Abstract
Morio Kasai is one of the most influential Japanese pediatric surgeons. He is best recognized in the United States for his pioneering efforts in the field of biliary atresia. His work revolutionized the treatment of infants born with biliary atresia throughout the world. Less is known about his remarkable impact in the fields of general surgery and pediatric surgery. This review highlights some of Dr. Kasai’s major contributions and highlights the influence he had in the establishment of pediatric surgery as field.
Keywords: Kasai procedure, biliary atresia
INTRODUCTION
Surgical leaders in the US are generally well known and their stories are often told to generations of young surgeons during training. The recent history of surgical progress and development outside the US is not as well publicized. Morio Kasai (1922–2008) is considered one of the greatest innovators in the field of pediatric surgery (Fig 1) [1]. He was a very modest Japanese man about whom little is known in the Western Hemisphere beyond the operation that bears his name. In Japan, he is considered one of the early surgeon-scientists who was also appreciated by many as an exemplary teacher and role model. During the 1950s, as Japan was rebuilding after the destruction it sustained in World War II, Dr. Kasai emerged as an early proponent of clinical research in surgery, and especially in pediatric surgery. Much as Drs. Gross [2] and Ladd [3] did in the United States, he was instrumental in establishing pediatric surgery as a distinct surgical specialty in Japan. His revolutionary and extensive work in the area of biliary atresia has proven to be one of the most significant advances in pediatric surgery in the last century. He is best known for the development of the procedure that bears his name, the hepatic-portoenterostomy or the Kasai procedure for treatment of biliary atresia in infancy. A monumental accomplishment in its own right, it remains only a partial element of his complete legacy. Throughout his life, Dr. Kasai remained actively involved in the world of pediatric surgery, which he helped to develop until he died on September 29, 2008 at the age of 86. The goal of this review, which has not been easy because of his modesty, is to detail Morio Kasai’s varied contributions to the development of the field of pediatric surgery.
Figure 1.
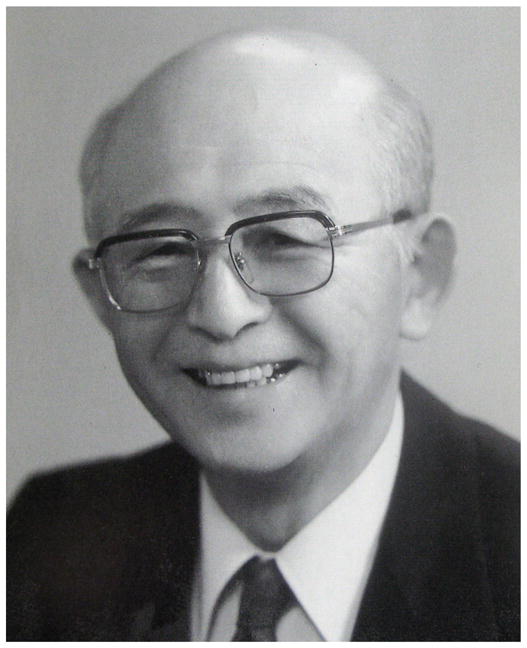
Portrait of Morio Kasai, MD
EDUCATION, PROFESSIONAL, AND PERSONAL LIFE
Dr. Kasai was born in 1922, in Aomori Prefecture, the northernmost prefecture of the mainland of Japan, far from Tokyo, the longstanding center of medical and political life in Japan. He began his medical studies in Sendai at the end of World War II, during a time of economic hardship and social changes in Japan. He graduated from the National Tohoku University School of Medicine in 1947 and remained at Tohoku University for his surgical training and then joined what was known as the 2nd Department of Surgery at that institution. He began his career as a general surgeon, at a time before pediatric surgery had been recognized as a separate specialty in Japan. At Tohoku University School of Medicine, Dr. Kasai and his colleagues were involved in diverse research efforts in the fields of surgical oncology, esophageal surgery, and pediatric surgery. He was a strong proponent of the surgeon-scientist model, which just began to be encouraged in the US and in some surgical training programs in parts of Western Europe. His early work focused on water and electrolyte metabolism in surgical patients with particular attention to post-operative fluid therapy in children [4]. During this time, similar research was ongoing at the Peter Bent Brigham Hospital in Boston under the direction of Dr. Francis D. Moore. This work led to the first major book on fluid management in postsurgical patients, “The Metabolic Care of the Surgical Patient,” published by the Boston group in 1959 [5].
In 1959, Dr. Kasai completed a 1-year research fellowship with Charles Everett Koop, MD, the surgeon-in-chief at the Children’s Hospital of Philadelphia (CHOP). His experience in Philadelphia led to this young surgeon’s lifelong dedication to the surgery of children. Upon his return from Philadelphia, Dr. Kasai was promoted to Associate Professor of Surgery at Tohoku University and in 1963, at the age of 41, he became Professor and Chief of the 2nd Department of Surgery and continued in this role until he was forced to retire from the University by academic regulations at the age of 63, as are most professors at academic centers in Japan. As chairman, Dr. Kasai led his department in many innovations, which are listed briefly later in this brief biography, including especially development of the field of pediatric surgery. During his tenure, he trained four pediatric surgeons who carried his ideas and methods to all corners of Japan by disseminating his expertise in the surgical care of infants and children. He also helped Dr. Koop establish a biliary atresia program at CHOP in the 1970’s. Upon his retirement in 1986, Dr. Kasai became the Emeritus Professor at National Tohoku University and soon after that, the director of NTT Tohoku Hospital where he worked until his retirement in 1993. He continued to influence surgery, and especially pediatric surgery until his death, even after being hampered by a stroke in 1999.
Dr. Kasai was also well recognized by his contemporaries for his activities outside the biomedical world. He was known for being an avid skier and a mountain climber. In 1986, he headed the Tohoku University mountain-climbing team, which was the first in the world to successfully climb the Nyainquntanglha Mountains, the highest mountains in Tibet. He was well known by his colleagues as highly sociable, particularly when sharing sake among friends [1,6].
THE KASAI PROCEDURE
Dr. Kasai’s reputation in the western hemisphere has been based primarily on his many contributions to the knowledge and therapeutic advancements in the area of biliary atresia, improving the care and outcomes for children afflicted with this rare disorder. Biliary atresia is a serious condition affecting infants with an incidence of 1 in 15,000 live births and is the most common surgical cause of neonatal jaundice [7]. It is characterized by an obliterative cholangiopathy that affects all or part of the extrahepatic biliary tree. In the 1950s, the condition was considered fatal in practically all cases. Dr. Kasai’s efforts to understand the pathologic processes that lead to biliary atresia, cholestasis, and eventual cirrhosis, paved the way for the surgical intervention that he developed. He is appropriately credited for his original contributions to the development of the hepatic portoenterostomy technique, aptly known as the Kasai Procedure. In 1955, he performed the first Kasai procedure in a 72-day-old infant, who was diagnosed with biliary atresia. During the procedure, Dr. Kasai noted no evidence of extrahepatic bile ducts and after further dissection encountered significant bleeding. In an attempt to achieve hemostasis, he is purported to have placed the duodenum over the porta hepatis in the incised region where the bleeding appeared to originate. All were astonished at the appearance of bile pigment in the feces postoperatively and with the eventual complete resolution of jaundice [8]. Dr. Kasai’s original procedure was first published in Japanese in the journal named Shujutsu in 1959 [9].
This major surgical innovation failed to receive international recognition until the 1960s when it was first translated and published in English-language journals. Early attempts at replicating the Kasai procedure in the U.S. were largely unsuccessful. Many American surgeons, including Dr. John R Lilly, traveled to Japan in order to perfect the technique by watching Dr. Kasai. By the mid 1970’s, however, many centers around the U.S. were beginning to report successful outcomes after the Kasai procedure, more than a decade after its introduction in Japan [10].
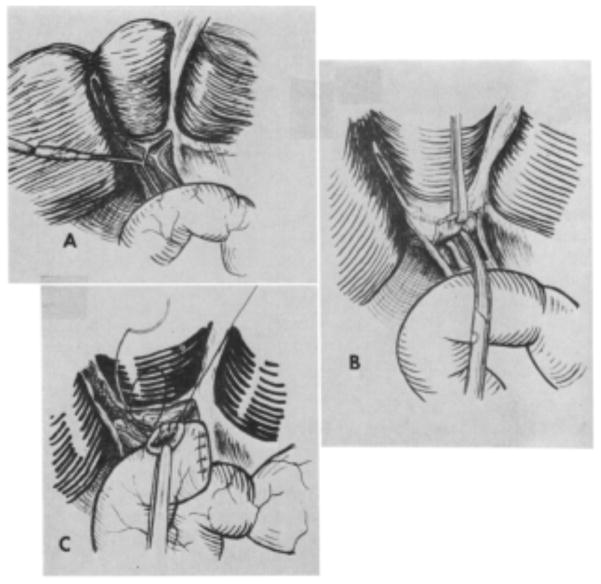
The Kasai procedure is designed to alleviate biliary obstruction and jaundice in infants with biliary atresia. The obliterated bile ducts are resected and a Roux-en-Y jejunal limb is anastomosed to the portal plate to allow drainage of bile via the microscopic ducts within the porta hepatis (Fig 2). Two thirds of infants will clear their jaundice after a portoenterostomy procedure. Even after a well-executed Kasai procedure, however, about one third of children will ultimately require liver transplantation due to progressive cholestasis and cirrhosis [7]. Dr. Kasai also published extensively on the long-term complications following attempted correction of biliary atresia, including portal hypertension. Through his experience, he noted that portal hypertension could be minimized by early corrective repair and prevention of postoperative cholangitis [11,12]. Failure of the Kasai procedure to restore biliary drainage leaves liver transplantation as the only path to survival in these children. Dr. Kasai was very humble and did not wish to have this surgical procedure bear his name but despite this it has remained best known as “the Kasai” in recognition of its originator. Further work by Kasai was aimed at establishing postsurgical clinical management protocols for children undergoing the hepatic portoenterostomy procedure, many of which continue to be used throughout the world today. The oldest living survivor from the Kasai procedure is in his 50’s and currently living in Japan.
Figure 2.
Taken from Kasai et al., Surgical Treatment of Biliary Atresia. JPS 1968; 3: 668. Early description of the steps in a hepatic portoenterostomy.
OTHER SURGICAL CONTRIBUTIONS
Early in his career, Dr. Kasai became interested in pediatric oncology and his studies of the histopathology and surgical treatment of pediatric liver tumors proved to be seminal in that field when originally presented [13]. He and his collegues are credited with devising one of the first pathologic classification systems for hepatoblastoma, the most common primary liver tumor in childhood [14].
Dr. Kasai also investigated methods to improve the established management of children with Hirschsprung’s disease. In 1948, Swenson reported the use of a pull-through rectosigmoidectomy for children with Hirschsprung’s disease [15]. Since Dr. Kasai felt that this procedure was not feasible for small infants due to technical difficulties and since while awaiting this procedure many succumbed to enterocolitis despite the use of a temporary colostomy. Dr. Kasai therefore conceived of a novel procedure, a rectal myotomy with colectomy, for infants with Hirschsprung’s disease to specifically address what he described as the “anorectal achalasia” [16]. This procedure minimized pelvic dissection and preserved rectal sensation. Dr. Kasai went on to refine this procedure by performing a rectoplasty with posterior triangular colonic flap to eliminate the weak point in the myotomized portion of the rectum (Fig 3)[17].
Figure 3.
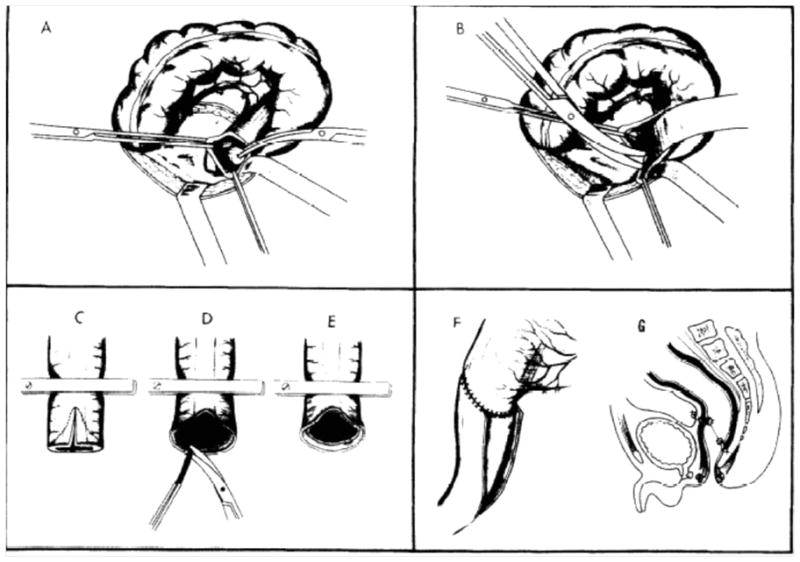
Taken from Kasai et al., Rectal myotomy with colectomy: A radical operation for Hirschsprung’s disease. JPS 1971, 6; 37.
Dr. Kasai also challenged the established paradigm that surgery for esophageal cancer was palliative. He described a large series of patients treated with primary excision of the esophagus with a jejunal interposition with remarkable 5-year outcomes [18]. In addition to these remarkable technical innovative contributions and not frequently recognized, Dr. Kasai’s original work as a resident and as a young attending focused on understanding and improving the treatment of peritonitis in neonates and children. These diverse interests within surgery resulted in 632 publications including chapters in textbooks and original papers published in distinguished scientific journals.
A LEGACY OF DISNTINCTION
Late in his career, Dr. Kasai focused on the importance of clinical research and on unifying the research studies in the field of pediatric surgery throughout Japan and eventually throughout the world. To this end, Dr. Kasai founded several scientific associations, many of which continue to advance his vision of pediatric surgery as a central and distinct division within general surgery. He was the founder or helped to create the Japanese Society of Pediatric Surgeons, the Japanese Society for Surgical Metabolism and Nutrition, Japanese Society of Pediatric Oncology, and the Pacific Association of Pediatric Surgeons. One of his lasting contributions was the creation, in 1976, of the Japanese Society of Biliary Atresia Study Group. This organization continues to conduct annual meetings and operates a registry on biliary atresia at a national level in Japan. Along with this effort, Dr. Kasai also founded the International Symposium of Biliary Atresia in 1976, which meets every five years to discuss advances in management of biliary atresia on a global level. His grand vision helped shape Japan as one of the leaders in pediatric oncology, while his interest in teaching, mentoring, guiding, and organizing both young and older surgeons left a remarkable tradition of respect, admiration, and affection in those who knew him or worked with him [1,6].
Dr. Kasai went on to receive numerous awards for his work in pediatric hepatobiliary surgery. In Japan, he received the Asahi prize in 1992, the Ministry of Education Award in 1995, and The Order of Sacred Treasure, Gold and Silver Star in 1997. Internationally, he was honored with the distinguished Denis Brown Gold Medal from the British Association of Pediatric Surgeons in 1986, the Herbert Coe Medal from the Pacific Association of Pediatric Surgeons in 1987, and the prestigious William E. Ladd Medal from the American Academy of Pediatrics in 1991. He also received the Surgeon General’s Medallion from the U.S. Public Health Service in 1989 awarded to him by one of his American mentors, Dr. C. Everett Koop, the Surgeon General at that time. Among many of his other honors Dr. Kasai was elected as an honorary member of the American Surgical Association, distinguishing himself as 1 of only 7 surgeons from Japan to have been so honored [1,6].
CONCLUSION
Dr. Kasai is well recognized as one of the most influential Japanese surgeons by his contributions to pediatric and general surgery and to the field of surgical education and research. His influence on surgical practice, particularly in pediatric surgery, continues to be felt today across the globe through his pioneering contributions to treatment of children afflicted with biliary atresia. The Kasai procedure remains the gold standard in the initial surgical management for infants with biliary atresia, more than half a century after its original description. His contributions to liver tumors and to fluid and electrolyte balance in pediatrics, although less recognized, are no less significant. Dr. Kasai’s impressive list of contributions and his influence over at least two generations of surgeons worldwide constitute a remarkable legacy. His creativity and rigor have left a lasting impact on future generations of pediatric surgeons.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ohi R. Obituary: Morio Kasai, MD, 1922–2008. J Pediatr Surg. 2009;44:481–482. [Google Scholar]
- 2.Fisher JC, Hardy MA, Widmann WD. Robert E. Gross: The Heart of a Surgeon Current Surgery. 2005;62(5):495–499. doi: 10.1016/j.cursur.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Xydas S, Widmann WD, Hardy MA, William E. Ladd: Father of Pediatric Surgery. Curr Surg. 2003:47–50. doi: 10.1016/S0149-7944(02)00727-4. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki H, Kimura S, Ohashi E, et al. Water and electrolyte metabolism of newborn infants after surgical operations. Tohoku J Exp Med. 1968;94:187–202. doi: 10.1620/tjem.94.187. [DOI] [PubMed] [Google Scholar]
- 5.Moore F. Metabolic Care of the Surgical Patient. Philadelphia, PA: W. B. Saunders; 1959. [Google Scholar]
- 6.Miyano T. Morio Kasai, MD, 1922–2008. Pediatr Surg Int. 2009;25:307–308. [Google Scholar]
- 7.Khalil BA, Perera MT, Mirza DF. Clinical practice: Management of biliary atresia. Eur J Pediatr. 2010;169:395–402. doi: 10.1007/s00431-009-1125-7. [DOI] [PubMed] [Google Scholar]
- 8.Ohi R. A History of the Kasai Operation: Hepatic Portoenterostomy for Biliary Atresia. World J Surg. 1988;12:871–874. doi: 10.1007/BF01655504. [DOI] [PubMed] [Google Scholar]
- 9.Kasai M, Suzuki M. A new operation for non-correctable biliary atresia: hepatic portoenterostomy. Shujutsu. 1959;13:733–739. [Google Scholar]
- 10.Altman RP. The portoenterostomy procedure for biliary atresia: A five-year experience. Ann Surg. 1978;188:351–361. doi: 10.1097/00000658-197809000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kasai M, Okamoto A, Ohi R, et al. Changes of portal vein pressure and intrahepatic blood vessels after surgery for biliary atresia. J Pediatr Surg. 1981;16:152–159. doi: 10.1016/s0022-3468(81)80342-9. [DOI] [PubMed] [Google Scholar]
- 12.Ohi R, Mochizuki I, Komatsu K, et al. Portal hypertension after successful hepatic portoenterostomy in biliary atresia. J Pediatr Surg. 1986;21:271–274. doi: 10.1016/s0022-3468(86)80852-1. [DOI] [PubMed] [Google Scholar]
- 13.Kasai M, Kimura S, Sasaki M, et al. Successful total right hepatic lobectomy for primary hepatoma in an infant. Surgery. 1963;54:351–355. [PubMed] [Google Scholar]
- 14.Kasai M, Watanabe I. Histologic classification of liver-cell carcinoma in infancy and childhood and its clinical evaluation. A study of 70 cases collected in Japan. Cancer. 1970;25:551–563. doi: 10.1002/1097-0142(197003)25:3<551::aid-cncr2820250309>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 15.Swenson O, Bill AH. Resection of rectum and rectosigmoid with preservation of the sphincter for benign spastic lesions producing megacolon. Surgery. 1948;24:212–220. [PubMed] [Google Scholar]
- 16.Kasai M, Suzuki H, Ohi R, et al. Rectoplasty with posterior triangular colonic flap- A radical operation for Hirschsprung’s disease. J Pediatr Surg. 1977;12:207–211. doi: 10.1016/s0022-3468(77)80009-2. [DOI] [PubMed] [Google Scholar]
- 17.Kasai M, Suzuki H, Watanabe K. Rectoplasty with posterior triangular colonic flap- A radical new operation for Hirschsprung’s Disease. J Pediatr Surg. 1971;6:36–41. doi: 10.1016/s0022-3468(77)80009-2. [DOI] [PubMed] [Google Scholar]
- 18.Kasai M, Mori S, Watanabe T. Follow-up results after resection of thoracic esophageal carcinoma. World J Surg. 1978;2:543–551. doi: 10.1007/BF01563699. [DOI] [PubMed] [Google Scholar]