Abstract
INTRODUCTION
Hepatocellular carcinoma (HCC) is a major cause of cancer-related deaths around the world. Nearly half of patients with HCC display metastatic disease at the time of initial diagnosis, frequently involving the liver, bone, brain, lungs, and adrenal glands, but gastrointestinal involvement is rare. Melena occurring secondary to a metastatic tumor from HCC is particularly rare. Herein, we present a case of melena secondary to metastatic HCC after chemoradiation to lung and brain metastases from HCC, diagnosed preoperatively by double-balloon enteroscopy. To the best of our knowledge, this represents the first such case to be reported.
PRESENTATION OF CASE
60-Year-old man had been diagnosed with hepatitis B virus-associated hepatocellular carcinoma (HCC). He was readmitted for investigation of general fatigue and iron-deficiency anemia. Esophagogastroduodenoscopy, total colonoscopy, and CT failed to identify any cause for gastrointestinal bleeding. Double-balloon enteroscopy, however, revealed small bowel metastasis from HCC preoperatively. After 5 days of conservative management, segmental small bowel resection and end-to-end anastomosis were performed. The histological appearances were considered typical for moderately differentiated HCC.
DISSCUSSION
Endoscopic findings of gastrointestinal metastasis from HCC vary, such as raised and centrally ulcerated lesions, polypoid tumors, or submucosal tumors. Immunohistochemical findings are thus key to differentiating HCC from adenocarcinoma in the diagnosis of GIT metastasis. Some patients with gastrointestinal bleeding remain undiagnosed even after upper endoscopy and total colonoscopy, and most such patients will display bleeding sites in the small bowel. Video capsule endoscopy and DBE have been introduced recently for the evaluation of the small bowel. DBE, which was developed by Yamamoto et al.,5 allowed us to obtain biopsy specimens, circumventing one limitation of capsule endoscopy. In this case, DBE contributed significantly to diagnosis and treatment.
CONCLUSION
DBE thus seems to represent a valuable method, particularly in the preoperative setting, due to the possibility of precisely identifying the tumor site and achieving preoperative diagnosis.
Keywords: Hepatocellular carcinoma, Small bowel metastasis, Double-balloon enteroscopy
1. Introduction
Hepatocellular carcinoma (HCC) is a so highly invasive tumor that metastasizes hematogenously and lymphogenously to distant site. Frequent sites are lungs, regional lymphnode, brain, and adrenal glands. But metastasis to the gastrointestinal involvement is rare. Melena occurring secondary to a metastatic tumor from HCC is particularly rare. Small bowel mass lesions are a relatively cause of obscure gastrointestinal bleeding. Their detection has been limited by the inability to endoscopically examine the entire small intestine. This has changed with the introduction of capsule endoscopy and double balloon enteroscopy (DBE) into clinical practice. Herein, we present a case of melena secondary to metastatic HCC after chemoradiation to lung and brain metastases from HCC, diagnosed preoperatively by DBE.
2. Case report
A 60-year-old man had been diagnosed with hepatitis B virus-associated hepatocellular carcinoma (HCC) (T4N M stage IVB) 3 years earlier. Eleven months before presentation, HCC with lung metastasis and brain metastasis was diagnosed on computed tomography (CT) with elevated levels of serum alpha-fetoprotein (1345 ng/ml) and vitamin K antagonist II (329 mAU/ml). Chemoradiation with cisplatin and vinorelbine ditartrate was performed for lung and brain metastases. He had subsequently experienced multiple intrahepatic recurrences and underwent transcatheter arterial chemo-embolization (TACE) and radiofrequency ablation (RFA) on each occasion. Although follow-up was performed with CT and laboratory investigations, he was readmitted for investigation of general fatigue and iron-deficiency anemia. Esophagogastroduodenoscopy, total colonoscopy, and CT failed to identify any cause for gastrointestinal bleeding. DBE, however, revealed protrusions covered with normal mucosa showing central ulceration and mild bleeding (Fig. 1). Examination of biopsy specimens showed these protrusions contained tumor cells, consistent with HCC. Immunohistochemical examination revealed tumor cells positive for polyclonal carcinoembryonic antigen and hepatocyte antigen, and the protrusions were diagnosed as metastatic HCC of the small bowel. After 5 days of conservative management, segmental small bowel resection and end-to-end anastomosis were performed. Macroscopic examination of the surgical specimen showed multiple luminal protruding submucosal masses with extension to the subserosa (Fig. 2). The histological appearances were considered typical for moderately differentiated HCC (Fig. 3). These findings supported HCC metastasis to the small bowel.
Fig. 1.

A protruding lesion measuring 20–30 mm is clearly seen on double-balloon enteroscopy. This protrusion is covered with normal mucosa, with central ulceration and evidence of mild bleeding.
Fig. 2.
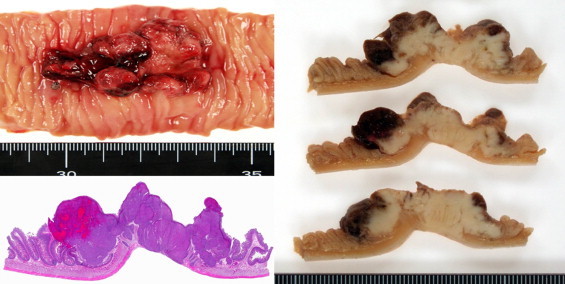
Surgical specimen showed that the mass arising from the submucosa has grown into the lumen and has a dimpling portion and bleeding portion on the top of the tumor.
Fig. 3.
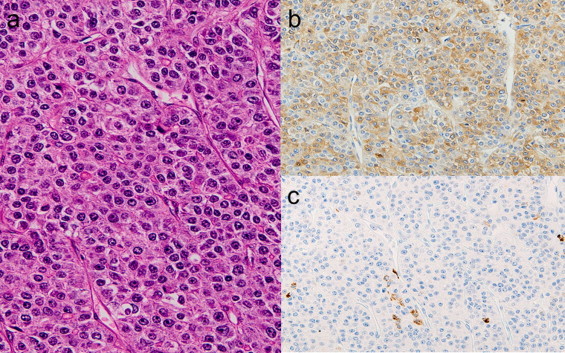
(a) Tumor cells show eosinophilic granular cytoplasm and large nuclei containing prominent nucleoli, resembling HCC (HE, 400×). (b) Tumor cells are positive for alpha-fetoprotein. (c) Positive results for hepatocytes.
3. Discussion
HCC is so highly invasive that extrahepatic metastases are frequently observed.1,2 The most common site of metastasis is the lung, followed by regional lymph nodes, adrenal glands and bone. HCC metastasis to the gastrointestinal tract is rare, found in only 4–12% of cases from an autopsy series.3 These metastatic lesions are usually asymptomatic, and most are discovered on postmortem examination. As the survival period of patients with HCC can be relatively long, some unusual metastatic sites originating from HCC have been identified. However, very few reports have described premorterm diagnosis of gastrointestinal tract involvement by HCC. In particular, small bowel metastasis from HCC diagnosed by DBE has not previously been reported. HCC metastasis is known to occur hematogenously, by lymphatic spread and by local infiltration.4 The presumed mode of metastasis of HCC to the gastrointestinal tract is mostly by direct invasion to the adjacent tract via adhesion to the serosal side of a bulky mass. HCC has a high incidence of venous invasion and thrombosis formation. Hematogenous spread of HCC to the gastrointestinal tract may thus result from tumor thrombi via the portal system, then dissemination by hepatofugal portal spread to the gastrointestinal tract. Endoscopic findings of gastrointestinal metastasis from HCC vary, such as raised and centrally ulcerated lesions, polypoid tumors, or submucosal tumors. Immunohistochemical findings are thus key to differentiating HCC from adenocarcinoma in the diagnosis of GIT metastasis. Some patients with gastrointestinal bleeding remain undiagnosed even after upper endoscopy and total colonoscopy, and most such patients will display bleeding sites in the small bowel. Video capsule endoscopy and DBE have been introduced recently for the evaluation of the small bowel. DBE, which was developed by Yamamoto et al.,5 allowed us to obtain biopsy specimens, circumventing one limitation of capsule endoscopy. In this case, DBE contributed significantly to diagnosis and treatment. Nonetheless, we can conclude that gastrointestinal tract metastases should be considered in patients with HCC presenting with abdominal symptoms, and aggressive abdominal surgery for these patients is worthwhile in a selected group of patients despite the poor prognosis of GIT metastasis from HCC, as this intervention provides the potential for good palliation and reasonable survival.
The surgical procedure should be tailored according to the extent of disease and should provide adequate palliation of the presenting symptoms. DBE thus seems to represent a valuable method, particularly in the preoperative setting, due to the possibility of precisely identifying the tumor site and achieving preoperative diagnosis.
4. Conclusion
We reported an extremely rare case of metastatic HCC to small intestine, which diagnosed preoperatively by DBE. Up to our knowledge, this is the first such case to be reported
Conflict of interest statement
No conflict of interest.
Funding
No sources of funding.
Ethical approval
Written informed consent was obtained from the patient for the information to be included in our manuscript. His information has been de-identified to the best of our ability to protect his privacy.
Author contributions
Each author participated in writing the manuscript and all agreed to accept equal responsibility for the accuracy of the content of the paper.
References
- 1.Kay C.J. Primary hepatic cancer: review of 96 case. Arch Intern Med. 1964;113:120–131. doi: 10.1001/archinte.1964.00280070048010. [DOI] [PubMed] [Google Scholar]
- 2.Yeo W., Sung J.Y., Ward S.C., Chung S.C., Lee W.Y., Li A.K. A prospective study of upper gastrointestinal hemorrhage in patients with hepatocellular carcinoma. Dig Dis Sci. 1995;40:2516–2521. doi: 10.1007/BF02220435. [DOI] [PubMed] [Google Scholar]
- 3.Nakashima T., Okuda K., Kojiro M., Jimi A., Yamaguchi R., Sakamoto K. Pathology of hepatocellular carcinoma in Japan. 232 consecutive cases autopsied in ten years. Cancer. 1983;51:863–877. doi: 10.1002/1097-0142(19830301)51:5<863::aid-cncr2820510520>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 4.Chen L.T., Chen C.Y., Jan C.M., Wang W.M., Lan T.S., Hsieh M.Y. Gastrointestinal tract involvement in hepatocellular carcinoma: clinical, radiological and endoscopic studies. Endoscopy. 1990;22:118–123. doi: 10.1055/s-2007-1012815. [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto H., Sekine Y., Sato Y., Higashizawa T., Miyata T., Iino S. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216–220. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]


