Abstract
Objectives
The risk of short-term mortality after an emergency department (ED) visit for syncope is poorly understood, resulting in prognostic uncertainty and frequent hospital admission. The authors determined patterns and risk factors for short-term mortality after a diagnosis of syncope or near syncope to aid in medical decision-making.
Methods
A retrospective cohort study was performed of adult members of Kaiser Permanente Southern California seen at 11 EDs from 2002 to 2006 with a primary discharge diagnosis of syncope or near syncope (ICD-9 780.2). The outcome was 30-day mortality. Proportional hazards time-to-event regression models were used to identify risk factors.
Results
There were 22,189 participants with 23,951 ED visits, resulting in 307 deaths by 30 days. A relatively lower risk of death was reached within two weeks for ages 18 to 59 years, but not until three months or more for ages 60 and older. Pre-existing comorbidities associated with increased mortality included heart failure (hazard ratio [HR] 14.3 in ages 18 to 59 years, HR 3.09 in ages 60 to 79 years, HR 2.34 in ages 80 years plus, all P < 0.001), diabetes (HR 1.49, P = 0.002), seizure (HR 1.65, P = 0.016), and dementia (HR 1.41, P = 0.034). If the index visit followed one or more visits for syncope in the previous 30 days, it was associated with increased mortality (HR 1.86, P = 0.024). Absolute risk of death at 30 days was under 0.2% in those under 60 years without heart failure and >2.5% across all ages in those with heart failure.
Conclusions
The low risk of death after an ED visit for syncope or near syncope in patients younger than 60 years old without heart failure, may be helpful when deciding who to admit for inpatient evaluation. The presence of one or more comorbidities that predict death, and a prior visit for syncope, should be considered in clinical decisions and risk stratification tools for patients with syncope. Close clinical follow-up seems advisable in patients 60 years and older due to a prolonged risk of death.
Introduction
Syncope, defined as a transient loss of consciousness, is a common presentation to emergency departments (EDs). Syncope is often benign, but may herald life-threatening medical events. As a result of uncertainty about risks, patients presenting with syncope to EDs are frequently hospitalized, and the inpatient diagnostic evaluation typically focuses on cardiac etiologies of syncope. Syncope accounts for 1% to 2% of all ED visits, and an equal percent of hospital admissions from the ED-based data from the 1980s to 2008.1-8 Unfortunately, current admission practices result in marginal diagnostic and therapeutic benefits from hospitalization.9,10 Between 39% and 50% of admitted patients are discharged without an explanation for syncope.2,11 The health care costs of syncope-related admissions in the United States are substantial, accounting for $2.4 billion annually.12
Emergency department decision-making for patients who present with syncope can be improved by knowledge of the short-term risks faced by population subgroups. In particular, identification of patients at low risk of short-term mortality may lead to fewer unnecessary hospitalizations, especially when outpatient follow-up is available. Several studies have examined risk factors for mortality and morbidity at one year or longer after an episode of syncope,11,13-15 although this time frame is not ideal for making acute care hospitalization decisions. A few studies have examined predictors of short-term medical events.16-19 However, robust analysis of short-term mortality has been limited by small sample sizes, with cohorts between 175 to 791 patients.16,18,20,21 These cohorts were enrolled at single, tertiary care centers, limiting the generalizability of the findings.18-21 Therefore, prediction rules based on the identified risk factors (e.g., the San Francisco Syncope Rule) may not predict well outside of certain settings.17,22-28 More information is needed based on larger, representative cohorts and predictors of short-term mortality.
The goal of this large, retrospective cohort study was to describe the epidemiologic patterns and pre-existing risk factors for short-term mortality after an ED evaluation that yielded a primary diagnosis of syncope or near syncope (ICD-9 780.2). In so doing, we focus on a population for whom disposition decisions (i.e., admit to hospital, observe in ED, or send home) are most difficult. We examined short-term mortality (up to 30 days) since we expected this time frame to reflect the full consequences of ED treatment, and yield information that could influence the urgency of follow-up care.
Methods
Study Design
We conducted a retrospective cohort study using electronic data from a large, regional, integrated health system. The study protocol was reviewed and approved by the institutional review board of Kaiser Permanente Southern California, and the University of California, Los Angeles. Sponsors (see front matter) had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Study Setting and Population
Kaiser Permanente Southern California provides comprehensive care to 3.1 million members throughout Southern California. All members have very similar health care benefits, including coverage of emergency services both within and outside the health system. Electronic administrative and clinical care databases track all health care encounters within the health system. A claims reimbursement system tracks health care provided at outside facilities. All members are assigned a unique medical record number, which is used for data linkage. At the time of the study, there were 11 health system EDs available to members.
Study participants were members of Kaiser Permanente Southern California with at least one ED visit for syncope from January 1, 2002 to December 31, 2006. Subjects were required to be members of the health plan for at least one month at the time of the ED visit. Participants were restricted to age 18 years and older due to the different nature of syncope in children.29
We included only ED visits with a primary ED discharge diagnosis code for syncope: ICD-9 code 780.2 “Syncope and Collapse: Blackout; Fainting; (Near) (Pre) Syncope; Vasovagal Attacks.” Visits to health system EDs had a single primary diagnosis; however, visits to EDs outside the health system sometimes had more than one primary diagnosis code due to billing practices. ED visits outside the health system were excluded if there was more than one primary diagnosis because syncope may have been a consequence of an alternative, primary diagnosis (e.g. myocardial infarction with syncope). Patients who left against medical advice yet had a diagnosis (a minority of cases) were included.
Study Protocol
Demographic information on date of birth, age, sex, and race were obtained from administrative databases. Race and ethnicity were collected by the health plan during the time period of this study through a combination of self-report and staff identification. Preexisting comorbid conditions were identified using data from as far back as 1st Jan. 1998 to one day prior to the ED visit. Comorbidity identification criteria are listed in the Data Supplement (available online). Case-identification criteria for diabetes included a combination of inpatient and outpatient diagnosis codes, medications, and laboratory tests.30 Identification of other comorbidities was based solely on diagnosis and procedural codes. A prior, recent history of syncope was defined by one or more ED visits with a sole, primary discharge diagnosis of syncope within 30 days of a subsequent visit.
To validate the accuracy of discharge codes for identifying patients with syncope, a physician investigator (BCS) blinded to the ED discharge codes reviewed 200 charts, including 100 charts with an ED discharge code of 780.2 as a primary or secondary diagnosis, and 100 charts without an ED discharge code of 780.2. The reviewer noted whether there was explicit chart documentation of syncope or an imminent sensation of syncope. The operational definition of syncope was transient loss of consciousness with spontaneous recovery. Compared to physician chart review, 92 of 100 patient charts with ICD-9 code 780.2 had syncope or near syncope, while eight had no evidence of either diagnosis (92% positive predictive value). None of 100 patients without ICD-9 code 780.2 had syncope or near syncope (100% negative predictive value).
The primary outcome was all-cause death at 30 days. Mortality data came from California death certificate files and the Social Security Death Index for out-of-state deaths, and was available regardless of health plan enrollment status. Cause of death was examined to better understand identified risk factors and was categorized according to ICD-10 groupings.
Data Analysis
We determined the risk of death following an ED visit for syncope using standard survival analysis techniques.31 The first ED visit was used to describe comorbidities and determine rates of death. Risk was examined for ages 18 to 39, 40 to 59, 60 to 79, and 80 plus years; subsequently, the youngest two age categories were combined due to similar risk. After multivariable analyses to identify risk factors, the absolute risk (probability) of death was determined in high risk subgroups using the Kaplan-Meier method.
Multivariable Cox proportional hazards regression was used to estimate the hazard ratio (HR) for death associated with demographic characteristics, pre-existing comorbid conditions, and a recent history of syncope. Logistic regression produced very similar results, and the same associations between predictors and death (not shown). The proportional hazard assumption was met using plots of Kaplan-Meier estimates of the survival function versus time. Repeated visits by the same patient were analyzed by censoring on a subsequent visit with re-entry. Correlations within participants with multiple visits were clustered for correction of standard errors using the robust, sandwich estimator.32 Regression analysis excluded visits in the first month of the study to provide a 30-day prior history of syncope for all participant visits. Age and comorbidities were updated for each ED visit in patients with multiple visits. Age was entered as a categorical variable to model non-linear associations. Interactions were separately tested between age and significant comorbid conditions, including a recent visit for syncope; the same process was followed for sex interactions. All interactions with P < 0.2 were combined into a single model, which was reduced by deletion of non-significant (P > 0.05) interaction terms. The log-likelihood test confirmed the non-significance of the deleted interaction set, and goodness-of-fit (AIC) confirmed the use of simplified age categories (<60, 60-79, ≥80 years).
All analyses were conducted at Kaiser Permanente Southern California's Department of Research using SAS 9.1 (SAS Institute, Cary NC).
Results
Characteristics of Study Subjects
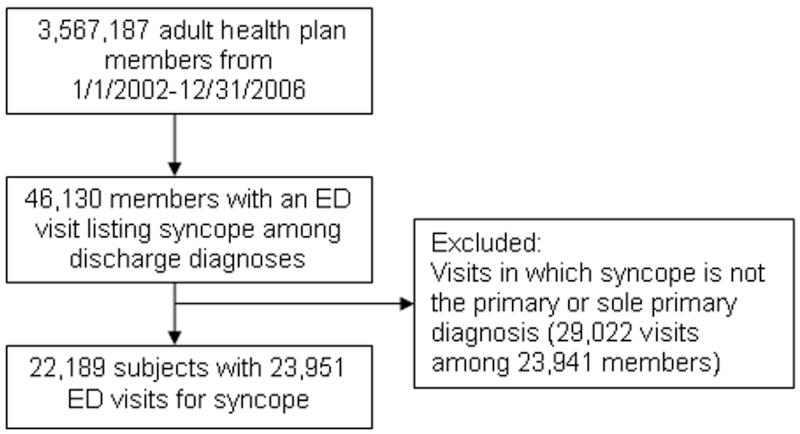
Over the five-year observation period, there were 46,130 health plan members who had one or more ED visits with syncope listed among discharge diagnoses. This represented 1.5% of all ED visits. Approximately half of visits were to health plan facilities. Of all visits with syncope listed among discharge diagnoses, about half had syncope as the sole primary diagnosis. The study cohort was composed of 22,189 participants with 23,951 ED visits with a sole primary diagnosis of syncope (Figure 1). Ninety-three percent of participants had one visit for syncope during the study time-frame; the remaining 7% had two or more visits, with a maximum of nine. Thirty-four percent of all ED visits for syncope resulted in a hospital admission on the day of or the day after the encounter (Table 1). The mean age of participants was 58.8 (SD ±21.0) years, and 57.4% were female (Table 1). Pre-existing, chronic diseases were common (Table 1). The mean and median (IQR) health plan enrollment times at the first ED visit for syncope were 7.8 (SD ±9.9) and 3.9 years (IQR 1.2 to 10.1), respectively.
Figure 1.
Flow diagram of study cohort assembly.
Table 1.
Characteristics of study participants at the time of their first ED visit during the study period.
| Characteristic | Study Cohort (N = 22,189) |
Survived past 30 days (n = 21,908) |
Died by 30 days (n = 281) |
P-value * |
|---|---|---|---|---|
| Age (years)† mean (±SD) | 58.8 (±21.0) | 58.5 (±21.0) | 76.9 (±12.2) | <0.001 |
| Age (years)† n (%) | <0.001 | |||
| 18-39 | 5,008 (22.57) | 5,005 (22.85) | 3 (1.07) | |
| 40-59 | 5,599 (25.23) | 5,574 (25.44) | 25 (8.90) | |
| 60-79 | 7,464 (33.64) | 7,339 (33.50) | 125 (44.48) | |
| 80 plus | 4,118 (18.56) | 3,990 (18.21) | 128 (45.55) | |
| Female n (%) | 12,727 (57.36) | 12,602 (57.52) | 125 (44.48) | <0.001 |
| Race/ethnicity, n (%) | <0.001 | |||
| White | 10,186 (45.91) | 10,013 (45.7) | 173 (61.57) | |
| Hispanic | 3,907 (17.61) | 3,875 (17.69) | 32 (11.39) | |
| Black or African American | 2,874 (12.95) | 2,837 (12.95) | 37 (13.17) | |
| Asian or Pacific Islander | 1,106 (4.98) | 1,090 (4.98) | 16 (6.1) | |
| Other, multiple, unknown | 4,116 (18.55) | 4,093 (18.68) | 23 (8.19) | |
| Admitted to hospital†‡ n (%) | 7,571 (34.12) | 7,356 (33.58) | 215 (76.51) | <0.001 |
| Syncope visits per subject mean (±SD) | 1.08 (±0.34) | 1.08 (±0.34) | 1.03 (±0.17) | 0.011 |
| Pre-existing comorbidity†,§ n (% of cohort) | ||||
| Diabetes | 4,195 (18.91) | 4,083 (18.64) | 112 (39.86) | <0.001 |
| Heart failure | 2,436 (10.98) | 2,316 (10.57) | 120 (42.70) | <0.001 |
| Hypertension | 11,387 (51.32) | 11,169 (50.98) | 218 (77.58) | <0.001 |
| Dysrhythmia§ | 2,729 (12.30) | 2,638 (12.04) | 91 (32.38) | <0.001 |
| Valvular heart disease | 1,575 (7.10) | 1,516 (6.92) | 59 (21.00) | <0.001 |
| Myocardial infarction | 1,165 (5.25) | 1,122 (5.12) | 43 (15.30) | <0.001 |
| Cerebrovascular disease | 1,413 (6.37) | 1,378 (6.29) | 35 (12.46) | <0.001 |
| Seizure | 809 (3.65) | 787 (3.59) | 22 (7.83) | <0.001 |
| Dementia | 1,281 (5.77) | 1,236 (5.64) | 45 (16.01) | <0.001 |
| Gastrointestinal hemorrhage | 591 (2.66) | 578 (2.64) | 13 (4.63) | 0.058 |
P-value for comparison of a characteristic between the group who died and the group who survived at 30 days based on a two-sided hypothesis: Fischer's Exact test and Wilcoxon Rank Sum test.
Based on first ED visit for syncope during the study period in subjects with multiple visits.
Admission the same day or the day after the ED visit.
Comorbidity definitions are provided in the Data Supplement. Dysrhythmia included a past history of 3rd degree heart block, Mobitz II heart block, other heart block, ventricular tachycardia, ventricular fibrillation or flutter, atrial fibrillation or flutter, paroxysmal atrial tachycardia, SA node dysfunction, anomalous AV excitation (pre-excitation), other conduction disorders, and cardiac arrest.
Main Results
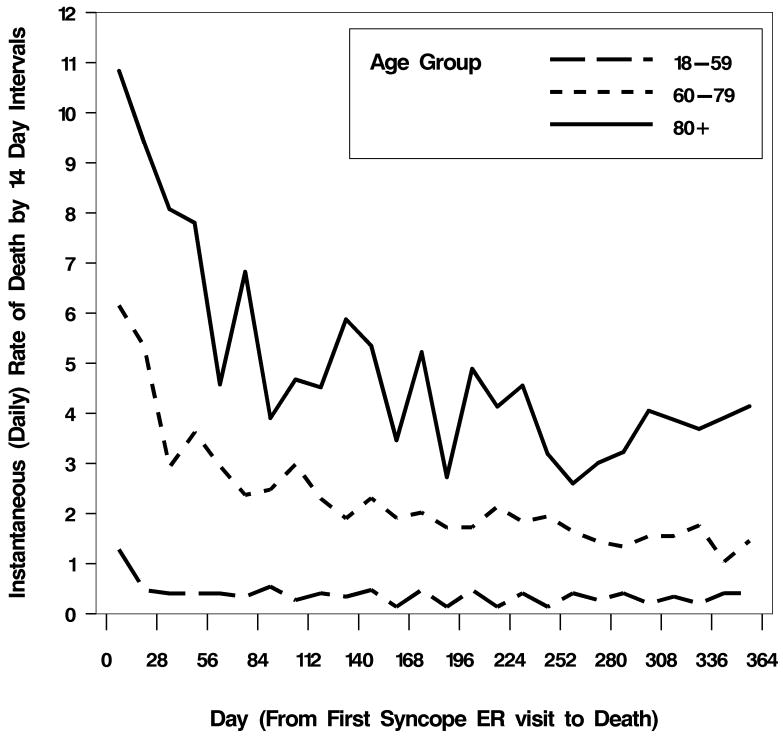
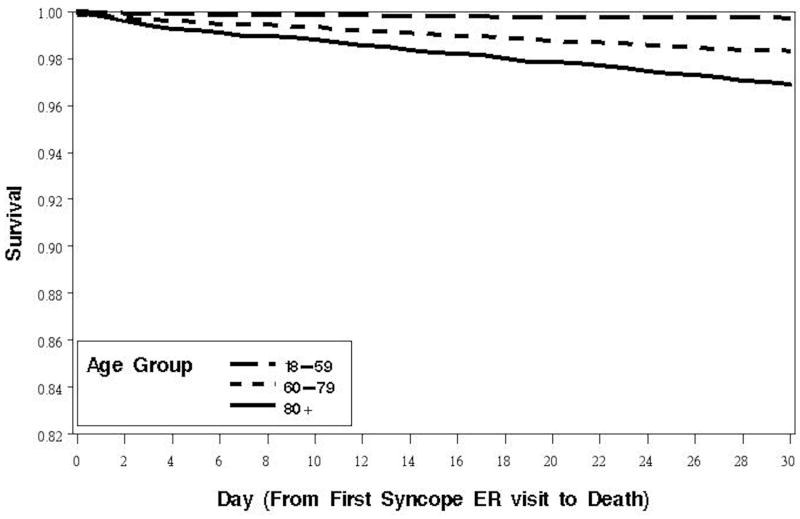
Deaths were infrequent and the hazard rate for mortality declined with time. There were 107, 321, and 1,655 deaths by 7, 30, and 365 days, respectively, after an ED visit for syncope during the study period. The unadjusted hazard function (instantaneous rate of death per day) averaged over 2 week intervals out to one year after the first ED visit is shown in Figure 2. Mortality risk varied greatly with age. In participants under 60 years old, the risk of death declined after 14 days to a roughly steady rate. In those 80 years and older, the risk of death remained elevated during the first 3 to 6 months after the ED visit, compared to risk levels after 6 months. Participants aged 60-79 years had an elevated risk of death for 6 months or more compared to risk during the latter part of the one year follow-up. Figure 3 shows unadjusted, cumulative survival to 30 days in each age strata. By 30 days, more than 1% of those 60 years and older had died. By 30 days, there were 215 deaths (2.84%) among those who were hospitalized from the ED, and 66 deaths (0.45%) among those who were not hospitalized.
Figure 2.
Hazard of death to 1 year by age strata after the first ED visit for syncope during the study period.
Footnote: The y-axis denotes the instantaneous rate of death at 14-day time intervals given survival to the end of the interval. Points are graphed at the center of each time interval.
Figure 3.
Survival to 30 days by age strata after the first ED visit for syncope during the study period.
Cause of death by 0 to 7 days and 8 to 30 days are listed in Table 2. Overall, the most common causes of death by far were heart disease (35%) and cancer (19%). At 7 days, heart disease deaths predominated (39%); between 7 and 30 days, there was a substantial increase in the proportion of cancer deaths, from 14% to 23%. Two-thirds of deaths occurred between 7 and 30 days.
Table 2.
Causes of death by time interval following the final ED visit for syncope during the study period.
| Cause of Death | 0-7 days | 8-30 days | Total by 30 days |
|---|---|---|---|
| Heart disease | 42 (39.25) | 71 (33.18) | 113 (35.20) |
| Cancer | 15 (14.02) | 50 (23.26) | 65 (19.31) |
| Stroke | 10 (9.35) | 16 (7.48) | 26 (6.54) |
| Respiratory | 4 (3.74) | 16 (7.48) | 20 (5.92) |
| Injuries* | 5 (4.67) | 5 (2.34) | 10 (3.12) |
| Diabetes | 2 (1.87) | 13 (6.07) | 15 (4.67) |
| Alzheimer's, other dementia | 3 (2.80) | 10 (4.67) | 13 (4.05) |
| Liver | 1 (0.93) | 1 (0.47) | 2 (0.62) |
| Renal | 4 (3.74) | 8 (3.74) | 12 (3.74) |
| Infectious | 6 (5.61) | 7 (3.27) | 13 (4.05) |
| Other | 13 (12.15) | 12 (5.61) | 25 (7.79) |
| Missing cause | 2 (1.87) | 5 (2.34) | 7 (2.18) |
| Total (column) | 107 (100) | 214 (100) | 321 (100) |
Includes unintentional and intentional injuries.
Values are reported as n (%)
Cause of death was categorized according to the ICD-10 category blocks.
Proportional hazards regression was used to identify demographic characteristics and pre-existing comorbidities that were associated with an increased risk for short-term death (Table 3). Race and ethnicity had no significant association with death before or after adjustment for other covariates; for parsimony this variable was dropped from final results. Male sex was weakly associated with an increased risk of death (HR 1.36, P = 0.009). Increasing age was strongly associated with an increasing risk of death: HR 6.59 for ages 60 to 79 years, and HR 11.73 for ages 80 and over, compared to ages 18 to 59 years (each P < 0.001). A prior visit for syncope was associated with an increased risk of death (HR 1.86, P = 0.024).
Table 3.
Risk factors for death by 30 days subsequent to any ED visit for syncope during the study period (proportional hazards model).
| Characteristics | Death by 30 days | ||
|---|---|---|---|
| HR | (95% CI) | P-value | |
| Male | 1.36ˆ | 1.08-1.72 | 0.009 |
| Age* | |||
| 60-79 years | 6.59ˆ | 3.83-11.34 | <0.001 |
| 80 plus years | 11.73ˆ | 6.58-20.92 | <0.001 |
| Recent visit for syncope† | 1.86ˆ | 1.08-3.18 | 0.024 |
| Diabetes | 1.49ˆ | 1.16-1.90 | 0.002 |
| Hypertension | 0.79 | 0.57-1.10 | 0.161 |
| Dysrhythmia | 1.14 | 0.88-1.48 | 0.318 |
| Valvular heart disease | 1.16 | 0.86-1.56 | 0.332 |
| Myocardial infarction | 1.16 | 0.83-1.62 | 0.380 |
| Cerebrovascular disease | 0.92 | 0.66-1.28 | 0.622 |
| Seizure | 1.65ˆ | 1.10-2.48 | 0.016 |
| Dementia | 1.41ˆ | 1.03-1.94 | 0.034 |
| Gastrointestinal hemorrhage | 0.88 | 0.52-1.51 | 0.652 |
| Heart failure‡ | |||
| 18-59 years | 14.3ˆ | 6.28-32.5 | <0.001 |
| 60-79 years | 3.09ˆ | 2.12-4.49 | <0.001 |
| 80 plus years | 2.34ˆ | 1.63-3.36 | <0.001 |
Reference group: age 18-59 years.
Defined as one or more visits within the 30 days of the index ED visit.
HR for presence vs. absence of the comorbidity within the same age group.
Significant associations (P<0.05).
Multivariable Cox proportional hazards model using all ED visits for syncope during the study period. Multiple visits by a participant were clustered for correction of standard errors using the robust, sandwich estimator. ED visits among 415 patients during the first month of the study (Jan 2002) were dropped from analysis so that all patients included in the regression model had at least one month of observation to determine a history of prior syncope visits within 30 days of the index ED visit. Among the 21,774 patients included in the model, there were 23,491 visits, 103 deaths at 7 days, and 307 deaths at 30 days.
Comorbidity definitions are provided in the Data Supplement.
Of all pre-existing conditions, heart failure was most strongly predictive of an increased risk of death, and this relationship varied by age. In 18 to 59 year olds, the HR associated with heart failure was 14.3; for ages 60 to 79 and 80 and over, the HRs were 3.09 and 2.34, respectively (each P < 0.001). A history of diabetes was associated with an increased risk of death (HR 1.49, P = 0,002). Among non-cardiovascular conditions, increased death was associated with dementia (HR 1.41, P = 0.034), and a history of seizures (HR 1.65, P = 0.016).
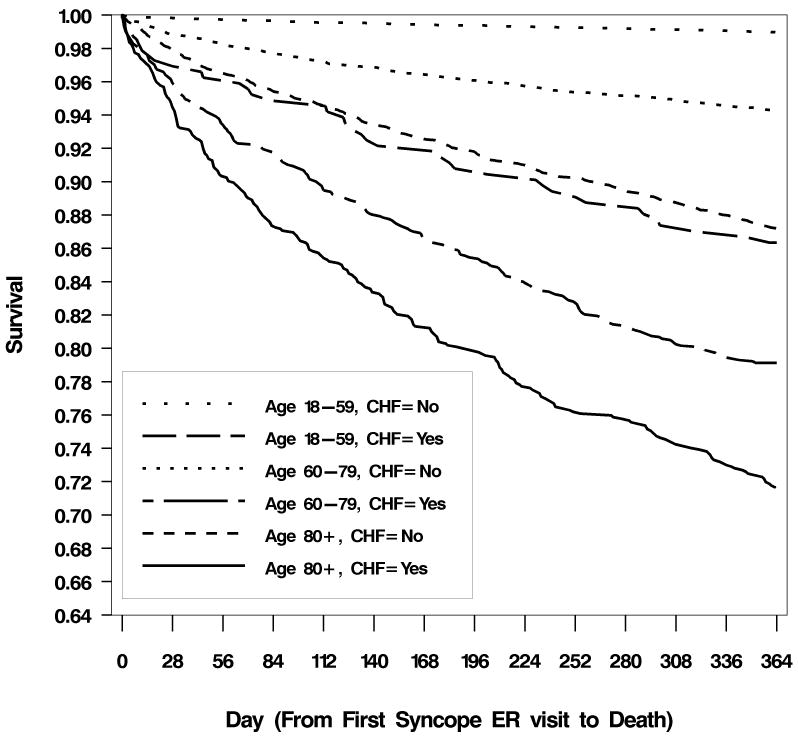
Table 4 presents the probability (absolute risk) of death by 30 days in subgroups with and without heart failure, by age and sex. The probability of death was relatively low (fewer than two deaths per 1,000 cases) in person under age 60 years without heart failure. The probability of death was relatively high (more than 25 deaths per 1,000 cases) in anyone with heart failure and in men aged 80 years and older without heart failure. The risk associated with a diagnosis of heart failure in different age groups is persistently high, as demonstrated by the one-year survival curves of Figure 4.
Table 4.
Mortality at 30 days given heart failure, sex, and age.
| Sex and Age (years) | Deaths per 1,000 Cases (95% CI) Heart Failure |
|
|---|---|---|
| No | Yes | |
| Males | ||
| 18-59 | 1.9 (0.7-3.8) | 33.5 (7.2-59.9) |
| 60-79 | 14.5 (10.6-19.3) | 41.9 (28.0-60.0) |
| 80 plus | 35.4 (25.7-47.3) | 55.9 (36.8-80.9) |
| Females | ||
| 18-59 | 1.8 (0.9-3.2) | 26.3 (5.5-75.0) |
| 60-79 | 9.0 (6.0-12.9) | 45.9 (29.3-68.1) |
| 80 plus | 13.0 (8.4-19.1) | 66.8 (46.7-92.1) |
Confidence intervals were based on the binomial distribution and determined using the exact method. Cells with zero had no deaths. The numbers of participants with pre-existing heart failure is provided in Table 1.
Figure 4.
Survival to one year by age and heart failure strata after the first ED visit for syncope during the study period.
Discussion
We performed a large retrospective cohort study among members of an integrated health system that collects comprehensive data on comorbidities and outcomes. To our knowledge, this is the largest cohort study of short-term mortality following a primary diagnosis of syncope or near syncope, and contains sufficient numbers of decedents to generate stable inferences. Studies of short-term mortality are most informative for ED decision-making, and provide data to drive hypotheses about risk factors for the development of risk prediction tools in prospective studies. Our findings build on existing literature and reveal novel insights into population-level patterns and risk factors for short-term mortality after an ED visit. Risk factors previously identified from studies of long-term mortality following syncope (i.e., heart failure, diabetes) were confirmed as risk factors for short-term mortality. The sharply increased risk of all-cause mortality immediately following syncope or near syncope declined more gradually at older ages, taking several months in elders. The risk of death by 30 days was less than 1% in those under 60 years old who did not have a past history of heart failure. Finally, one or more recent visits with syncope or near syncope as the primary diagnosis increased the risk death.
A diagnosis of syncope or near syncope appears to confer transient and excess mortality risk in all age groups based on a decreasing daily risk of death over time (Figure 2). To confirm this impression, we calculated the daily risk of death over the course of a year in members without an ED visit for syncope based on ICD-9 code 780.2 (i.e., those excluded from study when progressing from the first to the second box of Figure 1). The “background” risk of death per 10,000 persons aged 18 to 59, 60 to 79, and 80 years and over was 0.09, 0.69, and 3.05, respectively. Compared to Figure 2, these numbers indicate that the background risk of death is reached by about 6 months in the younger and older age groups with syncope or near syncope. In 60 to 79 year olds with syncope or near syncope, the risk of death never drops as low as the background level in those without syncope over the course of one year. Thus our data indicate that in patients 60 years and older, mortality risk remains elevated for at least 3 months after the index ED visit.33 These results suggest that older patients require close outpatient follow-up, even when an acute precipitant cannot be identified after initial ED evaluation.
Not surprisingly, age was identified as the most powerful risk factor for short-term mortality after syncope or near syncope, consistent with previous studies.13,15,16,18 Comparison of a regression model with age and sex as the only predictors (results not shown) and the model presented suggests that a significant proportion of age-related risk is attenuated by the addition of pre-existing cardiovascular conditions. Nevertheless, significant age-related risk remained after adjusting for diagnosed cardiovascular conditions. The slower return to lower levels of risk in older patients may be attributable in part to age-related recovery versus decline in health due to decompensation of chronic illnesses.34
Male sex conferred modestly increased 30-day mortality risk. Male sex may be associated with increased risk of unrecognized cardiovascular disease. In the Framingham Heart Study, men who experienced syncope were more likely to have a cardiac cause than women.35 Other investigations have found a univariate association between male sex and adverse events including mortality; in multivariate analyses, this finding has been confirmed19 less often than not.13,16,36 However, these studies may have had insufficient power (n = 516 to 676) to detect clinically important associations.
Consistent with prior studies of long-term syncope outcomes, we found that a history of congestive heart failure was associated with increased mortality.15,37 A similar, statistically significant pattern for heart failure was seen for seven-day mortality (data not shown). A history of heart failure may be a marker of structural heart disease and increased risk of sudden death. A previous cohort study (n = 400) noted negative interaction effects between increasing age and heart failure, and between age and cardiac cause of syncope, when assessing two-year risk of all-cause mortality and sudden death.38 In our larger cohort, we observed a relatively larger risk of 30-day death among younger subjects with heart failure. The absolute risk associated with heart failure was relatively high early after the ED visit, and persisted across time in all age strata, indicating the importance of a diagnosis of heart failure.
We also found that dementia was associated with increased 30-day mortality, and that dementia was more commonly noted as the cause of death from 8 to 30 days after the syncope or near syncope event. Dementia may be a marker of additional comorbidities, severity of illness, or variations in care associated with increased mortality over time, rather than a risk factor specific to syncope.35,39,40 In addition, a prior history of seizures was associated with increased mortality, as has been reported in the Framingham cohort.30 ED presentation of seizure, although not in the context of syncope, has been associated with 10-year mortality in a Swedish study.41 Some patients with a diagnosis of seizures may have unrecognized cardiac conditions.31
Finally, our study provides clinically relevant information about the short-term prognostic implications of recurrent syncope or near syncope. The risk of death was increased 86% in patients who had one or more ED visits for syncope or near syncope within the prior month. Because we included in analysis only visits with a primary diagnosis of syncope or near syncope, these recurrent episodes may be more likely to represent events without an identified cause. Our findings suggest that patients with recurrent syncope or near syncope within 30 days may benefit from close clinical follow-up. These results contrast with those from a single center, prospective cohort of 433 patients with syncope.42 In this study, mortality at three years was not affected by the presence of recurrent syncope. However, this cohort included patients with and without known etiologies for syncope, focused on long-term outcomes, and defined prior syncope as an event that occurred at any time prior to evaluation.
Limitations
Our study identified syncope and near syncope using ED discharge diagnosis codes. It is possible that screening by discharge diagnosis codes may not correctly identify patients with syncope or near syncope. The physician chart review for accuracy of ICD-9 code 780.2 yielded a good positive predictive value (92%) and negative predictive value (100%) for syncope or near syncope. We were not able to distinguish between syncope and near syncope. These two symptoms are related by degree of brain hypoperfusion, have parallel outcomes, and present a similar clinical dilemma;43 thus, their grouping by ICD-9 diagnosis code does not appear problematic for identification of risk factors and mortality patterns.
Syncope and near syncope are symptoms caused by some specific diagnosis rather than a clinical diagnosis in themselves. We did not attempt to identify possible causes of syncope symptoms. We wished to focus on patients with an unclear cause of syncope since they present a difficult decision regarding hospitalization. The population of patients presenting with syncope or near syncope likely contains a mixture of those with and without an identifiable cause either during or after ED evaluation. To mitigate this potential limitation, our study cohort included only those patients with a sole primary discharge diagnosis of syncope or near syncope. We selected this approach because patients with an identified cause of syncope, such as arrhythmia or coronary ischemia, were deemed unlikely to have syncope as the primary diagnosis. Patients with syncope due to an identified or likely cause are a substantially different clinical problem.
Decision-making in the ED requires estimating the risk of short-term events, for which diagnostic or therapeutic hospitalization may be beneficial.44 The appropriate time frame for measuring outcomes after a syncope visit is controversial, and investigators have suggested a range of two to 30 days.17,44 In additional analyses (data not shown), we identified no risk factors for 7-day mortality that were not also identified at 30 days, thus simplifying decision-making with respect to risk factors.
The demographic characteristics of this managed care population are similar to those of the surrounding population in southern California. However, compared to syncope ED visits in a nationally representative sample,7 our study cohort has a higher proportion of non-white and Hispanic patients. In addition, care processes in this integrated health system may be different from those of other settings, and admission rates are lower than in other cohort studies.17,22,45 Access to outpatient services exists for all health plan members. Therefore, our findings may not generalize to settings with limited continuity of care or to the uninsured.
We did not attempt to measure the increased risk above baseline due to syncope in those with an otherwise similar clinical presentation. We collected pre-existing co-morbidity information using administrative data. A complete electronic health record was not fully available during the time frame of this study, thus it was not feasible to collect potentially important clinical elements gathered during the evaluation of syncope, including associated symptoms, vital signs, physical exam findings, and electrocardiogram abnormalities.13,15-19,36,46 However, clinical findings at the time of the event can be meaningfully separated from pre-existing risk factors to allow for clinically informative, general risk stratification of presenting patients. In a separate, chart-review investigation, we examined co-existing clinical factors as predictors of 30-day clinical events in a sample of 2,584 health plan members age 60 and older; however, there were too few 30-day deaths (n = 41) to perform meaningful analyses of short-term death.47
Conclusions
We described the epidemiologic patterns and identified pre-existing risk factors for short-term mortality after an ED visit and primary diagnosis of syncope or near syncope. Short-term mortality after syncope is an uncommon occurrence, and prior studies have been forced to combine outcomes or look at longer time intervals to assess risk factors. Mortality risk was increased subsequent to an ED visit for syncope or near syncope in all age groups; in patients 60 years and older, there was a gradual reduction in mortality risk over the first three or more months. The risk of death by 30 days was less than 0.2% in those under 60 years who did not have a past history of heart failure. Patients with heart failure had particularly high (>2.5%) short-term mortality, regardless of age. Finally, a history of an ED visit for syncope in the previous month predicted increased mortality at 30-days. Our findings include new information on risk factors and confirm the importance of some previously identified risk factors from studies that were small in size or based on long-term rather than short-term mortality. This information may aid ED decision-making for patients with a primary diagnosis of syncope or near syncope and the development of risk prediction tools for identifying patients who will benefit from hospital admission.
Supplementary Material
Acknowledgments
We thank the Greater Los Angeles Veteran's Affairs Health Services Research and Development Fellowship for their support of Dr. Gabayan. We thank Robert Weiss, UCLA School of Public Health Professor of Biostatistics, for his helpful manuscript review.
Financial Support: This research was supported by grants from American Geriatrics Society Dennis Jahnigen Career Development Award (20051687, B. Sun) and University of California, Los Angeles, National Institutes of Aging K12 Mentored Clinical Scientist Development Program in Geriatrics (AG 02-004, B. Sun). Dr. Sun received support from the UCLA Older Americans Independence Center, NIH/NIA Grant P30-AG028748, and the content does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Footnotes
Disclosures: The authors have no disclosures or conflicts of interest to report.
References
- 1.Ammirati F, Colivicchi F, Santini M. Diagnosing syncope in clinical practice. Implementation of a simplified diagnostic algorithm in a multicentre prospective trial - the OESIL 2 study (Osservatorio Epidemiologico della Sincope nel Lazio) Eur Heart J. 2000;21(11):935–40. doi: 10.1053/euhj.1999.1910. [DOI] [PubMed] [Google Scholar]
- 2.Blanc JJ, L'Her C, Touiza A, Garo B, L'Her E, Mansourati J. Prospective evaluation and outcome of patients admitted for syncope over a 1 year period. Eur Heart J. 2002;23(10):815–20. doi: 10.1053/euhj.2001.2975. [DOI] [PubMed] [Google Scholar]
- 3.Brignole M, Disertori M, Menozzi C, et al. Management of syncope referred urgently to general hospitals with and without syncope units. Europace. 2003;5(3):293–8. doi: 10.1016/s1099-5129(03)00047-3. [DOI] [PubMed] [Google Scholar]
- 4.Casini-Raggi V, Bandinelli G, Lagi A. Vasovagal syncope in emergency room patients: analysis of a metropolitan area registry. Neuroepidemiol. 2002;21(6):287–91. doi: 10.1159/000065525. [DOI] [PubMed] [Google Scholar]
- 5.Day SC, Cook EF, Funkenstein H, Goldman L. Evaluation and outcome of emergency room patients with transient loss of consciousness. Am J Med. 1982;73(1):15–23. doi: 10.1016/0002-9343(82)90913-5. [DOI] [PubMed] [Google Scholar]
- 6.Sarasin FP, Louis-Simonet M, Carballo D, et al. Prospective evaluation of patients with syncope: a population-based study. Am J Med. 2001;111(3):177–84. doi: 10.1016/s0002-9343(01)00797-5. [DOI] [PubMed] [Google Scholar]
- 7.Sun BC, Emond JA, Camargo CA., Jr Characteristics and admission patterns of patients presenting with syncope to U.S. emergency departments, 1992-2000. Acad Emerg Med. 2004;11:1029–34. doi: 10.1197/j.aem.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 8.National Hospital Ambulatory Medical Care Survey (NHAMCS) National Hospital Ambulatory Medical Care Survey: 2008 emergency department summary tables. [Accessed Jan 21, 2012]; Available at: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/namcssum2008.pdf.
- 9.Kapoor WN, Karpf M, Maher Y, Miller RA, Levey GS. Syncope of unknown origin. The need for a more cost-effective approach to its diagnosis evaluation. JAMA. 1982;247(19):2687–91. doi: 10.1001/jama.247.19.2687. [DOI] [PubMed] [Google Scholar]
- 10.Mozes B, Confino-Cohen R, Halkin H. Cost-effectiveness of in-hospital evaluation of patients with syncope. Isr J Med Sci. 1988;24(6):302–6. [PubMed] [Google Scholar]
- 11.Getchell WS, Larsen GC, Morris CD, McAnulty JH. Epidemiology of syncope in hospitalized patients. J Gen Intern Med. 1999;14(11):677–87. doi: 10.1046/j.1525-1497.1999.03199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun BC, Emond JA, Camargo CA., Jr Direct medical costs of syncope-related hospitalizations in the United States. Am J Cardiol. 2005;95(5):668–71. doi: 10.1016/j.amjcard.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Colivicchi F, Ammirati F, Melina D, Guido V, Imperoli G, Santini M. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J. 2003;24(9):811–9. doi: 10.1016/s0195-668x(02)00827-8. [DOI] [PubMed] [Google Scholar]
- 14.Kapoor WN, Karpf M, Wieand S, Peterson JR, Levey GS. A prospective evaluation and follow-up of patients with syncope. N Engl J Med. 1983;309(4):197–204. doi: 10.1056/NEJM198307283090401. [DOI] [PubMed] [Google Scholar]
- 15.Martin TP, Hanusa BH, Kapoor WN. Risk stratification of patients with syncope. Ann Emerg Med. 1997;29(4):459–66. doi: 10.1016/s0196-0644(97)70217-8. [DOI] [PubMed] [Google Scholar]
- 16.Costantino G, Perego F, Dipaola F, et al. Short- and long-term prognosis of syncope, risk factors, and role of hospital admission: results from the STePS (Short-Term Prognosis of Syncope) study. J Am Coll Cardiol. 2008;51(3):276–83. doi: 10.1016/j.jacc.2007.08.059. [DOI] [PubMed] [Google Scholar]
- 17.Quinn J, McDermott D, Stiell I, Kohn M, Wells G. Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes. Ann Emerg Med. 2006;47(5):448–54. doi: 10.1016/j.annemergmed.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 18.Sarasin FP, Hanusa BH, Perneger T, Louis-Simonet M, Rajeswaran A, Kapoor WN. A risk score to predict arrhythmias in patients with unexplained syncope. Acad Emerg Med. 2003;10:1312–7. doi: 10.1111/j.1553-2712.2003.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 19.Reed MJ, Newby DE, Coull AJ, Prescott RJ, Jacques KG, Gray AJ. The ROSE (risk stratification of syncope in the emergency department) study. J Am Coll Cardiol. 2010;55(8):713–21. doi: 10.1016/j.jacc.2009.09.049. [DOI] [PubMed] [Google Scholar]
- 20.Quinn JV, Stiell IG, McDermott DA, Kohn MA, Wells GA. The San Francisco Syncope Rule vs physician judgment and decision making. Am J Emerg Med. 2005;23(6):782–6. doi: 10.1016/j.ajem.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224–32. doi: 10.1016/s0196-0644(03)00823-0. [DOI] [PubMed] [Google Scholar]
- 22.Birnbaum A, Esses D, Bijur P, Wollowitz A, Gallagher EJ. Failure to validate the San Francisco Syncope Rule in an independent emergency department population. Ann Emerg Med. 2008;2(52):151–9. doi: 10.1016/j.annemergmed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Cosgriff TM, Kelly AM, Kerr D. External validation of the San Francisco Syncope Rule in the Australian context. CJEM. 2007;9(3):157–61. doi: 10.1017/s1481803500014986. [DOI] [PubMed] [Google Scholar]
- 24.Esses D, Birnbaum A, Wollowitz A, Bijur P, Gallagher EJ. Failure to validate the San Francisco Syncope Rule in an independent ED population (abstract) Acad Emerg Med. 2007;14:S162–a. doi: 10.1016/j.annemergmed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 25.Fischer CM, Shapiro NI, Lipsitz LA, et al. External validation of the San Francisco Syncope Rule (abstract) Acad Emerg Med. 2005;12(Suppl 1):127. [Google Scholar]
- 26.Reed MJ, Newby DE, Coull AJ, Jacques KG, Prescott RJ, Gray AJ. The risk stratification Of Syncope in the Emergency department (ROSE) pilot study: a comparison of existing syncope guidelines. Emerg Med J. 2007;24(4):270–5. doi: 10.1136/emj.2006.042739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sun BC, Mangione CM, Merchant G, et al. External validation of the San Francisco Syncope Rule. Ann Emerg Med. 2007;49(4):420–7. doi: 10.1016/j.annemergmed.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 28.Thiruganasambandamoorthy V, Hess EP, Alreesi A, Perry JJ, Wells GA, Stiell IG. External validation of the San Francisco Syncope Rule in the Canadian setting. Ann Emerg Med. 2010;55(5):464–72. doi: 10.1016/j.annemergmed.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Driscoll DJ, Jacobsen SJ, Porter CJ, Wollan PC. Syncope in children and adolescents. J Am Coll Cardiol. 1997;29(5):1039–45. doi: 10.1016/s0735-1097(97)00020-x. [DOI] [PubMed] [Google Scholar]
- 30.Petitti DB, Contreras R, Ziel FH, Dudl J, Domurat ES, Hyatt JA. Evaluation of the effect of performance monitoring and feedback on care process, utilization, and outcome. Diabetes Care. 2000;23(2):192–6. doi: 10.2337/diacare.23.2.192. [DOI] [PubMed] [Google Scholar]
- 31.Kleinbaum DG, Klein M. Survival Analysis: A Self-Learning Text. 2nd. New York, NY: Springer-Verlag Inc.; 2005. [Google Scholar]
- 32.Binder DA. Fitting Cox's proportional hazards models from survey data. Biometrika. 1992;7(1):139–47. [Google Scholar]
- 33.Barlas D, Homan CS, Rakowski J, Houck M, Thode HC., Jr How well do patients obtain short-term follow-up after discharge from the emergency department? Ann Emerg Med. 1999;34(5):610–4. doi: 10.1016/s0196-0644(99)70163-0. [DOI] [PubMed] [Google Scholar]
- 34.Lipsitz LA, Wei JY, Rowe JW. Syncope in an elderly, institutionalised population: prevalence, incidence, and associated risk. Q J Med. 1985;55(216):45–54. [PubMed] [Google Scholar]
- 35.Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med. 2002;347(12):878–85. doi: 10.1056/NEJMoa012407. [DOI] [PubMed] [Google Scholar]
- 36.Del Rosso A, Ungar A, Maggi R, et al. Clinical predictors of cardiac syncope at initial evaluation in patients referred urgently to general hospital: the EGSYS score. Heart. 2008;94(12):1620–6. doi: 10.1136/hrt.2008.143123. [DOI] [PubMed] [Google Scholar]
- 37.Middlekauff HR, Stevenson WG, Stevenson LW, Saxon LA. Syncope in advanced heart failure: high risk of sudden death regardless of origin of syncope. J Am Coll Cardiol. 1993;21(1):110–6. doi: 10.1016/0735-1097(93)90724-f. [DOI] [PubMed] [Google Scholar]
- 38.Kapoor W, Snustad D, Peterson J, Wieand HS, Cha R, Karpf M. Syncope in the elderly. Am J Med. 1986;80(3):419–28. doi: 10.1016/0002-9343(86)90716-3. [DOI] [PubMed] [Google Scholar]
- 39.Llinas-Regla J, Lopez-Pousa S, Vilalta-Franch J, Garre-Olmo J, Roman GC. Mortality after a diagnosis of dementia in a population aged 75 and over in Spain. Neuroepidemiology. 2008;31(2):80–8. doi: 10.1159/000144088. [DOI] [PubMed] [Google Scholar]
- 40.Raji MA, Kuo YF, Freeman JL, Goodwin JS. Effect of a dementia diagnosis on survival of older patients after a diagnosis of breast, colon, or prostate cancer: implications for cancer care. Arch Intern Med. 2008;168(18):2033–40. doi: 10.1001/archinte.168.18.2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Safwenberg U, Terent A, Lind L. Differences in long-term mortality for different emergency department presenting complaints. Acad Emerg Med. 2008;15:9–16. doi: 10.1111/j.1553-2712.2007.00004.x. [DOI] [PubMed] [Google Scholar]
- 42.Kapoor WN, Peterson J, Wieand HS, Karpf M. Diagnostic and prognostic implications of recurrences in patients with syncope. Am J Med. 1987;83(4):700–8. doi: 10.1016/0002-9343(87)90901-6. [DOI] [PubMed] [Google Scholar]
- 43.Grossman SA, Babineau M, Burke L, et al. Do outcomes of near syncope parallel syncope? Am J Emerg Med. 2010;30(1):203–6. doi: 10.1016/j.ajem.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 44.Gallagher EJ. Hospitalization for fainting: high stakes, low yield. Ann Emerg Med. 1997;29(4):540–2. [PubMed] [Google Scholar]
- 45.Sun BC, Hoffman JR, Mangione CM, Mower WR. Older age predicts short-term, serious events after syncope. J Am Geriatr Soc. 2007;55(6):907–12. doi: 10.1111/j.1532-5415.2007.01188.x. [DOI] [PubMed] [Google Scholar]
- 46.Sun BC, Hoffman JR, Mower WR, Shlamovitz GZ, Gabayan GZ, Mangione CM. Low diagnostic yield of electrocardiogram testing in younger patients with syncope. Ann Emerg Med. 2008;51(3):240–6. doi: 10.1016/j.annemergmed.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 47.Sun BC, Derose SF, Liang LJ, et al. Predictors of 30-day serious events in older patients with syncope. Ann Emerg Med. 2009;54(6):769–78. doi: 10.1016/j.annemergmed.2009.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.