Abstract
Food insecurity is defined as limited or uncertain ability to acquire nutritionally adequate and safe foods in socially acceptable ways. The United States Department of Agriculture (USDA) has divided food insecurity into two categories: low food security and very low food security. Low food security is characterized by irregular access to food, binge eating when food is available, overconsumption of energy-dense foods, obesity, and even type 2 diabetes. This type of food insecurity occurs in impoverished urban areas of high-income countries such as the United States. In contrast, very low food security is distinctly different from low food security and can lead to undernutrition and frank starvation. Very low food security is found in developing countries in both rural areas and urban slums. In these countries, food insecurity is often exacerbated by natural disasters and climate changes that compromise food availability. With a focus on the social, economic, and behavioral factors that promote obesity and cardiometabolic disease in food insecure households in the United States, this review will first define the key terms and concepts associated with food insecurity. Then, the characteristics of food insecure households and the relationship to cardiometabolic disease will be discussed. Finally, the cardiac consequences of food insecurity in developing countries will be briefly described.
Keywords: Food insecurity, obesity, malnutrition, overnutrition, undernutrition, hunger
Introduction
Cardiometabolic disease is defined by a cluster of risk factors that promote the development of type 2 diabetes and cardiovascular disease [1]. These risk factors are central obesity, insulin resistance, hyperglycemia, dyslipidemia, and hypertension. Since food insecurity is strongly associated with these risk factors, food insecurity is a risk factor for cardiometabolic disease. Food insecurity is defined as “limited or uncertain ability to acquire nutritionally adequate and safe foods in socially acceptable ways” [2].
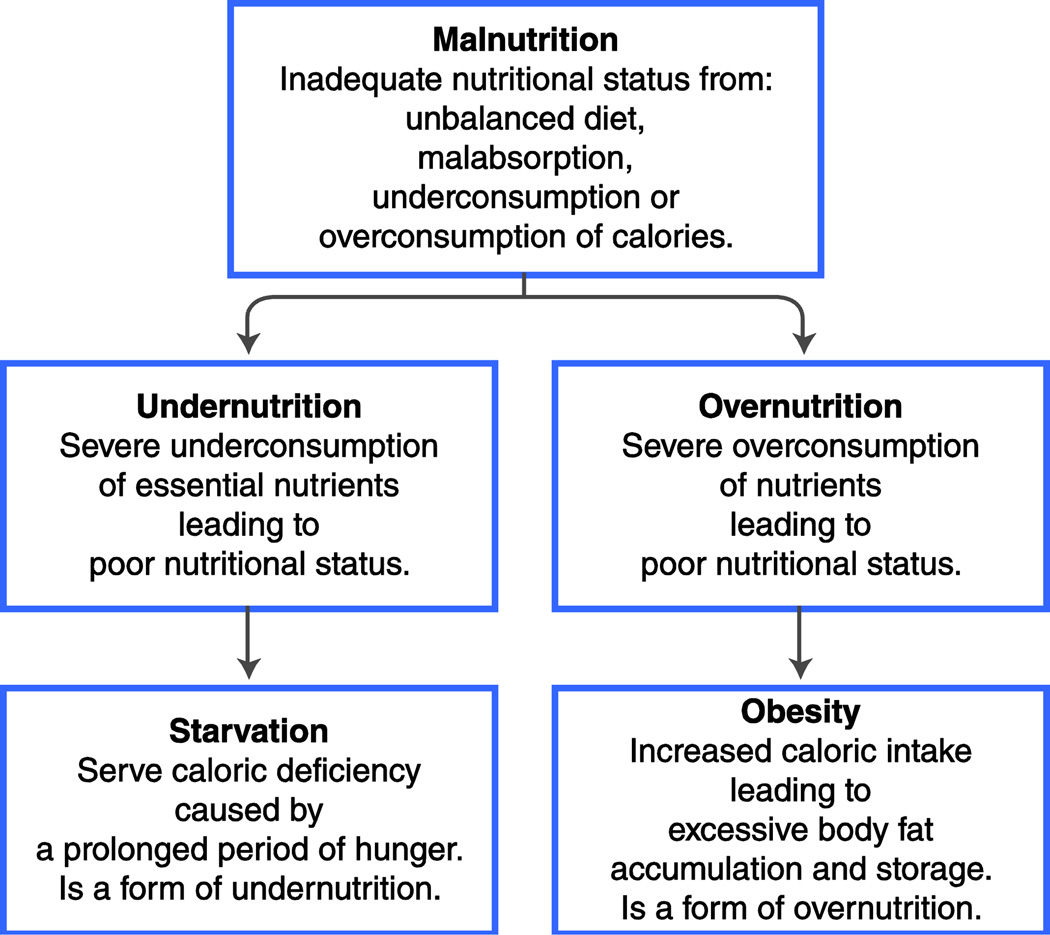
Food insecurity occurs in both wealthy countries and developing nations. A consequence of food insecurity in low-income countries is malnutrition, defined as inadequate nutritional status caused by an unbalanced diet, malabsorption, and underconsumption or overconsumption of calories (Fig. 1). In low-income countries, food insecurity is associated with undernutrition and starvation [3, 4]. Undernutrition is a type of malnutrition characterized by a severe underconsumption of essential nutrients leading to poor nutritional status and increasing the risk of nutritional diseases such as marasmus and kwashiorkor. An undernourished person who experiences hunger for a prolonged period of time can also suffer from starvation, a form of undernutrition. Wasting, stunting, and underweight from starvation can also cause abnormalities in heart muscle, heart rhythm, and ultimately congestive heart failure [5].
Figure 1.
The two types of malnutrition.
In contrast, food insecurity in affluent countries has been linked to a different less obvious type of malnutrition, specifically overnutrition. Overnutrition occurs when there is a severe overconsumption of nutrients [6]. Obesity is the most recognized form of overnutrition and is characterized by increased caloric intake and excessive accumulation and storage of fat. The impact of food insecurity on overnutrition and cardiometabolic disease is greater in women than men. Furthermore, when food insecurity occurs during pregnancy there can be long-term consequences for the mother and child. Epidemiologists, social scientists, and medical researchers have come to realize that food insecurity and unhealthy dietary patterns, lead to obesity, cardiovascular disease (CVD), and type 2 diabetes.
Food Insecurity in the United States
In response to the National Nutrition Monitoring and Related Research Act of 1990, the United States Department of Agriculture (USDA) and United States Department of Health and Human Services created a measurement tool to assess food insecurity, specifically the United States Household Food Security Survey Module. Since 1995, food insecurity data in the United States has been collected by the Economic Research Service (ERS) of USDA. As of 2006, the USDA divided food insecurity into two categories: low food security and very low food security (Table 1). In the United States, low food security is more common than very low food security. Low food security most often occurs in rural areas and low-income urban neighborhoods [7••]. People with low food security are more likely to be overweight and obese due to the decreased intake of fruits, vegetables, and fiber and increased intake of energy-dense foods, including foods rich in fat and sugar [8••, 9]. In the United States, very low food security occurs less often than low food security. Altogether, the prevalence in the United States of low and very low food security is 9.1% and 5.4%, respectively [10].
Table 1.
Terminology used in this article
| Term | Definition |
|---|---|
| Food Securitya | “Access by all people at all times to enough nutritious food for an active and healthy life.” |
| a. High Food Securitya | “Households that had no problems, or anxiety about, consistently accessing adequate food.” |
| b. Marginal Food Secuirtya | “Households that had problems at times, or anxiety about, accessing adequate food, but the quality, variety, and quantity of their food intake were not substantially reduced.” |
| Food Insecurityb | “Limited or uncertain ability to acquire nutritionally adequate and safe foods in socially acceptable ways.” |
| c. Low Food Security a | “Households that reduced the quality, variety and desirability of their diets, but the quantity of food intake and normal eating patterns were not substantially disrupted.” |
| d. Very Low Food Security a | “At times during the year, eating patterns of one or more household members were disrupted and food intake reduced because the household lacked money and other resources of food.” |
| Hungerc | “A potential consequence of food insecurity that, because of prolonged, involuntary lack of food, results in discomfort, illness, weakness, or pain that goes beyond the usual uneasy sensation.” |
| Food Desertd | “Area in the United States with limited access to affordable and nutritious food, particularly such an area composed of predominantly lower income neighborhoods and communities.” |
| Federal Poverty Guidelines e | Is the minimum income necessary to cover all the expenses of a family. The measurement is used to determine poverty status in the United States. It is based on the poverty thresholds of the Census, size of the family and the age of the members. |
Defined by US Department of Agriculture.
Defined by Anderson 1990 [2].
Defined by US Department of Agriculture and the Committee on National Statistics of the National Academies.
Defined by Farm Bill (2008), US Congress, Title VI, Sec. 7527.
Adapted from the US Department of Health and Human Services.
In the first decade of the 21st century, the prevalence of food insecure households in the United States markedly increased from 10.1% in 1999 to 14.7% in 2009 [10]. Unemployment and rising food costs were two factors that contributed to this increase [11]. Other risk factors for food insecurity were low income, living in a single-mother household with children less than 6 years of age, and self-identification as black or Hispanic [12–15, 16•]. Households living above federal poverty guidelines may also experience food insecurity in the presence of an unexpected event, such as marital separation, exhaustion of savings, and unemployment [10, 17].
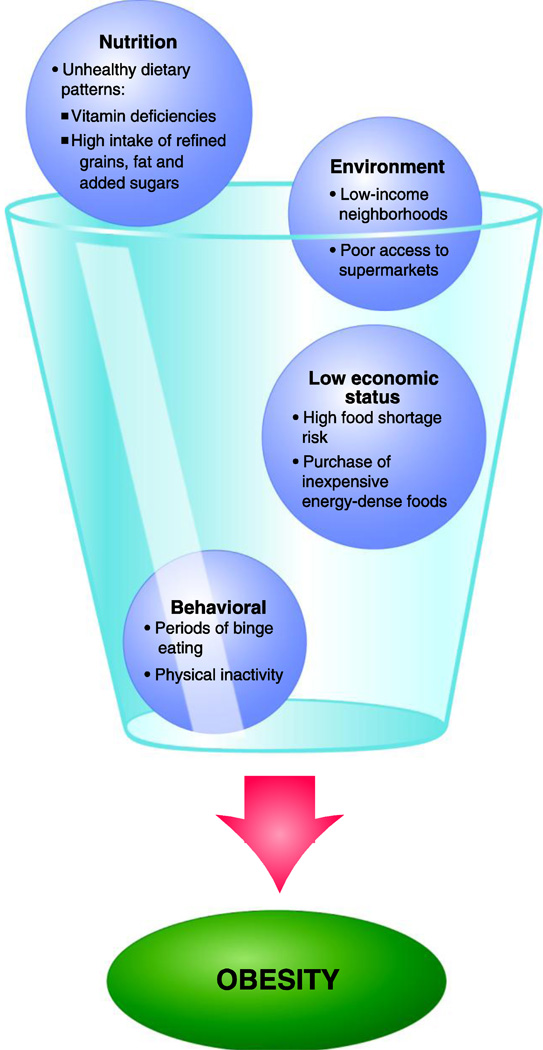
Food insecure households are characterized by low education levels, physical inactivity, and a high risk for obesity (Fig. 2) [18•, 19•, 20]. This risk is often exacerbated by behavioral and lifestyle factors such as skipping meals, binge eating when food is available, and an overall unhealthy dietary pattern. As energy-dense foods are often less expensive than healthier foods such as fruits, vegetables, and whole-grain foods, heads of low-income households often purchase food of poor nutritional quality [7••, 8••, 13]. However, cost is not the only factor. Low-income consumers may choose to buy food outside the house because they live in housing with inadequate kitchens. Another factor influencing the food choices of low-income individuals is the palatability of energy-dense foods [20, 21]. Overall, the absence of health education combined with physical inactivity and the consumption of readily accessible, highly palatable foods rich in fat and sugar can lead to weight gain and obesity related diseases (Fig. 2).
Figure 2.
Factors relating food insecurity to the development of obesity.
The environment surrounding food insecure households also plays a key role in cardiometabolic disease risk. Food insecure households often lack neighborhood grocery stores. In fact, many low-income neighborhoods are in food deserts, which are residential areas located more than 1 mile from an affordable grocery store. Larson et al. [22••] has reported that local access to food has a major impact on the food choices of residents. Specifically, low-income neighborhoods have a paucity of supermarkets and higher density of fast-food restaurants and corner stores that sell calorie-rich foods. In contrast, wealthy neighborhoods have many supermarkets with healthy food options and less obesity [19•, 23, 24]. However, other investigators report no association between obesity risk and the fast-food availability in low-income neighborhoods [7••, 25]. Yet, in support of Larson et al. [22••], intervention studies have shown that either opening new grocery stores or changing the food options available in the corner store positively impacts food choices [26, 27]. Under these new circumstances, low-income customers increase their fruit and vegetable consumption [26]. Overall, increased health literacy combined with improved supermarket access, enhanced neighborhood safety, and more exercise facilities leads to less obesity-related health disparities.
Diabetes is a major health problem in the United States. Food insecurity may contribute to the high prevalence of type 2 diabetes in low-income areas [28, 29, 30, 31••]. In addition, diabetic patients who experience food insecurity have worse glycemic control than their food secure counterparts [29, 30]. Diabetes control in food insecure individuals is often made more difficult by concomitant obesity, insulin resistance, physical inactivity, and high intake of refined grains and sugar. Furthermore, low educational attainment, which is common in food insecure households, is highly correlated with poor adherence to diabetes treatment and control [29, 31••].
Smoking is on the decline in the United States. However, smoking is common in low-income, food insecure households. Smoking is strongly associated with poverty and a lack of higher education [13, 18, 32, 33•]. The prevalence of tobacco use is 28.9% among adults living under the federal poverty guidelines compared to 18.3% for those who live above the federal poverty guidelines [34]. Low-income smokers may have less money available to buy food because they are spending income on the purchase of cigarettes. Consequently, low-income smokers are more likely to purchase inexpensive, obesogenic foods. Overall, due to the combined effect of unhealthy dietary patterns and the potentiating effect of smoking on the development of arterial plaques [35], food insecure smokers are at great risk of cardiometabolic disease.
Food Insecurity in the United States and the Link with Obesity, Diabetes and Heart Disease: Emphasis on Women and Children
Food insecurity is not associated with obesity in men, but food insecurity promotes obesity in women and adolescents [36–38]. However, for children the association between obesity and food insecurity is less clear [39]. Based on participation in the Supplemental Nutrition Assistance Program (SNAP), women who receive food stamps are more likely to be overweight and centrally obese than food secure women [40]. Yet, an association between SNAP participation and obesity in children has not been found [41]. It is possible that mothers eat less nourishing, less expensive food in order to maintain safe and adequate nutrition for their children [16•, 42]. Nonetheless, the relationship between obesity and the use of food stamps is complicated. Families receiving food stamps often consume their monthly allotment in less than 30 days. This reality may lead to binge eating behavior when food is available [43]. In addition, when food is scarce, low-income households may increase their reliance on inexpensive, energy-dense foods.
When addressing women’s health, the impact of pregnancy must be considered. Food insecurity during pregnancy increases the risk of both weight gain and gestational diabetes mellitus [44]. Pregnant women with gestational diabetes need long-term follow up and early intervention in order to ameliorate the risk of subsequently developing type 2 diabetes and cardiovascular disease [45]. Furthermore, if mothers have either gestational diabetes mellitus or type 1 diabetes during pregnancy, their offspring are at higher risk to develop pre-diabetes or type 2 diabetes as adults [46]. A longitudinal study conducted in Canadian food insecure households reported that infants born with either lower or higher weight than expected were more likely to develop childhood obesity than infants of normal birth weight [47]. Therefore, food insecure pregnant women are at enhanced risk for gestational diabetes and their children are at greater risk for childhood obesity and type 2 diabetes.
Independent of the effect of the in utero environment, food insecurity during childhood can also affect the development and overall health of children. Food insecure youth may experience delayed growth, depression, psychological problems, and poor academic performance [13, 43]. A particularly vulnerable group is immigrant children. Immigrant households are more likely to be food insecure than households with US-born mothers. Furthermore, both food insecurity rates and childhood obesity rates are higher among minority groups.
Although the direct association between food insecurity and high body mass index (BMI) among children and adolescents has been extensively investigated, the relationship is stronger in adolescents than children [33•]. Nonetheless, it is generally believed that children in food insecure households are at risk for the subsequent development of obesity as adolescents. Hence, obesity in both children and adolescents has become a national problem [48]. In the past 30 years, the prevalence of obesity increased from 7% to 20% for children between the ages of 6 and 11, and 5% to 18% for youth between the ages of 12 and 19 years [49, 50]. Therefore, risk factors for cardiovascular disease that are common in adults, such as dyslipidemia, hypertension, and impaired glucose tolerance, are now present in obese children and adolescents [51–53].
Food Insecurity in the Developing World
In developing nations, food insecurity is an enormous, multifaceted complex problem. It is estimated that the number of undernourished people in the world in 2010 was 925 million [54]. The regions of the world with the highest rates of undernourishment are in the Asia-Pacific rim and sub-Saharan Africa. Both low and very low food insecurity have to be considered.
Low food security is found in newly industrialized countries where socioeconomic and demographic changes have promoted economic growth and internal migration from rural to urban areas [9]. Low food insecurity is characteristic of disadvantaged, low-income, urban neighborhoods and slums. In contrast, very low food security is a more common situation in less industrialized countries where food availability is directly tied to agricultural conditions. In these countries, food shortages may be precipitated by natural disasters, climate change, and human-induced disasters including war [54, 55].
Underweight, stunting, and wasting are some of the health consequences of prolonged hunger and undernutrition [3]. Moreover, severely malnourished people are at high risk of cardiac complications. Clinical signs of undernourishment related to poor heart health-include bradycardia, low blood pressure, and decreased blood volume. In addition, extreme protein deficiency can significantly weaken the heart by reducing the myocardial muscle mass and overall cardiac size. Myocardial atrophy is highly associated with sudden and otherwise unexplained death [5].
Conclusions
Food insecurity is a worldwide problem that can lead not only to malnutrition, but also to obesity and the development of cardiometabolic disease. In affluent countries such as the United States, low food security is contributing to the high prevalence of obesity, cardiovascular disease, and diabetes. To reverse food insecurity, food deserts have to be eliminated and effective public health policies instituted to increase the opportunity for healthy eating and a healthy, physically active lifestyle. In developing countries where very low food security is common, political, social, environmental, and economic conditions have to be stabilized, and then distinct cardiac implications and other conditions related to undernourishment can be addressed. With each country working within its borders and simultaneously contributing to international efforts, the elimination of food insecurity should be an achievable 21st century goal.
Acknowledgments
Darleen C. Castillo, Natalie LM Ramsey, Sophia SK Yu, Madia Ricks, and Anne E. Sumner are supported by the intramural program of NIDDK, NIH. Sophia SK Yu is also supported through the Clinical Research Training Program, a public-private partnership supported jointly by the NIH and Pfizer Inc (via a grant to the Foundation for NIH from Pfizer Inc). Amber B. Courville is supported by the Clinical Center, NIH.
Footnotes
Disclosure
No conflicts of interest relevant to this article were reported.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as:
• Of importance
• • Of major importance
- 1.Brunzell JD, Davidson M, Furberg CD, et al. Lipoprotein management in patients with cardiometabolic risk: consensus conference report from the American Diabetes Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2008 Apr 15;51(15):1512–1524. doi: 10.1016/j.jacc.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 2.Anderson SA. Core indicators of nutritional state for difficult-to-sample populations. J Nutr. 1990 Nov;120(Suppl 11):1559–1600. doi: 10.1093/jn/120.suppl_11.1555. [DOI] [PubMed] [Google Scholar]
- 3.Pasricha SR, Biggs BA. Undernutrition among children in South and South-East Asia. J Paediatr Child Health. 2010 Sep;46(9):497–503. doi: 10.1111/j.1440-1754.2010.01839.x. [DOI] [PubMed] [Google Scholar]
- 4.Tanumihardjo SA, Anderson C, Kaufer-Horwitz M, et al. Poverty, obesity, and malnutrition: an international perspective recognizing the paradox. J Am Diet Assoc. 2007 Nov;107(11):1966–1972. doi: 10.1016/j.jada.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Webb JG, Kiess MC, Chan-Yan CC. Malnutrition and the heart. Cmaj. 1986 Oct 1;135(7):753–758. [PMC free article] [PubMed] [Google Scholar]
- 6.Sarlio-Lahteenkorva S, Lahelma E. Food insecurity is associated with past and present economic disadvantage and body mass index. J Nutr. 2001 Nov;131(11):2880–2884. doi: 10.1093/jn/131.11.2880. [DOI] [PubMed] [Google Scholar]
- 7. Ploeg MV, Breneman V, Farrigan T, et al. Access to affordable and nutritious food: measuring and understanding food deserts and their consequences. Washington, DC: US Department of Agriculture, Economic Research Service; 2009. Publication No. (AP-036). This is a complete report made by the US Department of Agriculture on food insecurity and its consequences.
- 8. Popkin BM. Contemporary nutritional transition: determinants of diet and its impact on body composition. Proc Nutr Soc. 2011 Feb;70(1):82–91. doi: 10.1017/S0029665110003903.. This article discusses nutritional transition in global dietary patterns over the past few years and how this energy imbalance affects body composition.
- 9.Shariff ZM, Khor GL. Obesity and household food insecurity: evidence from a sample of rural households in Malaysia. Eur.J Clin Nutr. 2005 Sep;59(9):1049–1058. doi: 10.1038/sj.ejcn.1602210. [DOI] [PubMed] [Google Scholar]
- 10.Nord M, Coleman-Jensen A, Andrews M, Carlson S. Household food security in the United States. Washington D.C.: US Department of Agriculture, Economic Research Service; 2010. Report No. (ERR-108) [Google Scholar]
- 11.Naylor RL, Falcon WP. Food security in an era of economic volatility. Popul Dev Rev. 2010;36(4):693–723. doi: 10.1111/j.1728-4457.2010.00354.x. [DOI] [PubMed] [Google Scholar]
- 12.Laraia BA, Borja JB, Bentley ME. Grandmothers, fathers, and depressive symptoms are associated with food insecurity among low-income first-time African-American mothers in North Carolina. J Am Diet Assoc. 2009 Jun;109(6):1042–1047. doi: 10.1016/j.jada.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holben DH. Position of the American Dietetic Association: food insecurity in the United States. J Am Diet Assoc. 2010 Sep;110(9):1368–1377. doi: 10.1016/j.jada.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 14.Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006 Jan;136(1):177–182. doi: 10.1093/jn/136.1.177. [DOI] [PubMed] [Google Scholar]
- 15.Cook J, Jeng K. Child food insecurity: the economic impact on our nation: Feeding America. 2009 [Google Scholar]
- 16. Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J Community Health. 2012 Feb;37(1):253–264. doi: 10.1007/s10900-011-9420-4.. This article is a review of recent literature on food insecurity and its relationship with obesity.
- 17.Institute of Medicine. Hunger and obesity: understanding a food insecurity paradigm: workshop summary. The National Academies Press; 2011. [PubMed] [Google Scholar]
- 18. Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol. 2010 Aug;36:349–370. doi: 10.1146/annurev.soc.012809.102529.. This stellar review article examines factors that influence the inverse relationship of unhealthy lifestyle and socioeconomic status.
- 19. Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7–20. doi: 10.1093/epirev/mxp005.. This review article discusses the relationship between the built environment and obesity-related health disparities of disadvantaged populations
- 20.Drewnowski A. Obesity, diets, and social inequalities. Nutr Rev. 2009 May;67(1) Suppl 1:S36–S39. doi: 10.1111/j.1753-4887.2009.00157.x. [DOI] [PubMed] [Google Scholar]
- 21.Offer A, Pechey R, Ulijaszek S. Obesity under affluence varies by welfare regimes: the effect of fast food, insecurity, and inequality. Econ Hum Biol. 2010 Dec;8(3):297–308. doi: 10.1016/j.ehb.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 22. Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009 Jan;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025.. This superb review summarizes the findings of over 50 research studies that have examined neighborhood differences and their influence in access to food, dietary intake, and obesity.
- 23.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethn Dis. 2006 Winter;16(1):275–280. [PubMed] [Google Scholar]
- 24.Morland K, Filomena S. Disparities in the availability of fruits and vegetables between racially segregated urban neighbourhoods. Public Health Nutr. 2007 Dec;10(12):1481–1489. doi: 10.1017/S1368980007000079. [DOI] [PubMed] [Google Scholar]
- 25.Richardson AS, Boone-Heinonen J, Popkin BM, Gordon-Larsen P. Neighborhood fast food restaurants and fast food consumption: a national study. BMC Public Health. 2011;11(543):543. doi: 10.1186/1471-2458-11-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Research Council. The public health effects of food deserts: workshop summary. The National Academies Press; 2009. http://www.nap.edu/openbook.php?record_id=12623. [PubMed] [Google Scholar]
- 27.Gittelsohn J, Song HJ, Suratkar S, et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ Behav. 2010 Jun;37(3):390–402. doi: 10.1177/1090198109343886. [DOI] [PubMed] [Google Scholar]
- 28.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007 Jul;22(7):1018–1023. doi: 10.1007/s11606-007-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bawadi HA, Ammari F, Abu-Jamous D, Khader YS, Bataineh S, Tayyem RF. Food insecurity is related to glycemic control deterioration in patients with type 2 diabetes. Clin Nutr. 2011 Nov 25;25:25. doi: 10.1016/j.clnu.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010 Feb;140(2):304–310. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Seligman HK, Jacobs EA, Lopez A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012 Feb;35(2):233–238. doi: 10.2337/dc11-1627.. This is the first study to evaluate whether food insecurity is associated with poor glycemic control in low-income adults with type 2 diabetes.
- 32.Armour BS, Pitts MM, Lee CW. Cigarette smoking and food insecurity among low-income families in the United States, 2001. Am J Health Promot. 2008 Jul-Aug;22(6):386–392. doi: 10.4278/ajhp.22.6.386. [DOI] [PubMed] [Google Scholar]
- 33. Kursmark M, Weitzman M. Recent findings concerning childhood food insecurity. Curr Opin Clin Nutr Metab Care. 2009 May;12(3):310–316. doi: 10.1097/MCO.0b013e3283298e37.. This review article summarizes the recent findings of the effect of food insecurity on the overall health of the child
- 34.Center for Disease Control and Prevention. Vital signs: current cigarette smoking among adults aged >/=18 years--United States, 2005–2010. MMWR Morb Mortal Wkly Rep. 2011 Sep 9;60(35):1207–1212. [PubMed] [Google Scholar]
- 35.Reid RD, Mullen KA, Pipe AL. Systematic approaches to smoking cessation in the cardiac setting. Curr Opin Cardiol. 2011 Sep;26(5):443–448. doi: 10.1097/HCO.0b013e3283497499. [DOI] [PubMed] [Google Scholar]
- 36.Ivers LC, Cullen KA. Food insecurity: special considerations for women. Am J Clin Nutr. 2011 Dec;94(6):1740S–1744S. doi: 10.3945/ajcn.111.012617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lohman BJ, Stewart S, Gundersen C, Garasky S, Eisenmann JC. Adolescent overweight and obesity: links to food insecurity and individual, maternal, and family stressors. J Adolesc Health. 2009 Sep;45(3):230–237. doi: 10.1016/j.jadohealth.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 38.Gooding HC, Walls CE, Richmond TK. Food Insecurity and Increased BMI in Young Adult Women. Obesity (Silver Spring) 2011 Jul 21;21(10):233. doi: 10.1038/oby.2011.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gundersen C, Garasky S, Lohman BJ. Food insecurity is not associated with childhood obesity as assessed using multiple measures of obesity. J Nutr. 2009 Jun;139(6):1173–1178. doi: 10.3945/jn.109.105361. [DOI] [PubMed] [Google Scholar]
- 40.Leung CW, Willett WC, Ding EL. Low-income Supplemental Nutrition Assistance Program participation is related to adiposity and metabolic risk factors. Am J Clin Nutr. 2012 Jan;95(1):17–24. doi: 10.3945/ajcn.111.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crawford PB, Webb KL. Unraveling the paradox of concurrent food insecurity and obesity. Am J Prev Med. 2011 Feb;40(2):274–275. doi: 10.1016/j.amepre.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 42.Olson CM. Food insecurity and maternal health during pregnancy. J Am Diet Assoc. 2010 May;110(5):690–691. doi: 10.1016/j.jada.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 43.Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007 Nov;107(11):1952–1961. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 44.Laraia BA, Siega-Riz AM, Gundersen C. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain, and pregnancy complications. J Am Diet Assoc. 2010 May;110(5):692–701. doi: 10.1016/j.jada.2010.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee AJ, Hiscock RJ, Wein P, Walker SP, Permezel M. Gestational diabetes mellitus: clinical predictors and long-term risk of developing type 2 diabetes: a retrospective cohort study using survival analysis. Diabetes Care. 2007 Apr;30(4):878–883. doi: 10.2337/dc06-1816. [DOI] [PubMed] [Google Scholar]
- 46.Clausen TD, Mathiesen ER, Hansen T, et al. High prevalence of type 2 diabetes and pre-diabetes in adult offspring of women with gestational diabetes mellitus or type 1 diabetes: the role of intrauterine hyperglycemia. Diabetes Care. 2008 Feb;31(2):340–346. doi: 10.2337/dc07-1596. [DOI] [PubMed] [Google Scholar]
- 47.Dubois L, Farmer A, Girard M, Porcherie M. Family food insufficiency is related to overweight among preschoolers. Soc Sci Med. 2006 Sep;63(6):1503–1516. doi: 10.1016/j.socscimed.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 48.Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obes Rev. 2011 May;12(5):e73–e83. doi: 10.1111/j.1467-789X.2010.00820.x. [DOI] [PubMed] [Google Scholar]
- 49.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. Jama. 2010 Jan 20;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 50.Center for Disease Control and Prevention. Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2007–2008. National Center for Health Statistics, Centers for Disease Control and Prevention. 2010 http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.htm.
- 51.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001 Sep;108(3):712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 52.Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010 May;91(5):1499S–1505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011 Nov 17;365(20):1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 54.Food and Agriculture Organization of the United Nations. The state of food insecurity in the world 2010: Adressing food insecurity in protracted crises. 2010 http://www.fao.org/docrep/013/i1683e/i1683e.pdf.
- 55.Sheeran J. The challenge of hunger. Lancet. 2008 Jan 19;371(9608):180–181. doi: 10.1016/S0140-6736(07)61870-4. [DOI] [PubMed] [Google Scholar]