Abstract
Objectives
To use the theory of planned behavior to identify predictors of intentions to use cessation aids when quitting smoking.
Methods
African American smokers completed a survey to assess intentions, attitudes, and normative and control beliefs regarding the use of smoking cessation aids.
Results
Participants held mildly positive attitudes regarding the use of cessation aids. Beliefs related to the utility of aids, support of referents, and accessibility of a doctor were most strongly associated with intention to use cessation aids.
Conclusions
African American smokers may be amenable to the use of cessation aids, and specific beliefs may be targets for intervention.
Keywords: theory of planned behavior, smoking cessation, cessation aids
Smoking is the cause of over $100 billion in health care costs annually and accounts for approximately 443,000 deaths each year.1 Although the prevalence of smoking among African Americans is very similar to that of whites (currently 21% for both groups),2 African Americans experience a greater risk for tobacco-related morbidity and mortality.3,4 Studies also indicate that although African Americans have more quit attempts in a given year when compared to whites,5,6 they are much less likely to succeed in quitting.7,8
Although many biopsychosocial factors likely contribute to lower quitting success among African American smokers, one reason may be lower use of pharmacotherapy to aid in cessation attempts. Although pharmacotherapy has been shown to increase cessation success,9 there is evidence that pharmacotherapy is generally underused across all racial groups.10,11 However, studies of nicotine replacement use indicate that African Americans have even lower use rates (10–20%) when compared to those of whites (29–34%).6,10,12–18 In general, reasons for underuse include cost, lack of knowledge regarding efficacy,19 concerns about safety, and a perceived lack of access.20 However, whether similar or different reasons account for underuse by African Americans has not received much attention.
One qualitative study examined several ethnic minorities’ attitudes and beliefs about pharmacotherapy.21 Results revealed that, similar to findings from previous studies of mostly white smokers, African American smokers (n = 26) were aware of the existence of cessation pharmacotherapy but were not knowledgeable regarding the specific benefits for cessation, such as reduced cravings and withdrawal symptoms. In addition, many smokers were skeptical of the effectiveness of all forms of cessation pharmacotherapy and were particularly reluctant to accept a medication in pill form. African American participants also reported believing that the side effects of all cessation aids would likely be worse than the health effects of smoking.
The generalizability of these qualitative results to most African American smokers is unknown. Furthermore, Fu and colleagues21 did not determine which beliefs among those identified would be most significant in influencing participant decision making about the use of pharmacotherapy. Given the importance of increasing cessation among African American smokers and the dearth of research in this area, there is a need to extend this qualitative work to address these limitations.
Examining Pharmacotherapy Use Using the Theory of Planned Behavior
In this study, we used a theoretically driven, quantitative approach to examine attitudes and beliefs related to pharmacotherapy use for smoking cessation among African American smokers.
Constructs examined were drawn from the theory of planned behavior (TPB) which have been used extensively in health behavior studies,22,23 including in studies of smoking behavior.24 According to the TPB, and consistent with meta-analyses of TPB studies,25 intentions are the proximal cause of volitional behavior.26 Intention is determined by attitude towards the behavior, subjective norm, and perceived behavioral control. Attitude toward the behavior is a function of behavioral beliefs regarding the anticipated outcomes of a behavior and the value placed on these outcomes (outcome evaluations). Subjective norm is a function of individuals’ beliefs about whether others important to them (referents) want them to engage in the behavior (normative beliefs), and the individual’s degree of motivation to comply with referent opinions. Perceived behavioral control is a function of control beliefs about the extent of personal control over a behavior (eg, opportunities/resources and barriers/impediments likely to facilitate/hinder the behavior) and an evaluation of how strongly the behavior is likely to be affected by the facilitating/hindering factors (perceived power).
According to the TPB, in order to determine key predictors of intention it is first necessary to conduct elicitation interviews to identify the specific behavioral beliefs, normative referents, and control beliefs relevant to the particular population and target behavior in question. This is followed by a quantitative assessment of beliefs that might predict the behavior and/or the intention to engage in the behavior. In order to build on the work of Fu et al,21 we used the theoretical constructs of the TPB to identify the beliefs of African American smokers regarding the use of smoking cessation aids in a smoking quit attempt. Specifically, we developed and administered a TPB-based questionnaire to a sample of inner-city African American smokers, tested the TPB model, and identified key predictors of intention to use pharmacotherapy. Because we thought it possible that predictors might differ for intention to use nicotine replacement versus oral agents (ie, bupropion and varenicline), we examined predictors for each type of medication independently.
METHOD
Participants
Participants were recruited from the lobby of an urban outpatient health center that serves a predominantly African American community in the spring of 2009. Participants were eligible if they identified as African American or black, smoked at least 5 cigarettes per day (to ensure the relevance of using cessation aids), and had a telephone number for follow-up contact. In order to ensure that participants could meaningfully consider the manner in which they would quit smoking should they decide to do so, participants were excluded if they indicated that they were not interested in quitting during the next 6 months or if they had only started smoking within the last 30 days. Of those screened, more than 90% were eligible and agreed to participate. Although 200 participants were enrolled, one participant was found to have completed the survey twice so that the number of participants analyzed was 199. Participants received $5 in cash to compensate them for their time. This study was approved by the human subjects institutional review board at the University of Missouri-Kansas City.
Measures
Demographics and smoking characteristics
Demographic measures included age, number of years smoked, income, and education level. Smoking characteristics included cigarettes smoked per day, nicotine dependence level as assessed using the Fagerstrom Test for Nicotine Dependence (FTND),27 previous use of smoking cessation aids, and number of previous quit attempts.
TPB constructs
Questionnaire items were developed for each of the TPB constructs of interest (ie, behavioral intent, attitude, subjective norm, perceived behavioral control, behavioral beliefs, behavioral outcomes, normative beliefs and motivation to comply, and control belief and perceived power) using established TPB scaling methods.22 Survey item content (ie, specific outcome beliefs, specific control beliefs, specific referents) was based primarily on a review of the focus group results reported by Fu et al21 and supplemented with items we thought might be relevant. Two sets of measures were created with one focused on use of nicotine replacement therapy and one focused on the use of oral cessation medications. Prior to use in the study the instrument was pilot tested with 10 volunteers recruited in the same manner as the study participants.
TPB Outcome Variables
Intention to use cessation aids was measured with a single item--“I plan to use [nicotine replacement therapy/oral cessation medications] in the next 6 months”-- rated on a 7-point scale (1=Likely, 7 = Unlikely).
TPB Higher Order Constructs
Measures of the constructs used to predict intention (ie, attitude, social norms, and perceived control) were obtained by means of semantic differential, 7-point scales scored −3 to +3, as suggested by Ajzen and Fishbein.18 For assessment of attitude, participants rated 7 items (scored +3 to −3) to indicate whether “My using (Nicotine Replacement Therapy/Oral cessation medications such as Zyban or Chantix) is” (wise/unwise), (easy/difficult), (safe/dangerous), (enjoyable/unenjoyable), (beneficial/harmful), (like/dislike), (good/bad). Internal consistency was calculated for the attitude measure for both NRT and OCM (α= .863 and .913, respectively). For assessment of subjective norm, participants rated 2 items (scored +3 to −3) to indicate whether “Most people important to me think I (should/should not) use (Nicotine Replacement Therapy/pills like Zyban or Chantix) to help me quit smoking” and whether “People I respect and admire (do/do not) want me to use (Nicotine Replacement Therapy/pills like Zyban or Chantix) to help me quit smoking”. For perceived behavioral control, participants rated whether “Using (Nicotine Replacement Therapy/pills like Zyban or Chantix) to quit smoking is (up/not up) to me” (scored +3 to −3).
TPB Primary Level Constructs
Individual behavioral beliefs and corresponding outcome evaluations were measured using bipolar 7-point semantic differential scales. For each behavioral belief (eg, “Using NRT will help me to quit smoking”), participants rated how likely or unlikely the outcome was (scored from +3 to −3) and for each corresponding outcome evaluation participants rated whether the outcome (eg, “Quitting smoking…”) was good/bad (scored from +3 to −3). There were 10 behavioral belief/outcome evaluation pairs that were used for both nicotine replacement and oral cessation medications and an additional behavioral belief/outcome evaluation pair (“If I use NRT I will still be addicted to nicotine”) used only for NRT (see Table 3).
Table 3.
Behavioral Belief Strength, Outcome Evaluation, and Correlation With Intention to Use Medication (N=199)
| Behavioral Beliefs | Belief strength
|
Outcome evaluation
|
Intentiona |
||
|---|---|---|---|---|---|
| M | SD | M | SD | r | |
| NRT will help me to quit smoking. | 1.05 | 1.78 | 2.41 | 1.35 | .273** |
| OCM will help me to quit smoking. | .61 | 1.92 | 2.41 | 1.35 | .466** |
| NRT will be effective in helping me to quit. | .82 | 1.91 | 2.41 | 1.35 | .354** |
| OCM will be effective in helping me to quit. | .79 | 1.82 | 2.41 | 1.35 | .508** |
| NRT will help lower my cravings to smoke. | 1.28 | 1.75 | 1.96 | 1.63 | .294** |
| OCM will help lower my craving to smoke. | .80 | 1.83 | 1.96 | 1.63 | .305** |
| NRT will help lower my withdrawal symptoms. | 1.20 | 1.77 | 1.68 | 1.81 | .105 |
| OCM will help lower my withdrawal symptoms. | .75 | 1.84 | 1.68 | 1.81 | .225** |
| NRT will cause serious side effects. | −.33 | 1.84 | −2.16 | 1.45 | .120 |
| OCM will cause serious side effects. | −.32 | 1.93 | −2.16 | 1.45 | −.064 |
| NRT will cause side effects that are worse than the effects of smoking. | −.55 | 1.86 | −.97 | 1.96 | .074 |
| OCM will cause side effects that are worse than the effects of smoking. | −.38 | 1.76 | −.76 | 1.86 | .135 |
| NRT will cost a lot of money. | .34 | 2.03 | −2.02 | 1.54 | −.051 |
| OCM will cost a lot of money. | .47 | 1.92 | −2.02 | 1.54 | .145* |
| NRT is available to me. | .66 | 2.06 | 1.72 | 1.68 | .071 |
| OCM is available to me. | .35 | 2.12 | 1.36 | 1.82 | .045 |
| If I use NRT to quit smoking I will feel like I used a crutch. | −.58 | 2.09 | −.58 | 2.09 | −.101 |
| If I use OCM to quit smoking I will feel like I used a crutch. | −.30 | 2.00 | −.58 | 2.09 | .080 |
| Using NRT will alter my mind. | −.53 | 2.04 | −.91 | 2.25 | .125 |
| Using OCM will alter my mind. | −.45 | 1.88 | −.91 | 2.25 | .258** |
| If I use NRT I will still be addicted to nicotine. | −.77 | 1.93 | −2.33 | 1.38 | .213** |
Correlations in this column represent the result of correlating the product of each specific belief strength score and its corresponding outcome evaluation score with the overall intention to use either NRT or OCM
All behavioral beliefs and outcome evaluation possible means ranged from −3 to 3
NRT = nicotine replacement therapy; OCM = oral cessation medications
P<.05
P<.01
Six normative beliefs and corresponding motivation to comply ratings were measured for both NRT and oral cessation medications using bipolar 7-point semantic differential scales. For normative beliefs, participants responded to 6 items rating the extent to which they thought their boyfriend/girlfriend/husband/wife, friends, pastor, family, doctor, and God thought they (should/should not) use oral cessation medications or nicotine replacement therapy (scored from +3 to −3) to help them quit smoking. For each normative referent, participants indicated the extent (from 1 to 7) to which they were motivated to comply with the referent (ie,“do not want to do/want to do what my [referent] thinks I should do”).
Six control beliefs and corresponding perceived power ratings were measured for both NRT and oral cessation medications using bipolar 7-point semantic differential scales. For control beliefs, participants rated 6 items indicating the extent to which access to a doctor, access to a pharmacy, sufficient money, support from those around them, taking it as prescribed, not having too much stress (rated from not at all true to very true; −3 to +3) was necessary or important to using NRT/oral cessation medications (eg, “To use NRT one needs access to a doctor”). For perceived power, participants rated the extent to which each of these potential barriers/facilitators would be difficult/easy to achieve or overcome (scored from −3 to +3).
Procedures
Participants who were interested in participating completed informed consent. To increase the likelihood that participants were aware of the cessation aids in question, participants were shown pictures of each item prior to survey administration and encouraged to ask questions if anything was unclear. Approximately 5 participants asked questions related to understanding vocabulary and the scaling of the items. Upon completion of the survey, participants were reimbursed with $5 in cash. Participants also consented to a 6-months follow-up survey to assess actual medication use. However, at the 6-month follow-up less than 20% of participants were reached when called using the contact information provided. Therefore, analyses concerning medication use were aborted.
Analyses
Analyses were conducted using SPSS 16 and AMOS 16.28 Analyses followed the steps described by Davis and colleagues.29 First the applicability of the TPB for predicting intention to use pharmacotherapy for smoking cessation was examined. Second, the correlation of each behavioral, normative, and control belief with intention to use pharmacotherapy was examined.
Validity of the TPB models
The same sets of analyses were conducted for each target behavior (ie, intention to use nicotine replacement therapy and intention to use oral cessation medications). The first step examined the association between the higher order construct measures (ie, direct measures of attitude, subjective norm, and perceived control) and intention to use medication. This analysis was conducted using path analysis.28 Direct paths were specified from attitude, subjective norm, and perceived behavioral control to intention. Attitude, subjective norm, and perceived behavioral control were allowed to covary. In addition to calculating chi-square, fit was assessed using a number of additional fit indices including goodness of fit (GFI), adjusted goodness of fit (AGFI), and root mean square error of approximation (RMSEA). Acceptable values for these indices include a value of .95 or higher for CFI, a value of .07 or less for RMSEA, and a nonsignificant chi-square.
The second step was to evaluate whether the primary level components (ie, the specific behavioral, normative, and control beliefs) were correlated with their respective higher order constructs (attitude, subjective norm, and perceived control). This was accomplished by examining the correlation between each direct measure (eg, attitude) with the summed products of the corresponding primary level components (eg, behavioral beliefs and corresponding outcome expectations). A moderate correlation (.4–.6) was considered indicative of a good fit between the primary level and higher order constructs.21
Predictors of intention
The final set of analyses examined the correlation between each primary level component with behavioral intention to determine which individual beliefs were significant in predicting cessation aid use. In these analyses, the product of each primary level construct pair (eg, a particular behavioral belief and its corresponding outcome expectation rating) was correlated with intention.
RESULTS
Validity of the TPB Models
Demographics and smoking characteristics are displayed in Table 1.
Table 1.
Smoking and Demographic Variables (N=199)
| Variable | Mean | SD | % |
|---|---|---|---|
| Age | 44.2 | 10.7 | |
| Cigarettes per day | 12.5 | 7.5 | |
| Quit attempts in the last year a | 4.4 | 5.6 | |
| Years smoked | 21.1 | 11.3 | |
| Motivation to quit (out of 10) | 8.4 | 2.0 | |
| FTND b | 5.4 | 2.1 | |
| Gender (male) | 58.3 % | ||
| High school graduate (or less) | 72.4% | ||
| Income (household less than $900 per month) | 74.9% | ||
| Employed full or part time | 19.6% | ||
| Previous Nicotine Replacement Therapy use | 20.7% | ||
| Previous oral cessation medication use | 9.2% |
Median quit attempts in last year is 3.0.
The Fagerstrom Test of Nicotine Dependence is an indication of level of dependence on nicotine, and scores range from 0–10, with a level of 10 indicating a higher level of nicotine dependence.
Means, standard deviations, and intercorrelations between the primary level constructs are displayed in Table 2. Correlations between all constructs within each behavioral domain (ie, NRT and oral cessation medications) were all significant with the strongest associations emerging between the attitude and intention measures.
Table 2.
Intercorrelations Between Variables (N=199)
| Variable | M | SD | Correlations
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| 1) Attitude (NRT) | 1.24 | 1.31 | - | ||||||
| 2) Attitude (OCM) | 1.14 | 1.42 | .77* | - | |||||
| 3) Subjective Norm (NRT) | 1.39 | 1.69 | .41* | .38* | - | ||||
| 4) Subjective Norm (OCM) | 1.25 | 1.77 | .43* | .43* | .73* | - | |||
| 5) Perceived Behavioral Control (NRT) | 6.14 | 1.48 | .23* | .22* | .21* | .38* | - | ||
| 6) Perceived Behavioral Control (OCM) | 6.10 | 1.51 | .26* | .26* | .22* | .37* | .76* | - | |
| 7) Intention to use (NRT) | 4.93 | 1.92 | .48* | .45* | .22* | .34* | .33* | .35* | - |
| 8) Intention to use (OCM) | 4.59 | 1.96 | .44* | .57* | .11 | .33* | .21* | .35* | .67* |
P<.01
The means for variables 1–4 could range from −3 to 3; the means for variables 5–8 could range from 1 to 7.
NRT = nicotine replacement therapy, OCM = oral cessation medication.
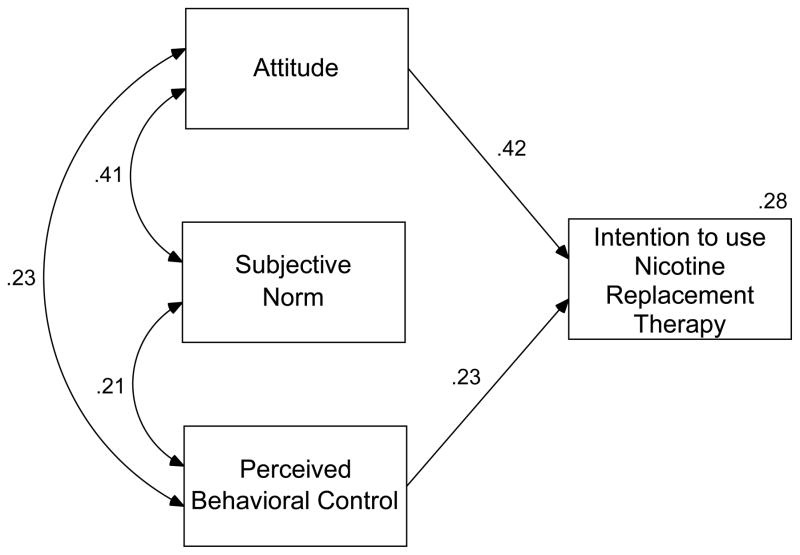
Path analysis: NRT
The fit for the proposed model for NRT was inconclusive as the model was saturated (parameters estimated equals observed variables), χ2 (0) = 0.0, P = not computable, CFI = 1.0, RMSEA = .230. However, all specified paths were significant except subjective norm to intention. Therefore, a second model was run in which the path from subjective norm to intention was excluded (see Figure 1). This second model had very good fit, χ2(1)= 0.1, P = .978, CFI = 1.0, RMSEA = .000; and all paths were significant (all P’s <.01). Together, these models accounted for 28% of the variance in intention to use NRT.
Figure 1.
Theory of Planned Behavior Model Predicting Intention to Use Nicotine Replacement Therapy
All associations are significant at the P < .01 level
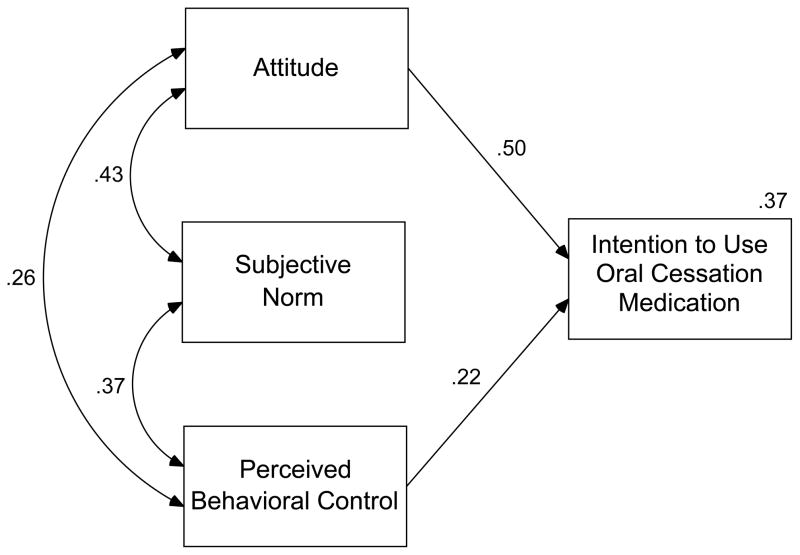
Oral cessation medications
Results for the proposed model for oral cessation medications were similar to those of the model for NRT. The model was again saturated, and all specified paths were significant except the path from subjective norm to intention. A second model (see Figure 2) in which the path from subjective norm to intention was excluded had very good fit, χ2(1)= 0.110, P = .740, CFI = 1.0, RMSEA = .000; and all paths were significant (all P’s <.01). Together, these models accounted for 37% of the variance in intention to use oral cessation medications.
Figure 2.
Theory of Planned Behavior Model Predicting Intention to Use Oral Cessation Medications
All associations are significant at the P < .01 level
Additional regression models were conducted to further explore the nonsignificance of subjective norm as a predictor of intention. Results indicated that for both NRT and oral cessation medication models, subjective norm was a significant predictor on its own, but became nonsignificant when attitude and perceived behavioral control were included as predictors.
The second step in establishing the applicability of the TPB was to examine whether the primary level beliefs (ie, behavioral beliefs and corresponding outcome evaluations, normative beliefs and corresponding motivation to comply, and control beliefs and corresponding perceived power) correlated with their corresponding higher order constructs (ie, attitude, subjective norm, and perceived control, respectively). The correlation between the direct measures of attitude towards using either NRT or oral cessation medication and the summed products of corresponding behavioral beliefs and outcome evaluations was .56 (P <.01) and .53 (P <.01), respectively. The correlation between the direct measure of subjective norm for using either NRT or oral cessation medication and the summed products of the 6 normative beliefs and motivation to comply was .53 (P < .01) and .61 (P < .01), respectively. The correlations between the direct measure of perceived behavioral control for intention to use either NRT or oral cessation medication and the summed products of control beliefs multiplied by perceived power were not significant.
Predictors of Intention
The final set of analyses examined the association between each of the specific beliefs underlying attitude, subjective norm, and perceived control and intention to use.
Behavioral beliefs × outcome evaluation
As shown in Table 3, with the exception of “using NRT/oral cessation medications will cost a lot of money,” all beliefs were favorable toward the use of medication as indicated by the magnitude (.33 to 1.28 out of 3) and direction of the belief strength means relative to zero (positive indicating agreement and negative indicating disagreement) and the direction (positive versus negative) of the corresponding outcome evaluation.
Table 3 also shows the correlation between the product of the belief strength and its corresponding outcome evaluation and intention to use pharmacotherapy. Beliefs that the medication was helpful, effective, and would lower cravings were significantly related to greater intentions to use for both types of medication (all P’s < .01). For NRT, the belief that one would still be addicted to nicotine was also related to greater intention (P < .01). For oral cessation medications, beliefs that medications would lower withdrawal symptoms, be mind-altering, and cost a lot were also significantly related to greater intention (all P’s < .05).
Normative belief × motivation to comply
Although subjective norm was not an independent predictor of intention in the SEM model, we nevertheless examined the underlying normative referent beliefs. As can be seen in Table 4, all belief strength means were greater than zero, and motivation to comply was greater than 5 out of 7. This indicated that most participants believed that all normative referents were in favor of their using NRT or oral cessation medications when attempting to quit smoking and that they were generally motivated to comply. The correlation of the product of each normative referent belief and the corresponding motivation to comply with intention to use NRT and oral cessation medication revealed that with the exception of the belief/motivation to comply for significant other and NRT use, beliefs related to all referents were significantly related to intention to use (all P’s <. 01).
Table 4.
Normative Referent Belief Strength, Motivation to Comply, and Correlation With Intention to Use Medication (N=199)
| Normative referent (use behavior) | Belief strength
|
Motivation to comply
|
Intentiona |
||
|---|---|---|---|---|---|
| M | SD | M | SD | r | |
| Significant other (use NRT) | .77 | 2.27 | 5.30 | 2.00 | .018 |
| Significant other (use OCM) | .04 | 2.14 | 5.30 | 2.00 | .238** |
| Friend (use NRT) | .94 | 2.06 | 5.33 | 2.06 | .201** |
| Friend (use OCM) | .92 | 1.97 | 5.33 | 2.06 | .372** |
| Pastor (use NRT) | 1.08 | 2.02 | 5.68 | 1.75 | .264** |
| Pastor (use OCM) | 1.03 | 2.07 | 5.68 | 1.75 | .254** |
| Family(use NRT) | 1.41 | 1.96 | 5.77 | 1.78 | .270** |
| Family (use OCM) | 1.19 | 1.94 | 5.77 | 1.78 | .327** |
| Doctor(use NRT) | 1.61 | 1.84 | 5.95 | 1.65 | .280** |
| Doctor (use OCM) | 1.12 | 2.06 | 5.95 | 1.65 | .273** |
| God (use NRT) | 1.20 | 2.14 | 5.97 | 1.69 | .276** |
| God (use OCM) | 1.22 | 2.15 | 5.97 | 1.69 | .237** |
Intention to use nicotine replacement therapy or oral cessation medications is correlated with the product of belief strength for each normative referent and its corresponding degree of motivation to comply.
NRT = nicotine replacement therapy, OCM = oral cessation medications
P<.05
P<.01
Control belief × perceived power
Although the individual control beliefs assessed did not correlate significantly with the direct measure of perceived control, we examined the underlying individual control beliefs as predictors of intention. Mean scores for each of the control beliefs were positive, indicating agreement with each belief; however, perceived power associated with the control belief varied from positive to negative (easy to difficult to overcome). However, for both NRT and oral cessation medications, only control beliefs about access to a doctor and the need to take medications as prescribed were predictive of intention. For oral cessation medications, the control belief that one needs enough money was also significant.
Discussion
The path analyses for both NRT and oral cessation medications revealed that the TPB model was a good fit for the data with the exception that subjective norm was not a significant predictor of intention. Additional analyses showed that this was likely due to subjective norm’s overlap with attitude and perceived behavioral control. The amount of variance explained by the models (ie, 28% for NRT and 37% for oral cessation medications) is in the same range (~39%) as those of other studies that have used the TPB.30 Overall the results suggested that the TPB model was useful and generalizable to this population of African American smokers for predicting intention to use cessation aids.
The associations between the primary level and higher order variables, for both NRT and oral cessation medications, revealed that attitude and subjective norm were good representations of individual beliefs, but perceived behavioral control was not. One possible explanation for this finding is that not all primary level control beliefs were correctly identified. The control beliefs were primarily based on the themes identified by Fu et al21; however, it is possible that there are other important control beliefs that did not emerge during these focus groups that might better account for smokers’ perceived control over medication use. For example, individuals may hold beliefs that acquiring cessation aids is difficult because of transportation or managing other life priorities that we did not assess. More work is needed to identify the key control beliefs that account for African American smokers’ perceived control for using smoking cessation aids.
The overall results were also very similar for NRT and oral cessation medications. This is in contrast to the focus group findings of Fu et al,21 which indicated that smokers made a clear distinction in their beliefs between NRT and oral cessation medications.
Examination of Individual Beliefs
One of the biggest values in using the TPB is that it allows examination of the individual beliefs that may be important for determining intention and actual behavior. In our study, mean scores indicated that there was an overall slightly positive perception of cessation aids. On average, participants responded that they believed that cessation aids would be useful in helping them to quit, would not cause negative side effects, and most of their significant referents would approve of their using cessation aids. This overall positive perspective is encouraging and contrasts with the results of the focus groups that indicated that African American smokers are generally wary of the effectiveness of cessation aids, think they will cause bad side effects and many people in their life would not find them useful in quitting.21 Nevertheless, the ratings also indicate that there is ample room for increasing the strength of positive beliefs about cessation aids.
With respect to the individual behavioral beliefs that best distinguish smokers differing in intention to use aids, those who believed that cessation aids would have utility in helping with cessation were more likely to intend to use them. Smokers who believed that cessation aids could help them to quit, would be effective in helping them to quit, and would reduce cravings were more likely to intend to use such aids. In addition, for oral cessation medications, the belief that they would reduce withdrawal symptoms was also significantly associated with intention to use them. These findings were consistent with general population studies that indicate that beliefs about medication efficacy is a key issue in medication use.19
There were also beliefs about potential problems with cessation aids that were significantly associated with intentions. Smokers who endorsed the belief that NRT would continue their addiction to nicotine were less likely to intend to use NRT. This is consistent with Fu et al’s21 qualitative data that indicated that many smokers thought that they would remain addicted to nicotine by using NRT products. Similarly, smokers who believed that oral cessation medications would alter their mind were also less likely to intend to use them. Although safety concerns have also been identified as a problem in the general population,19 this latter concern may relate to the well-documented general distrust of medicine and research by African Americans.31 It may also account for Fu et al’s21 finding that oral cessation medications were seen as different from and more dangerous than NRT.
In addition, the belief that oral cessation medications would be cost prohibitive was significantly associated with intentions to use. Perceived cost has been identified as a barrier for NRT use in the general population of smokers.19 However, among African Americans in the current study, it appears that cost concerns were focused on oral cessation medications rather than NRT. These beliefs are consistent with the higher cost of oral cessation medications and highlights the potential importance of subsidizing the cost of effective medications (whether through insurance coverage or other methods) to increase uptake.
Regarding normative beliefs, our list of referents included “pastor’ and “God’s will” because we believed these might be particularly salient referents among African Americans.32 Results indicated that smokers on average perceived normative referents to be in favor of their using cessation aids. Importantly, except for the “significant other” referent for NRT, all referent beliefs (including their pastor and God) were predictive of intention to use cessation aids. This suggests that interventions to enhance medication could target all of these referents to increase the likelihood that smokers will encourage medication use.
Regarding control beliefs, perceived ability to see a doctor, to take medications as prescribed, and the affordability of medications were most strongly predictive of intention to use cessation aids. These perceived control predictors are consistent with well-established predictors of poor health outcomes among African Americans33 and highlight yet another way in which these traditional barriers may impact health (ie, through perceived lack of control to use cessation aids).
General Implications
Previous use of NRT among African Americans in this study was somewhat lower than in other studies. Use was 20.7%, compared to 25% to 40% from previous studies of the general population.10,34 Our findings, though based on a convenience sample, suggest oral cessation medication use is much lower (9%). This information appears to confirm the need to increase use of NRT and oral cessation medications among this population for smoking cessation. Although our findings suggest that, in general, similar beliefs related to utility can be targeted for NRT and oral cessation medications, they also indicate that interventions targeting African Americans may need to address specific concerns about addiction to nicotine from NRT and the potential psychological side effects and cost associated with oral cessation medications. Providing more information on the potential for oral cessation medications to lower withdrawal symptoms may address a crucial gap in knowledge about the way oral cessation medications work. Finally, the results suggest the TPB and theory-based approach may be useful for understanding reduced use of cessation aids in underserved populations.
Limitations
Our reliance on the themes identified by Fu et al21 to develop item content rather than conducting elicitation interviews with African American smokers in the community in which we conducted the survey may have led us to fail to assess beliefs that are important for predicting intention. In addition, because we followed the TPB approach and developed novel measures for this study, we were not able to use established reliable and valid measures. Nevertheless, our final TPB model was a good fit, increasing confidence in the findings.
Another study limitation was that the participant’s smoking status was not biochemically verified. There is the possibility that some participants were not smokers and participated only for the small cash incentive. It is also important to recognize that our failure to successfully assess medication use among our participants at follow-up resulted in models based on intention to use rather than actual use. Confirming the present results with use behavior as the outcome is an important next step. Caution is also warranted in generalizing these findings. Although a strength of the study was its focus on an underserved population, the results may not apply to other African American communities or settings (particularly those of higher income than this lower income sample), nonoutpatient samples, or smokers from other ethnic groups.
Conclusion
In spite of these limitations, the results provide preliminary evidence that African American smokers may be amenable to the use of smoking cessation aids. The findings also point to a number of key attitudes and beliefs that may be valuable intervention targets for future intervention research studies or social marketing and advertising campaigns.
Table 5.
Control Belief Strength, Perceived Power, and Correlation With Intention to Use Medication (N=199)
| Control beliefs | Belief strength | Perceived power | Intentiona | ||
|---|---|---|---|---|---|
| M | SD | M | SD | r | |
| To use NRT one needs access to a doctor. | .41 | 2.24 | .92 | 2.15 | .157* |
| To use OCM one needs access to a doctor. | .73 | 2.08 | .92 | 2.15 | .164* |
| To use NRT one needs access to a pharmacy. | .21 | 2.25 | 1.02 | 2.04 | .042 |
| To use OCM one needs access to a pharmacy. | .55 | 2.03 | 1.02 | 2.04 | .035 |
| To use NRT one needs enough money. | .41 | 2.15 | −1.15 | 1.87 | .125 |
| To use OCM one needs enough money. | .68 | 1.97 | −1.15 | 1.87 | .218** |
| To use NRT one needs the support of those around them. | .83 | 2.18 | .65 | 1.98 | .066 |
| To use OCM one needs the support of those around them. | .95 | 1.95 | .65 | 1.98 | .109 |
| It is important to take NRT as prescribed. | 1.52 | 1.87 | 1.20 | 1.82 | .268** |
| It is important to take OCM as prescribed. | 1.49 | 1.73 | 1.11 | 1.84 | .242** |
| To use NRT one needs to not have too much Stress. | .60 | 2.05 | −.47 | 1.90 | −.118 |
| To use OCM one needs to not have too much Stress. | .57 | 1.96 | −.47 | 1.90 | −.031 |
Intention to use nicotine replacement therapy or oral cessation medications is correlated with the product of the strength for each control belief and the corresponding degree of perceived power.
NRT = nicotine replacement therapy, OCM = oral cessation medications
P<.05
P<.01
Acknowledgments
The authors would like to thank Swope Health Services and the patients who volunteered to participate for making this study possible. This research was partially supported by grant R01 CA133068 from the National Cancer Institute.
Contributor Information
Ian Lynam, Department of Psychology, University of Missouri-Kansas City, 5100 Rockhill Road, Kansas City, MO 64110, 816-235-1318.
Delwyn Catley, Department of Psychology, University of Missouri-Kansas City, 5100 Rockhill Road, Kansas City, MO 64110, 816-235-1073.
Kari Jo Harris, School of Public and Community Health Sciences, The University of Montana, Missoula, MT 59812, 406-243-4685.
Kathy Goggin, Department of Psychology, University of Missouri-Kansas City, 5100 Rockhill Road, Kansas City, MO 64110, 816-235-1059.
Jannette Berkley-Patton, Department of Psychology, University of Missouri-Kansas City, 5100 Rockhill Road, Kansas City, MO 64110, 816-235-6362.
Janet Thomas, University of Minnesota, Division of General Internal, Medicine, MMC 741, 420 Delaware Street SE, Minneapolis, MN 55455, 612-625-0414.
References
- 1.CDC State-specific smoking attributable mortality and years of potential life lost-United States, 2000–2004. MMWR. 2009;58:29–33. [PubMed] [Google Scholar]
- 2.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. National Center for Health Statistics. Vital Health Stat. 2010;10(249):10–11. [PubMed] [Google Scholar]
- 3.USDHHS. Tobacco Use Among U.S. Racial/Ethnic Minority Groups — African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General. MMWR. 1998;47:1–16. [PubMed] [Google Scholar]
- 4.American Cancer Society. Cancer Facts and Figures for African Americans 2007–2008. American Cancer Society; 2007. [Google Scholar]
- 5.Fiore MC, Novotny TE, Pierce JP, et al. Trends in cigarette smoking in the United States. The changing influence of gender and race. JAMA. 1989;261(1):49–55. [PubMed] [Google Scholar]
- 6.Fu S, Sherman S, Yano E, et al. Ethnic disparities in the use of nicotine replacement therapy for smoking cessation in an equal access health care system. Am J Health Promot. 2005;20:108–116. doi: 10.4278/0890-1171-20.2.108. [DOI] [PubMed] [Google Scholar]
- 7.Giovino GA, Schooley MW, Zhu BP, et al. Surveillance for selected tobacco-use behaviors--United States, 1900–1994. MMWR. 1994;43(3):1–43. [PubMed] [Google Scholar]
- 8.King G, Polednak A, Bendel R, et al. Disparities in smoking cessation between African Americans and Whites: 1990–2000. Am J Pub Health. 2004;94:1965–1971. doi: 10.2105/ajph.94.11.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiore M, Jaen C, Baker T, et al. A clinical practice guideline for treating tobacco use and dependence: 2008 update. Am J Prev Med. 2008;35(2):158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bansal MA, Cummings KM, Hyland A, Giovino GA. Stop-smoking medications: who uses them, who misuses them, and who is misinformed about them? Nicotine Tob Res. 2004;6(Suppl 3):S303–S310. doi: 10.1080/14622200412331320707. [DOI] [PubMed] [Google Scholar]
- 11.Hammond D, McDonald PW, Fong GT, Borland R. Do smokers know how to quit? Knowledge and perceived effectiveness of cessation assistance as predictors of cessation behaviour. Addiction. 2004;99(8):1042–1048. doi: 10.1111/j.1360-0443.2004.00754.x. [DOI] [PubMed] [Google Scholar]
- 12.Botello-Harbaum M, Schroeder J, Collins C, Moolchan E. Nicotine replacement therapy use among adolescent smokers seeking cessation treatment. Ethn Dis. 2010;20(2):180–184. [PubMed] [Google Scholar]
- 13.Cummings KM, Hyland A, Giovino GA, et al. Are smokers adequately informed about the health risks of smoking and medicinal nicotine? Nicotine Tob Res. 2004;6(Suppl 3):S333–S340. doi: 10.1080/14622200412331320734. [DOI] [PubMed] [Google Scholar]
- 14.Fu S, Sherman S, Yano E, et al. Ethnic disparities in the use of nicotine replacement therapy for smoking cessation in an equal access health care system. Am J Health Promot. 2005;20(2):108–116. doi: 10.4278/0890-1171-20.2.108. [DOI] [PubMed] [Google Scholar]
- 15.Fu S, Kodl M, Joseph A, et al. Racial/ethnic disparities in the use of nicotine replacement therapy and quit ratios in lifetime smokers age 25 to 44 years. Cancer Epidemiol Biomarkers Prev. 2008;17(7):1640–1647. doi: 10.1158/1055-9965.EPI-07-2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hymowitz N, Jackson J, Carter R, Eckholdt H. Past quit smoking assistance and doctors’ advice for white and African-American smokers. J Natl Med Assoc. 1996;88(4):249–252. [PMC free article] [PubMed] [Google Scholar]
- 17.Klesges LM, Johnson KC, Somes G, et al. Use of nicotine replacement therapy in adolescent smokers and nonsmokers. Arch Pediatr Adolesc Med. 2003;157(6):517–522. doi: 10.1001/archpedi.157.6.517. [DOI] [PubMed] [Google Scholar]
- 18.Shiffman S, Ferguson SG, Rohay JM, Gitchell J. Perceived safety and efficacy of nicotine replacement therapies among US smokers and ex-smokers: Relationship with use and compliance. Addiction. 2008;103:1371–178. doi: 10.1111/j.1360-0443.2008.02268.x. [DOI] [PubMed] [Google Scholar]
- 19.Etter JF, Perneger TV. Attitudes toward nicotine replacement therapy in smokers and ex-smokers in the general public. Clin Pharmacol Ther. 2000;69(3):175–183. doi: 10.1067/mcp.2001.113722. [DOI] [PubMed] [Google Scholar]
- 20.Zhu S, Melcer T, Sun J, et al. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000;18(4):305–311. doi: 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]
- 21.Fu SS, Burgess D, van Ryn M, et al. Views on smoking cessation methods in ethnic minority communities: a qualitative investigation. Prev Med. 2007;44(3):235–240. doi: 10.1016/j.ypmed.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- 23.Montano DE, Kasprzyk D. Health Behavior and Health Education: Theory, Research and Practice. 3. San Francisco: Jossey Bass; 2002. The theory of reasoned action and the theory of planned behavior; pp. 67–98. [Google Scholar]
- 24.Norman P, Conner M, Bell R. The theory of planned behavior and smoking cessation. Health Psych. 1999;18:89–94. doi: 10.1037//0278-6133.18.1.89. [DOI] [PubMed] [Google Scholar]
- 25.Armitage J, Conner M. Efficacy of the Theory of Planned Behaviour: a meta-analytic review. Br J Soc Psych. 2001;40:471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 26.Ajzen I. The theory of planned behavior. Org Beh Human Dec Proc. 1991;50:179–211. [Google Scholar]
- 27.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 28.SPSS. Statistical Package for Social Sciences (Version 16.0) Chicago, IL: SPSS Inc; 2008. [Google Scholar]
- 29.Davis LE, Ajzen I, Saunders J, Williams T. The decision of African American students to complete high school: an application of the theory of planned behavior. J Educ Psychol. 2002;94(4):810–819. [Google Scholar]
- 30.Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(Pt 4):471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 31.Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Intern Med. 2002;162:2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 32.Pew Forum on Religion and Public Life. A religious portrait of African Americans, US Religious Landscape Survey. Pew Research Center; Washington, DC: 2009. [Accessed November 20, 2010]. Available at: http://pewforum.org/docs/?DocID=389. [Google Scholar]
- 33.CDC. Health disparities experienced by Black or African Americans - United States. MMWR. 2005;54(1):1–3. [PubMed] [Google Scholar]
- 34.Mooney ME, Leventhal AM, Hatsukami DK. Attitudes and knowledge about nicotine and nicotine replacement therapy. Nicotine Tob Res. 2006;8(3):435–446. doi: 10.1080/14622200600670397. [DOI] [PubMed] [Google Scholar]