacts of SHS and are displaying classic cognitive dissonance behaviours, as well as employing the aforementioned protective smoking practices. The authors conclude that mass media campaigns could be used to give information on the ineffectuality of these behaviours in order to reduce ‘half-way’ measures.24
The Health Bill enacting smoke-free legislation (SFL) in England was passed in February 2006 and SFL was implemented on 1 July 2007. Awareness of the dangers and concerns about the impact of SHS might have been expected to be particularly salient during the build-up to SFL. In 2003, debate surrounding the issue of smoke free started in earnest and was highly publicized in the media as a result. In the same year, a government-funded TV, press and billboard campaign on the effect of SHS on children, titled ‘If you smoke, I smoke’ was launched. Anti-SHS mass media campaigns frequently ran between December 2003 and April 2007.25 Thereafter, government-funded campaigns focused on compliance with SFL. Action for Smoking and Health (ASH) monitored their personal media coverage and noted it was at its highest between March 2004 and February 2006, with stories mentioning ASH England reaching an average audience of 4.5 million people a week.25
Evidence suggests that media coverage of debates over smoke-free policies and SHS mass media health promotion campaigns help disseminate the implicit message that SHS exposure is unacceptable.26 Furthermore, increased awareness of the issue, including knowledge of the dangers of SHS, may influence subsequent knowledge and smoking behaviours.
In England, recent evidence shows that 79% of children whose parents smoke are still exposed to SHS at home.27 In the absence of definitive evidence of what works in terms of increasing the prevalence of smoke-free homes,28 it is worth exploring the factors that may be influential in achieving reduced SHS exposure in children. This paper aims to quantitatively explore levels of and trends in knowledge of the health impacts of SHS exposure in England, the predictors of knowledge and, in turn, to assess whether knowledge is associated with SHS-protective behaviours.
Methods
Data
The Omnibus Survey (OS) is a monthly survey conducted using a multistage design by the Office of National Statistics to produce a nationally representative sample of adults living in private households in Great Britain, with one interviewee per household.29 A smoking module was conducted in October and November every year, apart from 1998. Data from 2007 onwards were therefore collected post-SFL. A sampling error compromised the 2008 survey results, and therefore the 2008 survey was repeated in February and March 2009. For simplicity, we refer to these data as the 2008 data. The smoking module was discontinued in 2009. Between 1996 and 2004, ∼1800 adults were interviewed each month; ∼1200 were interviewed since 2005. Response rates from 1996 to 2008 ranged from 61 to 70% of the eligible sample.
Outcome measures
Knowledge
Respondents were asked 10 questions about their knowledge of SHS-related illnesses, 5 about illnesses in children and 5 in adults. ‘Do you think that living with someone who smokes does, or does not, increase a child's risk of: asthma/ear infection/cot death/chest infections/other infections?’ and ‘Do you think that breathing in someone else's smoke increases the risk of a non-smoker getting: asthma/lung cancer/heart disease/bronchitis/coughs & colds?’ Response options are ‘increases risk’ or ‘does not increase risk’ of each illness.
SHS-protective behaviour
Since 2006, the OS asked ‘all’ respondents to describe their home smoking policy: smoking is not allowed at all, smoking is allowed in some rooms or at some times, smoking is allowed everywhere or don't know. In our analyses, a smoke-free home describes a household where smoking is not allowed at all.
Since 1997, ‘smokers only’ have been asked about their smoking behaviour when in a room with a non-smoking adult and a child; whether they smoke the same number of cigarettes as usual, smoke fewer, do not smoke at all or other. Smokers are asked regardless of whether they report a smoke-free home as it does not only refer to smoking within their own home.
Analyses
We examined the levels of and trends (1996–2008) in knowledge of SHS-related illnesses before creating a composite knowledge score by giving one point for every correctly identified illness. As knowledge of respiratory illnesses is relatively common1 and many of the questions asked were about respiratory illnesses, a total score of 8–10 was taken to indicate good knowledge.
To determine the predictors of good knowledge and SHS-protective behaviours, the data were analysed using univariate and multivariate logistic regression, with adjustments made for the OS complex sampling design. A weighting factor was applied to correct for unequal probability of selection.
The predictor variables included were age group, gender, smoking status, social class, number of cars owned, number of adults in the household and age of youngest child. To evaluate changes over time and to crudely assess whether mass media campaigns have impacted on knowledge or SHS-protective behaviour, three time periods were created, 1996–2002 (pre-SHS-media campaigns), 2003–06 (during SHS-media campaigns) and 2007–08 (post-SFL). Although one campaign on the impacts of SHS ran between March and April 2007, from then until July 2007 the campaigns focused on explaining compliance with legislation. No SHS-mass media campaigns were run in 2008.
The predictive ability of each model was assessed using predicted probabilities to compute the receiver operating characteristic. A value of 1 represents perfect predictive fit, whereas 0.5 means the model is synonymous with a random guess.30 An area under the curve (AUC) value of 0.7 is representative of a good fit.31
The SHS-protective behaviour analyses included knowledge of SHS-related illnesses and attitudes towards restrictions in three public places. A composite score of 0–3 was created for agreement with smoking restrictions in pubs, restaurants and workplaces.
Results
The sample distribution for gender and age for each annual sample are consistent with national population estimates.32 A total sample of 32 630 respondents was obtained across the 12-year period (Table 1). Approximately 50% of respondents had never smoked, 27% were ex-smokers and 24% were current smokers (17% light and 7% heavy smokers). Examining annual smoking prevalence rates showed that, in line with other national surveys,33 smoking prevalence decreased from 28% in 1996 to 21% in 2007.
Table 1.
Characteristics of the OS England sample by year (1996–2008); proportion of respondents in each socio-demographic subgroup (%)
| Socio-demographics | 1996 | 1997 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008a | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | |||||||||||||
| Male | 49 | 46 | 46 | 49 | 43 | 46 | 46 | 46 | 45 | 46 | 47 | 45 | 15 101 (46) |
| Female | 51 | 54 | 54 | 51 | 57 | 54 | 54 | 54 | 55 | 54 | 53 | 55 | 17 529 (54) |
| Age group (years) | |||||||||||||
| 16–24 | 12 | 13 | 13 | 12 | 13 | 12 | 14 | 12 | 11 | 12 | 11 | 9 | 4008 (12) |
| 25–44 | 38 | 36 | 37 | 35 | 35 | 34 | 34 | 35 | 36 | 34 | 33 | 31 | 11 450 (35) |
| 45–64 | 32 | 33 | 31 | 32 | 31 | 33 | 32 | 33 | 32 | 34 | 35 | 36 | 10 585 (32) |
| 65+ | 18 | 18 | 19 | 22 | 21 | 20 | 20 | 20 | 21 | 20 | 20 | 24 | 6587 (20) |
| Smoking status | |||||||||||||
| All smokers | 28 | 25 | 26 | 25 | 23 | 25 | 23 | 22 | 22 | 24 | 21 | 19 | 7924 (24) |
| Light (0–20/day) | 19 | 17 | 18 | 17 | 16 | 17 | 16 | 16 | 16 | 18 | 15 | 5 | 2244 (7) |
| Heavy (20+/day) | 9 | 8 | 8 | 8 | 7 | 8 | 7 | 6 | 6 | 6 | 6 | 14 | 5680 (17) |
| Ex | 26 | 28 | 28 | 28 | 26 | 26 | 26 | 28 | 26 | 27 | 27 | 36 | 8917 (27) |
| Never | 46 | 47 | 46 | 47 | 51 | 49 | 51 | 50 | 51 | 49 | 52 | 55 | 15 721 (48) |
| Social class | |||||||||||||
| Professional and managerial | 32 | 30 | 34 | 34 | 33 | 32 | 34 | 33 | 32 | 31 | 34 | 36 | 10 547 (32) |
| Skilled non-manual and manual | 41 | 42 | 39 | 38 | 42 | 42 | 39 | 41 | 42 | 41 | 39 | 40 | 13 260 (41) |
| Part skilled and unskilled | 23 | 23 | 23 | 21 | 20 | 19 | 19 | 19 | 19 | 19 | 19 | 16 | 6357 (20) |
| Never worked/unclassifiedb | 4 | 5 | 4 | 6 | 5 | 7 | 8 | 7 | 7 | 8 | 8 | 8 | 2465 (8) |
| Total sample | 3202 | 3174 | 3003 | 2881 | 3032 | 3316 | 3050 | 3095 | 2097 | 2013 | 1956 | 1812 | 32 630 |
Not all variable classifications will add up to the sample totals due to the missing data for those variables.
aThe 2008 data were collected in February and March 2009 due to a sampling error in October and November 2008.
bNot included in the final sample.
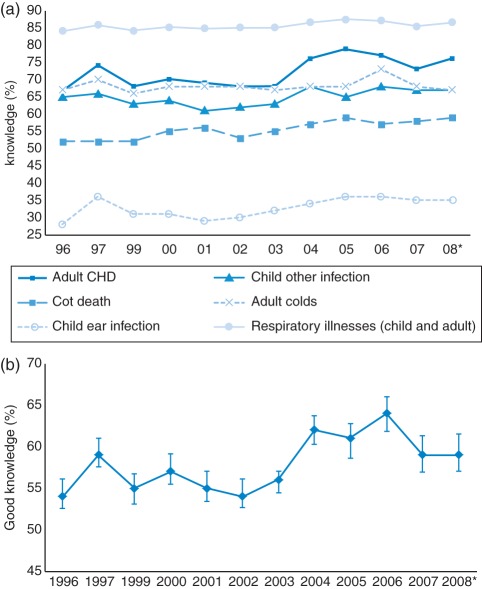
Levels of and trends in knowledge of SHS-related illnesses
Overall, more than 80% of respondents knew that SHS causes respiratory illnesses (Fig. 1a) but fewer were aware of the role of SHS in cot death (55%) and other infections (64%) in children and the links to coronary heart disease (71%) and coughs and colds in adults (68%). Knowledge of childhood ear infections was particularly poor (33%). There was a small increase in this knowledge between 1996 and 2008 for cot death (6%), ear infection (7%) and coronary heart disease (6%). Using the composite score, it was clear that knowledge increased from 1996 (Fig. 1b). The most marked increase was between 2003 and 2004 from 56% (54.4–57.0%) to 62% (60.3–63.7%). The highest level of knowledge was reached in 2006 (64%) but this fell significantly to 59% in 2007, and remained constant in 2008.
Fig. 1.
(a) Trends in respondents' knowledge of illnesses linked to SHS (1996–2008). *The 2008 data were collected in February and March 2009 due to a sampling error in October and November 2008. (b) Trends in the percentage of respondents with good knowledge of the illnesses caused by SHS.
A higher proportion of never smokers had good knowledge (65%, 64.0–65.5%) compared with ex- (59%, 58.1–60.1%), light (46%, 44.6–47.2%) and heavy (34%, 31.9–35.8%) smokers (Table 2). Unfortunately, the trend data for each subgroup are not reliable due to sample size limitations.
Table 2.
Logistic regression predicting ‘good’ knowledge (1996–2008)
| Predictor variables | n | Good knowledge (%) |
Univariate |
Multivariate |
||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Gender | ||||||
| Female | 16 721 | 59 | 1.00 | 1.00 | ||
| Male | 13 641 | 56 | 0.87 | 0.83–0.92 | 0.90 | 0.86–0.95 |
| Age (years) | ||||||
| 45–64 | 9721 | 57 | 1.00 | 1.00 | ||
| 16–24 | 1936 | 57 | 1.03 | 0.94–1.13 | 1.05 | 0.94–1.18 |
| 25–44 | 11 035 | 62 | 1.27 | 1.20–1.35 | 1.20 | 1.12–1.29 |
| 65+ | 7670 | 52 | 0.82 | 0.77–0.88 | 0.77 | 0.72–0.83 |
| Social class | ||||||
| Skilled manual and non-manual | 13 237 | 57 | 1.00 | 1.00 | ||
| Managerial and professional | 10 583 | 61 | 1.21 | 1.15–1.28 | 1.09 | 1.03–1.16 |
| Part skilled and unskilled | 6542 | 53 | 0.86 | 0.80–0.92 | 0.93 | 0.87–1.00 |
| Number of cars | ||||||
| 1 | 13 754 | 57 | 1.00 | |||
| 0 | 7117 | 52 | 0.80 | 0.75–0.85 | 0.96 | 0.89–1.03 |
| 2+ | 9491 | 61 | 1.17 | 1.12–1.24 | 1.03 | 0.96–1.09 |
| Smoking status | ||||||
| Never | 13 937 | 65 | 1.00 | 1.00 | ||
| Ex | 8811 | 59 | 0.79 | 0.75–0.84 | 0.86 | 0.81–0.92 |
| Light | 5375 | 46 | 0.46 | 0.43–0.49 | 0.45 | 0.42–0.48 |
| Heavy | 2239 | 34 | 0.28 | 0.25–0.31 | 0.28 | 0.25–0.31 |
| Adults in household | ||||||
| 2 | 16 323 | 59 | 1.00 | 1.00 | ||
| 1 | 9804 | 54 | 0.80 | 0.76–0.84 | 0.96 | 0.91–1.03 |
| 3+ | 4235 | 57 | 0.90 | 0.84–0.96 | 0.89 | 0.83–0.96 |
| Child in the household | ||||||
| No child <16 | 21 930 | 55 | 1.00 | 1.00 | ||
| <16 years | 8432 | 63 | 1.39 | 1.32–1.47 | 1.24 | 1.16–1.33 |
| Year | ||||||
| 2003–06 | 9392 | 56 | 1.00 | 1.00 | ||
| 1996–2002 | 17 510 | 60 | 0.83 | 0.79–0.88 | 0.85 | 0.80–0.90 |
| 2007–08a | 3460 | 59 | 0.95 | 0.88–1.03 | 0.92 | 0.84–1.01 |
For every consecutive increase in the predictor variable ‘year’, the OR represents the increase in odds of the outcome occurring. For all categorical variables, the OR describes a multiplicative change in the outcome compared with the reference category.
aThe 2008 data were collected in February and March 2009 due to a sampling error in October and November 2008.
Predictors of good knowledge
Adjusted multivariate logistic regression found age, gender, social class, smoking status, number of adults in the household, having a child under 16 in the household and time period, all independently predicted knowledge (Table 2). Odds of good knowledge were highest for 25- to 44-year-olds (OR: 1.20, 95% CI: 1.12–1.29) compared with 45- to 64-year-olds and for those of managerial and professional occupations (OR: 1.09, 1.03–1.16) compared with those of skilled occupation. Heavy (odds 0.28, 0.25–0.31), light (OR: 0.45, 0.42–0.48) and ex-smokers (OR: 0.86, 0.81–0.92) were all less likely to have good knowledge than never smokers. The presence of children in the household increased the odds of good knowledge (OR: 1.24, 1.16–1.33) compared with households with no children, whereas those living in households with three or more adults had lower odds (0.89, 0.83–0.96) compared with households with two adults. Odds of good knowledge were lower in 1996–2002 compared with 2003–06 (Odds 0.85, 0.80–0.90). There was no significant difference in the odds of good knowledge between 2007 and 2008 and between 2003 and 2006. The AUC value testing the predictive ability of the model was 0.63, P< 0.05, suggesting that the model was unable to fully explain all the variation in knowledge.
SHS-protective behaviours
In 2008, the percentage of respondents with smoke-free homes was 72% (69.4–73.6%); this was an 11% absolute increase since 2006. Amongst smokers, there was a smaller increase from 27% (22.6–30.4%) to 30% (25.0–34.7%) during the same period. In 2008, smoking abstinence was higher when in a room with a child (67%) than that with an adult (49%).
Knowledge and SHS-protective behaviours
The prevalence of smoke-free homes and smoking abstinence varied markedly with respondents' level of knowledge of SHS-related illnesses (Table 3).
Table 3.
Relationship between knowledge of SHS-related illnesses and SHS-protective behaviours
| Number of illnesses correctly identified |
Percentage respondents (95% confidence intervals) |
|||
|---|---|---|---|---|
|
Smoke-free home (2006–08) |
Smoking abstinence (1997–2008) with |
|||
| All | Smokers only | A child | Non-smoking adult | |
| 0–5 | 39 (35.7–41.5) | 16 (12.8–19.9) | 56 (54.2–58.1) | 42 (40.5–44.4) |
| 6–7 | 65 (62.5–68.0) | 33 (27.4–38.7) | 72 (69.3–73.8) | 49 (46.3–51.3) |
| 8–10 | 75 (73.9–76.7) | 35 (30.9–38.7) | 74 (72.8–76.0) | 54 (52.5–56.0) |
| Total | 66 (65.1–67.6) | 28 (25.8–30.8) | 67 (62.2–68.4) | 49 (47.7–50.0) |
Of those respondents who knew of 0–5 SHS-related illnesses, only 39% (35.7–41.5%) had smoke-free homes, whereas 75% (73.9–76.7%) of those with knowledge of 8–10 illnesses did. Similarly, amongst smokers, only 16% (12.8–19.9%) with knowledge of 0–5 illnesses had smoke-free homes compared with 35% (30.9–38.7%) of smokers with good knowledge.
Smoking abstinence in a room with a child for those with knowledge of 0–5 SHS-related illnesses was 56% (54.2–58.1%), while for those who were aware of 8–10 illnesses it was 74% (72.8–76.0%). Although abstinence was less prevalent when in a room with a non-smoking adult, better knowledge was associated with an increased proportion of abstinent smokers, 54% (52.5–56.0%) of those with knowledge of 8–10 illnesses compared with 42% (40.5–44.4%) of those who knew about only 0–5 illnesses.
Predictors of smoke-free homes: the population as a whole
Adjusted multivariate analysis found that knowledge of SHS-related illnesses predicted smoke-free homes with odds increasing by 18% (14–21%) for every unit increase in knowledge (Table 4). There was a significant increase in the prevalence of smoke-free homes between 2006 and 2007 (OR: 1.30, 1.09–1.56) and between 2006 and 2008 (OR: 1.58, 1.31–1.90). Respondents with part skilled or unskilled occupations and those with no car had poorer odds of having a smoke-free home (OR: 0.70, 0.57–0.86 and OR: 0.64, 0.53–0.78, respectively) compared with those of skilled occupation and those with one car. Heavy (OR: 0.09, 0.06–0.13), light (OR: 0.18, 0.14–0.22) and ex-smokers (OR: 0.81, 0.68–0.97) all had lower odds of a smoke-free home than never smokers. Those with a child under the age of 5 had much greater odds of a smoke-free home (OR: 2.33, 1.71–3.19) than those with no children under 16 years residing. Respondents' odds of a smoke-free home increased with each additional public place in which they agreed smoking restrictions were necessary (OR: 1.78, 1.61–1.97). The AUC was 0.82, P< 0.05, indicating that the model was a good fit of the data.
Table 4.
Logistic regression predicting smoke-free home incidence for all respondents and smokers only (2006–2008)
| Predictors |
All respondents |
Smokers only |
||||||
|---|---|---|---|---|---|---|---|---|
| n | Smoke free (%) | Univariate OR | Multivariate OR | n | Smoke free (%) | Univariate OR | Multivariate OR | |
| Sex | ||||||||
| Female | 2388 | 67 | 1.00 | 1.00 | 599 | 32 | 1.00 | |
| Male | 2842 | 65 | 0.92 (0.82–1.04) | 1.06 (0.91–1.24) | 565 | 24 | 1.47 (1.19–1.94) | 1.39 (1.00–1.93) |
| Age group (years) | ||||||||
| 45–64 | 1872 | 66 | 1.00 | 1.00 | 396 | 25 | 1.00 | 1.00 |
| 16–24 | 264 | 59 | 0.74 (0.59–0.93) | 0.95 (0.65–1.38) | 106 | 36 | 1.64 (1.06–2.55) | 0.97 (0.52–1.79) |
| 25–44 | 1739 | 69 | 1.17 (1.01–1.35) | 1.08 (0.88–1.33) | 477 | 31 | 1.33 (0.96–1.83) | 0.77 (0.51–1.16) |
| 65+ | 1416 | 66 | 1.01 (0.86–1.17) | 1.09 (0.90–1.33) | 185 | 16 | 0.59 (0.35–0.98) | 0.74 (0.41–1.35) |
| Social class | ||||||||
| Skilled manual and non-manual | 2346 | 66 | 1.00 | 1.00 | 567 | 29 | 1.00 | 1.00 |
| Managerial and professional | 1911 | 73 | 1.44 (1.25–1.66) | 0.98 (0.83–1.17) | 290 | 33 | 1.23 (0.88–1.73) | 0.96 (0.66–1.41) |
| Part skilled and unskilled | 1034 | 55 | 0.63 (0.53–0.74) | 0.70 (0.57–0.86) | 307 | 21 | 0.67 (0.46–0.99) | 0.79 (0.51–1.21) |
| Number of cars | ||||||||
| 1 | 2361 | 65 | 1.00 | 513 | 28 | 1.00 | 1.00 | |
| 0 | 1129 | 50 | 0.53 (0.46–0.62) | 0.64 (0.53–0.78) | 359 | 14 | 0.43 (0.29–0.62) | 0.47 (0.30–0.75) |
| 2+ | 1801 | 74 | 1.49 (1.29–1.71) | 1.17 (0.97–1.40) | 292 | 40 | 1.74 (1.27–2.39) | 1.46 (1.00–2.13) |
| Smoking status | ||||||||
| Never | 2444 | 79 | 1.00 | 1.00 | — | — | ||
| Ex | 1683 | 73 | 0.72 (0.62–0.84) | 0.81 (0.68–0.97) | — | — | ||
| Light | 846 | 33 | 0.13 (0.11–0.16) | 0.18 (0.14–0.22) | 846 | 33 | 1.00 | 1.00 |
| Heavy | 318 | 15 | 0.04 (0.03–0.06) | 0.09 (0.06–0.13) | 318 | 15 | 0.34 (0.23–0.49) | 0.47 (0.31–0.72) |
| Number of adults | ||||||||
| 2 | 2842 | 69 | 1.00 | 1.00 | 509 | 31 | 1.00 | 1.00 |
| 1 | 1745 | 58 | 0.61 (0.54–0.69) | 1.04 (0.88–1.23) | 475 | 16 | 0.42 (0.31–0.56) | 0.75 (0.51–1.10) |
| 3+ | 704 | 66 | 0.85 (0.72–1.00) | 1.07 (0.85–1.35) | 180 | 33 | 1.10 (0.78–1.54) | 1.07 (0.69–1.67) |
| Age of youngest child (years) | ||||||||
| No child <16 | 3982 | 64 | 1.00 | 1.00 | 813 | 24 | 1.00 | 1.00 |
| 0–4 | 597 | 77 | 1.85 (1.50–2.29) | 2.33 (1.71–3.19) | 154 | 42 | 2.36 (1.62–3.43) | 2.96 (1.77–4.96) |
| 5–10 | 392 | 66 | 1.09 (0.87–1.35) | 1.17 (0.87–1.58) | 115 | 29 | 1.29 (0.81–2.06) | 1.34 (0.77–2.33) |
| 11–15 | 320 | 71 | 1.34 (1.04–1.71) | 1.42 (1.03–1.97) | 82 | 41 | 2.18 (1.35–3.52) | 1.54 (0.94–2.52) |
| Year | ||||||||
| 2006 | 1833 | 61 | 1.00 | 1.00 | 444 | 27 | 1.00 | 1.00 |
| 2007 | 1785 | 67 | 1.26 (1.09–1.45) | 1.30 (1.09–1.56) | 393 | 29 | 1.14 (0.82–1.57) | 1.19 (0.82–1.71) |
| 2008a | 1673 | 72 | 1.58 (1.36–1.83) | 1.58 (1.31–1.90) | 327 | 30 | 1.18 (0.83–1.66) | 1.22 (0.81–1.83) |
| Knowledge of SHS illnesses | 1.29 (1.26–1.32) | 1.18 (1.14–1.21) | 1.16 (1.11–1.22) | 1.10 (1.04–1.16) | ||||
| Agreement with restrictions | 2.75 (2.52–2.99) | 1.78 (1.61–1.97) | 1.87 (1.60–2.19) | 1.64 (1.35–1.97) | ||||
The continuous predictors, knowledge and agreement with restrictions in public places produce a multiplier that describes the ORs of the outcome occurring for each unit increase in the predictor variable. For all categorical variables, the OR describes a multiplicative change compared with the reference category.
aThe 2008 data were collected in February and March 2009 due to a sampling error in October and November 2008.
Predictors of smoke-free homes: smokers only
Odds of a smoke-free home increased by 10% (4–16%) with every unit increase in knowledge. Smokers' odds also increased with agreement with restrictions in each additional public place. Heavy smokers had lower odds of having a smoke-free home (OR: 0.47, 0.31–0.72) compared with light smokers, as did those with no car (OR: 0.47, 0.30–0.75) compared with those with a car. Smokers with a child under 5 years had greater odds of a smoke-free home (OR: 2.96, 1.77–4.96). The AUC (0.74, P< 0.05) indicated that the model was a good fit.
Smokers' abstinence in a room with children and non-smoking adults: smokers only
The odds of abstinence when in a room with children increased by 11% (9–14%) for each unit increase in composite knowledge score and the odds of abstinence when in a room with a non-smoking adult by 6% (4–8%; Table 5). Additionally, the odds of abstinence were greater for each additional public place that smokers added to their list. Heavy smokers, compared with light smokers, respondents with a part skilled or unskilled occupation, compared with those of skilled occupation, and those with no car, compared with those with a car, were less likely to abstain, whilst those with two or more cars and those of managerial or professional occupation were more likely to. However, for the latter group, this relationship was only significant when in a room with a child (OR: 1.52, 1.29–1.78). Older smokers had greater odds of abstinence in both contexts than younger smokers. Having children 0–10 years old in the household predicted abstinence when in a room with non-smoking adults and having children aged 5–15 years predicted abstinence when in a room with children. Interestingly, having infants (0–4 years) in the household was significantly associated with being less likely to abstain in a room with children. The number of adults residing and gender were not significant predictors of abstinence when in a room with a child. However, compared with women, men were less likely to abstain when in a room with other non-smoking adults (OR: 0.88, 0.79–0.99). Compared with the period 2003–06, the odds of abstinence in a room with a child were lower in 1996–2002 (OR: 0.85, 0.74–0.97) but higher in 2007–08 (OR: 1.77, 1.40–2.24). However, abstinence in a room with adults was not significantly higher in this final period. The model for abstinence with children was a good fit of the data (AUC = 0.71, P< 0.05), whilst the model for abstinence with adults was not so good (AUC = 0.67, P< 0.05).
Table 5.
Logistic regression predicting smoking abstinence when in a room with a child or a non-smoking adult (smokers only, 1997–2008)
| Predictors |
Abstain when in a room with |
|||||||
|---|---|---|---|---|---|---|---|---|
|
A child |
A non-smoking adult |
|||||||
| n | Abstain (%) | Univariate OR | Multivariate OR | n | Abstain (%) | Univariate OR | Multivariate OR | |
| Sex | ||||||||
| Female | 3618 | 68 | 1.00 | 1.00 | 3619 | 51 | 1.00 | 1.00 |
| Male | 3071 | 67 | 0.97 (0.87–1.08) | 0.93 (0.82–1.05) | 3082 | 47 | 0.84 (0.77–0.93) | 0.88 (0.79–0.99) |
| Age group (years) | ||||||||
| 45–64 | 2099 | 65 | 1.00 | 1.00 | 2105 | 53 | 1.00 | 1.00 |
| 16–24 | 671 | 70 | 1.23 (1.02–1.48) | 0.95 (0.76–1.19) | 672 | 39 | 0.59 (0.49–0.70) | 0.42 (0.34–0.53) |
| 25–44 | 3049 | 67 | 1.08 (0.95–1.22) | 0.97 (0.83–1.14) | 3050 | 48 | 0.83 (0.74–0.93) | 0.59 (0.51–0.69) |
| 65+ | 870 | 71 | 1.32 (1.10–1.59) | 1.38 (1.12–1.69) | 874 | 57 | 1.18 (1.00–1.40) | 1.25 (1.04–1.50) |
| Social class | ||||||||
| Skilled manual and non-manual | 3108 | 67 | 1.00 | 1.00 | 3116 | 49 | 1.00 | 1.00 |
| Managerial and professional | 1677 | 77 | 1.64 (1.42–1.90) | 1.52 (1.29–1.78) | 1678 | 54 | 1.21 (1.06–1.38) | 1.07 (0.93–1.22) |
| Part skilled and unskilled | 1904 | 60 | 0.74 (0.65–0.84) | 0.82 (0.72–0.95) | 1907 | 45 | 0.83 (0.73–0.94) | 0.88 (0.77–1.01) |
| Number of cars | ||||||||
| 1 | 2962 | 68 | 1.00 | 1.00 | 2965 | 50 | 1.00 | 1.00 |
| 0 | 2084 | 61 | 0.73 (0.65–0.83) | 0.79 (0.68–0.92) | 2093 | 42 | 0.71 (0.63–0.80) | 0.80 (0.69–0.92) |
| 2+ | 1643 | 73 | 1.26 (1.10–1.45) | 1.17 (1.00–1.37) | 1643 | 53 | 1.11 (0.98–1.26) | 1.15 (1.00–1.33) |
| Smoking status | ||||||||
| Light | 4754 | 74 | 1.00 | 1.00 | 4760 | 54 | 1.00 | 1.00 |
| Heavy | 1935 | 51 | 0.37 (0.33–0.42) | 0.44 (0.38–0.50) | 1941 | 36 | 0.47 (0.42–0.53) | 0.50 (0.44–0.57) |
| Number of adults | ||||||||
| 2 | 3137 | 67 | 1.00 | 1.00 | 3140 | 50 | 1.00 | 1.00 |
| 1 | 2554 | 65 | 0.90 (0.81–1.00) | 0.99 (0.86–1.13) | 2562 | 48 | 0.90 (0.81–0.99) | 1.05 (0.93–1.19) |
| 3+ | 998 | 69 | 1.08 (0.93–1.25) | 1.04 (0.88–1.24) | 999 | 47 | 0.88 (0.77–1.01) | 1.01 (0.86–1.18) |
| Age of youngest child (years) | ||||||||
| No child <16 | 4437 | 70 | 1.00 | 1.00 | 4448 | 48 | 1.00 | 1.00 |
| 0–4 | 991 | 68 | 0.90 (0.78–1.05) | 0.89 (0.73–1.07) | 991 | 49 | 1.04 (0.90–1.19) | 1.27 (1.07–1.51) |
| 5–10 | 764 | 57 | 0.57 (0.48–0.67) | 0.52 (0.43–0.64) | 765 | 52 | 1.17 (1.00–1.38) | 1.36 (1.12–1.65) |
| 11–15 | 497 | 60 | 0.66 (0.54–0.80) | 0.61 (0.49–0.77) | 497 | 48 | 0.99 (0.81–1.20) | 1.11 (0.89–1.38) |
| Year | ||||||||
| 2003–06 | 2231 | 69 | 1.00 | 1.00 | 2232 | 47 | 1.00 | 1.00 |
| 1996–2002 | 3741 | 64 | 0.78 (0.69–0.88) | 0.85 (0.74–0.97) | 3751 | 50 | 1.13 (1.01–1.26) | 1.27 (1.12–1.43) |
| 2007–08a | 717 | 78 | 1.55 (1.26–1.91) | 1.77 (1.40–2.24) | 718 | 50 | 1.11 (0.93–1.33) | 1.15 (0.95–1.40) |
| Knowledge of SHS illnesses | 1.14 (1.12–1.16) | 1.11 (1.09–1.14) | 1.08 (1.06–1.09) | 1.06 (1.04–1.08) | ||||
| Agreement with restrictions | 1.55 (1.46–1.63) | 1.35 (1.27–1.44) | 1.44 (1.36–1.51) | 1.31 (1.23–1.39) | ||||
The continuous predictors, knowledge and agreement with restrictions in public places produce a multiplier that describes the ORs of the outcome occurring for each unit increase in the predictor variable. For all categorical variables, the OR describes a multiplicative change compared with the reference category.
aThe 2008 data were collected in February and March 2009 due to a sampling error in October and November 2008.
Discussion
Main findings of this study
To our knowledge, this quantitative study is the first in England to assess the trends in, and determinants of, knowledge of the specific illnesses related to SHS and to explore the relationship between knowledge and the implementation of SHS-protective behaviours such as smoke-free homes and smoking abstinence around others. Our findings show that respondents know SHS increases the risk of respiratory illnesses but are less aware of non-respiratory diseases. A quarter of the population were unaware that SHS exposure can cause heart disease in adults, whilst only a third knew SHS could cause ear infection in children and 55% cot death. Awareness has improved over the last decade, yet levels of knowledge remain low for these conditions.
‘Good knowledge’ (correct identification of an association between SHS and at least 8 of the 10 SHS-related illnesses) was most prevalent amongst never smokers (65%), falling to 34% among those smoking over 20 per day. In addition to being a non-smoker, having a child in the household, being aged 25–44 years, female and of higher social class were all predictive of good knowledge.
Our multivariate analysis suggests that knowledge was highest during the period of frequent SHS-related mass media campaigns (2003–06) and that post-SFL there was no further increase in knowledge. This coincided with the end of SHS-related mass media campaigns which in 2007 ran from March to April only.34 To our knowledge, there have been no further national, government-funded mass media campaigns that have focused specifically on SHS between May 2007 and March 2009—the last data collection point of this study. Campaigns in late 2007 and 2008/09 focused on smoking cessation34 and since April 2010 there have been no mass media campaigns at all.35
Knowledge was associated with smoke-free homes and abstinence from smoking when in a room with others even once potential confounders had been adjusted for. The odds of smokers having a smoke-free home increased by 9% with each unit increase in knowledge. Similarly, with each additional unit increase in knowledge, the odds of smoking abstinence increased by 11% when with children and 6% when with adults. Although our findings are cross sectional in nature, they do support earlier findings of a relationship between knowledge and smoking-related behaviour.18,19,24,36
Knowledge did not increase in 2007–08 but smoking abstinence with children did, as did smoke-free homes amongst non-smokers. There was no increase in abstinence around adults or smoke-free homes amongst smokers in 2007–08 compared with 2003–06. Whilst it is unknown why abstinence increased with children when knowledge concurrently decreased, it may be the case that smoking parents are subject to social desirability bias which may lead them to either falsely report abstinence or truly abstain when in a room with a child but not go as far to implement a smoke-free home. What is clear from this study is that more smokers with good knowledge have a smoke-free home compared with those with poor knowledge, 35 versus 16%, respectively (Table 3).
What is already known on this topic
Our findings are consistent with qualitative studies which suggest a relationship between knowledge of the dangers of SHS and SHS-protective behaviour.16,24,36 In California, smokers who believed that SHS was harmful were five times more likely to report living in a smoke-free home16 and in Tasmania, a mass media campaign highlighting the link between SHS and cot death successfully reduced child SHS exposure.36
As outlined above, to reduce experiences of cognitive dissonance, it is not uncommon for people to revise their beliefs to complement their behaviour.9 A qualitative study in England showed smoking mothers who smoked at home used risk-minimizing beliefs to justify their behaviour.37 Increasing knowledge of the impacts of SHS is required to challenge cognitive dissonance-based rationalizations that smokers make to justify their smoking behaviour and to encourage them to change their behaviour rather than their beliefs.24,38,39 Given that our results show that good knowledge was not more likely in 2007–08 compared with 2003–06, there is a case for further education campaigns in order to increase knowledge. This knowledge should be framed so that it combats functional and risk-minimizing beliefs and provides practical advice on how to protect children from SHS. Research investigating the impact of mass media campaigns on SHS-related knowledge and subsequent behaviour is also warranted.
Although we recognize that knowledge alone is unlikely to be sufficient to bring about behaviour change, given that knowledge acquisition is an important step in the process of behaviour change and that without knowledge, behaviour change is unlikely,1,6,7,39 the low levels of knowledge revealed in our study are cause for concern. This concern is further heightened by our findings of the significant link between knowledge and protective behaviours and that 52% of children with smoking parents in England still live in homes where smoking occurs.40
What this study adds
This study quantifies levels of knowledge by population subgroups and provides quantitative evidence that the knowledge of SHS-related illnesses is predictive of keeping a smoke-free home and abstaining from smoking in the presence of children and non-smoking adults. This link between knowledge and behaviour and its concurrence with topical mass media campaigns has potential implications for policy and practice. Given the lack of evidence for what really works in terms of producing smoke-free homes,41,42 and that little has hitherto been known about the levels of national SHS knowledge in England, our findings suggest a role for including knowledge in the development of future interventions and supports the recent call for further mass media campaigns to highlight the dangers of SHS24,41 in combination with information on the ineffectuality of some ‘protective’ measures and how smoke-free homes can be achieved.
Limitations of this study
Our data are cross sectional; it would be useful to examine the relationship between knowledge and SHS-protective behaviours using longitudinal data but such data were not available. Our logistic regression model for ‘good’ knowledge could have been a better fit, suggesting that there may be other important predictors of knowledge that we have not included in our analyses.
Due to the nature of self-reported data, we cannot rule out the possibility of social desirability bias amongst parents which leads them to report smoke-free homes and smoking abstinence in a room with a child as they wish to be seen as a considerate smoker, neither can we deny that this bias may have increased over time. However, cotinine measures have been used to verify self-reported prevalence of smoke-free homes in previous studies.27,40 Furthermore, some smokers may have a different view of ‘smoke free’ than others. A study with smoking mothers found a discrepancy whereby some women describe their homes as non-smoking whilst also reporting that they smoke in an open doorway, believing that this still constitutes a non-smoking home.43
Finally, it was not possible to discern whether respondents had a suitable outdoor space to smoke. One of the reported barriers to smoking outdoors is lack of appropriate space;44 future work needs to encompass the impact of such barriers.
Funding
This work was supported by the Policy Research Programme of the Department of Health (PR-SF-0707-10004). A.G. is supported by a Health Foundation Clinician Scientist Fellowship. A.G. is also a member of the UK Centre for Tobacco Control Studies (UKCTCS), a centre for public excellence which is funded by the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council, the Medical Research Council and the National Institute of Health Research. This funding is gratefully acknowledged.
Acknowledgements
This is an independent report and the views expressed are not necessarily those of the department.
References
- 1.Klesges RC, Somes G, Pascale RW, et al. Knowledge and beliefs regarding the consequences of cigarette smoking and their relationships to smoking status in a biracial sample. Health Psychol. 1988;7(5):387–401. doi: 10.1037//0278-6133.7.5.387. [DOI] [PubMed] [Google Scholar]
- 2.Farquhar JW, Maccoby N, Solomon DS. Community applications of behavioral medicine. In: Gentry WD, editor. Handbook of Behavioral Medicine. New York: Guilford; 1984. pp. 437–78. [Google Scholar]
- 3.Potvin L, Richard L, Edwards AC. Knowledge of cardiovascular disease risk factors among the Canadian population: relationships with indicators of socioeconomic status. Can Med Assoc J. 2000;162(9):S5–11. Suppl. [PMC free article] [PubMed] [Google Scholar]
- 4.Nourjah P, Wagener DK, Eberhardt M, et al. Knowledge of risk factors and risk behaviours related to coronary heart disease among blue and white collar males. J Public Health Policy. 1994;15:443–59. [PubMed] [Google Scholar]
- 5.Janz N, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 6.Siahpush M, McNeill A, Hammond D, et al. Socioeconomic and country variations in knowledge of health risks of tobacco smoking and toxic constituents of smoke: results from the 2002 International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl. III):iii65–70. doi: 10.1136/tc.2005.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stead M, MacAskill S, MacKintosh A-M, et al. ‘It's as if you're locked in’: qualitative explanations for area effects on smoking in disadvantaged communities. Health Place. 2001;7(4):333–43. doi: 10.1016/s1353-8292(01)00025-9. doi:10.1016/S1353-8292(01)00025-9. [DOI] [PubMed] [Google Scholar]
- 8.Festinger L. A Theory of Cognitive Dissonance. Stanford, CA: Stanford University Press; 1957. [Google Scholar]
- 9.Aronson E. The theory of cognitive dissonance: a current perspective. In: Berkowitz L, editor. Advances in Experimental Social Psychology. New York: Academic Press; 1969. [Google Scholar]
- 10.West R, Fidler J. Key Findings from the Smoking Toolkit Study. 2010. www.smokinginengland.info. archived by WebCite® at http://www.webcitation.org/5vUOJrB6v . [Google Scholar]
- 11.McMaster C, Lee C. Cognitive dissonance in tobacco smokers. Addict Behav. 1991;16(–):349–53. doi: 10.1016/0306-4603(91)90028-g. [DOI] [PubMed] [Google Scholar]
- 12.Lawton R, Conner M, McEachan R. Desire or reason: predicting health behaviors from affective and cognitive attitudes. Health Psychol. 2009;28(1):56–65. doi: 10.1037/a0013424. [DOI] [PubMed] [Google Scholar]
- 13.US Department of Health and Human Services. Atlanta, GA: US Department of Health and Human Services; 2007. Children and secondhand smoke exposure. Excerpts from the health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. [Google Scholar]
- 14.US Department of Health and Human Services. Atlanta: US Department of Health and Human Services, Centres for Disease Control and Prevention, National Centre for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. The health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. [Google Scholar]
- 15.Jamieson P. Risk perception and the 14–22 smoker and non-smoker. Unpublished Results. [Google Scholar]
- 16.Gilpin E, White M, Farkas A, et al. Home smoking restrictions: which smokers have them and how are they associated with smoking behavior. Nicotine Tob Res. 1999;1:153–62. doi: 10.1080/14622299050011261. [DOI] [PubMed] [Google Scholar]
- 17.Dunn J, Greenbank S, McDowell M, et al. Community knowledge, attitudes and behaviours about environmental tobacco smoke in homes and cars. Health Promot J Austr. 2008;19(2):113–17. doi: 10.1071/he08113. [DOI] [PubMed] [Google Scholar]
- 18.Phillips R, Amos A, Ritchie D, et al. Smoking in the home after the smoke-free legislation in Scotland: qualitative study. Br Med J. 2007;335:553. doi: 10.1136/bmj.39301.497593.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kegler MC, Malcoe L. Smoking restrictions in the home and car among rural native American and white families with young children. Prevent Med. 2002;35:334–42. doi: 10.1006/pmed.2002.1091. [DOI] [PubMed] [Google Scholar]
- 20.Weinstein ND. Smokers’ recognition of the vulnerability to harm. In: Slovic P, editor. Smoking: Risk, Perception and Policy. London: 2001. [Google Scholar]
- 21.Davidson WP. The third person effect in communication. Public Opin Q. 1983;47(1):1–15. [Google Scholar]
- 22.Mahabee-Gittens M. Smoking in parents of children with asthma and bronchitis in a pediatric emergency department. Pediatr Emerg Care. 2002;18(1):4–7. doi: 10.1097/00006565-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Blackburn C, Spencer N, Bonas S, et al. Effect of strategies to reduce exposure of infants to environmental tobacco smoke in the home: cross sectional survey. Br Med J. 2003;327:257–61. doi: 10.1136/bmj.327.7409.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones L, Atkinson O, Longman J, et al. The motivators and barriers to a smokefree home among disadvantaged caregivers: identifying the positive levers for change. Nicotine Tob Res. 2011;13(6):479–86. doi: 10.1093/ntr/ntr030. [DOI] [PubMed] [Google Scholar]
- 25.Arnott D, Dockrell M, Sandford A, et al. Comprehensive smoke-free legislation in England: how advocacy won the day. Tob Control. 2007;16(6):423–8. doi: 10.1136/tc.2007.020255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borland R, Mullins R, Trotter L, et al. Trends in environmental tobacco smoke restrictions in the home in Victoria, Australia. Ann Rev Public Health. 1999;8:266–71. doi: 10.1136/tc.8.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jarvis MJ, Mindell J, Gilmore A, et al. Smoke-free homes in England: prevalence, trends and validation by cotinine in children. Tob Control. 2009;18:491–5. doi: 10.1136/tc.2009.031328. [DOI] [PubMed] [Google Scholar]
- 28.Callinan JE, Clarke A, Doherty K, et al. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption (review) Cochrane Database Syst Rev. 2010;(4):1–126. doi: 10.1002/14651858.CD005992.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Economic and Social Data Service. The Office of National Statistics Omnibus Survey: resources. http://www.esds.ac.uk/government/omnibus/resources/ 12 August 2010, date last accessed.
- 30.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd edn. New York: Wiley; 2000. [Google Scholar]
- 31.Field A. Discovering Statistics Using SPSS (and Sex, Drugs and Rock ‘n’ Roll) 2nd edn. London: Sage; 2005. [Google Scholar]
- 32.Office of National Statistics. Estimates for UK, England, Wales, Scotland and Northern Ireland: Current Datasets. http://www.statistics.gov.uk/statbase/Product.asp?vlnk=15106. 12 August 2010, date last accessed. [Google Scholar]
- 33.Robinson S, Lader D. Smoking and Drinking amongst Adults, 2007. The General Household Survey. Newport: Office for National Statistics; 2009. [Google Scholar]
- 34.Department of Health. Smokefree England. 2007. http ://www.smokefreeengland.co.uk/thefacts/campaigns.html. (11 January 2011, date last accessed)
- 35.Aveyard P, Amos A, Bauld L, et al. Is the UK's coalition government serious about public health? Lancet. 2010;376:589. doi: 10.1016/S0140-6736(10)61288-3. [DOI] [PubMed] [Google Scholar]
- 36.Ponsonby A, Couper D, Dwyer T. Features of infant exposure to tobacco smoke in a cohort study in Tasmania. J Epidemiol Community Health. 1996;50:40–6. doi: 10.1136/jech.50.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robinson J, Kirkcaldy AJ. ‘You think that I'm smoking and they're not’: why mothers still smoke in the home. Soc Sci Med. 2007;65(4):641–52. doi: 10.1016/j.socscimed.2007.03.048. [DOI] [PubMed] [Google Scholar]
- 38.Yong HH, Borland R. Functional beliefs about smoking and quitting activity among adult smokers in four countries: findings from the International Tobacco Control Four-Country Survey. Health Psychol. 2008;27(3):S216–23. doi: 10.1037/0278-6133.27.3(suppl.).s216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borland R, Yong HH, Wilson N, et al. How reactions to cigarette packet health warnings influence quitting: findings from the ITC four-country survey. Addiction. 2009;104:669–75. doi: 10.1111/j.1360-0443.2009.02508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jarvis MJ, Sims M, Gilmore A, et al. Impact of smokefree legislation on children's exposure to secondhand smoke: cotinine data from the Health Survey for England. Tob Control. 2011 doi: 10.1136/tc.2010.041608. Published Online First 27 April 2011. doi://10.1136/tc.2010.041608 http://tobaccocontrol.bmj.com/content/early/2011/04/27/tc.2010.041608.full.pdf . [DOI] [PubMed] [Google Scholar]
- 41.Royal College of Physicians. Passive Smoking and Children: A Report by the Tobacco Advisory Group. London: RCP; 2010. [Google Scholar]
- 42.Roseby R, Waters E, Polnay A, et al. Family and carer smoking control programmes for reducing children's exposure to environmental tobacco smoke (review) Cochrane Database Syst Rev. 2002;(3) doi: 10.1002/14651858.CD001746. CD001746. [DOI] [PubMed] [Google Scholar]
- 43.Robinson J, Kirkcaldy AJ. Disadvantaged mothers, young children and smoking in the home: mothers’ use of space within their homes. Health Place. 2007;13:894–903. doi: 10.1016/j.healthplace.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 44.Hill L, Farquharson K, Borland R. Blowing smoke: strategies smokers use to protect non-smokers from environmental tobacco smoke in the home. Health Promot J Austr. 2003;14(3):196–201. [Google Scholar]