Abstract
INTRODUCTION
Invasion of the portal and hepatic veins by hepatocellular carcinoma (HCC) is common, but macroscopic bile duct invasion is rare. Once a tumor thrombus completely obstructs the main bile duct, it causes obstructive jaundice. This type of HCC, known as icteric-type HCC (IHCC), has a poor prognosis.
PRESENTATION OF CASE
A 72-year-old woman had been treated for chronic hepatitis C since 1997. In 2002, percutaneous ethanol injection therapy was performed for HCC in segment 8. HCC recurrence occurred in 2004, and she underwent transarterial embolization (TAE) and radiofrequency ablation (RFA). In 2006, an S8 segmentectomy was performed for re-recurrence of HCC. Three years after surgery, computed tomography (CT) revealed a tumor occupying the right anterior intrahepatic bile duct and extending into its right main branch. With a preoperative diagnosis of HCC recurrence in the bile duct, we performed a right hepatectomy and thrombectomy. Histological examination showed moderately to poorly differentiated HCC. No tumor tissue other than the intrahepatic bile duct tumor was detected in the resected liver specimen.
DISCUSSION
HCC with biliary tumor thrombus is associated with a poor prognosis. In general, IHCC is difficult to diagnose and treat in the early stages. A characteristic radiological finding for this type of IHCC is the hypervascularity of the tumor thrombus.
CONCLUSION
To the best of our knowledge, this is a rare case of IHCC recurrence as a tumor thrombus without recurrence in the resected liver specimen.
Keywords: Hepatocellular carcinoma (HCC), Intraductal tumor, Tumor thrombus
1. Introduction
Hepatocellular carcinoma (HCC) is known to invade the portal and hepatic veins, but intrabiliary invasion is rare. Lin et al. referred to this type of HCC as “icteric-type HCC” (IHCC).1 The initial symptom of IHCC is obstructive jaundice due to compression or occlusion of the bile duct by the tumor. HCC with bile duct invasion has been reported in another study, enabling identification of the characteristics of this particular disease.2
Tumor thrombus in the bile duct is one of the main reasons for obstructive jaundice, and its incidence varies from 0.53% to 9%.3,4 Several studies have reported HCC with no obvious intrahepatic tumor but with a tumor thrombus in the bile duct.3,5 This special type of HCC is difficult to identify preoperatively because the characteristic radiological findings are not well known. The prognosis of HCC with a tumor thrombus is dismal, but it is better than that of jaundice caused by hepatic insufficiency. Identification at an early stage is important in a clinical setting. Here, we report a case of HCC with a tumor thrombus and provide imaging findings to facilitate preoperative diagnosis.
2. Presentation of case
A 72-year-old woman was admitted to our hospital in April 2009. She had been treated for hepatitis C virus infection. In 2002, percutaneous ethanol injection therapy was performed for primary HCC in segment 8. In 2003, she underwent transarterial embolization (TAE) for HCC recurrence. Radiofrequency ablation (RFA) was performed for HCC recurrence 1 year after TAE. Pathological findings indicated that the surgical margin was preserved. The woman refused to undergo surgery, although she knew that surgical resection was the best treatment for HCC. She subsequently underwent an S8 segmentectomy for HCC recurrence. Histopathological examination showed moderate-to-poorly differentiated HCC. In addition, no invasion into the portal vein or bile duct was observed. Thereafter, she had no sign of recurrence for 3 years. On admission to hospital in 2009, a mass was detected in the right lobe of her liver by routine US. Tumor markers were within the normal range: carcinoembryonic antigen, 2.9 ng/ml (≤5.0 ng/ml); carbohydrate antigen 19-9, 91 U/ml (<37 U/ml); α-fetoprotein, 2.9 ng/ml (≤10.0 ng/ml); and protein induced by vitamin K absence or antagonist-II (PIVKA-II), 13 mAU/ml (≤40.0 mAU/ml). Computed tomography (CT) revealed a tumor in the right anterior intrahepatic bile duct; this tumor extended into the right main branch. However, no significant lesions were observed in the liver (Fig. 1a). CT hepatic arteriography and arterial portography demonstrated that the tumor was enhanced in the early phase and washed out in the late phase (Fig. 1b and c); this is a typical radiological finding in HCC cases. Magnetic resonance imaging with the hepatocyte-specific contrast agent gadolinium ethoxybenzyl diethylenetriaminepentaacetic acid showed that the tumor was of low intensity in the hepatobiliary phase (Fig. 2). With a preoperative differential diagnosis of recurrent HCC invading the bile duct or intraductal cholangiocellular carcinoma, we performed a right hepatectomy and thrombectomy. Intraoperative US showed that the tumor thrombus reached the top of the common bile duct. We first performed hepatectomy and then made an incision anterior to the common bile duct. The tumor thrombus was easily removed without bleeding (Fig. 3a). Residual tumor tissue was not detected in the common bile duct or the left bile duct on cholangioscopy. The tumor thrombus was 30 mm × 40 mm in size, without bleeding, and was not adhered to the bile duct (Fig. 3b). On histological examination, the tumor thrombus showed poorly differentiated HCC (Fig. 4). No obvious intrahepatic mass was detected in the resected liver specimen. The patient was discharged without any major complications 26 days after surgery because some time was required to identify a suitable hospital for her rehabilitation. The patient remained disease free after 1 year of follow-up.
Fig. 1.
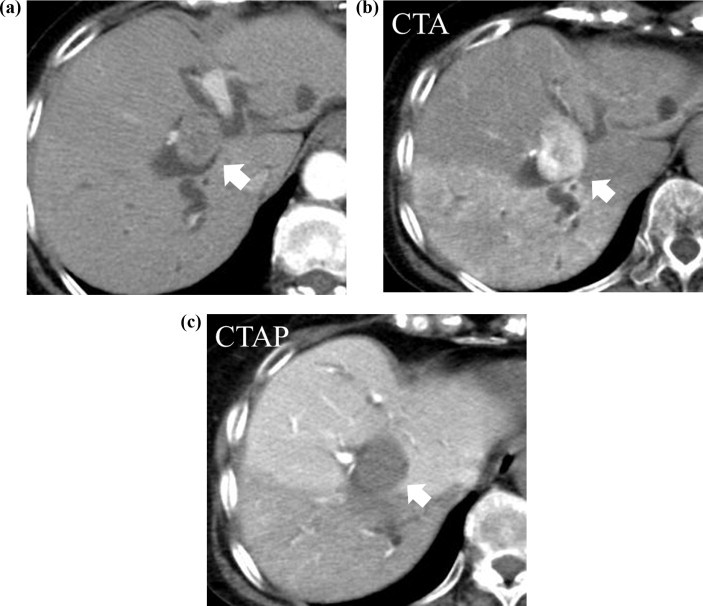
(a) CT showing a well-enhanced tumor with a clear margin in the right bile duct (arrow) accompanied by peripheral bile duct dilation. (b) The tumor was well enhanced in the early phase (arrow). (c) The tumor stain was washed out in the portal phase (arrow).
Fig. 2.
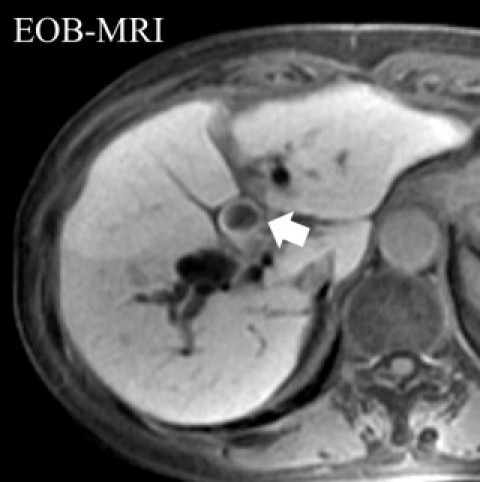
Magnetic resonance imaging with gadolinium ethoxybenzyl diethylenetriaminepentaacetic acid (Gd-EOB-MRI) revealed that the tumor in the intrahepatic bile duct had a low intensity in the hepatobiliary phase (arrow).
Fig. 3.
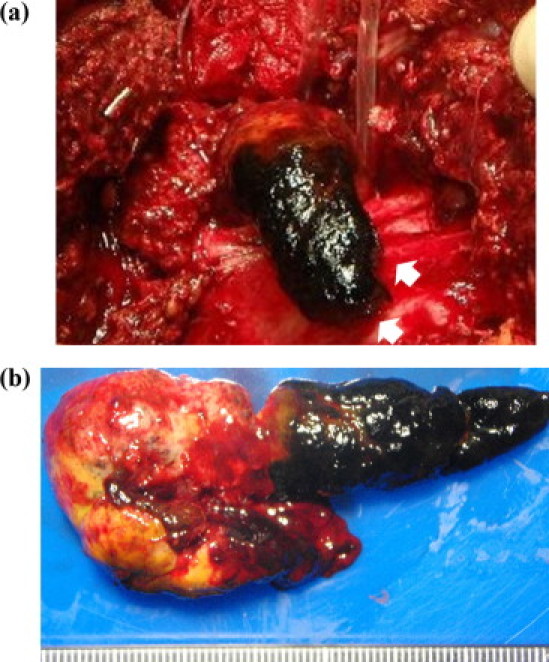
(a) The tumor thrombus was easily removed without bleeding. (b) The tumor thrombus was 30 mm × 40 mm in size and was not adhered to the bile duct.
Fig. 4.

Histopathological examination showed poorly differentiated hepatocellular carcinoma (HCC) (hematoxylin and eosin staining, 200×).
3. Discussion
There are 2 theories for the origin of a tumor thrombus in the bile duct. (1) It originates in the ectopic liver tissue of the bile duct.6 An ectopic liver, which is an accessory lobe, is often incidentally found near the gallbladder, hepatic ligaments, omentum, retroperitoneum, and thorax.7,8 (2) In most cases, the tumor thrombus in the bile duct is derived from a HCC lesion in the liver. Once the thrombus completely obstructs the main bile duct, it causes obstructive jaundice. Lin et al. referred to this type of HCC as IHCC.1 HCC invades biliary systems through 1 of the following 3 mechanisms: (1) the tumor may grow continuously in a distal fashion, filling the entire extrahepatic biliary system with a solid cast of tumor; (2) a fragment of necrotic tumor may separate from the proximal intraductal growth, migrating to the distal common bile duct and causing obstruction; or (3) hemorrhage from the tumor may partially or completely fill the biliary tree with blood clots.9 In our patient, no tumor tissues were identified in the resected liver on histological examination despite careful sectioning and examination. The tumor thrombus showed poorly differentiated HCC. Cellular differentiation in sections of the thrombus was similar to that in the HCC that had been surgically removed 3 years previously. Therefore, the HCC in this patient was believed to be formed by slow growth of a residual tumor fragment in the bile duct.
Regardless of remarkable advances in imaging modalities, it remains difficult to obtain a preoperative diagnosis for IHCC. US and CT often misdiagnose these lesions as a “bile duct stone” or as cholangiocarcinoma. Magnetic resonance cholangiography (MRCP) is a noninvasive modality that has been shown to be superior to endoscopic retrograde cholangiopancreatography (ERCP) in detecting the presence of biliary obstruction. Dilation of the biliary system and a primary liver tumor can be observed on MRCP. Tamada et al. reported that intraductal US (IDUS) can be used to distinguish between tumor thrombi caused by HCC and the polypoid type of cholangiocarcinoma.10 However, ERCP and IDUS are more invasive and require more specialized equipment than does MRCP. The characteristic finding of tumor thrombi is an early enhancement pattern on dual-phase contrast-enhanced CT; this is important in differentiating cholangiocarcinoma.
The ideal treatment for a patient with obstructive jaundice secondary to HCC is complete extirpation of the tumor by hepatic resection. If tumor involvement is observed in the extrahepatic ducts, the ducts can be resected en bloc along with the liver tumor. If the ducts show tumor involvement, as with free floating-tumor fragments that cause biliary obstruction, the tumor fragments can be removed. This can then be followed by liver resection without biliary-enteric anastomosis.11 In most cases, a tumor growing within the bile duct does not adhere tightly to the duct wall; it usually adheres to the mucosa of the duct, but not the submucosal layer. Such a tumor thrombus can be easily removed from the bile duct during surgery. This is important from a surgical viewpoint because even if the tumor thrombus in the bile duct protrudes into the contralateral side of the tumor-bearing lobe, it can usually be removed from the bile duct.12,13 Some authors have concluded that tumor thrombectomy through a choledochotomy is contraindicated for the treatment of a tumor thrombus because it might cause peritoneal dissemination.14,15 However, most surgeons believe that the best treatment for tumor thrombus is liver resection and thrombectomy, which result in a much better survival rate compared with that after no resection.3,5 Therefore, to improve survival, if the patient's general condition and liver function are suitable, it is suggested that major liver resection with thrombectomy should be performed.
Ueda et al. reported a successful case in which the patient presented with a tumor thrombus 57 months after hepatectomy and thrombectomy.2 These patients underwent a thrombectomy but not reconstruction of the biliary tract. The blood supply to the thrombus should be noted, and care should be taken to avoid massive bleeding during thrombectomy.2,16 Active hemorrhage during thrombectomy can be controlled by suturing, electrocauterization, compression, Pringle's maneuver, and hepatic arterial ligation are a few alternative means of achieving hemostasis.3
The prognosis is poorer in such cases than in other types of HCC.12 Most patients already have advanced-stage HCC at the time of diagnosis, and curative resection is impossible. However, hepatic resection is the only treatment that can prolong survival. Tumors in such cases must be detected at an early stage, even in asymptomatic carriers of viral hepatitis, by abdominal US. Tumor markers such as AFP and PIVKA-II should also be assessed.17
4. Conclusion
We presented a case of intrahepatic bile duct recurrence of HCC without a detectable tumor in the liver. Such cases have been reported to have a poor prognosis in general, and surgical intervention is recommended for cases similar to ours.18 However, if the tumor is small and can be completely removed, the prognosis may improve. Differentiation from cholangiocellular carcinoma is relatively difficult, especially in cases of HCC. From a histological viewpoint, liver resection should be performed if the patient's liver function is suitable. Although this procedure is rarely performed, it must be kept in mind. Patients with suspected HCC should be investigated thoroughly because they require aggressive treatment at an earlier stage.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
T.A., K.S., K.K. and G.T. evaluated the patient and wrote the manuscript. T.A., K.K., K.S. and N.H. performed surgery. T.N. was the leader of the treatment.
References
- 1.Lin T.Y., Chen K.M., Chen Y.R., Lin W.S., Wang T.H. Icteric type of hepatoma. Med Chir Dig. 1975;4:267–270. [PubMed] [Google Scholar]
- 2.Ueda M., Takeuchi T., Takayasu T., Takahashi K., Okamoto S., Tanaka A. Classification and surgical treatment of hepatocellular carcinoma (HCC) with bile duct thrombi. Hepatogastroenterology. 1994;41:349–354. [PubMed] [Google Scholar]
- 3.Qin L.X., Ma Z.C., Wu Z.Q., Fan J., Zhou X.D., Sun H.C. Diagnosis and surgical treatments of hepatocellular carcinoma with tumor thrombosis in bile duct: experience of 34 patients. World J Gastroenterol. 2004;10:1397–1401. doi: 10.3748/wjg.v10.i10.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang J.F., Wang L.Y., Lin Z.Y., Chen S.C., Hsieh M.Y., Chuang W.L. Incidence and clinical outcome of icteric type hepatocellular carcinoma. J Gastroenterol Hepatol. 2002;17:190–195. doi: 10.1046/j.1440-1746.2002.02677.x. [DOI] [PubMed] [Google Scholar]
- 5.Long X.Y., Li Y.X., Wu W., Li L., Cao J. Diagnosis of bile duct hepatocellular carcinoma thrombus without obvious intrahepatic mass. World J Gastroenterol. 2010;16:4998–5004. doi: 10.3748/wjg.v16.i39.4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arakawa M., Kimura Y., Sakata K., Kubo Y., Fukushima T., Okuda K. Propensity of ectopic liver to hepatocarcinogenesis: case reports and review of the literature. Hepatology. 1999;29:57–61. doi: 10.1002/hep.510290144. [DOI] [PubMed] [Google Scholar]
- 7.Watanabe M., Matsuura T., Takatori K., Ueki K., Kobatake T., Hidaka M. Five cases of ectopic liver and a case of accessory lobe of the liver. Endoscopy. 1989;21:39–42. doi: 10.1055/s-2007-1012892. [DOI] [PubMed] [Google Scholar]
- 8.Asada J., Onji S., Yamashita Y., Okada S., Morino M. Ectopic liver observed by peritoneoscopy: report of a case. Gastroenterol Endosc. 1982;24:309–312. [Google Scholar]
- 9.Chen M.F., Jan Y.Y., Jeng L.B., Hwang T.L., Wang C.S., Chen S.C. Obstructive jaundice secondary to ruptured hepatocellular carcinoma into the common bile duct. Surgical experiences of 20 cases. Cancer. 1994;73:1335–1340. doi: 10.1002/1097-0142(19940301)73:5<1335::aid-cncr2820730505>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 10.Tamada K., Isoda N., Wada S., Tomiyama T., Ohashi A., Satoh Y. Intraductal ultrasonography for hepatocellular carcinoma with tumor thrombi in the bile duct: comparison with polypoid cholangiocarcinoma. J Gastroenterol Hepatol. 2001;16:801–805. doi: 10.1046/j.1440-1746.2001.02527.x. [DOI] [PubMed] [Google Scholar]
- 11.Lau W.Y., Leung K.L., Leung T.W.T., Liew C.T., Chan M.S.Y., Yu S.C.H. A logical approach to hepatocellular carcinoma presenting with jaundice. Ann Surg. 1997;225:1281–1285. doi: 10.1097/00000658-199703000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tada K., Kubota K., Sano K., Noie T., Kosuge T., Takayama T. Surgery of icteric-type hepatoma after biliary drainage and transcatheter arterial embolization. Hepatogastroenterology. 1999;46:843–848. [PubMed] [Google Scholar]
- 13.Kojiro M., Kawabata K., Kawano Y., Shirai F., Takemoto N., Nakashima T. Hepatocellular carcinoma presenting as intrabile duct tumor growth. A clinicopathological study of 24 cases. Cancer. 1982;49:2144–2147. doi: 10.1002/1097-0142(19820515)49:10<2144::aid-cncr2820491026>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 14.Mok K.T., Chang H.T., Liu S.I., Jou N.W., Tsai C.C., Wang B.W. Surgical treatment of hepatocellular carcinoma with biliary tumor thrombi. Int Surg. 1996;81:284–288. [PubMed] [Google Scholar]
- 15.Wang H.J., Kim J.H., Kim J.H., Kim W.H., Kim M.W. Hepatocellular carcinoma with tumor thrombus in the bile duct. Hepatogastroenterology. 1999;46:2495–2499. [PubMed] [Google Scholar]
- 16.Kiso S., Kashihara T., Ohki A., Fujimori E., Kawakami F., Tako H. A case report: transcatheter arterial embolization was effective for hepatocellular carcinoma with bile duct invasion. Jpn J Gastroenterol. 1990;87:1248. [PubMed] [Google Scholar]
- 17.Shimada M., Takenaka K., Hasegawa H., Shirabe K., Gion T., Kano T. Hepatic resection for icteric type hepatocellular carcinoma. Hepatogastroenterology. 1997;44:1432–1437. [PubMed] [Google Scholar]
- 18.Makino T., Nakamori S., Kashiwazaki M., Masuda N., Ikenaga M. An icteric type hepatocellular carcinoma with no detectable tumor in the liver: report of a case. Surg Today. 2006;36:633–637. doi: 10.1007/s00595-006-3214-9. [DOI] [PubMed] [Google Scholar]


