Abstract
The immunogenic Heat shock proteins (HSPs) gp96, hsp70 and calreticulin bind to CD91 on antigen presenting cells for cross-presentation of the HSP-chaperoned peptides. This event leads to priming of T cell responses. We show that CD91 serves as a signaling receptor for these HSPs allowing for the maturation of the antigen presenting cells (APC), secretion of cytokines, and priming of T helper cells. Specifically, CD91 is phosphorylated in response to HSPs in a unique pattern and phospho-CD91 triggers signaling cascades to activate NF-κB. Each HSP-CD91 interaction on antigen presenting cells stimulates a unique cytokine profile which dictates priming of specific T helper cell subsets. Thus, in a TGF-β tumor microenvironment, immunization with calreticulin but not gp96 or hsp70 primes Th17 cell responses in a CD91-dependent manner. These results are important for development of T cell responses in situ in tumor-bearing hosts and for vaccination against cancer and infectious disease.
Keywords: Heat shock protein, CD91/LRP1, Th17 cells, NF-κB
INTRODUCTION
Heat shock proteins (HSPs) gp96, hsp70, hsp90 and calreticulin prime immune responses that have been utilized for immunotherapy of cancer and infectious disease (1–3). These immune responses, which are primarily T cell responses primed against the peptides that these HSPs chaperone (4–5), mediate their effects through cytotoxicity of antigen expressing cells. In several antigenic systems tested in vitro and in vivo, dendritic cells and macrophages acquire extracellular HSPs via the receptor CD91 and cross-present the peptides that are naturally chaperoned by these HSPs on MHC molecules (6–12), providing signal 1 for T cell priming.
Less is known about how HSPs stimulate APCs to provide co-stimulation. APCs stimulated with HSPs have been shown to activate NF-κB, release pro-inflammatory cytokines, and up-regulate the expression of CD40, B7 and MHC II, the classic markers of DC maturation (13). While CD91 is the key receptor for HSP-mediated endocytosis and cross-presentation of chaperoned peptides, the HSP receptor that is responsible for these innate responses in APCs is not known. Several candidates have been proposed. The TLR2/4 touted as HSP receptors (14,15), have been mired in controversy since the results have been indistinguishable from endotoxin-mediated responses. Complete removal of contaminating endotoxin from HSP preparations, the use of GLP-grade HSP, or the use of TLR2/4−/− cells or mice, have shown no dependence on TLRs (16). In addition, affinity chromatography and cross-linking experiments have not shown any association of HSPs with TLRs (6).
Since CD91 was the primary receptor isolated in those studies we have asked the question whether CD91 is involved in innate responses elicited by HSPs thereby acting as a signaling receptor. We show, first, CD91 is the receptor for the HSP-induced innate responses. Specifically we show that activation of NF-κB in APCs by gp96, hsp70 and calreticulin is dependent on CD91 and the phosphorylation of its cytosolic domain. Interestingly while all 3 HSPs engage CD91 on APCs, gp96 and calreticulin utilize different phosphorylation sites on the receptor from hsp70 for the activation of NF-κB. Second, the unique cytokine profile resulting from each HSP-CD91 interaction determines the nature of the effector T cells that are ultimately primed. In a TGF-β-secreting tumor microenvironment, calreticulin but not gp96 or hsp70 immunization is able to prime Th17 cells in draining lymph nodes. We show that IL-6 and TNF-α, but not IL-21 or IL-23 (17), are necessary for calreticulin-mediated Th17 priming. The results show how each immunogenic HSP can direct different T cell responses through a single receptor CD91 and are important in understanding the initiation of immune responses when HSPs are released into the extracellular environment from tumor or infected cells (13,18). These data also directly impact clinical trials where HSPs are used for cancer immunotherapy (19,20). Thus, CD91 acts as a signaling receptor for the immunogenic HSPs and the resulting immune responses can be skewed to various T helper subsets.
RESULTS
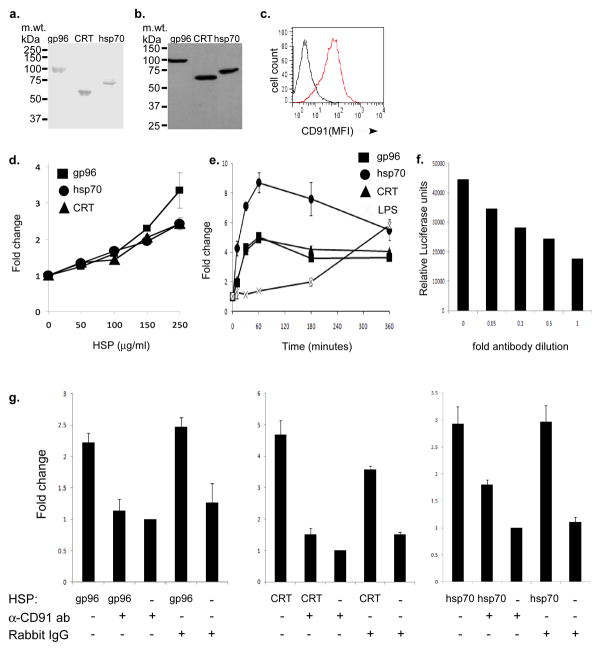
HSP-mediated NF-κB activation is CD91 dependent
Immunogenic HSPs, gp96, hsp70 and calreticulin bind to CD91 (6,7). To determine if CD91 was a signaling receptor for HSPs, gp96, hsp70 and calreticulin were purified from mouse tissues in an endotoxin-free procedure to apparent homogeneity as characterized by SDS-PAGE (Fig. 1a) and immunoblotting (Fig. 1b). RAW264.7 cells which express high levels of CD91 (Fig. 1c), were transfected with the NF-κB reporter construct such that NF-κB activation could be monitored by a luciferase assay. Reporter-transfected RAW264.7 cells were pulsed with increasing doses of gp96, hsp70 or calreticulin as indicated for 30 mins. NF-κB was measured in the supernatants and plotted as fold increase over PBS-pulsed cells. All three HSPs activated NF-κB in a dose dependent manner (Fig. 1d). In a time course experiment, gp96, hsp70 and calreticulin activated NF-κB rapidly and achieved maximum response within 60 mins and waned thereafter (Fig. 1e). The kinetics of NF-κB activation by LPS was different; 1 EU of LPS did not elicit a response at 60 mins but rather achieved its maximum response at 6 hrs, fully consistent with previous observations (13). To determine if activation of NF-κB was dependent on CD91, transfected RAW264.7 cells were incubated with HSPs in the presence or absence of anti-CD91 antibody or control IgG. Prior to use in this experiment the amount of anti-CD91 antibody was carefully titrated and optimized (Fig. 1f). A dose of 20μg (per 100μl reaction volume) was considered the maximal blocking concentration that did not compromise cell viability. We found that anti-CD91 antibody was able to fully abrogate NF-κB activation (to background levels set by antibody alone groups) when cells were pulsed with gp96 or calreticulin (Fig. 1g) (Student’s t-test, p<0.001, p<0.002 respectively). The NF-κB signal was partially abrogated (~50%) when cells were pulsed with hsp70 (Student’s t-test, p<0.01) (Fig. 1g). Neither antibody by itself activated NF-κB. These data demonstrate that CD91 was acting as a signaling receptor for the immunogenic HSPs and that this activation was not due to undetectable amounts of endotoxin.
Figure 1. HSP-mediated NF-κB activation is CD91 dependent.
a. Gp96, Calreticulin (CRT) or hsp70 were purified and 1μg was analyzed on a 10% SDS-PAGE. b. Gp96, CRT or hsp70 were immunoblotted with their corresponding antibodies. c. The macrophage cell line RAW264.7 was stained with rabbit anti-CD91 IgG (red) or control rabbit IgG (black) and then with a FITC-labeled secondary antibody. Mean fluorescent intensities (MFI) are measured. d. RAW264.7 cells transfected with NF-κB-luciferase reporter were pulsed with gp96, CRT or hsp70 at different concentrations and luminescence was measured after 30 min. Results are plotted as fold change in luciferase activity of HSP-pulsed cells over that of PBS pulsed cells. e. RAW264.7 cells transfected with NF-κB-luciferase reporter were pulsed with equimolar amounts of gp96, CRT, or hsp70, 1 EU LPS or PBS for different times and luminescence was measured. Results are plotted as fold change in luciferase activity of HSP-pulsed or LPS-pulsed cells over that of PBS-pulsed cells. f. RAW264.7 cells transfected with the NF-κB-luciferase reporter were incubated with 100μg/ml of gp96 without (0) anti-CD91 antibody or with increasing antibody concentrations. NF-κB activation was plotted by relative luciferase units. g. RAW264.7 cells transfected with the NF-κB-luciferase reporter plasmid were pulsed with gp96, CRT or hsp70 in the presence or absence of the anti-CD91 IgG or control rabbit IgG. Control cells were incubated with the antibodies alone without HSPs. The relative luciferase units were measured after 30 min incubation and plotted as fold change over anti-CD91 antibody alone. Error bars in (d–g) represent the standard deviation of triplicates. Figure shows one of at least 3 independent experiments with similar results.
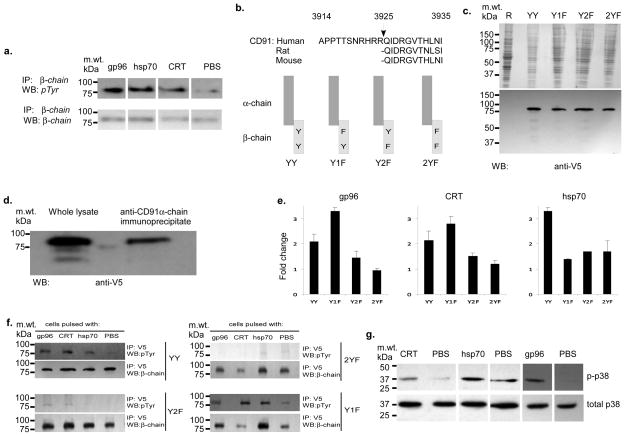
HSPs use alternative tyrosine phosphorylation sites on CD91
Signaling receptors typically utilize tyrosine phosphorylation to transmit signals intracellularly. CD91 consists of an extracellular α-chain non-covalently associated with a β-chain. The β-chain harbors the transmembrane and intracellular domains with two tyrosine phosphorylation (NPXY) motifs. To test for phosphorylation of CD91, RAW264.7 cells were pulsed with gp96, hsp70 or calreticulin and the β-chain was immunoprecipitated. The β-chain immunoprecipitates were probed via immunoblotting with anti-phosphotyrosine (pTyr) antibodies (Fig. 2a). We found that with each HSP, the β-chain was phosphorylated while PBS pulsed cells did not show such phosphorylation. Equal amounts of β-chain were immunoprecipitated in each group.
Figure 2. HSPs use alternative tyrosine phosphorylation sites on CD91.
a. RAW264.7 cells were pulsed with gp96, CRT, hsp70 or PBS for 30 min and CD91 was immunoprecipitated with mouse anti-CD91 β-chain antibody. Immunoprecipitates were probed with 4G10/PY20 anti-phosphotyrosine antibodies (pTyr) or with β-chain specific antibody (β-chain). b. Alignment of the CD91 sequence from human, rat and mouse showing the highly conserved furin cleavage site which forms the α- and β-chains. The two NPXY motifs in the β-chain of CD91, where the tyrosines can be phosphorylated for intracellular signaling, is shown. Mutations of these tyrosines individually (YIF, Y2F) or together (2YF) to phenylalanine along with wild type (YY) construct were cloned in fusion with the V5 epitope. Constructs are depicted. c. The 4 constructs were transfected separately in RAW264.7 carrying the NFκB luciferase reporter. The cell lysates of the untransfected (R) or transfected cells were analyzed by SDS-PAGE and immunoblotted with anti-V5 antibody to probe for the expression of the 85kDa exogenous β-chain. d. The α-chain of CD91 was immunoprecipitated from the cell lysate of RAW264.7 cells transfected with the representative YY construct using anti-CD91α-chain antibody. The cell lysate and the immunoprecipitate were analyzed by SDS-PAGE and immunoblotted with anti-V5. Similar results were obtained with the other constructs. e. Each of the doubly transfected RAW264.7 cells (NF-κB-luciferase reporter and β-chain mutant) were pulsed with gp96, CRT, hsp70 or PBS. The relative luciferase units were measured after 30 min incubation and plotted as fold change in luciferase activity of HSP-pulsed cells over that of PBS-pulsed cells. Error bars represent standard deviation of tripicates. f. RAW264.7 transfected with wild type β-chain (YY) or with β-chain mutants (Y2F, 2YF or YIF) were pulsed with gp96, CRT or hsp70 or PBS for 30 min. The β-chains were immunoprecipitated from cell lysates with anti-V5 antibody and probed for phospho-Tyr (pTyr) or β-chain. g. RAW264.7 was pulsed with gp96, CRT, hsp70 or PBS for 30 min and cell lysates obtained. The lysates were immunoblotted with anti-phospho-p38 (p-p38) and anti-p38 (total p38) antibodies. Data are representative of at least 3 independent experiments with similar results.
To determine which tyrosine in the two NPXY motifs of the β-chain of CD91 were utilized for signal transduction we took advantage of the inherent processing of CD91 to mutate the tyrosine. The 600 kDa polypeptide chain of CD91 is cleaved in the ER at a furin cleavage site (conserved in rodents and humans) into the α and β-chains which then re-associate non-covalently (Fig. 2b) (22,23). We cloned the β-chain (YY), attached the ER signal sequence of the α-chain and a C-terminal V5 epitope by PCR to this construct and used site-directed mutagenesis to change the membrane proximal (Y1F) or the distal (Y2F) or both (2YF) tyrosine(s) in the NPXY motifs to phenylalanine as depicted (Fig. 2b). The constructs were expressed in RAW264.7 cells which endogenously express wild type α and β-chains. Similar levels of expression were observed for each construct in immunoblotting of RAW264.7 cell lysates for the V5-epitope tag (Fig. 2c). We tested if the mutant β-chain constructs associated with the endogenous α-chain. The endogenous α-chain was immunoprecipitated from cells expressing each of the various mutants and the immunoprecipitates were probed with anti-V5-epitope antibody. A representative immunoblot in Fig. 2d shows that the expressed β-chain (YY) co-immunoprecipitated with the endogenous α-chain. We tested the dependence of the HSP on each tyrosine for signal transduction. RAW264.7 cells doubly transfected with the NF-κB reporter construct and one of the respective mutant CD91 β-chain were pulsed with gp96, hsp70 or calreticulin or PBS. We found that gp96 and calreticulin both required the membrane distal but not the proximal tyrosine for NF-κB activation because activation was significantly abrogated in Y2F cells (Fig. 2e). NF-κB was slightly enhanced in Y1F cells. On the other hand, hsp70 required both the proximal and distal tyrosines for NF-κB activation because activation was abrogated in both Y2F and Y1F cells (Fig. 2e). No further significant reduction in NF-κB activation was observed when (2YF) cells with both tyrosines mutated were pulsed with any HSP. These results show that while gp96, hsp70 and calreticulin all signal through CD91, they do so in different ways by utilizing either the membrane distal (gp96, hsp70, calreticulin) or proximal (hsp70) NPXY motifs. We confirmed the results in Fig. 2e by immunoprecipitations of the β-chain and immunoblotting for pTyr. The loss of NF-κB signal observed in cells transfected with Y2F and 2YF after pulsing with each HSPs observed in Fig. 2e is also seen by immunoblotting where a decrease in phosphorylation signal is seen with tyrosine mutations (Fig. 2f). In addition to activation of NF-κB we examined HSP-pulsed RAW264.7 cells for activation of other signaling molecules. We observed that phospho-p38 MAPK was increased in cells pulsed with gp96, hsp70 or calreticulin when compared to PBS-pulsed cells (Fig. 2g). Total p38 in all groups remained the same. No specific phosphorylation of Akt, ERK1/2, JNK1/2/3, MKK3/6 or MAK2 was observed.
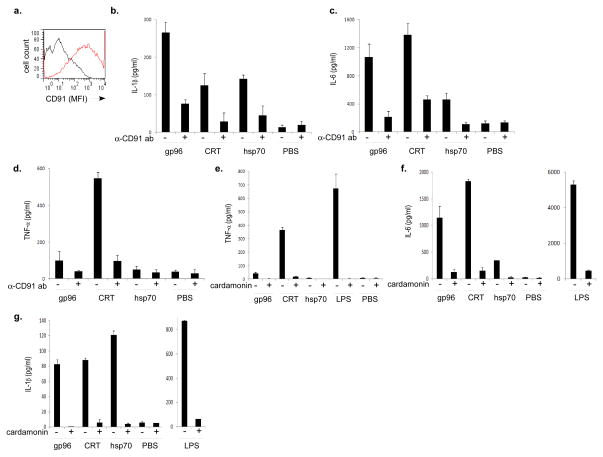
HSP-CD91 interactions provide distinct cytokine profiles
The differences observed in the way the HSPs use the receptor CD91 suggested that the outcomes of the signaling cascades initiated by receptor phosphorylation would be different for each HSP. We analyzed an array of cytokines and chemokines secreted, first, by the RAW264.7 cell line in a cytokine array profiler (Table 1). RAW264.7 cells were pulsed with gp96, hsp70 or calreticulin. Supernatants were harvested after 20 hrs and analyzed by immunoblot-arrays. Two observations were made; first, cytokines released included known NF-κB dependent (e.g. IL-6, IL-1β) and independent genes (e.g. G-CSF), and second, the cytokines released in response to each HSP were distinct (e.g. CXCL11) and overlapping (e.g. IL-1β, IL-12p70). These results suggest that multiple and NF-κB independent pathways exist for APC activation and that the differences seen at the CD91-phosphorylation level are translated to the respective cytokine profiles. Secondly, we analyzed five cytokines known to be important for T helper cell differentiation and/or proliferation by the more quantitative ELISA. We used inherent (un-manipulated) murine APCs to mimic what would happen in vivo in response to extracellular HSPs. Peritoneal exudate cells (PECs) which as a population express high levels of CD91 (Fig. 3a) and cross-present HSP-chaperoned peptides (7,24), were isolated from naïve mice and immediately pulsed with equimolar amounts of gp96, hsp70, calreticulin or PBS. Supernatants were harvested after 20 hrs and analyzed by ELISA for IL-1, IL-6, IL-21, IL-23 and TNF-α (Fig. 3b–d). The incubations were performed in the presence or absence of anti-CD91 antibody. Several observations were made; first, IL-1β was released in comparable amounts by PECs pulsed with gp96, calreticulin or hsp70 (Fig. 3b), second, gp96- or calreticulin -pulsed PECs released IL-6 while hsp70-pulsed PECs released significantly less IL-6 (Fig. 3c), third, calreticulin-pulsed PECs released 5 times more TNF-α than PECs pulsed with gp96 or hsp70 (Fig. 3d), and fourth, all 3 cytokines elaborated by PECs in response to HSPs were CD91-dependent since anti-CD91 antibody significantly inhibited these responses (Fig. 3b–d) (Student’s t-test, p<0.05 comparing with and without anti-CD91 antibody in all groups). No IL-21 or IL-23 was detected when PECs were pulsed with any of the HSPs. In a second set of experiments we tested the dependence of cytokine secretion on NF-κB activation. PECs were isolated from naïve mice and immediately pulsed with gp96, hsp70, calreticulin, LPS or PBS in the presence or absence of the NF-κB inhibitor Cardamonin. Supernatants were harvested after 20 hrs and analyzed by ELISA for IL-1β, IL-6, and TNF-α (Fig. 3e–g). In each situation where HSP- or LPS-pulsed PECs released the cytokines IL-1β, IL-6 or TNF-α, Cardamonin was able to significantly abrogate the response (Student’s t-test, p<0.05 comparing with and without Cardamonin in all groups). Cytokines released by HSP-pulsed PECs were therefore CD91- and NF-κB- dependent.
Table 1. Distinct cytokine release profiles by HSPs.
RAW264.7 cells were pulsed with gp96, calreticulin or HSP70 or PBS for 20 hr. Supernatants were harvested and analyzed with a mouse cytokine array kit and quantified with Kodak imager.
| gp96 | Calreticulin | Hsp70 | Regulation | |
|---|---|---|---|---|
| IL-1ra | ++++ | ++ | − | NF-κB |
| G-CSF | + | + | − | MAPK |
| IL-6 | +++ | +++ | + | NF-κB/MAPK |
| CXCL10 | + | + | + | NF-κB |
| CCL17 | + | + | + | NF-κB |
| IL-12p70 | ++ | ++ | ++ | NF-κB |
| CXCL11 | − | + | − | NF-κB |
| TREM1 | ++++ | ++ | − | unknown |
| IL-1β | +++ | +++ | +++ | NF-κB |
| TNF-α | + | ++++ | − | NF-κB |
+ indicates fold increase over PBS pulsed cells. Data is representative of 3 independent experiments.
Figure 3. HSP-CD91 interactions provide distinct cytokine profiles.
a. Peritoneal exudate cells obtained from C57BL/6 mice were stained with rabbit anti-CD91 antibody (red) or control IgG (black) and then with the FITC-labeled secondary antibody. PECs obtained from C57BL/6 mice were incubated for 20 hr with gp96, CRT or hsp70 or PBS. Incubations were done in the presence (+) or absence (-) of anti-CD91 antibody. Supernatants were harvested and assayed by ELISA for; b. IL-1β, c. IL-6 or d. TNF-α. PECs obtained from C57BL/6 mice were incubated for 20 hr with gp96, CRT or hsp70 or 1EU LPS or PBS. Incubations were done in the presence (+) or absence (−) of 10 μM of the NF-κB inhibitor Cardamonin. Supernatants were harvested and assayed by ELISA for e. TNF-α, f. IL-6 or g. IL-1β. Error bars in b–g. represent standard deviation of triplicates. Figure represents one of at least 2 a or 3 b–g independent experiments with similar results.
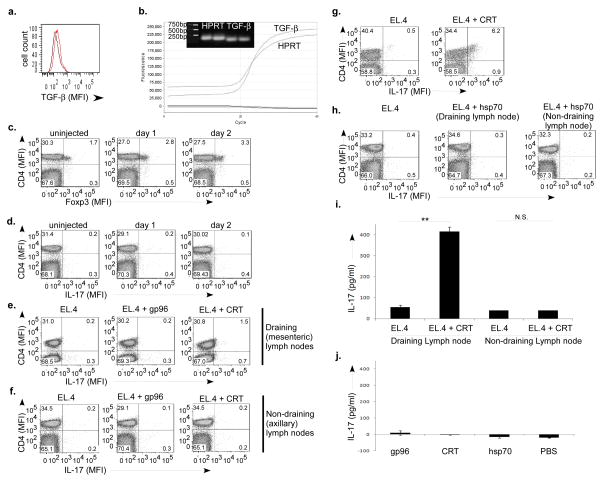
Calreticulin primes Th17 cells in a TGF-β microenvironment
HSP immunization typically targets lymph nodes distant from the tumor, where the release of pro-inflammatory cytokines such as IL-1β, TNF-α, and IL-12 by targeted APCs skew responses to the Th1/CTL phenotype (1,3,4,13). However, targeting HSP immunization to local APCs and tumor-draining lymph nodes with different cytokine milieus may generate alternate phenotypes. We asked the question whether HSP immunization at draining lymph nodes, could bias responses to a Th17 phenotype in a TGF-β microenvironment (25), given the robust IL-6 production from gp96 or calreticulin -treated PECs (Fig. 3c). The EL.4 tumor expresses TGF-β (26) and was used as a constant source of TGF-β in vivo. We confirmed TGF-β expression by our EL.4 cell line by flow cytometry (Fig. 4a), consistent with previous studies (26). In addition, TGF-β expression was confirmed by real time and RT-PCR, alongside the housekeeping gene hypoxanthine-guanine phosphoribosyl transferase (HPRT). Fig. 4b shows that TGF-β is expressed by real time PCR and by electrophoresis of RT-PCR. To determine if these levels of TGF-β had any immune relevance we injected the EL.4 tumor into the peritoneum of mice. Mesenteric lymph nodes were harvested from mice every 24 hrs after injection and proliferation of CD4+Foxp3+ cells was monitored. We found that this population increased over the course of 2 days (Fig. 4c) (in 4 mice per group tested; Student’s t-test, p=0.018). No difference in the Th17 population was observed as a result of tumor inoculation over this period (in 4 mice per group tested; Student’s t-test, p=0.39) (Fig. 4d). Mice were then immunized with EL.4 tumor cells alone or simultaneously with gp96 or calreticulin. Draining mesenteric (Fig. 4e) or non-draining axillary (Fig. 4f) lymph nodes were harvested after 6 days and stained for Th17 cells. Co-immunization of EL.4 and calreticulin primed Th17 cells in draining lymph nodes (in 6 of 8 responders; Student’s t-test, p=0.047) while co-immunization of EL.4 tumor with gp96 did not prime Th17 cells (in 8 mice tested, Student’s t-test, p=0.216) (Fig. 4e). No Th17 responses were observed in non-draining lymph nodes (Fig. 4f). The Th17 cells observed in EL.4 + calreticulin immunized mice could be significantly expanded ex vivo by stimulation with PMA/ionomycin for 4 hrs (with golgi plug) to reveal a distinct CD4+IL17+ population (in 8 mice tested, Student’s t-test, p<0.002) (Fig. 4g). No such phenotype was observed in mice immunized with EL.4 cells alone. Mice co-immunized with EL.4 tumor and hsp70 did not prime Th17 cells in draining (in 8 mice tested, Student’s t-test, p=0.28) or non-draining lymph nodes (Fig. 4h). To confirm the presence of a population of Th17 cells in the EL.4 + calreticulin immunized mice, draining or non-draining lymph node cells were harvested, sorted for CD4+ cells and stimulated ex vivo with plate bound anti-CD3 and irradiated spleen for 3 days. Culture supernatants were harvested and tested for IL-17A by ELISA. Culture supernatants from this group were observed to have 8 fold higher amounts of IL-17A compared to lymph node cells derived from mice immunized with EL.4 cells alone (Fig. 4i). In addition, no IL-17A was detected in non-draining lymph nodes (Student’s t-test, p>0.1). For other controls, mice were immunized with HSPs alone, i.e. in the absence of TGF-β (no EL.4 cells). No Th17 cells were detected (Student’s t-test, p> 0.2 any HSP compared to PBS) (Fig. 4j).
Figure 4. Calreticulin primes Th17 cells in a TGF-β microenvironment.
a. EL.4 cells were analyzed by flow cytometry for intracellular TGF-β (red). Black line is irrelevant isotype antibody. b. Expression level of TGF-β1 in EL.4 cells was analyzed by real time RT-PCR and compared to the positive control HPRT. Agarose gel electrophoresis of RT-PCR for HPRT (214bp) and TGF-β1 (145bp) is shown in duplicates. c. C57BL/6 mice were injected intraperitoneally with EL.4 cells on day 0 and the mesenteric lymph nodes were harvested from groups of mice on every day and stained for CD4 and Foxp3. d. Mice were administered EL.4 cells on day 0 and the mesenteric lymph nodes analyzed by flow cytometry for IL-17. e. Mice were administered EL.4 cells alone or with gp96 or CRT. The mesenteric lymph nodes were harvested on day 6 and analyzed by flow cytometry for IL-17. f. Mice were administered EL.4 cells alone or with gp96 or CRT. The non-draining lymph nodes were harvested on day 6 and analyzed by flow cytometry for IL-17. g. C57BL/6 mice were administered EL.4 cells alone or with CRT. The mesenteric lymph nodes were harvested on day 6 and stimulated for 4 hrs with PMA and ionomycin. Cells were analyzed by flow cytometry for IL-17. h. Mice were administered EL.4 cells alone or with hsp70. The draining or non-draining (axillary) lymph nodes were harvested on day 6 and analyzed by flow cytometry for IL-17. i. Mesenteric or axillary lymph node CD4+ cells were cultured ex vivo for 3 days with anti-CD3 and irradiated spleen and supernatants were tested for IL-17A by ELISA. Error bars represent standard deviation of triplicates (**Student’s t-test p<0.01, N.S is non-significant). j. Mice were administered HSPs or PBS. The mesenteric lymph nodes were harvested on day 6 and were cultured ex vivo for 3 days with anti-CD3 and irradiated spleen. Culture supernatants were tested for IL-17A. Error bars represent standard deviation of triplicates. Figure is representative of one set of a total of 4 (c,d), or 8 (e–h) or 3 sets of mice (i,j), tested in independent experiments.
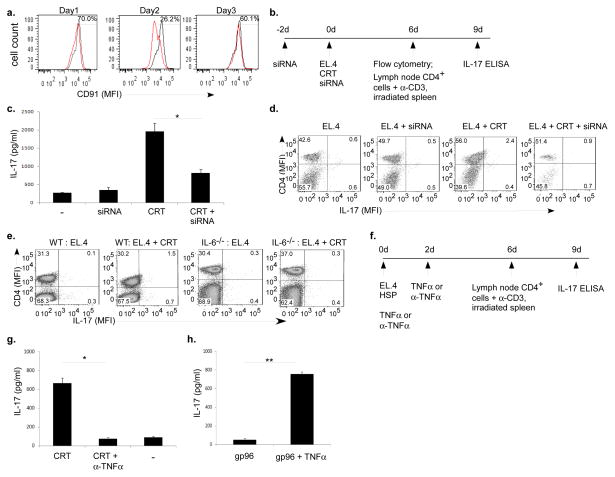
Th17 priming is dependent on CD91 and IL-6 and TNF-α
We have demonstrated the requirement of CD91 for HSP signaling in APCs in vitro (Fig. 1g & 3). We tested if CD91 signaling was required for Th17 priming in vivo by administering CD91-targeting siRNA to mice intraperitoneally. PECs were harvested every 24 hrs and CD91 expression was monitored by flow cytometry. We observed that CD91 expression was diminished by 30% and 73% on day 1 and day 2 post-administration, respectively (Fig. 5a). Cells began to recover CD91 expression after day 2. We then designed an experimental scheme to test the dependence of Th17 priming on CD91 (Fig. 5b). CD91-targeting siRNA was administered intraperitoneally on day -2 and day 0 to ensure CD91 expression remained diminished spanning calreticulin introduction. EL.4 with or without calreticulin was then administered on day 0. Draining (mesenteric) lymph nodes were harvested on day 6, sorted for CD4+ cells, cultured with plate bound anti-CD3 and irradiated spleen cells and tested for IL-17A on day 9. The high IL-17A levels observed with EL.4 + calreticulin was effectively abrogated when CD91-targeting siRNA was administered (Fig. 5c). Administration of EL.4 with or without siRNA set the background IL-17A level. These data were confirmed by flow cytometry on day 6. Draining lymph node cells from EL.4 + calreticulin immunized mice demonstrated a significant population of Th17 cells which was diminished in the presence of CD91-siRNA (in 9 pairs of mice tested in 3 independent experiments, Student’s t-test, p<0.04) (Fig. 5d). No Th17 responses were detected in mice administered EL.4 with or without siRNA. The cytokines tested for in Fig. 3, were those that have been shown to be necessary for or supported Th17 differentiation and/or proliferation (27,28). We therefore tested the role of IL-6 and TNF-α in calreticulin-mediated Th17 priming. IL-6 deficient or wild type mice were immunized with EL.4 alone or co-immunized with EL.4 + calreticulin. Priming of Th17 cells observed in wild type mice was abrogated in IL-6 deficient mice (3 mice per group in 3 independent experiments, Student’s t-test, p=0.48) (Fig. 5e) indicating that IL-6 was necessary for the calreticulin-mediated Th17 priming. We tested the role of TNF-α in two independent assays (Fig. 5f). First, mice were administered EL.4 + calreticulin in the presence or absence of anti-TNF-α antibody. Further antibody was administered on day 2. Draining (mesenteric) lymph nodes were harvested on day 6, sorted for CD4+ cells, cultured with plate bound anti-CD3 and irradiated spleen cells and tested for IL-17A on day 9. The robust IL-17A production observed in the EL.4 + calreticulin group of mice was effectively abrogated by anti-TNF-α antibody (Fig. 5g). Second, mice were administered EL.4 + gp96 together with recombinant TNF-α. Further rTNF-α was given on day 2. Draining (mesenteric) lymph nodes were harvested on day 6, sorted for CD4+ cells, cultured with plate bound anti-CD3 and irradiated spleen cells and tested for IL-17A on day 9. In the presence of rTNF-α, gp96 was able to prime cells to produce IL-17A (Fig. 5h). Our results show that Th17 priming by calreticulin was dependent on CD91, IL-6 and TNF-α.
Figure 5. Th17 priming is dependent on CD91 and IL-6 and TNF-α.
a. Mice were inoculated intraperitoneally with CD91-targeting siRNA for various times. PECs were analyzed by flow cytometry every 24 hrs. b. Experimental scheme for determining the dependence of Th17 priming on CD91. CD91-targeting siRNA was administered to mice prior to (day -2) and during EL.4 + CRT administration (day 0). c. Draining lymph nodes were harvested on day 6. CD4+ cells were isolated and stimulated with α-CD3 and irradiated spleen ex vivo. Culture supernatants were tested on day 9. Controls include mice administered EL.4 alone (−) and EL.4 + siRNA (siRNA). Error bars represent standard deviation of triplicates (*Student’s t-test p<0.05). d. Draining lymph node cells from mice administered EL.4 + CRT, with or without siRNA, were harvested on day 6 and stained for CD4 and IL-17 and analyzed by flow cytometry. Controls include mice administered EL.4 alone and EL.4 + siRNA. e. Wild type or IL-6 deficient mice were inoculated with EL.4 alone or EL.4 + CRT. Draining lymph node cells from all mice were harvested on day 6 and analyzed by flow cytometry. Figure is representative of one pair of a total of 3 pairs of mice. f. Experimental scheme for determining the dependence of Th17 priming on TNF-α. Mice were administered EL.4 cells together with gp96 or CRT. Mice receiving EL.4 + CRT were administered α-TNF-α antibody on day 0 and day 2. Mice receiving EL.4 + gp96 were administered rTNF-α on day 0 and day 2. CD4+ cells were isolated from the lymph node cells on day 6 and stimulated with α-CD3 and irradiated spleen ex vivo. Culture supernatants were tested on day 9 for IL-17A. g. ELISA for IL-17A from mice administered EL4 + CRT and α-TNF-α antibody. Controls include mice administered only EL.4 + CRT (CRT) or EL.4 alone (−)(*Student’s t-test p<0.003). h. ELISA for IL-17A from mice administered EL4 + gp96 and rTNF-α. Mice were administered EL.4 + gp96 (gp96) as a control (**Student’s t-test p< 0.004). Figure represents one of 3 independent experiments with similar results in c, g and h.
DISCUSSION
Immunization with HSPs elicits potent Th1/CTL anti-tumor immune response. HSPs engage CD91 on APCs which allows for cross-priming of the chaperoned peptide antigen (6,7). These events have been well characterized. One question that has remained unresolved was the mechanism by which HSPs provided signal 2 necessary for priming T cells and what alternative T cell responses may be obtained. We describe here that the receptor CD91 plays a central role in signal transduction by HSPs via activation of p38 MAPK and NF-κB. HSPs utilize different phosphorylation sites on CD91 which may account for distinct cytokine profiles released by APCs in response to respective HSPs. These cytokine patterns (for calreticulin) are shown to be capable of directing T cells responses to a Th17 phenotype.
CD91 was shown to be the endocytic receptor for the immunogenic HSPs including gp96, hsp90, hsp70 and calreticulin and it is required for cross-presentation of HSP-chaperoned peptides and tumor immunity (6–12). In one study where CD91 independence of HSP responses was described (29), the results were shown to be a result of several lacunae in experimental design (8). Once these lacunae are addressed, CD91 is shown to play a vital role in the interaction of gp96 with APCs.
CD91 is a typical scavenger receptor, which binds and internalizes multiple structurally and functionally diverse ligands. It is synthesized as a 600 kDa type I transmembrane protein which, during transit to the cell surface, is processed by furin (22) into a 515 kDa α- and a 85 kDa β-subunit in the trans-Golgi network (23). A number of CD91 ligands, including tPA, α2M, apoE, MMP-9, and connective tissue growth factor, have recently been shown to activate signaling cascades after binding to CD91 (30–35). For example, the activation of both MAPK and NF-κB has been observed following binding of α2M to CD91 which in turn induces MMP-9 production (35). In these studies CD91 may regulate the cellular microenvironment by its ability to endocytose diverse extracellular mediators, facilitating endocytosis of other transmembrane receptors involved in cell signaling or directly regulating cell signaling and gene transcription via adaptor proteins. Given the emerging role of CD91 in signaling, our data extends the role of CD91 to immune system regulation through its interaction with extracellular HSPs. Basu et al., described the activation and nuclear translocation of NF-κB in response to HSPs (13). We now show that the activation happens through CD91. By selective mutations of the two tyrosines of CD91, gp96 and calreticulin were determined to utilize membrane-proximal tyrosine 4507 while hsp70 utilizes both tyrosine 4473 and tyrosine 4507 to transduce signals. Unlike LDLR, the NPXY motifs of CD91 do not play a role in endocytosis (36) but are rather involved in binding pTyr-binding domains of intracellular signaling proteins (37–40). We are yet to confirm adaptor proteins but a number of candidates exist in the literature; PI3K, Shp-2, CSK, Shc-3, Grb-2 have been shown to associate with tyrosine 4507 of CD91 in response to various (non-HSP) ligands (41). These candidates may be used by the HSPs to transmit signals. For hsp70 there may be other binding partners which interact with tyrosine 4473. Downstream, we show that p38 MAPK is activated. Others kinases, ERK and PI3kinase, are also phosphorylated in a CD91 dependent manner (42). These signaling proteins along with NF-κB activation and p38 phosphorylation may constitute a single or multiple pathways. The full signaling cascade is currently under investigation. We have been extremely careful in these studies with respect to endotoxin contamination. TLR2/4 have been suggested to be involved in HSP-mediated signaling and activation of APCs. However a large body of literature, including our data presented here suggests that the TLRs have no contribution to HSP-mediated signaling events (for review see 16).
The current literature on HSP-signaling presents a disjointed picture due to the use of APCs manipulated in vivo or in vitro (13), cell lines, and HSPs with varying levels of endotoxin contamination (14,15). We have used the macrophage cell line to examine the influence of the signaling cascade on cytokine secretion and unmodified PECs from naïve mice to investigate what the cytokine milieu would be if (endotoxin free) HSPs were present in the extracellular space in the peritoneum. Both NF-κB -dependent and -independent cytokine genes were observed to be activated suggesting that more than a single signaling pathway was being utilized. IL-12, TNF-α and IL-1β are transcribed from genes that are regulated by NF-κB (43–46) and direct immune responses to the Th1/CTL phenotype. We observed that the pro-inflammatory cytokine IL-6 was released by PECs in response to gp96 or calreticulin but to a much lesser degree by hsp70. The difference between gp96 or calreticulin and hsp70 could stem from the difference noted at the receptor tyrosine phosphorylation level although a direct connection between the two events has not yet been made. Indeed IL-6 expression can be regulated by p38 MAPK alone (47) or in combination with NF-κB dependent events (48). This may suggest that an additional NF-κB independent signaling cascade may be invoked by calreticulin and/or gp96. In support of this, calreticulin, but to a much lesser degree gp96 or hsp70, stimulated PECs to release TNF-α.
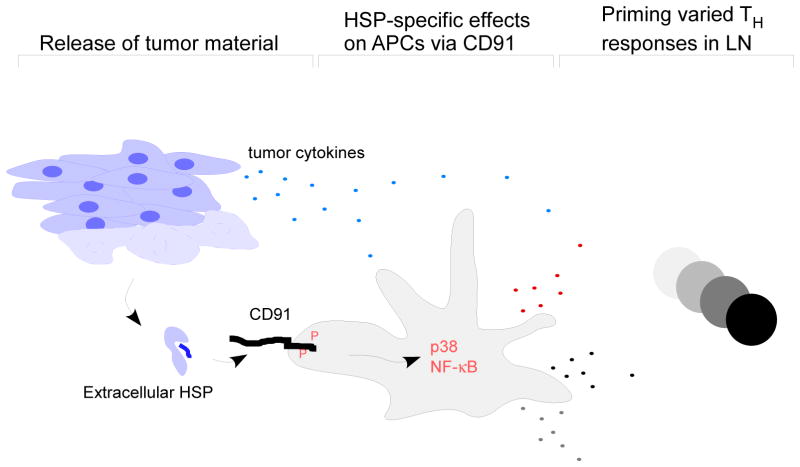
There appears to be a reciprocal development pathway for Treg and Th17 cells with IL-6 playing a pivotal role by inhibiting the generation of Treg cells and inducing the production of Th17 cells. In a TGF-β tumor microenvironment, IL-6 secreted in response to calreticulin, was necessary to direct priming of Th17 cells as demonstrated by the lack of such priming in IL-6−/− mice. However IL-6 was insufficient by itself because gp96, which stimulates PECs to release similar amounts of IL-6, did not prime Th17 cells. However TNF-α production in response to calreticulin correlated with the ability to prime Th17. Hsp70 did not prime Th17 cells probably due to the lack of IL-6 and TNF-α production. IL-21 or IL-23 can act as a polarizing cytokine for Th17 priming in the absence of IL-6 or can enhance the effects of IL-6 (17). Both IL-21 and IL-23 were not released by PECs in response to any HSP. The priming of Th17 cells by calreticulin is currently being tested in various autoimmune disease models but it may also play a role in anti-tumor immunity (49). Extracellular HSPs, introduced via vaccination or released from cells thus have the ability to prime T cell responses of the Th1 (3,18,50), Th2 (51), Treg (52,53) or Th17 type (Fig. 6). The resulting phenotype will depend on the relative abundance of each HSP in the extracellular environment, affinity of each HSP for CD91, the APC type and the contributions of other cell types in the microenvironment. These results have far reaching implications from long term non-progressor HIV patients (50), cancer immunotherapy (19,20) and initiation of immune responses to tumors (13,18).
Figure 6. A model of T helper cell priming by extracellular HSPs.
The release of HSPs from tumor cells (or introduced through vaccination) into the extracellular environment has the potential to stimulate APCs through CD91. The APCs will advertise HSP-specific effects through a unique pattern of co-stimulation (cytokines described here and co-stimulatory molecules [13]) in the draining lymph nodes where they prime Th cell subsets of different types. These effects are nevertheless influenced by other cytokines the tumor cells themselves may release like TGF-β.
METHODS
Molecular biology methods
Total RNA was isolated from mouse liver by using RNeasy Mini Kit (Qiagen, ON, Canada) and treated with RNase-free DNase to eliminate any potential genomic DNA contamination. Aliquots of 1 μg of total RNA were used for first-strand cDNA synthesis by using the Omniscript RT kit (Qiagen). The cDNA was used for amplification (in the 5′-3′ direction) by the primer pair CCCCTGCTCAGTGCTCTAGTTGCTGCTCAGATCGACCGCGGAGTCACCCACCTCA ATATTTC (CD91NT1) and CGCCAAGGGATCTCCTATCTCGTCTTCAGGTCCCCG (CD91CT) and the resulting PCR product was used for amplification by the primer pair CCGATGCTGACCCCGCCGTTGCTGCTGCTGCTGCCCCTGCTCAGTGCTCTGGTTG CTGCTCAG (CD91NT2) and CD91CT for mouse CD91 beta chain. CD91NT1 and CD91NT2 primers add the nucleotides encoding the signal sequence of the CD91 α-chain, which ensures the expression of the exogenous β-chain in the same compartment as the alpha chain. PCR amplification was performed by using 2X Mango Mix (Bioline USA Inc, MA) for 30 cycles (94°C for 30 sec, 55°C for 30 sec, and 72°C for 75 sec). After amplification, the 1.8 kb PCR product was cloned into pEF6/V5-His-TOPO vector (Invitrogen, Carlsbad, CA), containing a V5 epitope at the carboxyl terminal and transformed into E. coli. The wild type CD91 protein has two tyrosine residues at 4473 (NPTY) and 4507 (NPVY) so the wild type β-chain construct was used to make the tyrosine to phenylalanine mutants of CD91 β-chain by using the QuikChange XL Site-Directed Mutagenesis Kit (Stratagene, Santa Clara, CA). The individual mutation of the membrane proximal- and distal-tyrosine was termed as Y1F and Y2F, respectively. The wild type and the mutant with both tyrosine mutated to Phenyalanin was termed as YY and 2YF, respectively. RAW264.7 macrophages were stably transfected with each of the aforementioned plasmids by using Fugene6 transfection reagent (Roche Molecular Biochemicals, Indianapolis, IN). DNA sequencing was performed at Genewiz (La Jolla, CA)
Real Time PCR
Total RNA was prepared from EL.4 cells using the RNeasy mini kit (Qiagen, Hilden, Germany) according to the manufacturer’s instruction. To avoid contamination with genomic DNA, RNA samples were treated with RNase-free DNAse I (Roche Diagnostics GmbH, Mannheim, Germany). To generate cDNA from cell culture samples, 500 ng of total RNA was reverse transcribed using iScript cDNA synthesis kit (Biorad). cDNA was analyzed by real-time PCR by using StepOne Real Time PCR system (Amersham). For amplification, QuantiTect TGF beta1 primers (Qiagen) or custom synthesized HPRT primers (GTAATGATCAGTCAACGGGGGAC forward; CCAGCAAGCTTGCAACCTTAACCA reverse) were used with the iQ SYBR Green supermix (BioRad). For standard RT-PCR using the same primers, the following conditions were used: 35 cycles of 94°C for 30 sec, 55°C for 30 sec, and 72°C for 30 sec. The PCR products were analyzed by agarose gel electrophoresis in 1X TAE buffer (Biorad).
Cell Culture
RAW264.7 and 11H4 cells (American Type Culture Collection, Manassas, VA) were cultured in complete DMEM (1% sodium pyruvate, 1% penicillin and streptomycin, 1% glutamine, 1% non-essential amino acids, 0.1% 2-mercaptoethanol) and 10% FBS (GIBCO/Invitrogen,Carlsbad, CA). The mouse lymphoma cell line EL.4 (ATCC) cells and PECs were cultured in complete RPMI with 5% FBS. RAW264.7 cells transfected with the NF-κB luciferase vector (pNFκB-MetLuc2) or β-chain mutants were grown in 0.4 g/L Geneticin and 2 mg/L Blasticidin, respectively. All cell cultures were maintained at 37°C in a humidified atmosphere containing 5% CO2. To measure IL-17A levels, CD4+ T cells were purified from single suspensions of lymph node cells by negative selection (Miltenyi Biotec, Auburn, CA). CD4+ T cells were plated at equal numbers in anti-CD3 coated plates with irradiated spleen as a source of CD28 ligands in 24 well plates. Culture supernatants were harvested on day 3 and used for IL17A ELISA. For investigating the role of TNF-α, C57BL/6 mice were immunized at day 0 with a single intraperitoneal injection of 2×106 EL.4 cells with the following: (1) 100μg of gp96 or equimolar amounts of calreticulin, (2) 100 μg of gp96 and 10 ng of rTNF-α (ThermoFisher, Pittsburgh, PA) or (3) equimolar amounts of calreticulin and 125μg of anti-TNF-α antibody (Thermofisher). At day 2, another dose of rTNF-α and anti-TNF-α antibody was administered to the respective mice and the mice were euthanized at day 6. The mesenteric lymph nodes were harvested and cell suspensions were used for IL-17A ELISA.
Immunoprecipitation and immunoblotting
Cells (1×106) were grown in P6 culture dishes and pulsed with the HSPs for 30 min. The cells were rinsed with cold PBS and lysed in 1 ml of NP40 Tris Lysis buffer. Lysates were cleared by centrifugation at 10,000 g for 15 min in a microcentrifuge, incubated with 5 μl of polyclonal antiserum or 1 μg of monoclonal antibody for 1 hr on ice, and subsequently for 1 hr with 100 μl of 10% protein G-Sepharose at 4°C on an agitator. Sepharose beads were collected by centrifugation and washed 4 times with NP40 lysis buffer. Immunoprecipitates were boiled for 3 min in SDS sample buffer and resolved by SDS-PAGE. Membranes were blocked for 1 hr in Tris Buffer with tween (TBST) and 5% dried milk, incubated with 1:1000 dilution of polyclonal antisera in TBST 5% milk for 1 hr followed by incubation with horseradish-peroxidase-conjugated polyclonal IgG antibody (Sigma, St. Louis, MO) all at room temperature. Reactive proteins were visualized by ECL (Amersham Pharmacia Biotech, Piscataway, NJ). The protein size was confirmed by molecular weight standards (Bio-Rad, Hercules, CA). Full length immunoblots representing those in Figure 2 are shown in Supplementary Figure S1.
Purification of HSPs
Calreticulin, hsp70 and gp96 were simultaneously purified from C57BL/6 mouse liver tissue according to previously described methods (1–3). No recombinant HSPs were used in any experiment and all proteins had undetectable amounts of endotoxin present. Pulsing experiments in vitro were performed with 100μg/ml of gp96 and equimolar amounts of calreticulin or hsp70 (Figs.1–3). The amounts of HSPs used to pulse cells in vitro was estimated based on calculation of the average amount of HSP produced per cell (2–3 pg) and the average volume of a cell (50μm). Mice were injected with 100μg of gp96 or equimolar amounts of calreticulin or hsp70 (Figs.4 &5)
Expression of CD91 and knockdown using siRNA
CD91 expression on RAW264.7 cells and PECs was measured by staining the cells with 5μg of anti-CD91 antibody for 15 min on ice and after two washes with PBS, incubated with anti-rabbit-FITC antibody. The cells were washed twice with PBS and analyzed by Flow Cytometry. The CD91-targeting siRNA was obtained from Sigma; 5 sequences targeting various portions of the mRNA were mixed (1 nM each). To verify knock down of CD91 in vivo, the siRNA was administered intraperitoneally and PECs were harvested on day 1, 2 and 3 after injection. The cells were stained as mentioned above for CD91 expression which showed highest decrease at day 2 after injection. To determine dependence of Th17 priming on CD91, mice were injected with siRNA two days prior to and during injection of EL.4 or EL.4 and HSP.
Mice and Reagents
Female C57BL/6 and B6.129S6-Il6tmKopf (IL6−/−) mice were obtained from Jackson Laboratory (Bar Harbor, ME) and housed in DLAR at the University of Pittsburgh and were used under the IACUC guidelines after approval of the relevant protocols at the University of Pittsburgh. The following kits were obtained and used according to the manufacturer’s recommendation; Ready to glow secreted luciferase reporter system (Clontech, Mountain View, CA), Mouse Th17/Treg Phenotyping kit (BD Biosciences, San Jose, CA), Oligotex mRNA purification kit (Qiagen, Valencia, CA), Mouse cytokine array panel A, Human Phospho-MAPK array kit. Oligonucleotides were obtained from Eurofins MWG/Operon (Huntsville, AL). The following antibodies were used; mouse anti-phospho-p38 MAPK (The180/Tyr182) (28B10), rabbit anti-p38 MAP Kinase antibody (Cell Signaling Technology, Boston MA), mouse anti-V5-HRP (Invitrogen), mouse anti-pTyr antibody clone 4G10 and clone PY20 (Millipore), anti-CD91 β-chain clone IgG-11H4 (ATCC), anti-TGF-β1,- β2,- β3-allophycocyanin (R&D Systems), Ready-set-Go mouse IL-21, IL-1β, IL-6, TNF-α, IL-23, IL-17A (homodimer) ELISA kits were from eBiosciences (San Diego, CA). Anti-CD3 antibody was a kind gift of Dr. Michael Turner (University of Pittsburgh). Cardamonin was obtained from TOCRIS Biosciences (Ellisville, MS) and used at a concentration of 10μM.
CD91 blocking
The anti-CD91 antibody was obtained from Agenus Inc (Lexington, MA), and was made by immunization of rabbits with the 95aa N-terminal fragment of the α-chain of CD91. The IgG was purified from total serum of the immunized rabbit using the Melon gel IgG purification kit (Pierce, Rockford, IL). Unimmunized rabbit IgG was used as control antibody.
Flow Cytometry
Mice were immunized with a single intraperitoneal injection of 2×106 EL.4 cells with or without 100μg of gp96 or equimolar amounts of calreticulin or hsp70. The mice were euthanized 6 days after the injection and the peritoneum draining (mesenteric) or non-draining (axillary) lymph node were harvested. Single cell suspensions of the lymph node were stained for Th17/Treg phenotypes as recommended by manufacturer’s kit (BD Pharmingen). In some experiments, cells were stimulated with PMA (50 ng/ml), ionomycin (1μg/ml) and golgi plug for 4 hrs prior to staining. Samples were run on LSRII Flow Cytometer (BD Biosciences) and the data was analyzed by FlowJo software.
Statistical analysis
P values were obtained by Student’s t-test.
Supplementary Material
Acknowledgments
The authors would like to thank Laura Kropp, Michelle Messmer, Yu Zhou and Dr. Shabaana Khader for critically reading the manuscript and for helpful insights. We thank Judong Lee, Dr. Larry Kane and Dr. Rohit Sharma for assistance with some experiments.
The study was supported by NIH grants CA137133 and AI079057.
Footnotes
AUTHOR CONTRIBUTIONS
S.P and R.B. designed and performed experiments, analyzed data and wrote the paper. R.B. conceived the study.
R.B is a named inventor of intellectual property and the technology has been licensed to Agenus Inc., in which Dr. Binder has no ownership interest or consulting contract and from which he has no sponsored research agreements.
References
- 1.Srivastava PK, DeLeo AB, Old LJ. Tumor rejection antigens of chemically induce sarcomas of inbred mice. Proc Natl Acad Sci USA. 1986;83:3407–3411. doi: 10.1073/pnas.83.10.3407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Udono H, Srivastava PK. Comparison of tumor-specific immunogenicities of stress-induced proteins gp96, hsp90 and hsp70. J Immunol. 1994;152:5398–5403. [PubMed] [Google Scholar]
- 3.Basu S, Srivastava PK. Calreticulin, a peptide-binding chaperone of the endoplasmic reticulum, elicits tumor- and peptide-specific immunity. J Exp Med. 1999;189:797–802. doi: 10.1084/jem.189.5.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Udono H, Levey DL, Srivastava PK. Cellular requirements for tumor-specific immunity elicited by heat shock proteins: tumor rejection antigen gp96 primes CD8+ T cells in vivo. Proc Natl Acad Sci USA. 1994;91:3077–3081. doi: 10.1073/pnas.91.8.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blachere NE, et al. Heat shock protein-peptide complexes, reconstituted in vitro, elicit peptide-specific cytotoxic T lymphocyte response and tumor immunity. J Exp Med. 1997;186:1315–1322. doi: 10.1084/jem.186.8.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Binder RJ, Han DK, Srivastava PK. CD91: a receptor for heat shock protein gp96. Nat Immunol. 2000;1:151–155. doi: 10.1038/77835. [DOI] [PubMed] [Google Scholar]
- 7.Basu S, Binder RJ, Ramalingam T, Srivastava PK. CD91 is a common receptor for heat shock proteins gp96, hsp90, hsp70, and calreticulin. Immunity. 2001;14:303–313. doi: 10.1016/s1074-7613(01)00111-x. [DOI] [PubMed] [Google Scholar]
- 8.Binder RJ, Srivastava PK. Essential role of CD91 in re-presentation of gp96-chaperoned peptides. Proc Natl Acad Sci USA. 2004;101:6128–6133. doi: 10.1073/pnas.0308180101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tobian AA, Canaday DH, Boom WH, Harding CV. Bacterial heat shock proteins promote CD91-dependent class I MHC cross-presentation of chaperoned peptide to CD8+ T cells by cytosolic mechanisms in dendritic cells versus vacuolar mechanisms in macrophages. J Immunol. 2004;172:5277–5286. doi: 10.4049/jimmunol.172.9.5277. [DOI] [PubMed] [Google Scholar]
- 10.Fischer N, et al. Involvement of CD91 and scavenger receptors in Hsp70-facilitated activation of human antigen-specific CD4+ memory T cells. Eur J Immunol. 2010;40:986–997. doi: 10.1002/eji.200939738. [DOI] [PubMed] [Google Scholar]
- 11.Robert J, Ramanayake T, Maniero GD, Morales H, Chida AS. Phylogenetic conservation of glycoprotein 96 ability to interact with CD91 and facilitate antigen cross-presentation. J Immunol. 2008;180:3176–3182. doi: 10.4049/jimmunol.180.5.3176. [DOI] [PubMed] [Google Scholar]
- 12.De Filippo A, et al. Human plasmacytoid dendritic cells interact with gp96 via CD91 and regulate inflammatory responses. J Immunol. 2008;181:6525–6535. doi: 10.4049/jimmunol.181.9.6525. [DOI] [PubMed] [Google Scholar]
- 13.Basu S, Binder RJ, Suto R, Anderson KM, Srivastava PK. Necrotic but not apoptotic cell death releases heat shock proteins, which deliver a partial maturation signal to dendritic cells and activate the NF-kappa B pathway. Int Immunol. 2000;12:1539–1546. doi: 10.1093/intimm/12.11.1539. [DOI] [PubMed] [Google Scholar]
- 14.Asea A, et al. Novel signal transduction pathway utilized by extracellular HSP70: role of toll-like receptor (TLR) 2 and TLR4. J Biol Chem. 2002;277:15028–15034. doi: 10.1074/jbc.M200497200. [DOI] [PubMed] [Google Scholar]
- 15.Vabulas RM, et al. The endoplasmic reticulum-resident heat shock protein Gp96 activates dendritic cells via the Toll-like receptor 2/4 pathway. J Biol Chem. 2002;277:20847–20853. doi: 10.1074/jbc.M200425200. [DOI] [PubMed] [Google Scholar]
- 16.Binder RJ. Hsp receptors: the cases of identity and mistaken identity. Curr Opin Mol Ther. 2009;11:62–71. [PubMed] [Google Scholar]
- 17.Korn T, et al. IL-21 initiates an alternative pathway to induce proinflammatory T(H)17 cells. Nature. 2007;448:484–487. doi: 10.1038/nature05970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Binder RJ, Srivastava PK. Peptides chaperoned by heat-shock proteins are a necessary and sufficient source of antigen in the cross-priming of CD8+ T cells. Nat Immunol. 2005;6:593–599. doi: 10.1038/ni1201. [DOI] [PubMed] [Google Scholar]
- 19.Testori A, et al. Phase III comparison of vitespen, an autologous tumor-derived heat shock protein gp96 peptide complex vaccine, with physician’s choice of treatment for stage IV melanoma: the C-100-21 Study Group. J Clin Oncol. 2008;26:955–962. doi: 10.1200/JCO.2007.11.9941. [DOI] [PubMed] [Google Scholar]
- 20.Wood C, et al. C-100-12 RCC Study Group. An adjuvant autologous therapeutic vaccine (HSPPC-96; vitespen) versus observation alone for patients at high risk of recurrence after nephrectomy for renal cell carcinoma: a multicentre, open-label, randomised phase III trial. Lancet. 2008;372:145–154. doi: 10.1016/S0140-6736(08)60697-2. [DOI] [PubMed] [Google Scholar]
- 21.Barnes H, Larsen B, Tyers M, van der Geer P. Tyrosine-phosphorylated low density lipoprotein receptor-related protein 1 (LRP1) associates with the adaptor protein SHC in SRC-transformed cells. J Biol Chem. 2001;276:19119–19125. doi: 10.1074/jbc.M011437200. [DOI] [PubMed] [Google Scholar]
- 22.Willnow TE, Moehring JM, Inocencio NM, Moehring TJ, Herz J. The low-density-lipoprotein receptor-related protein (LRP) is processed by furin in vivo and in vitro. Biochem J. 1996;313:71–76. doi: 10.1042/bj3130071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herz J, Kowal RC, Goldstein JL, Brown MS. Proteolytic processing of the 600 kD low density lipoprotein receptor-related protein (LRP) occurs in a trans-Golgi compartment. EMBO J. 1990;9:1769–1776. doi: 10.1002/j.1460-2075.1990.tb08301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Binder RJ, Karimeddini D, Srivastava PK. Adjuvanticity of alpha 2-macroglobulin, an independent ligand for the heat shock protein receptor CD91. J Immunol. 2001;166:4968–4972. doi: 10.4049/jimmunol.166.8.4968. [DOI] [PubMed] [Google Scholar]
- 25.Bettelli E, Korn T, Oukka M, Kuchroo VK. Induction and effector functions of T(H)17 cells. Nature. 2008;453:1051–1057. doi: 10.1038/nature07036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maeda H, Shiraishi A. TGF-beta contributes to the shift toward Th2-type responses through direct and IL-10-mediated pathways in tumor-bearing mice. J Immunol. 1996;156:73–78. [PubMed] [Google Scholar]
- 27.Veldhoen M, Hocking RJ, Atkins CJ, Locksley RM, Stockinger B. TGFbeta in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity. 2006;24:179–189. doi: 10.1016/j.immuni.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 28.Bettelli E, et al. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- 29.Berwin B, Hart JP, Pizzo SV, Nicchitta CV. Cutting edge: CD91-independent cross-presentation of GRP94(gp96)-associated peptides. J Immunol. 2002;168:4282–4286. doi: 10.4049/jimmunol.168.9.4282. [DOI] [PubMed] [Google Scholar]
- 30.Cam JA, Zerbinatti CV, Li Y, Bu G. Rapid endocytosis of the low density lipoprotein receptor-related protein modulates cell surface distribution and processing of the beta-amyloid precursor protein. J Biol Chem. 2005;280:15464–15470. doi: 10.1074/jbc.M500613200. [DOI] [PubMed] [Google Scholar]
- 31.Hu K, et al. Tissue-type plasminogen activator acts as a cytokine that triggers intracellular signal transduction and induces matrix metalloproteinase-9 gene expression. J Biol Chem. 2006;281:2120–2127. doi: 10.1074/jbc.M504988200. [DOI] [PubMed] [Google Scholar]
- 32.Bu G, Cam J, Zerbinatti C. LRP in amyloid-beta production and metabolism. Ann N Y Acad Sci. 2006;1086:35–53. doi: 10.1196/annals.1377.005. [DOI] [PubMed] [Google Scholar]
- 33.Mantuano E, et al. The hemopexin domain of matrix metalloproteinase-9 activates cell signaling and promotes migration of schwann cells by binding to low-density lipoprotein receptor-related protein. J Neurosci. 2008;28:11571–11582. doi: 10.1523/JNEUROSCI.3053-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mantuano E, Mukandala G, Li X, Campana WM, Gonias SL. Molecular dissection of the human alpha2-macroglobulin subunit reveals domains with antagonistic activities in cell signaling. J Biol Chem. 2008;283:19904–19911. doi: 10.1074/jbc.M801762200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Caceres LC, Bonacci GR, Sanchez MC, Chiabrando GA. Activated alpha2-macroglobulin induces matrix metalloproteinase 9 expression by low density lipoprotein receptor-related protein 1 through MAPK-ERK1/2 and NF-kappaB activation in macrophage derived cell lines. J Cell Biochem. 2010;111:607–617. doi: 10.1002/jcb.22737. [DOI] [PubMed] [Google Scholar]
- 36.Li Y, Marzolo MP, van Kerkhof P, Strous GJ, Bu G. The YXXL motif, but not the two NPXY motifs, serves as the dominant endocytosis signal for low density lipoprotein receptor-related protein. J Biol Chem. 2000;275:17187–17194. doi: 10.1074/jbc.M000490200. [DOI] [PubMed] [Google Scholar]
- 37.Trommsdorff M, Borg JP, Margolis B, Herz J. Interactions of cytosolic adaptor proteins with neuronal apolipoprotein E receptors and the amyloid precursor protein. J Biol Chem. 1998;273:1031–1039. doi: 10.1074/jbc.273.50.33556. [DOI] [PubMed] [Google Scholar]
- 38.Trommsdorff M, et al. Reeler/Disabled-like disruption of neuronal migration in knockout mice lacking the VLDL receptor and ApoE receptor 2. Cell. 1999;97:689–701. doi: 10.1016/s0092-8674(00)80782-5. [DOI] [PubMed] [Google Scholar]
- 39.Gotthardt M, et al. Interactions of the low density lipoprotein receptor gene family with cytosolic adaptor and scaffold proteins suggest diverse biological functions in cellular communication and signal transduction. J Biol Chem. 2000;275:25616–25624. doi: 10.1074/jbc.M000955200. [DOI] [PubMed] [Google Scholar]
- 40.Boucher P, et al. Platelet-derived growth factor mediates tyrosine phosphorylation of the cytoplasmic domain of the low Density lipoprotein receptor-related protein in caveolae. J Biol Chem. 2002;277:15507–15513. doi: 10.1074/jbc.M200428200. [DOI] [PubMed] [Google Scholar]
- 41.Guttman M, et al. Interactions of the NPXY microdomains of the low density lipoprotein receptor-related protein 1. Proteomics. 2009;22:5016–5028. doi: 10.1002/pmic.200900457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen JS, et al. Secreted heat shock protein 90alpha induces colorectal cancer cell invasion through CD91/LRP-1 and NF-kappaB-mediated integrin alphaV expression. J Biol Chem. 2010;285:25458–25466. doi: 10.1074/jbc.M110.139345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collart MA, Baeuerle PA, Vassalli P. Regulation of tumor necrosis factor alpha transcription in macrophages: involvement of four κB-like motifs and of constitutive and inducible form of NF-κB. Mol Cell Biol. 1990;10:1498–1506. doi: 10.1128/mcb.10.4.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shakhov AN, Collart MA, Vassalli P, Nedospasov SA, Jongeneel CV. κB-type enhancers are involved in lipopolysaccharide-mediated transcriptional activation of the tumor necrosis factor α gene in primary macrophages. J Exp Med. 1990;171:35–47. doi: 10.1084/jem.171.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Libermann TA, Baltimore D. Activation of interleukin-6 gene expression through the NF-κB transcription factor. Mol Cell Biol. 1990;10:2327–2334. doi: 10.1128/mcb.10.5.2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Voraberger G, Schafer R, Stratowa C. Cloning of the human gene for intercellular adhesion molecule 1 and analysis of its 5′-regulatory region: induction by cytokines and phorbol ester. J Immunol. 1991;147:2777–2786. [PubMed] [Google Scholar]
- 47.Azzolina A, Bongiovanni A, Lampiasi N. Substance P induces TNF-alpha and IL-6 production through NF kappa B in peritoneal mast cells. Biochim Biophys Acta. 2003;1643:75–83. doi: 10.1016/j.bbamcr.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 48.Kalesnikoff J, et al. Ship negatively regulates IgE+antigen-induced IL-6 production in mast cells by inhibiting NF-kappa B activity. J Immunol. 2002;168:4737–4746. doi: 10.4049/jimmunol.168.9.4737. [DOI] [PubMed] [Google Scholar]
- 49.Martin-Orozco, et al. T helper 17 cells promote cytotoxic T cell activation in tumor immunity. Immunity. 2009;31:787–798. doi: 10.1016/j.immuni.2009.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stebbing J, et al. The heat-shock protein receptor CD91 is up-regulated in monocytes of HIV-1-infected “true” long-term nonprogressors. Blood. 2003;101:4000–4004. doi: 10.1182/blood-2002-11-3353. [DOI] [PubMed] [Google Scholar]
- 51.Navaratnam M, Deshpande MS, Hariharan MJ, Zatechka DS, Jr, Srikumaran S. Heat shock protein-peptide complexes elicit cytotoxic T-lymphocyte and antibody responses specific for bovine herpesvirus 1. Vaccine. 2001;19:1425–1434. doi: 10.1016/s0264-410x(00)00381-9. [DOI] [PubMed] [Google Scholar]
- 52.Chandawarkar RY, Wagh MS, Srivastava PK. The dual nature of specific immunological activity of tumor-derived gp96 preparations. J Exp Med. 1999;189:1437–1442. doi: 10.1084/jem.189.9.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu Z, et al. Treg suppress CTL responses upon immunization with HSP gp96. Eur J Immunol. 2009;39:3110–3120. doi: 10.1002/eji.200939593. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.