Abstract
Desquamative gingival lesions are non-plaque induced inflammatory gingival lesions. It is a clinical description and not a diagnosis. These desquamative lesions represent oral manifestations of various dermatoses. Discoid lupus erythematosus is one of the rare dermatoses which show desquamative lesions as oral manifestations. This article presents a rare case report of discoid lupus erythematosus with oral lesions involving gingiva of a 66-year-old female patient.
Keywords: Dermatoses, desquamative gingivitis, discoid lupus erythematous
INTRODUCTION
Desquamative lesions of the gingiva are non plaque induced inflammatory gingival lesions.[1] It is not a specific disease entity, but a gingival response associated with a variety of conditions.[2] These desquamative lesions represent oral manifestations of various dermatoses which include Lichen planus, Pemphigus vulgaris, Erythema multiform, Lupus erythematosus, dermatitis herpetiformis, and chronic ulcerative stomatitis.[3]
Hence, it is of paramount importance to ascertain the identity of the disease responsible of desquamative gingivitis to establish the appropriate therapeutic approach and management. This paper reports a case of rare desquamative lesion involving the gingiva in a 66-year-old female patient.
CASE REPORT
A 66-year-old female patient reported to Department of Periodontics, M. S. Ramaiah Dental College and Hospital, Bangalore, with the complaint of burning sensation in the gums for the past one month which had started spontaneously, not associated with pain and aggravated on taking spicy foods and relieved gradually. She also had bleeding gums for the past one month, while brushing and eating. There was no relevant drug history or significant medical history. She had not received any dental treatment before. Her personal history reveals that she had no habits and she used medium brush with non-medicated paste.
On extra oral examination, she had some obvious skin lesions on the scalp which appeared as depigmented scarring alopecia of the scalp [Figure 1]. She also had a hyperkeratotic plaque behind her left ear [Figure 2].
Figure 1.

Depigmentation with scarring alopecia of the scalp
Figure 2.

Hyperkeratotic plaque present on the posterior auricle of the left ear
Intra oral examination of gingiva revealed reddish marginal, attached gingiva and interdental papilla in both maxillary and mandibular anterior region [Figure 3]. Desquamation of epithelium was present in the attached gingiva of maxillary right first molar region, mandibular right canine, between maxillary right premolars on the palatal aspect. Nikolsky's sign was positive [Figures 4–6]. Generalized bleeding on probing was present. There were no periodontal pockets, furcation involvement, and mobility. Excisional biopsy was done under local anesthesia in the maxillary anterior region. Specimen was sent for histopathologic examination.
Figure 3.

Desquamation of the gingiva -maxillary and mandibular anterior region
Figure 4.

Desquamation present – palatal
Figure 6.

Nikolsky's sign - positive
Figure 5.

Desquamation present – lingual
The H and E section showed parakeratinized stratified squamous epithelium overlying the connective tissue. The connective tissue showed dense inflammatory infiltrate beneath the basement membrane chiefly composed of lymphocytes [Figure 7]. Hematological examination included total white blood cell (WBC) count, differential white blood count, erythrocyte sedimentation rate, hemocrit, bleeding time, and clotting time were within normal limits.
Figure 7.
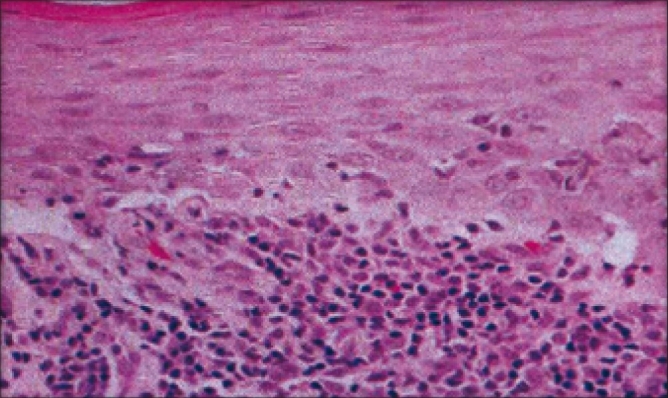
H and E section
Based on the clinical and histopathologic features, lesion was suggestive of discoid lupus erythematosus.
Hand scaling was performed as gently as possible in order to minimize tissue disruption. Hand scaling was preferred, soft tooth brush and mouth rise (chlorhexidine 0.12%) was recommended. Triamcinolone acteonide oral paste was advised to apply two to three times per day and was recalled for follow-up and maintenance.
DISCUSSION
Lupus erythematosus is an auto immune connective tissue disease which consists of discoid lupus erythematosus (DLE) and systemic lupus erythematosus (SLE). Either of these lesions may appear similar to oral lichen planus.[4] Discoid lupus erythematosus mucocutaneous lesions are indistinguishable clinically from those of systemic lupus erythematosus. It occurs by the age of 20 to 50 years. It is prevalent in afro-caribbean people. Marked sex predilection in females by 8:1.[5] It is caused by inter play of genetics, hormonal, and environmental. One to five percent of patients with discoid lupus may develop systemic lupus erythematosus[6] and 25% of patients with SLE may develop typical chronic discoid lesions at some time during their illness. Clinical features include red purple macules papules or small plaques with hyperkeratotic surface. Early classic DLE lesions typically evolve into sharply demarcated, coin shaped (i.e., discoid) erythematous plaques covered by a prominent, adherent scale that extends into the orifices of dilated hair follicles. The lesions typically expand with erythema and hyperpigmentation at the periphery leaving hallmark atrophic central scarring, telangiectasia, and hypopigmentation. When the adherent scale is lifted from more advanced lesions, keratotic spikes similar in appearance to carpet tacks can be seen to project from the under surface of the scale (i.e., the “carpet tack” sign).
Affected sites include face, scalp, ears, V area of the neck, and extensor aspects of the arms. A symmetric, hyperkeratotic, butterfly-shaped plaque is occasionally found over the malar areas of the face and bridge of the nose. Characteristic feature include itching or burning sensation.
Incidence of oral lesions of DLE is about 20 to 50%. Present with or without skin lesion.[7] The margins of the lesions are not sharply demarcated, but frequently show the formation of narrow zone of keratinization, hyperemia with edema, superficial, painful ulceration may occur with crusting, but no actual scale formation as is seen on the skin.
It is important to remember that patients with lupus erythematosus may be taking, systemic steroids or/and other anti-inflammatory medications such as aspirin or Non steroidal anti inflammatory drugs (NSAID's) consequently these patients may be at risk of developing adrenal insufficiency and bleeding disorders. In these situations, medical consultation is extremely important before performing routine dental treatment procedures.[8] Oral lesions may be the first clinical manifestation of DLE, so proper diagnosis is required for early detection and to establish better treatment planning, this promotes resolution of established lesions and prevents scarring of skin lesions and also, alleviates discomfort of the patients.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Mesa M, Kelner R, Pecoraro F, Deasy M. Oral discoid lupus erythematosus. A case report and review of the literature. J Periodontol. 1979;50:90–3. doi: 10.1902/jop.1979.50.2.90. [DOI] [PubMed] [Google Scholar]
- 2.Schiödt M, Halberg P, Hentzer B. A clinical study of 32 patients with oral discoid lupus erythematosus. Int J Oral Surg. 1978;7:85–94. doi: 10.1016/s0300-9785(78)80052-0. [DOI] [PubMed] [Google Scholar]
- 3.Mc carthy FP, Mc carthy PL. Shklar: Chronic desquamative gingivitis: A reconsideration. Oral Surg. 1960;13:1300. [Google Scholar]
- 4.Scully C, Porter SR. The clinical spectrum of desquamative gingivitis. Semin Qutan Med Surg. 1997;16:308. doi: 10.1016/s1085-5629(97)80021-1. [DOI] [PubMed] [Google Scholar]
- 5.Cawson RA, Odell EW. Essentials of oral pathology and oral medicine. London: Churchill Livingstone; 1997. pp. 301–2. [Google Scholar]
- 6.Fitzpatrick TB. In color atlas and synopsis of clinical dermatology. 4th ed. Boston USA: McGraw-Hill; 2003. p. 1523. [Google Scholar]
- 7.Shafer WG, Hine MK, Levy BM. A textbook of oral pathology. 7th ed. Philadelphia: W B Saunders; 1999. p. 8992. [Google Scholar]
- 8.Rhodes NL. The review of oral manifestation of systemis lupus erythematosis. Quintessence Int. 1990;21:461–5. [PubMed] [Google Scholar]


