Abstract
Background:
Trigeminal neuralgia is most commonly caused by vascular compression at the trigeminal nerve (TN) root entry zone. Microvascular decompression (MVD) has been established as a useful treatment. Outcome depends on the correct identification of the compression site and its adequate decompression at surgery. Preoperative identification of neurovascular compression might predict which patients will benefit from MVD. Management of persistent or recurrent trigeminal neuralgia after an MVD is a baffling problem for neurosurgeons. An accurate neuroradiological evaluation of the TN padding following a failed MVD might help identify the underlying cause and plan further treatment.
Case description:
A 68-year-old female presented with a right-sided trigeminal neuralgia (V3) refractory to medical therapy. A high-resolution three-dimensional magnetic resonance imaging (3D MRI) study included fast imaging employing steady-state acquisition (FIESTA) and time of flight multiple overlapping thin slab acquisition (TOF MOTSA) sequences to evaluate the neurovascular anatomy in the cerebellopontine angle. An unambiguous compression of the right TN at the rostral-medial site by the superior cerebellar artery (SCA) was identified. The SCA loop compressing the TN was identical in location and configuration to that predicted in the preoperative study. After the MVD, the patient was relieved from her pain and a postoperative high-resolution 3D MRI study confirmed the appropriate placement of the Teflon implant between the TN and SCA.
Conclusion:
To our knowledge, this is the first report that characterizes the proper TN padding by high-resolution 3D MRI after trigeminal MVD. The present case also emphasizes the importance of performing a 3D MRI in patients with trigeminal neuralgia to anticipate the surgeon's view and predict the outcome after MVD.
Keywords: Fast imaging employing steady-state acquisition, three-dimensional magnetic resonance angiography, three-dimensional magnetic resonance imaging, time of flight multiple overlapping thin slab acquisition, trigeminal neuralgia
INTRODUCTION
Vascular compression at the trigeminal nerve (TN) root entry zone in the cerebellopotine angle (CPA) is the most common cause of trigeminal neuralgia.[8,15,22] The presence and severity degree of vascular compression found during the surgery has been correlated with a remarkable improvement after microvascular decompression (MVD).[4,21,26,29] For this reason, a precise preoperative evaluation of the relation between clinical symptoms and the vascular compression of the TN has potentially an important implication for the patient selection, surgical planning, and outcome prediction after MVD.[23,33] Resolution of conventional two-dimensional magnetic resonance imaging (MRI) techniques is typically insufficient to interpret the complexity of CPA anatomy.[10,31] The recent introduction of three-dimensional (3D) MRI techniques offers high-spatial-resolution images to evaluate the neurovascular structures of the posterior fossa. These techniques permit an accurate prediction of the anatomical point of trigeminal compression.[3,17,23,33] Even though high-resolution 3D MRI is useful before a primary MVD, these techniques have not been used to evaluate the correct surgical decompression of the TN after an MVD. We believe that 3D MRI might be also helpful to identify the cause of persistent or recurrent trigeminal neuralgia after a failed MVD, which is a challenging problem for neurosurgeons.[25]
Two high-resolution 3D MRI strategies can be used in an attempt to improve the detection of vascular compression of the TN. First one is using high-spatial-resolution 3D T2-weighted MRI sequences, such as the fast imaging employing steady-state acquisition (FIESTA) sequence.[6,28] The FIESTA sequence uses the T2 steady-state contrast mechanism to provide high signal to noise ratio images with strong signal from cerebrospinal fluid while suppressing background tissue for contrast and anatomical detail of small solid structures, such as cranial nerves and blood vessels. In addition, the ultra short repetition time (TR) and echo time (TE) enable extremely short acquisition times and the images can be easily reformatted in any plane with excellent quality.[2] Second one is using 3D time of flight (TOF) MR angiography, such as the multiple overlapping thin slab acquisition (MOTSA), that demonstrates fast flowing blood and provides excellent visualization of arterial anatomy. The TOF MOTSA MR angiography is a hybrid TOF MR angiography technique that overcomes the disadvantage of spin saturation, and therefore results in better images.[14] In spite of the very fine anatomical detail visible with 3D FIESTA MRI, there is no signal differentiation between vessels and nerves, and thus the identification of specific structures requires an appropriate anatomical knowledge. TOF MOTSA MR angiography can be used to objectively distinguish nerves from blood vessels. To the best of our knowledge, the present instance represents the first report that correlates the surgical findings and neuroimaging features using these 3D MRI sequences before and after an MVD of the TN in a patient with typical trigeminal neuralgia.
CASE REPORT
We present a 68-year-old woman with recurrent episodes of lancinating face pain in the region of the third branch of the right TN [Figure 1]. The pain attacks had initiated 5 years ago and during the last year had become resistant to the medical treatment.
Figure 1.
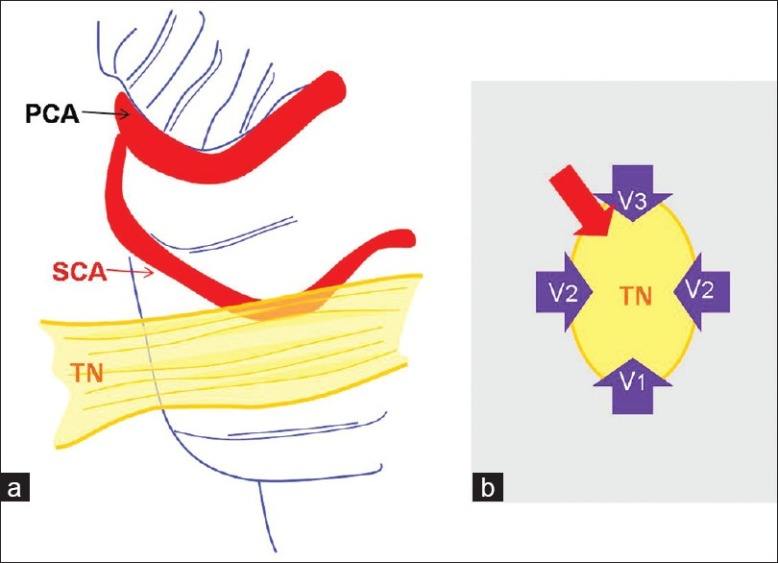
Vascular compression of the trigeminal nerve. (a) The superior cerebellar artery (SCA) can present an abnormal elongated loop causing compression on the trigeminal nerve (TN). This is the most common offending vessel of trigeminal neuralgia. (b) Clinical pathologic correlation of vascular compression on the TN: Rostral compression of the TN causes lower facial trigeminal neuralgia (V3), medial or lateral compression causes V2 pain, and compression of the caudal site causes V1 trigeminal neuralgia.[16] The present case had a rostral-medial compression by the SCA (red arrow). PCA, posterior cerebral artery
Imaging protocol
An MRI study was performed using a GE HDxT 1.5-T MR scanner and images were obtained using a dedicated commercially available high-resolution 8-channel head coil. Conventional T1- and T2-weighted studies were performed to prove that the patient had no brain tumor or demyelinating disease. In addition, we used the sequences 3D FIESTA and 3D TOF MOTSA to specifically evaluate the neurovascular anatomy of the CPA. Imaging using 3D FIESTA technique was centered on the pons in the region of the TN. Acquisition parameters for 3D FIESTA sequence included a TR of 4.8 msec, a TE of 2.2 msec, two excitations (NEX: 2), and a flip angle of 45°. The acquisition matrix was 224 × 224 for a field of view (FOV) 18 × 18 cm. The other imaging parameters included a bandwidth of 62.5 kHz per pixel, which gave a section thickness of 1.2 mm and an interslice distance of 0.6 mm. A total of 248 slices were obtained with an acquisition time of 4 min and 39 sec. MR angiography was performed by using 3D TOF MOTSA sequence with the following parameters: TR, 23 msec; TE, 2.9 msec; NEX, 1; flip angle, 20°; slice thickness, 1 mm; interslice distance, 0.5 mm; band width, 31.4 kHz; FOV, 22 × 22 cm; and matrix, 384 × 224. Ramp pulse, magnetization transference pulse, and fat saturation were used. A total of 208 slices were obtained. An acquisition scan time of 6 min and 43 sec was required. Both the 3D FIESTA and 3D TOF MOTSA images were acquired with the slabs oriented in the transverse direction. After data acquisition was completed, coronal and sagittal reformatted images were obtained by using a multiplanar reformation algorithm.
The preoperative MRI study [Figure 2a] showed that the site of compression of the right TN at its rostral-medial aspect was caused by the SCA. This is the nerve area corresponding to the anatomical location of the nerve fibers of the third branch [Figure 1b]. Therefore, the SCA was predicted as the offending vessel and the patient was scheduled for surgery.
Figure 2.
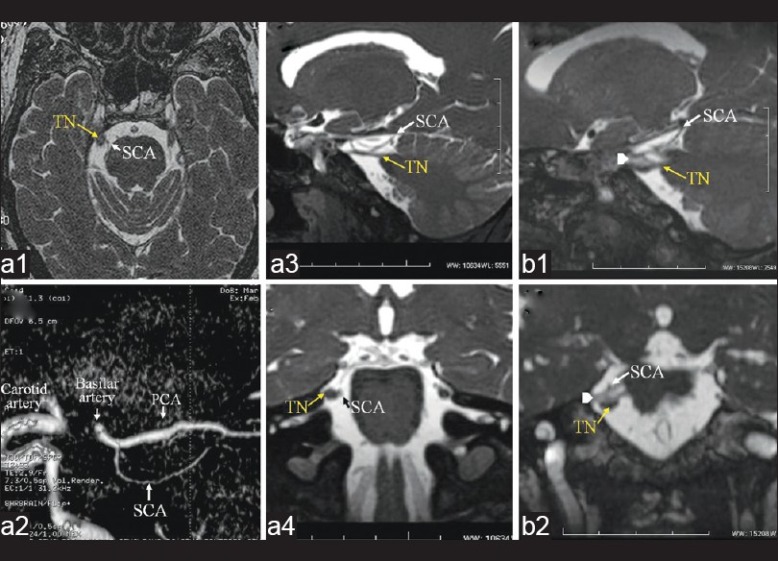
Preoperative (a) and postoperative (b) 3D FIESTA and 3D TOF MOTSA MRI scans. (a1) Transverse 3D FIESTA image at the level of pons. The small rounded structure medial to the trigeminal nerve (TN) corresponds to the right superior cerebellar artery (SCA). (a2) The SCA loop can be easily identified on the sagittal reformatted 3D TOF MOTSA image. Sagittal (a3) and coronal (a4) reformatted 3D FIESTA images demonstrate rostral-medial compression of the TN by the SCA loop. Postoperative sagittal (b1) and coronal (b2) reformatted 3D FIESTA images reveal the proper position of the Teflon implant (white arrowhead) between the SCA and the TN. PCA, posterior cerebral artery
Surgical treatment
An MVD was performed via a right retromastoid craniotomy to explore the root entry zone of the affected nerve [Figure 3a, b]. The intraoperative microscopic view was compared with the preoperative study, with special attention to identify the site of compression by the offending vessel. The SCA loop configuration and the point of neural compression were both identical to the neuroradiological findings observed on the FIESTA and MOTSA MRI sequences [Figure 3c].
Figure 3.
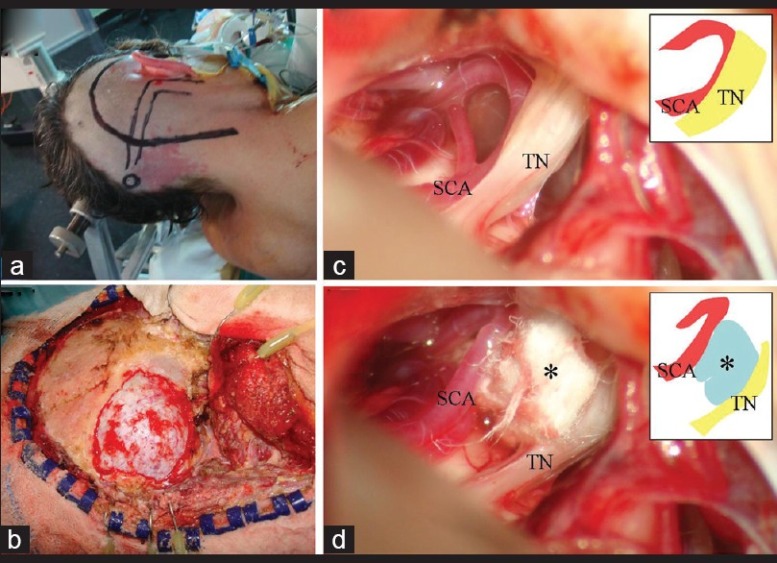
Operative photographs. (a) The patient was placed in the lateral position with an axillary roll and a three-point head holder attached to the head. The single line indicates the skin incision and the double line, the location of the transverse and sigmoid sinus. (b) The suboccipital retrosigmoid craniectomy was extended to the sigmoid and lateral sinuses. (c) The rostral-medial compression of the trigeminal nerve (TN) by the superior cerebellar artery (SCA) was confirmed at surgery. (d) The SCA loop was mobilized away from the nerve placing multiple Teflon felt implants (*) that were held in place with fibrin glue
Outcome and postoperative magnetic resonance imaging
The pain was eradicated after surgery and previous medical treatment was gradually suspended. A postoperative MRI study including the same 3D FIESTA protocol was obtained 1 month after the surgery with the aim to evaluate the correct placement of the Teflon implant. It was situated properly between the TN and the SCA, and its signal intensity was intermediate between that of cerebrospinal fluid and neurovascular structures [Figure 2b].
DISCUSSION
Elongated arterial loops, most commonly of the superior cerebellar artery (SCA), represent the usual cause of TN compression. In addition, small veins and arteries can also cause trigeminal neuralgia.[13,16,24] Trigeminal MVD can effectively relieve the pain among patients with typical trigeminal neuralgia when vascular compression of the TN is found and adequately solved at surgery.[4,5,9,29,32,34] However, any surgical procedure for posterior fossa exploration associates risks, especially among aged patients. Consequently, a thorough preoperative identification of the anatomical relationships between the TN and adjacent blood vessels is invaluable to plan the treatment strategy. MRI has been subjected to a rapid development with continuous improvements in the technology of three-dimensional studies, especially regarding high-resolution 3D T2-weighted MRI techniques and 3D MR angiography. These techniques provide a high spatial resolution to evaluate the neurovascular structures of the posterior fossa.[30]
Our case illustrates that 3D FIESTA MRI provides an optimal anatomic detail of cranial nerves and tiny vascular structures to identify the cause and site of TN compression among patients with unilateral typical trigeminal neuralgia. Because both vascular and nerves structures are visualized with a similar signal intensity using 3D FIESTA MRI, the additional information obtained with 3D MR angiography facilitates the differentiation between arteries and nerves and the proper identification of the offending vessel.[23,27] Reliability of neurovascular compression identified on preoperative 3D MRI is supported by our case and by recent prospective studies that have shown an identical compression at the operation in all the patients treated with MVD.[3,7,13,19,23,33,35] Identification of venous compression might be improved by using 3D contrast-enhanced MRI[3,13,20,35] and ultra-high-field MRI (3T) equipments.[20,23]
Management of persistent or recurrent trigeminal neuralgia after MVD is a challenging situation.[25] Decompression of a wrong nerve, formation of a Teflon granuloma, insertion of too much Teflon, and dislocation of the Teflon implant have been recognized as potential causes for a failed trigeminal MVD.[1,11,12,18] A precise neuroradiological exploration might identify the etiology and aid in the determination of the most appropriate treatment. To the best of our knowledge, this is the first report that provides high-resolution 3D MR images after an MVD. An appropriate decompression of the TN with the Teflon implant was confirmed, as expected after a successful MVD. Further studies are necessary to assess the usefulness of high-resolution 3D MRI techniques to evaluate the decompression of the TN following MVD.
CONCLUSION
This study emphasizes that a combination of 3D FIESTA MRI and 3D TOF MOTSA MR angiography is highly recommended in order to obtain an accurate preoperative evaluation in patients with typical trigeminal neuralgia. The excellent anatomical detail anticipates the surgeon's view, and therefore might help to distinguish patients who can benefit with MVD from those who cannot even if they present typical symptoms. High-spatial-resolution 3D MRI is also useful to confirm the adequate padding of the TN and might help identify the underlying causes of recurrent trigeminal neuralgia after a failed MVD.
ACKNOWLEDGMENT
We wish to express our gratefulness to Michelle Eraz for her linguistic assistance and a thorough review of the scientific style of the manuscript.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/50/96073
Contributor Information
Ruth Prieto, Email: rprieto29@hotmail.com.
José M. Pascual, Email: jmpasncj@hotmail.com.
Miguel Yus, Email: miguel_yus@yahoo.com.
Manuela Jorquera, Email: manuela.jorquera@gmail.com.
REFERENCES
- 1.Amador N, Pollock BE. Repeat posterior fossa exploration for patients with persistent or recurrent idiopathick trigeminal neuralgia. J Neurosurg. 2008;108:916–20. doi: 10.3171/JNS/2008/108/5/0916. [DOI] [PubMed] [Google Scholar]
- 2.Amemiya S, Aoki S, Ohtomo K. Cranial nerve assessment in cavernous sinus tumors with contrast-enhanced 3D fast-imaging employing steady-state acquisition MR imaging. Neuroradiology. 2009;51:467–70. doi: 10.1007/s00234-009-0513-z. [DOI] [PubMed] [Google Scholar]
- 3.Anderson VC, Berryhill PC, Sandquist MA, Ciaverella DP, Nesbit GM, Burchiel KJ. High-resolution three-dimensional spoiled gradient-recalled imaging in the evaluation of neurovascular compression in patients with trigeminal neuralgia: A double-blind pilot study. Neurosurgery. 2006;56:666–73. doi: 10.1227/01.NEU.0000197117.34888.DE. [DOI] [PubMed] [Google Scholar]
- 4.Barker FG, 2nd, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD. The long-term outcome of microvascular decompression for trigeminal reuralgia. N Engl J Med. 1996;334:1077–83. doi: 10.1056/NEJM199604253341701. [DOI] [PubMed] [Google Scholar]
- 5.Benderson JB, Wilson CB. Evaluation of microvascular decompression and partial sensory rhizotomy in 252 cases of trigeminal neuralgia. J Neurosurg. 1989;71:359–67. doi: 10.3171/jns.1989.71.3.0359. [DOI] [PubMed] [Google Scholar]
- 6.Benes L, Shiratori K, Gurschi M, Sure U, Tirakotai E, Krischek B, et al. Is preoperative high-resolution magnetic resonance imaging accurate in predicting neurovascular compression in patients with trigeminal neuralgia? A single-blind study. Neurosurg Rev. 2005;28:131–6. doi: 10.1007/s10143-004-0372-3. [DOI] [PubMed] [Google Scholar]
- 7.Boecher-Schwarz HG, Bruehl K, Kessel G, Guenthner M, Perneczky A, Stoeter P. Sensitivity and specificity of MRA in the diagnosis of neurovascular compression in patients with trigeminal neuralgia: A correlation of MRA and surgical findings. Neuroradiology. 1998;40:88–95. doi: 10.1007/s002340050546. [DOI] [PubMed] [Google Scholar]
- 8.Boto GR. [Trigeminal neuralgia] Neurocirugia. 2010;21:361–72. [Article in Spanish] [PubMed] [Google Scholar]
- 9.Broggi G, Ferroli P, Franzini A, Servello D, Dones I. Microvascular decompression for trigeminal neuralgia: Comments on a series of 250 cases, including 10 patients with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2000;68:59–64. doi: 10.1136/jnnp.68.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caillet H, Delvalle A, Doydon D, Sigal R, Francke JP, Halimi P, et al. Visibility of cranial nerves at MRI. J Neuroradiol. 1990;17:289–302. [PubMed] [Google Scholar]
- 11.Capelle HH, Brandis A, Tschan CA, Krauss JK. Treatment of recurrent trigeminal neuralgia due to Teflon granuloma. J Headache Pain. 2010;11:339–44. doi: 10.1007/s10194-010-0213-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho DY, Chang CG, Wang YC, Wang FH, Shen CC, Yang DY. Repeat operations in failed microvascular decompression for trigeminal neuralgia. Neurosurgery. 1994;35:665–70. doi: 10.1227/00006123-199410000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Chun-Cheng Q, Qing-Shi Z, Ji-Quing Z, Zhi-Gang W. A single-blinded pilot study assessing neurovascular contact by using high-resolution MR imaging in patients with trigeminal neuralgia. Eur J Radiol. 2008;69:459–63. doi: 10.1016/j.ejrad.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 14.Davis WL, Blatter DD, Harnsberger HR, Parker DL. Intracranial MR angiography: Comparison of single-volume three-dimensional time-of-flight and multiple overlapping thin slab acquisition techniques. AJR Am J Roentgenol. 1994;163:915–20. doi: 10.2214/ajr.163.4.8092035. [DOI] [PubMed] [Google Scholar]
- 15.Jannetta PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg. 1967;26:159–62. doi: 10.3171/jns.1967.26.1part2.0159. [DOI] [PubMed] [Google Scholar]
- 16.Jannetta PJ. Trigeminal disorders. Supralateral exposure of the trigeminal nerve in the cerebellopontine angle for microvascular decompression. In: Apuzzo ML, editor. Brain Surgery. New York: Complication avoidance and management; 1993. pp. 2085–96. [Google Scholar]
- 17.Kumon Y, Sakaki S, Kohno K, Ohta S, Ohue S, Miki H. Three-dimensional imaging for presentation of the causative vessels in patients with hemifacial spasm and trigeminal neuralgia. Surg Neurol. 1997;47:178–84. doi: 10.1016/s0090-3019(96)00364-3. [DOI] [PubMed] [Google Scholar]
- 18.Kureshi SA, Wilkins RH. Posterior fossa reexploration for persistent or recurrent trigeminal neuralgia or hemifacial spasm: Surgical findings and therapeutic implications. Neurosurgery. 1998;43:1111–7. doi: 10.1097/00006123-199811000-00061. [DOI] [PubMed] [Google Scholar]
- 19.Leal PR, Hermier M, Froment JC, Souza MA, Cristino-Filho G, Sindou M. Preoperative demonstration of the neurovascular compression characteristics with special emphasis on the degree of compression, using high-resolution magnetic resonance imaging: A prospective study, with comparison to surgical findings, in 100 consecutive patients who underwent microvascular decompression for trigeminal neuralgia. Acta Neurochir (Wien) 2010;152:817–25. doi: 10.1007/s00701-009-0588-7. [DOI] [PubMed] [Google Scholar]
- 20.Leal PP, Hermier M, Souza MA, Cristino-Filho G, Froment JC, Sindou M. Visualization of vascular compression of the trigeminal nerve with high-resolution 3T MRI: A prospective study comparing preoperative imaging analysis to surgical findings in 40 consecutive patients who underwent microvascular decompression for trigeminal neuralgia. Neurosurgery. 2011;69:15–26. doi: 10.1227/NEU.0b013e318212bafa. [DOI] [PubMed] [Google Scholar]
- 21.Li ST, Pan Q, Liu N, Shen F, Liu Z, Guan Y. Trigeminal neuralgia: What are the important factors for good operative outcomes with microvascular decompression. Surg Neurol. 2004;62:400–5. doi: 10.1016/j.surneu.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 22.Love S, Coakham HB. Trigeminal neuralgia: Pathology and pathogenesis. Brain. 2001;124:2347–60. doi: 10.1093/brain/124.12.2347. [DOI] [PubMed] [Google Scholar]
- 23.Miller J, Acar F, Hamilton B, Burchiel K. Preoperative visualization of neurovascular anatomy in trigeminal neuralgia. J Neurosurg. 2008;108:477–82. doi: 10.3171/JNS/2008/108/3/0477. [DOI] [PubMed] [Google Scholar]
- 24.Patel NK, Aquilina K, Clarke Y, Renowden SA, Coakham HB. How accurate is magnetic resonance angiography in predicting neurovascular compression in patients with trigeminal neuralgia? A prospective, single-blinded comparative study. Br J Neurosurg. 2003;17:60–4. [PubMed] [Google Scholar]
- 25.Pollock BE, Stein KJ. Surgical management of trigeminal neuralgia patients with recurrent or persistent pain despite three or more prior operations. World Neurosurg. 2010;73:523–8. doi: 10.1016/j.wneu.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 26.Pollock BE. Surgical management of medically refractory trigeminal neuralgia. Curr Neurol Neurosci Rep. 2012;12:125–31. doi: 10.1007/s11910-011-0242-7. [DOI] [PubMed] [Google Scholar]
- 27.Schwartz MS, Brackmann DE, Wilkinson EP, Go JL, Santos F. Trigeminal neuralgia resulting from auditory brainstem implant cable compression. J Neurosurg. 2011;14:186–8. doi: 10.3171/2010.5.JNS091709. [DOI] [PubMed] [Google Scholar]
- 28.Satoh T, Onoda K, Date I. Preoperative simulation for microvascular decompression in patients with idiopatic trigeminal neuralgia: Visualization with three-dimensional magnetic resonance cisternogram and angiogram fusion imaging. Neurosurgery. 2007;60:104–14. doi: 10.1227/01.NEU.0000249213.34838.C9. [DOI] [PubMed] [Google Scholar]
- 29.Sindou M, Leston J, Decullier E, Chapuis F. Microvascular decompression for trigeminal neuralgia: Long-term effectiveness and prognostic factors in a series of 362 consecutive patients with clear-cut neurovascular conflicts who underwent pure decompression. J Neurosurg. 2007;107:1144–53. doi: 10.3171/JNS-07/12/1144. [DOI] [PubMed] [Google Scholar]
- 30.Tanaka T, Morimoto Y, Shiiba S, Sakamoto E, Kito S, Matsufuji Y, et al. Utility of magnetic resonance cisternography using three-dimensional fast axymetric spin-echo sequences with multiplanar reconstruction: The evaluation of sites of neurovascular compression of the trigeminal nerve. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:215–25. doi: 10.1016/j.tripleo.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Tash RR, Sze G, Leslie DR. Trigeminal neuralgia: MR imaging features. Radiology. 1989;172:767–70. doi: 10.1148/radiology.172.3.2772186. [DOI] [PubMed] [Google Scholar]
- 32.Tronnier VM, Rasche D, Hamer J, Kienle AL, Kunze S. Treatment of idiopathic trigeminal neuralgia: Comparison of long-term outcome after radiofrequency rhizotomy and microvascular decompression. Neurosurgery. 2001;48:1261–7. [PubMed] [Google Scholar]
- 33.Yoshino N, Akimoto H, Yamada I, Nagaoka T, Tetsumura A, Kurabayashi T, et al. Trigeminal neuralgia: Evaluation of neuralgic manifestation and site of neurovascular compression with 3D CISS MR imaging and MR angiography. Radiology. 2003;228:539–45. doi: 10.1148/radiol.2282020439. [DOI] [PubMed] [Google Scholar]
- 34.Zakrzewska JM, Lopez B, Kim SE, Coakham HB. Patients reports of satisfaction after microvascular decompression and partial sensory rhizotomy for trigeminal neuralgia. Neurosurgery. 2005;56:1304–11. doi: 10.1227/01.neu.0000159883.35957.e0. [DOI] [PubMed] [Google Scholar]
- 35.Zhou Q, Liu Z, Li C, Qu C, Ni S, Zeng Q. Preoperative evaluation of neurovascular relationship by using contrast-enhanced and unenhanced 3D time-of-flight MR angiography in patients with trigeminal neuralgia. Acta Radiol. 2011;52:894–8. doi: 10.1258/ar.2011.110195. [DOI] [PubMed] [Google Scholar]


