Abstract
Background:
We report herein a case of cavernous sinus (CS)-dural arteriovenous fistula (DAVF) with brainstem venous congestion that was successfully treated by transarterial embolization, followed by radiotherapy.
Case Description:
An 80-year-old woman presented with right eye chemosis and left hemiparesis. T2-weighted magnetic resonance imaging showed hyperintensity of the pons. Diagnostic cerebral angiography demonstrated CS-DAVF draining into the right superior orbital vein and petrosal vein, and fed by bilateral internal and external carotid arteries. Transarterial embolization was performed and followed by radiotherapy, resulting in resolution of the pontine lesion and neurological and ophthalmological symptoms within 5 months.
Conclusions:
We also review the literature regarding therapy for CS-DAVF with brainstem venous congestion. Once CS-DAVF with venous congestion of the brainstem has been definitively diagnosed, immediate therapy is warranted. Treatment with transarterial embolization followed by radiation may be an important option for elderly patients when transvenous or transarterial embolization is not an option.
Keywords: Cavernous dural arteriovenous fistula, pontine venous congestion, radiation therapy, transarterial embolization
INTRODUCTION
Pontine venous congestion is a rare but serious complication of cavernous sinus (CS)-dural arteriovenous fistula (DAVF). Although the number of reports on CS-DAVF with brainstem venous congestion has been increasing in recent years,[1,5,6,9,11,12] appropriate clinical diagnosis and treatment for CS-DAVF with brainstem venous congestion remain challenging.[1,9] We describe herein a case of CS-DAVF with pontine venous congestion, which was successfully treated by transarterial embolization (TAE) followed by radiotherapy.
CASE REPORT
The patient was an 80-year-old woman with no past history of head injury, sinus thrombosis, or infections. She initially noticed redness of the sclera in the right eye and consulted a local ophthalmologist. Three months later, she was referred to our hospital. The right eye showed chemosis and swelling of the eyelid. Head computed tomography (CT) revealed exophthalmos and swelling of the right superior orbital vein (SOV). She was initially followed on an outpatient basis. One month later, symptoms including chemosis, facial swelling, and gait disturbance were found to be worsening and she was admitted to our hospital.
Neurological examination showed mild ataxia of the left lower extremity and dysarthria. A full range of eye movement was seen, and the patient did not complain of diplopia.
T2-weighted magnetic resonance (MR) imaging showed a hyperintense lesion on the right side of the upper pons and the right SOV was dilated [Figure 1a]. T1-weighted MR imaging of the same region showed good contrast enhancement with gadolinium [Figure 1b]. Diffusion weighted imaging (DWI) showed normal signal (not shown). The patient gave written informed consent before angiography and treatment.
Figure 1.
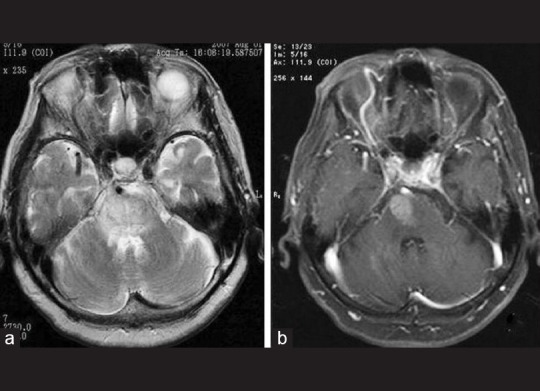
Magnetic resonance imaging of the patient showing hyperintensity in the upper pons and dilatation of the right superior orbital vein on (a) T2-weighted image, and good contrast enhancement after injection of gadolinium on (b) T1-weighted image
Cerebral angiography showed CS-DAVF supplied by the dural branches of bilateral internal and external carotid arteries, draining into the right SOV and petrosal vein [Figure 2].
Figure 2.

Lateral-view angiography demonstrating CS-DAVF draining into the right superior orbital vein (arrowhead) and petrosal vein (arrow), fed by dural branches of the internal and external carotid arteries
Because superselective catheterization through the petrosal sinus up to the pathologic shunt points was not successful, transvenous embolization was technically difficult. And then the TAE was attempted. We used polyvinyl alcohol (PVA) particles of 250–420 μm as embolic material and embolized bilateral accessory meningeal arteries. Radiotherapy was performed 2 weeks after TAE. Total dose was 34 Gy delivered in 17 fractions. These techniques have been described in detail previously.[4]
Eyelid swelling resolved within a few days after TAE and gait disturbance had not deteriorated by discharge. Follow-up MR imaging about 5 months after therapy showed resolution of brainstem edema and swelling, leaving a lacuna in the right side of the pons [Figure 3]. Left hemiparesis was dramatically improved. We confirmed complete disappearance of the lesion on MR imaging 5 months later [Figure 4]. The patient refused follow-up angiography. As of the time of writing, the patient remains in a good clinical condition with no evidence of recurrence after the 18-month follow-up.
Figure 3.
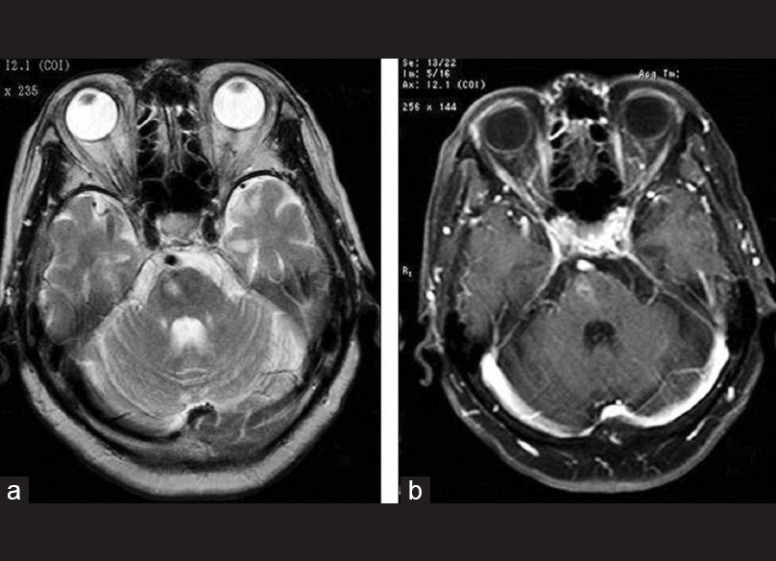
Follow-up (a) T2 and (b) post-gadolinium T1-weighted magnetic resonance images 5 months after therapy showing resolution of brainstem edema leaving with a small lacuna remaining on the right side of the pons
Figure 4.
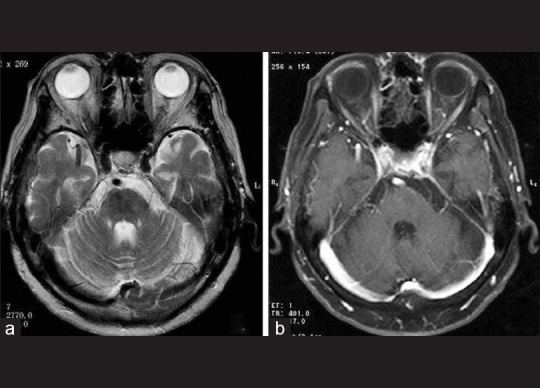
(a) T2 and (b) post-gadolinium T1-weighted magnetic resonance images 10 months after therapy showing complete disappearance of the lesion
DISCUSSION
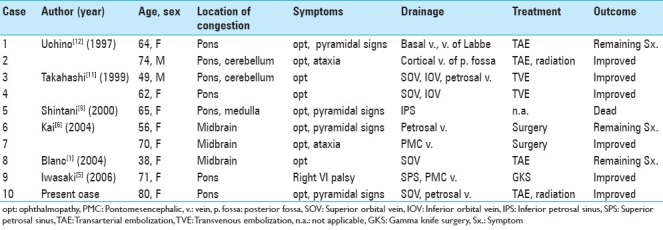
Brainstem venous congestion may develop in patients with DAVF of the posterior fossa.[8] However, brainstem venous congestion in the CS-DAVF is a rare[7] but serious complication.[1,9,12] Only isolated case reports have been described [Table 1], with no descriptions of large series. Some reports have described irreversible brainstem damage[1,12] or progression of symptoms leading to death.[8] The normal DWI before treatment may have indicated reversibility of the lesion in this case. CS-DAVF is thus a critical condition requiring immediate treatment.[1,5,12]
Table 1.
Summary of published cases
In the clinical diagnosis and treatment of common DAVF, patterns of venous drainage need to be considered.[1,3,5,7,10] In CS-DAVF with venous congestion of the brainstem, the petrosal sinus disappears or becomes incomplete on angiography, and this is considered to cause venous congestion of the brainstem.[5,12] Variations in the venous drainage have been reported, including the basal vein of Rosental,[5] cerebellar cortical vein,[6] deep Sylvian vein,[11] and superior petrosal sinus.[9] As cases without venous drainage to the posterior fossa have also been described,[1,11] the exact cause of venous congestion of the brainstem remains unclear. In our case, the route of drainage was through the SOV and petrosal vein. The venous hypertension within the superior petrosal vein, related to the arteriovenous shunting by the DAVF, was likely the cause of the pontine venous congestion.
Many treatment options have been presented for DAVF.[1,5,7,12] Spontaneous improvement can occur,[7] and in our case, the patient was initially followed on an outpatient basis. As symptoms in this case were exacerbating, invasive treatment was considered necessary. Transvenous embolization via the inferior petrosal sinus or superior ophthalmic vein can lead to complete resolution immediately;[7,11] however, it could not be achieved because of anatomical and technical aspects in this case. Another therapeutic option with radical open surgery,[6] radiotherapy,[5,12] and only TAE[1] has been described. Dilated glue as the embolic material may be accompanied by risk of infarction of normal brain tissue.[4] Another liquid agent, Onyx appears to offer many advantages over the other available embolic agents for the endovascular management of DAVF, however long-term follow-up is limited.[2] PVA, although often not as permanent as glue, is relatively easy to handle. Thus, we selected PVA particles as embolic material. TAE with PVA reduces the shunt flow and the symptoms can be improved immediately before radiotherapy,[4] and then complete fistula obliteration can be safely achieved with radiotherapy. Given the advanced age and general condition of the patient in our case, treatment with TAE followed by radiotherapy was considered one of the best options.
CONCLUSION
Once CS-DAVF with venous congestion of the brainstem has been definitively diagnosed, immediate therapy is warranted. Treatment with TAE followed by radiation may be an important option for elderly patients when transvenous or transarterial embolization is not an option.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/53/96076
Contributor Information
Takaaki Miyagishima, Email: miyagisi@med.gunma-u.ac.jp.
Tetsuo Hara, Email: thara@hosp.ncgm.go.jp.
Masato Inoue, Email: masatoinouens@yahoo.co.jp.
Naruhiko Terano, Email: n.terano@gmail.com.
Hiroyasu Ohno, Email: telomerases@yahoo.co.jp.
Kouichiro Okamoto, Email: kokamoto@hosp.ncgm.go.jp.
Kanehiro Hasuo, Email: khasuo@hosp.ncgm.go.jp.
REFERENCES
- 1.Blanc R, Maia Barros AD, Brugieres P, Méder JF, Gaston A. Cavernous sinus dural arteriovenous fistula complicated by edematous cerebral lesions from venous etiology. J Neuroradiol. 2004;31:220–4. doi: 10.1016/s0150-9861(04)96995-7. [DOI] [PubMed] [Google Scholar]
- 2.Carlson AP, Taylor CL, Yonas H. Treatment of dural arteriovenous fistula using ethylene vinyl alcohol (onyx) arterial embolization as the primary modality: short-term results. J Neurosurg. 2007;107:1120–5. doi: 10.3171/JNS-07/12/1120. [DOI] [PubMed] [Google Scholar]
- 3.Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671–80. doi: 10.1148/radiology.194.3.7862961. [DOI] [PubMed] [Google Scholar]
- 4.Hasuo K, Mizushima A, Matsumoto S, Uchino A, Uehara S, Miyoshi M, et al. Type D dural carotid-cavernous fistula. Results of combined treatment with irradiation and particulate embolization. Acta Radiol. 1996;37:294–8. doi: 10.1177/02841851960371P162. [DOI] [PubMed] [Google Scholar]
- 5.Iwasaki M, Murakami K, Tomita T, Numagami Y, Nishijima M. Cavernous dural arteriovenous fistula complicated by pontine venous congestion. A case report. Surg Neurol. 2006;65:516–9. doi: 10.1016/j.surneu.2005.06.044. [DOI] [PubMed] [Google Scholar]
- 6.Kai Y, Hamada JI, Morioka M, Yano S, Ushio Y. Brain stem venous congestion due to dural arteriovenous fistulas of the cavernous sinus. Acta Neurochir (Wien) 2004;146:1107–12. doi: 10.1007/s00701-004-0315-3. [DOI] [PubMed] [Google Scholar]
- 7.Miller NR. Diagnosis and management of dural carotid-cavernous sinus fistulas. Neurosurg Focus. 2007;23:E13. doi: 10.3171/FOC-07/11/E13. [DOI] [PubMed] [Google Scholar]
- 8.Probst EN, Christante L, Zeumer H. Brain-stem venous congestion due to a dural arteriovenous fistula in the posterior fossa. J Neurol. 1994;241:175–9. doi: 10.1007/BF00868346. [DOI] [PubMed] [Google Scholar]
- 9.Shintani S, Tsuruoka S, Shiigai T. Carotid-cavernous fistula with brainstem congestion mimicking tumor on MRI. Neurology. 2000;55:1929–31. doi: 10.1212/wnl.55.12.1929. [DOI] [PubMed] [Google Scholar]
- 10.Suh DC, Lee JH, Kim SJ, Chung SJ, Choi CG, Kim HJ, et al. New concept in cavernous sinus dural arteriovenous fistula correlation with presenting symptom and venous drainage patterns. Stroke. 2005;36:1134–9. doi: 10.1161/01.STR.0000166194.82027.63. [DOI] [PubMed] [Google Scholar]
- 11.Takahashi S, Tomura N, Watarai J, Mizoi K, Manabe H. Dural arteriovenous fistula of the cavernous sinus with venous congestion of the brainstem: Report of two cases. AJNR Am J Neuroradiol. 1999;20:886–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Uchino A, Kato A, Kuroda Y, Shimokawa S, Kudo S. Pontine venous congestion caused by dural carotid-cavernous fistula: Report of two cases. Eur Radiol. 1997;7:405–8. doi: 10.1007/s003300050175. [DOI] [PubMed] [Google Scholar]


