Abstract
Background
The object of this study was to determine if cerebrospinal fluid (CSF) shunt revision(s) are associated with increased risk of CSF shunt infection, after adjusting for baseline factors that contribute to infection risk.
Methods
This was a retrospective cohort study of 579 children ages 0 to 18 who underwent initial CSF shunt placement between 1/1/97 and 10/12/06 at a tertiary care children’s hospital. The outcome of interest was CSF shunt infection. Data for all subsequent CSF shunt revisions leading up to and including the initial CSF shunt infection, when applicable, were obtained. The likelihood of infection was determined using a Cox proportional hazard model accounting for patient characteristics and CSF shunt revisions, and is reported using hazard ratios (HR) with 95% confidence intervals (CI).
Results
There were 123 children who developed infection. Baseline factors independently associated with hazard of infection included age 0 to <6 months at CSF shunt placement (HR 2.4, 95% CI: 1.02, 6.7) and myelomeningocele (HR 0.4, 95% CI: 0.2, 0.8). Controlling for baseline factors, the risk of infection after shunt revision was significantly greater than at the time of initial placement (HR 3.0, 95% CI: 1.9, 4.7), and this risk increased as numbers of revisions increased (≥2 revisions HR 6.5, 95% CI: 3.6, 11.4).
Conclusions
While younger age is associated with increased hazard of infection, subsequent CSF shunt revision significantly increases infection risk.
Keywords: cerebrospinal, shunt, infection, revision, failure, children
Introduction
While placement of cerebrospinal fluid (CSF) shunts successfully treats hydrocephalus in children, CSF shunt complications – including shunt failure and infection – are common and frequently necessitate subsequent surgeries.1–3 CSF shunt infections in particular pose a serious problem for children with hydrocephalus, their parents, and their caregivers. Each year in the United States there are 2,200–2,400 infection admissions, accounting for 49–59,000 hospital days.4 Treatment typically involves two surgeries, as well as a prolonged hospitalization while receiving intravenous (IV) antibiotics.5 Re-infection rates are 20 to 25%.6,7
The association of both patient risk factors and factors at the time of initial CSF shunt placement with CSF shunt infection is complicated by intervening CSF shunt revisions. For example, it is known that the risk of shunt failure is highest immediately after CSF shunt surgery (both for initial CSF shunt placement and for revision) and declines with time.8 Risk of repeated shunt failure appears highest in those who require revision shortly after placement.9,10 Like the risk of shunt failure, the risk of infection also declines with time following revisions.8 Interval CSF shunt revision(s)11 and previous infection6,7,12 are associated with increased odds of infection. However, the relative contribution of each intervening revision surgery, and its relationship to baseline risk of infection for a given child, remains unknown.
Our previous work assembled a large and detailed retrospective cohort of 579 children undergoing initial CSF shunt placement, including details for all subsequent CSF shunt revisions leading up to and including initial CSF shunt infection.13 The object of this study was to quantify the extent to which CSF shunt revision(s) are associated with increased risk of CSF shunt infection, after adjusting for patient factors that may contribute to infection risk. We also considered as potential confounders surgeon as well as medical and surgical decisions at the time of last surgery (either initial shunt placement or revision surgery).
Materials and Methods
Study Design and Setting
As previously described,13 we conducted a retrospective cohort study at Primary Children’s Medical Center (PCMC. PCMC is a tertiary children’s hospital and pediatric neurosurgical referral center serving Utah, Idaho, Wyoming, Nevada, and Montana with more than 11,000 admissions per year. The study was reviewed and approved by the Institutional Review Boards at the University of Utah and Seattle Children’s Research Institute as research not requiring informed consent.
Study Population
Children 18 years of age who underwent initial CSF shunt placement with a discharge date between 1/1/1997 and 10/12/2006 at PCMC were eligible for inclusion as described previously. 13
Data Collection
Data from each neurosurgical admission for each cohort member up until the time of CSF shunt infection were collected using Intermountain Healthcare’s database and chart review. The date of censoring was the date of most recent surgery or 10/12/06, whichever was latest. When review of medical records found that a child had died, moved, or had their CSF shunt removed, the date of that event was the date of censoring.
Primary Outcome Variable
The primary outcome is the first CSF shunt infection the child experienced. CSF shunt infection was defined as the presence of bacteria in a culture or Gram stain of CSF, wound swab, and/or pseudocyst fluid or shunt erosion (visible hardware) or abdominal pseudocyst (even without positive culture). In children with a ventriculoatrial shunt, presence of bacteria in a blood culture was also diagnostic of infection.
Predictor variable
The main predictor variable of interest is CSF shunt revision, defined as an interventional neurosurgical operative procedure performed on the CSF shunt. In cases where a staged revision was performed in two or more stages (such as externalization of a shunt followed several days later by re-internalization), the procedures were considered as a single CSF shunt revision. The time period between staged procedures was considered non-contributory to infection risk, and details of medical and surgical decisions at the time of only the last neurosurgical procedure were considered in analyses. In the occasional case where a CSF shunt revision procedure preceded a CSF shunt infection neurosurgical procedure within 48 hours, the revision was not regarded as potentially contributory to the infection episode.
Baseline Factors and Potential Confounding Variables
Potential confounding variables included patient risk factors such as demographics (gender, race/ethnicity, insurance); risk factors prior to initial CSF shunt placement (birth weight, gestational age, length of hospital stay (LOS) before initial CSF shunt placement, antibiotic use during hospital stay before initial CSF shunt placement, prior surgeries, prior neurosurgical procedures, prior neurosurgical device infection (such as external ventricular drain (EVD), reservoir, lumboperitoneal shunt, baclofen pump); and risk factors at the time of initial CSF shunt placement (chronological age, indication for CSF shunt placement, weight at surgery, and complex chronic condition(s) (CCCs).13 Age at the time of initial CSF shunt placement was categorized and additionally, in sensitivity analyses, treated as a continuous variable (in weeks). To characterize co-morbidities, we used CCCs14–16 revised to exclude hydrocephalus 4 from the discharge diagnoses assigned prior to the initial shunt placement; CCCs include genetic disorders (neuromuscular, metabolic disorders, and congenital or genetic defects) and immunologic status (immunodeficiencies and malignancies).
In addition to patient factors and revision procedures, we also report surgeon factors and medical and surgical decisions at preceding CSF shunt surgeries (initial CSF shunt placement and/or CSF shunt revision) as previously described.13 Variables of interest that we considered included doses and timing of intraoperative antibiotics, shunt brand, intraoperative use of neuroendoscope and ultrasound, person preparing shunt site, case priority, duration of case in minutes, number of scrubbed people in operating room, use of antibiotic impregnated shunt tubing, proximal and distal shunt locations, IV antibiotic use 1 hour or more before surgical incision; and for CSF shunt revisions alone, we considered the indication for revision obtained from chart review; bedside procedures; and staged revisions. Bedside procedures were those for which data from the operating room database was not available and, in most cases, bedside location was confirmed in chart review.
Statistical Analyses
Cohort characteristics at baseline were summarized overall and by subsequent infection status. Binary and categorical variables were described using frequencies and percents, and continuous variables were described using means and standard deviations (SD) or medians and interquartile ranges (IQR) for duration of follow-up, time to infection, and other skewed variables. Univariate survival analyses were performed to test the associations of each cohort characteristics with infection.
Cox proportional hazard models were used to calculate hazard ratios (HR), a type of rate ratio estimate, and to test for the association between CSF shunt revision(s) and CSF shunt infection while controlling for possible confounding baseline characteristics.17,18 CSF shunt revision(s) were categorized as none, one, and two or more; and were treated as a time-dependent covariate, since an individual child’s revision status could change during the study period. For each day on which an infection occurred, this time-dependent model compared the infection hazard among children who had not experienced a shunt revision to date to those who had experienced one or two or more.
Baseline characteristics included a priori were age, gender, and indication for shunt placement. Additional baseline characteristics shown in Supplemental Digital Content 1 (Table) were evaluated for inclusion in the model using stepwise regression methodology.19,20 Using this approach, the model is initiated with a forward selection step in which a single variable is added to the model, and each forward selection step may be followed by one or more backward elimination steps in each of which a single variable may be removed from the model.21 Criterion for entry into the model was p ≤ 0.05; criterion for removal from the model was p > 0.05. Hazard ratios (HR) from the final multivariable models are presented with 95% profile likelihood confidence intervals (CI).
Sensitivity analyses were performed to investigate whether surgeon factors and medical and surgical decisions (either at initial placement or revision) may mediate the relationship between revisions and infection. These factors were evaluated in the final multivariable model to determine whether the association between revisions and infections was altered by inclusion of these additional factors.
All analyses were performed using SAS (version 9.1.3, SAS Institute, Cary, NC).
Results
Cohort characteristics
Baseline patient-level risk factors at the time of CSF shunt placement are shown in SDC 1 (table). The cohort had a median age of 14 weeks (IQR 2, 69), and indication for CSF shunt placement was distributed between myelomeningocele (21%), post-IVH due to prematurity (15%), aqueductal stenosis (12%), and other etiologies. The association of these baseline patient-level risk factors with CSF shunt infection is provided in the footnote to SDC 1 (table). In univariate survival analyses, factors that demonstrated a significant association with infection risk included shorter LOS preceding initial shunt placement, younger chronological age both in weeks and from age 0 to <6 months, and lower weight at initial CSF shunt placement. Myelomeningocele was associated with less infection risk compared with aqueductal stenosis.
In this cohort, infections were diagnosed by one or more of the following: presence of bacteria in a Gram stain (n=64) and/or culture of CSF (n=105), wound swab or pseudocyst fluid (n=14); visible hardware (n=20); abdominal pseudocyst (n=2); and blood culture in a VA shunt (n=5).
Of the 579 children in the cohort, the median duration of follow-up from initial CSF shunt placement was 1039 days (IQR 226– 2222 days) and from last surgery was 709 days (IQR 104– 1753 days). (Table 1) For the 123 children who developed shunt infection, the median time to infection was 39 days (IQR 17 – 171 days) from initial CSF shunt placement and 20 days (IQR 11- 39 days) from last surgery. Within the cohort there was sufficient follow-up for development of infection, which consistently developed at a median of 3 weeks (IQR 1.5 to 5 weeks) following CSF shunt surgery. Among the cohort, 504 (87%) children had follow-up for at least 12 months, during which time 106 children developed infection and there were 560 additional revisions. Within this cohort, we observed a one-year per-patient infection rate of 21% (95% CI: 17–25%) and associated per-procedure infection rate of 10% (95% CI: 8–12%).
Table 1.
Numbers of infections and median (IQR) duration of follow-up in days for the cohort
| Number of Revisions | Number of children | Duration of follow-up for all children | Number of infections | Time to infection for those infected |
|---|---|---|---|---|
| Since initial CSF shunt surgery | ||||
| Overall | 579 | 1039 (226, 2222) | 123 | 39 (17, 171) |
| No revisions | 352 | 745 (128, 1834) | 73 | 20 (12, 39) |
| One revision | 116 | 1292 (262, 2610) | 29 | 120 (45, 230) |
| Two or more revisions | 111 | 1848 (959, 2955) | 21 | 469 (130, 1533) |
| Since last CSF shunt surgery | ||||
| Overall | 579 | 709 (104, 1753) | 123 | 20 (11, 39) |
| No revisions | 352 | 745 (128, 1834) | 73 | 20 (12, 39) |
| One revision | 116 | 674 (95, 1782) | 29 | 26 (10, 69) |
| Two or more revisions | 111 | 598 (85, 1411) | 21 | 18 (11, 34) |
Association between revisions and infection risk
Our multivariable model of infection risk demonstrates the HRs for CSF shunt infection for each of the explanatory variables while controlling for the other explanatory variables. (Table 2) Age 0 to <6 months at CSF shunt placement was significantly associated with an increased risk of infection (HR 2.4, 95% CI: 1.02, 6.7), while myelomeningocele was significantly associated with a decreased risk of infection (HR 0.4, 95% CI: 0.2, 0.8). When age was handled as a continuous variable, a similar trend was seen; for each additional 4 weeks of age at the time of initial CSF shunt placement, hazard of infection decreased slightly HR 0.996 (95% CI: 0.991, 1.00007, p=0.053). Gender was not associated with infection.
Table 2.
Results from multivariable Cox proportional hazard model for the association between revisions and subsequent CSF shunt infection, adjusting for baseline characteristics and confounders
| Adjusted Hazard Ratio (95% CI)
|
|
|---|---|
| Revision procedure | |
| Two or more | 6.5 (3.6, 11.4) |
| One | 3.0 (1.9, 4.7) |
| None | Referent |
| Chronological age at initial shunt placement | |
| 0 to < 6 months | 2.4 (1.02, 6.7) |
| 6 to < 12 months | 1.5 (0.5, 4.9) |
| 1 to < 2 years | 2.7 (0.9, 8.7) |
| 2 to < 9 years | 2.2 (0.9, 6.1) |
| 9 to 18 years | Referent |
| Male gender | 0.9 (0.7, 1.4) |
| Indication for initial shunt placement | |
| Myelomeningocele | 0.4 (0.2, 0.8) |
| Post-IVH due to prematurity | 1.1 (0.6, 2.0) |
| Post-head injury | 0.5 (0.2, 1.4) |
| Tumor (posterior fossa, midbrain, supratentorial) | 0.6 (0.2, 1.3) |
| Cyst (other intracranial, posterior fossa) | 1.0 (0.5, 2.0) |
| Spontaneous ICH/IVH/SAH | 0.8 (0.3, 2.1) |
| Post-infectious | 0.6 (0.2, 1.5) |
| Congenital (communicating, other, encephalocele, craniosynostosis) | 1.1 (0.5, 2.3) |
| Other | 1.0 (0.3, 3.2) |
| Aqueductal stenosis | Referent |
Controlling for age, gender, and indication for shunt placement, infection hazard after subsequent revision(s) was significantly greater than during the time prior to first revision. In the time period following a single revision, infection hazard tripled (HR 3.0, 95% CI: 1.9, 4.7) compared with the time period prior to a single revision. Infection hazard was 6.5 times greater following two or more revisions (HR 6.5, 95% CI: 3.6, 11.4).
Sensitivity analyses
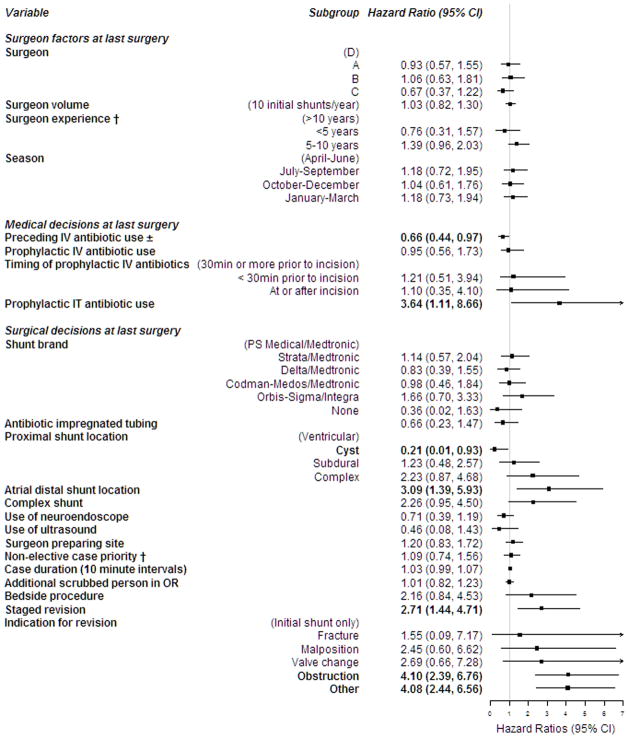
Sensitivity analyses were performed to determine whether the association between revisions and infections were confounded by surgeon factors and medical and surgical decisions. However, because medical and surgical decisions, as well as surgeon volume and experience, are highly confounded by surgeon in this small data set, our ability to draw meaningful conclusions about them is quite limited.13 Several surgeon factors, medical and surgical decisions at the preceding surgeries (initial CSF shunt placement and/or CSF shunt revision) were associated with infection hazard in univariate survival analysis including: prophylactic IT antibiotic use, atrial distal shunt location, staged revision procedure, and either obstruction or other as the indication for shunt revision. (Figure 1) Preceding IV antibiotic use and proximal shunt location in cyst appeared to be protective of CSF shunt infection. Each of the surgeon factors and medical and surgical decisions were added to the multivariable Cox proportional hazards model in Table 2 to evaluate whether the association between revisions and infection remained significant. Only two factors demonstrated a significant association with infection hazard: proximal shunt location in cyst and ultrasound use. However, the inclusion of these additional factors had no impact on the HR estimates for revisions or their significance.
Figure 1.
Discussion
In a large cohort of children undergoing initial CSF shunt placement and followed for a median of 34 months, 21% developed CSF shunt infection. We developed robust models that quantified the relative contributions of baseline patient factors (including indication for CSF shunt placement) as well as each revision surgery to the risk of infection. Baseline patient factors independently associated with subsequent infection included younger age (increased risk) and myelomeningocele (decreased risk). Revision surgery was significantly associated with infection risk, and this risk increased dramatically with subsequent revisions. Surgeon factors and medical and surgical decisions involved in shunt surgeries, both at initial placement and revision surgery, did not alter the relationship between revisions and infection. While observed in clinical practice, no previous studies have quantified this dramatic and clinically important risk of infection associated with revisions.
The 12-month rate of shunt infection in this large cohort of children undergoing initial CSF shunt placement was 21% per patient and 10% per procedure. These infection rates are comparable to previous work which has consistently ranged from 4 to 21%11 (usually 6–8% in published cohorts22–25) per patient and 3 to 13% per procedure.11 Our infection rate may be somewhat higher than previous studies in part because we removed children who did not have 12 months of follow-up within our health care system from the cohort.
Previous studies of CSF shunt infection at a procedure-level – which can be problematic in assessing patient-level factors since a given patient may be counted several times – have suggested that young chronological age is associated with infection,12,26–29 although a few have found the opposite.30,31 Two studies have examined risk of CSF shunt infection at a patient-level with young age and arrived at opposite conclusions.25,32 Like Vinchon et al.,25 this study found younger age was independently associated with risk of CSF shunt infection. The association of infection with young age may be due to alterations in the immunologic and dermatologic defenses among newborns, particularly among those who are premature.
Previous study of CSF shunt infection at a procedure-level has also suggested that indication for shunt placement (including IVH,12,28,30 CNS infection,28 and myelomeningocele33) may or may not 26,31,34,35 be associated with infection. One patient cohort found that both myelomeningocele and IVH were associated with CSF shunt infection.25 In our study, we did not replicate findings about myelomeningocele and actually found it associated with decreased infection risk. While we did not replicate an association of IVH with infection, we have shown that IVH in this cohort is associated with shunt failure,13 which was shown in this study to be strongly associated with infection.
Other patient risk factors considered in studies of CSF shunt infection – although again, studied mostly at a procedure-level – have included gender;12,26,28,34,36 birth weight; 28,37 gestational age;8,12,28,37 hospital days prior to shunt placement;34 weight at surgery;34 and co-morbidities.26,31,34 Conclusions about birth weight and gestational age are limited in this cohort due to missing data, and no additional factors were independently associated with infection risk in this study. Like Kulkarni et al., we saw an association between lower weight at surgery with infection in univariate survival analysis; however fewer hospital days prior to initial shunt placement were associated with infection in our study.
Conclusions about medical and surgical decisions are very limited in this small data set as they vary between and are highly confounded by surgeon.13 Medical and surgical decisions that prevent CSF shunt infection include use of prophylactic IV antibiotics;34,38 type of skin cleanser;39,40 site preparation including hair clipping40,41 and shampoo;40,42,43 antibiotic irrigation of hardware;40 and double gloving.34 However, because most studies are performed retrospectively and can be underpowered at single centers, they frequently arrive at opposing conclusions. Areas of ongoing controversy in the prevention of CSF shunt infection include the use of prophylactic IT antibiotics;30,39,44,45 type of shunt;31,46 antibiotic impregnated shunt tubing;47–50 distal shunt location;29,31,32,35,36,51 use of neuroendoscope;12,34 duration of case;34,36,40,51 case priority;30,32,34,40 and people in the operating room.34,39,40 In this study, none of the surgeon factors or medical and surgical decisions contributed substantially to infection risk beyond CSF shunt revision itself.
Our finding of each subsequent CSF shunt revision increasing infection risk for a patient is consistent with prior studies.11 This finding makes sense, since surgery represents an opportunity to introduce new organisms into the CSF and onto shunt hardware. Indeed, the close temporal relationship between surgery and infection seen in earlier work8 was replicated in this study. Both after initial placement and each revision, infection consistently developed at median of three weeks after surgery.
This work has several limitations inherent to retrospective studies that rely on medical record review. There are patient risk factors we may have failed to or are unable to capture in this analysis. Missing data on gestational age and birth weight limits our ability to draw conclusions about these patient factors. Factors that were not documented in the medical record were presumed not to have occurred; in a few cases, such as antibiotic-impregnated shunt tubing, this assumption may be erroneous. We were not able to consider several additional variables including type of skin cleanser;39,40 site preparation including hair clipping40,41 and shampoo;40,42,43 antibiotic irrigation of hardware;40 double gloving;34 and patient positioning. Some limitations were presented by conduct at a single center; our conclusions about medical and surgical decisions are highly confounded by their association with surgeon in this cohort. These findings must be validated in a larger cohort of patients with more surgeons and centers. Finally, while we were able to ascertain associations for various factors with infection, we have not established their causality of infection.
Despite the study’s limitations, this was a comprehensive study using a large, detailed retrospective observational cohort of children undergoing initial CSF shunt placement to examine risk factors for shunt infection. Baseline patient factors associated with subsequent infection included younger age (increased risk) and myelomeningocele (decreased risk), but infection risk increases most as numbers of revisions increase. Families of and care providers for children with recurrent CSF shunt revisions should be aware of their increased odds of CSF shunt infection.
Supplementary Material
Acknowledgments
We thank the following parties for assistance in the execution of this project: PCMC Division of Inpatient Medicine, particularly Christopher Maloney, Flory Nkoy, Gena Fletcher Lattin, and Ali Dowling (construction of the data collection tools); Neal Swensen and Jared Olson from PCMC Pharmacy (antibiotic data); Barb Nelson (medical chart retrieval); Jeff Yearley and Rene Enriquez (data management); the Pediatric Clinical and Translational Research program at the University of Utah including Heather Keenan and Carrie Byington (project conceptualization); Laina Mercer (figure construction); as well as Stephan Nemeth for support and valuable feedback.
Footnotes
Conflicts of Interest and Source of Funding: None of the authors have potential financial, personal, or professional conflicts of interest to disclose. This publication was supported by a PCMC Innovative Research Grant and the Children’s Health Research Center at the University of Utah which provided salary support for ML. Ongoing support for investigators includes Award K23NS062900 from the National Institute of Neurological Disorders And Stroke (NINDS) for TDS and KW; Seattle Children’s Center for Clinical and Translational Research and CTSA Grant Number ULI RR025014 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) for TDS, KW, and NMH; and the Child Health Corporation of America via the Pediatric Research in Inpatient Setting Network Executive Council for TDS. Past support for investigators included Award 1RC1NS068943-01 from NINDS for TDS, JRC, JK, and RH. None of the sponsors participated in design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH.
References
- 1.Browd SR, Gottfried ON, Ragel BT, Kestle JR. Failure of cerebrospinal fluid shunts: part II: overdrainage, loculation, and abdominal complications. Pediatr Neurol. 2006 Mar;34(3):171–176. doi: 10.1016/j.pediatrneurol.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 2.Browd SR, Ragel BT, Gottfried ON, Kestle JR. Failure of cerebrospinal fluid shunts: part I: Obstruction and mechanical failure. Pediatr Neurol. 2006 Feb;34(2):83–92. doi: 10.1016/j.pediatrneurol.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 3.Garton HJ, Kestle JR, Drake JM. Predicting shunt failure on the basis of clinical symptoms and signs in children. J Neurosurg. 2001 Feb;94(2):202–210. doi: 10.3171/jns.2001.94.2.0202. [DOI] [PubMed] [Google Scholar]
- 4.Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JR. Hospital care for children with hydrocephalus in the United States: utilization, charges, comorbidities, and deaths. J Neurosurg Pediatrics. 2008 Feb;1(2):131–137. doi: 10.3171/PED/2008/1/2/131. [DOI] [PubMed] [Google Scholar]
- 5.Whitehead WE, Kestle JR. The treatment of cerebrospinal fluid shunt infections. Results from a practice survey of the American Society of Pediatric Neurosurgeons. Pediatr Neurosurg. 2001 Oct;35(4):205–210. doi: 10.1159/000050422. [DOI] [PubMed] [Google Scholar]
- 6.Kulkarni AV, Rabin D, Lamberti-Pasculli M, Drake JM. Repeat cerebrospinal fluid shunt infection in children. Pediatr Neurosurg. 2001 Aug;35(2):66–71. doi: 10.1159/000050393. [DOI] [PubMed] [Google Scholar]
- 7.Kestle JR, Garton HJ, Whitehead WE, et al. Management of shunt infections: a multicenter pilot study. J Neurosurg. 2006 Sep;105(3 Suppl):177–181. doi: 10.3171/ped.2006.105.3.177. [DOI] [PubMed] [Google Scholar]
- 8.McGirt MJ, Leveque JC, Wellons JC, 3rd, et al. Cerebrospinal fluid shunt survival and etiology of failures: a seven-year institutional experience. Pediatr Neurosurg. 2002 May;36(5):248–255. doi: 10.1159/000058428. [DOI] [PubMed] [Google Scholar]
- 9.Piatt JH, Jr, Carlson CV. A search for determinants of cerebrospinal fluid shunt survival: retrospective analysis of a 14-year institutional experience. Pediatr Neurosurg. 1993 Sep-Oct;19(5):233–241. doi: 10.1159/000120738. discussion 242. [DOI] [PubMed] [Google Scholar]
- 10.Shah SS, Hall M, Slonim AD, Hornig GW, Berry JG, Sharma V. A multicenter study of factors influencing cerebrospinal fluid shunt survival in infants and children. Neurosurgery. 2008 May;62(5):1095–1102. doi: 10.1227/01.neu.0000325871.60129.23. discussion 1102–1093. [DOI] [PubMed] [Google Scholar]
- 11.Simon TD, Hall M, Riva-Cambrin J, et al. Infection rates following initial cerebrospinal fluid shunt placement across pediatric hospitals in the United States. Clinical article. J Neurosurg Pediatr. 2009 Aug;4(2):156–165. doi: 10.3171/2009.3.PEDS08215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ. Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis. 2003 Apr 1;36(7):858–862. doi: 10.1086/368191. [DOI] [PubMed] [Google Scholar]
- 13.Simon T, Whitlock K, Riva-Cambrin J, et al. Association of intraventricular hemorrhage secondary to prematurity with cerebrospinal fluid shunt surgery in the first year following initial shunt placement. Journal of Neurosurgery: Pediatrics. 2012;9(1):54–63. doi: 10.3171/2011.10.PEDS11307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001 Jun;107(6):E99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 15.Feudtner C, Silveira MJ, Christakis DA. Where do children with complex chronic conditions die? Patterns in Washington State, 1980–1998. Pediatrics. 2002 Apr;109(4):656–660. doi: 10.1542/peds.109.4.656. [DOI] [PubMed] [Google Scholar]
- 16.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000 Jul;106(1 Pt 2):205–209. [PubMed] [Google Scholar]
- 17.Allison MA, Daley MF, Crane LA, et al. Influenza vaccine effectiveness in healthy 6- to 21-month-old children during the 2003–2004 season. J Pediatr. 2006 Dec;149(6):755–762. doi: 10.1016/j.jpeds.2006.06.036. [DOI] [PubMed] [Google Scholar]
- 18.Allison PA. Survival analysis using the SAS system; a practical guide. Cary, North Carolina: SAS Institute, Inc; 1995. [Google Scholar]
- 19.Agresti A. Categorical Data Analysis. 2. New York: John Wiley & Sons; 2002. [Google Scholar]
- 20.Hosmer DW, Jr, Lemeshow S. Applied Logistic Regression. 2. New York: John Wiley & Sons; 2000. [Google Scholar]
- 21.SAS Institute I. SAS Help and Documentation. Cary, NC: SAS Institute, Inc; 2009. The PHREG Procedure: MODEL Statement. [Google Scholar]
- 22.Drake JM, Kestle JR, Milner R, et al. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery. 1998 Aug;43(2):294–303. doi: 10.1097/00006123-199808000-00068. discussion 303–295. [DOI] [PubMed] [Google Scholar]
- 23.Cochrane DD, Kestle J. Ventricular shunting for hydrocephalus in children: patients, procedures, surgeons and institutions in English Canada, 1989–2001. Eur J Pediatr Surg. 2002 Dec;12 (Suppl 1):S6–11. doi: 10.1055/s-2002-36864. [DOI] [PubMed] [Google Scholar]
- 24.Di Rocco C, Marchese E, Velardi F. A survey of the first complication of newly implanted CSF shunt devices for the treatment of nontumoral hydrocephalus. Cooperative survey of the 1991–1992 Education Committee of the ISPN. Childs Nerv Syst. 1994 Jul;10(5):321–327. doi: 10.1007/BF00335171. [DOI] [PubMed] [Google Scholar]
- 25.Vinchon M, Dhellemmes P. Cerebrospinal fluid shunt infection: risk factors and long-term follow-up. Childs Nerv Syst. 2006 Jul;22(7):692–697. doi: 10.1007/s00381-005-0037-8. [DOI] [PubMed] [Google Scholar]
- 26.Renier D, Lacombe J, Pierre-Kahn A, Sainte-Rose C, Hirsch JF. Factors causing acute shunt infection. Computer analysis of 1174 operations. J Neurosurg. 1984 Dec;61(6):1072–1078. doi: 10.3171/jns.1984.61.6.1072. [DOI] [PubMed] [Google Scholar]
- 27.Pople IK, Bayston R, Hayward RD. Infection of cerebrospinal fluid shunts in infants: a study of etiological factors. J Neurosurg. 1992 Jul;77(1):29–36. doi: 10.3171/jns.1992.77.1.0029. [DOI] [PubMed] [Google Scholar]
- 28.Dallacasa P, Dappozzo A, Galassi E, Sandri F, Cocchi G, Masi M. Cerebrospinal fluid shunt infections in infants. Childs Nerv Syst. 1995 Nov;11(11):643–648. doi: 10.1007/BF00300722. discussion 649. [DOI] [PubMed] [Google Scholar]
- 29.George R, Leibrock L, Epstein M. Long-term analysis of cerebrospinal fluid shunt infections. A 25-year experience. J Neurosurg. 1979 Dec;51(6):804–811. doi: 10.3171/jns.1979.51.6.0804. [DOI] [PubMed] [Google Scholar]
- 30.Quigley MR, Reigel DH, Kortyna R. Cerebrospinal fluid shunt infections. Report of 41 cases and a critical review of the literature. Pediatr Neurosci. 1989;15(3):111–120. [PubMed] [Google Scholar]
- 31.Davis SE, Levy ML, McComb JG, Masri-Lavine L. Does age or other factors influence the incidence of ventriculoperitoneal shunt infections? Pediatr Neurosurg. 1999 May;30(5):253–257. doi: 10.1159/000028806. [DOI] [PubMed] [Google Scholar]
- 32.Borgbjerg BM, Gjerris F, Albeck MJ, Borgesen SE. Risk of infection after cerebrospinal fluid shunt: an analysis of 884 first-time shunts. Acta Neurochir (Wien) 1995;136(1–2):1–7. doi: 10.1007/BF01411427. [DOI] [PubMed] [Google Scholar]
- 33.Odio C, McCracken GH, Jr, Nelson JD. CSF shunt infections in pediatrics. A seven-year experience. Am J Dis Child. 1984 Dec;138(12):1103–1108. doi: 10.1001/archpedi.1984.02140500009004. [DOI] [PubMed] [Google Scholar]
- 34.Kulkarni AV, Drake JM, Lamberti-Pasculli M. Cerebrospinal fluid shunt infection: a prospective study of risk factors. J Neurosurg. 2001 Feb;94(2):195–201. doi: 10.3171/jns.2001.94.2.0195. [DOI] [PubMed] [Google Scholar]
- 35.Schoenbaum SC, Gardner P, Shillito J. Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis. 1975 May;131(5):543–552. doi: 10.1093/infdis/131.5.543. [DOI] [PubMed] [Google Scholar]
- 36.Kontny U, Hofling B, Gutjahr P, Voth D, Schwarz M, Schmitt HJ. CSF shunt infections in children. Infection. 1993 Mar-Apr;21(2):89–92. doi: 10.1007/BF01710738. [DOI] [PubMed] [Google Scholar]
- 37.Bruinsma N, Stobberingh EE, Herpers MJ, Vles JS, Weber BJ, Gavilanes DA. Subcutaneous ventricular catheter reservoir and ventriculoperitoneal drain-related infections in preterm infants and young children. Clin Microbiol Infect. 2000 Apr;6(4):202–206. doi: 10.1046/j.1469-0691.2000.00052.x. [DOI] [PubMed] [Google Scholar]
- 38.Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992 Jan 30;326(5):281–286. doi: 10.1056/NEJM199201303260501. [DOI] [PubMed] [Google Scholar]
- 39.Shurtleff DB, Stuntz JT, Hayden PW. Experience with 1201 cerebrospinal fluid shunt procedures. Pediatr Neurosci. 1985;12(1):49–57. doi: 10.1159/000120218. [DOI] [PubMed] [Google Scholar]
- 40.Kestle JR, Hoffman HJ, Soloniuk D, Humphreys RP, Drake JM, Hendrick EB. A concerted effort to prevent shunt infection. Childs Nerv Syst. 1993 Jun;9(3):163–165. doi: 10.1007/BF00272269. [DOI] [PubMed] [Google Scholar]
- 41.Horgan MA, Piatt JH., Jr Shaving of the scalp may increase the rate of infection in CSF shunt surgery. Pediatr Neurosurg. 1997 Apr;26(4):180–184. doi: 10.1159/000121187. [DOI] [PubMed] [Google Scholar]
- 42.Winston KR. Hair and neurosurgery. Neurosurgery. 1992 Aug;31(2):320–329. doi: 10.1227/00006123-199208000-00018. [DOI] [PubMed] [Google Scholar]
- 43.Garibaldi RA. Prevention of intraoperative wound contamination with chlorhexidine shower and scrub. J Hosp Infect. 1988 Apr;11 (Suppl B):5–9. doi: 10.1016/0195-6701(88)90149-1. [DOI] [PubMed] [Google Scholar]
- 44.Ragel BT, Browd SR, Schmidt RH. Surgical shunt infection: significant reduction when using intraventricular and systemic antibiotic agents. J Neurosurg. 2006 Aug;105(2):242–247. doi: 10.3171/jns.2006.105.2.242. [DOI] [PubMed] [Google Scholar]
- 45.Lambert M, MacKinnon AE, Vaishnav A. Comparison of two methods of prophylaxis against CSF shunt infection. Z Kinderchir. 1984 Dec;39 (Suppl 2):109–110. doi: 10.1055/s-2008-1044298. [DOI] [PubMed] [Google Scholar]
- 46.Pollack IF, Albright AL, Adelson PD. A randomized, controlled study of a programmable shunt valve versus a conventional valve for patients with hydrocephalus. Hakim-Medos Investigator Group. Neurosurgery. 1999 Dec;45(6):1399–1408. doi: 10.1097/00006123-199912000-00026. discussion 1408–1311. [DOI] [PubMed] [Google Scholar]
- 47.Sciubba DM, Stuart RM, McGirt MJ, et al. Effect of antibiotic-impregnated shunt catheters in decreasing the incidence of shunt infection in the treatment of hydrocephalus. J Neurosurg. 2005 Aug;103(2 Suppl):131–136. doi: 10.3171/ped.2005.103.2.0131. [DOI] [PubMed] [Google Scholar]
- 48.Aryan HE, Meltzer HS, Park MS, Bennett RL, Jandial R, Levy ML. Initial experience with antibiotic-impregnated silicone catheters for shunting of cerebrospinal fluid in children. Childs Nerv Syst. 2005 Jan;21(1):56–61. doi: 10.1007/s00381-004-1052-x. [DOI] [PubMed] [Google Scholar]
- 49.Govender ST, Nathoo N, van Dellen JR. Evaluation of an antibiotic-impregnated shunt system for the treatment of hydrocephalus. J Neurosurg. 2003 Nov;99(5):831–839. doi: 10.3171/jns.2003.99.5.0831. [DOI] [PubMed] [Google Scholar]
- 50.Kan P, Kestle J. Lack of efficacy of antibiotic-impregnated shunt systems in preventing shunt infections in children. Childs Nerv Syst. 2007 Feb 7; doi: 10.1007/s00381-007-0296-7. [DOI] [PubMed] [Google Scholar]
- 51.Griebel R, Khan M, Tan L. CSF shunt complications: an analysis of contributory factors. Childs Nerv Syst. 1985;1(2):77–80. doi: 10.1007/BF00706686. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.