Abstract
Osteomas are benign slow growing, osteogenic lesions which may arise from proliferation of either cancellous or compact bone. They are usually sessile tumours composed of dense sclerotic, well formed bone projecting out from the cortical surface, most often of the skull and facial bones. This paper reports a case of a peripheral osteoma in the hard palate of a 45-year-old man, which was treated by periodontal flap surgery with surgical excision of the bony lesion. Peripheral osteomas of jaw bone are uncommon and usually associated with Gardner's syndrome. Histological examination confirmed the clinical impression of a peripheral osteoma. Patient was reviewed after one year and was asymptomatic with no recurrence of the lesion.
Keywords: Hard palate, maxilla, osteoma, periodontal pocket
INTRODUCTION
Osteoma is a benign osteogenic lesion, which was first described as a specific entity by Jaffe in 1935. It is composed of compact or cancellous bone. In the course of their slow but steady increase in size, osteomas of the maxillofacial bones remain asymptomatic until they attain sufficient sizes as to cause disfigurement and/or direct interference with the normal function of their anatomic location.[1]
Osteomas are bone lesions with different onset and slow growth that may be divided into: (1) cranial and mandibular exophytic osteomas (or eburnean exostoses); (2) paranasal sinuses, facial bones, and orbit osteomas (orbital cavity osteoma); (3) exostoses or bone islands; and (4) long bone superficial osteomas (juxtacortical).[2] Common sites include the body of the mandible and the condylar region.
The etiology seems to be unknown; however, it may be developmental, infectious, or of traumatic origin.[3] Solitary osteomas of the facial skeleton are quite rare, although multiple osteomas of the jaws have been reported as part of Gardner's Syndrome.[4]
Little information is available about the gender predilection; however, some authors suggest that there is a higher incidence of osteomas in male, especially in between second and fourth decade of life.[5]
CASE REPORT
A 45-year-old male patient was referred to the department of Periodontics, Krishnadevaraya College of Dental Sciences and Hospital, Bangalore, for the evaluation and treatment of a palatal bony swelling [Figures 1 and 2]. Patient complained of a slow growing, painless mass in the left palatal maxillary area, which was present since six months. He also gave a history of foreign body (fish bone) lodgement in 25 and 26 region seven months ago; however, no treatment was taken for the same. He was systemically healthy with no relevant medical history, and was asymptomatic except for the discomfort in that region and difficulty with mastication. On oral examination, a firm, lobulated, painless, well-circumscribed, exophytic, mass 1.5×1 cm in diameter was observed on the maxillary posterior left palatal area in relation to 25 and 26 regions. The lesion was bony hard and covered by normal mucosa. Periodontal probing revealed a 9 millimeter deep periodontal pocket associated with the mid palatal area of 26 which prompted us to intervene and surgically excise the bony mass. Clinically, the tooth was firm and not associated with any mobility [Figure 3].
Figure 1.

Bony lesion on palate
Figure 2.

Measured at 15×10 mm
Figure 3.

Nine millimeter pocket depth
Radiographic examination
A region of well defined opacity was seen in the palatal regions of 25 and 26 [Figure 4], when seen on a maxillary occlusal radiograph. The radio-opacity showed a well defined medial convex margin; laterally, the margins were indistinct with rest of the structures. No ossification or underlying bony destruction was apparent.
Figure 4.
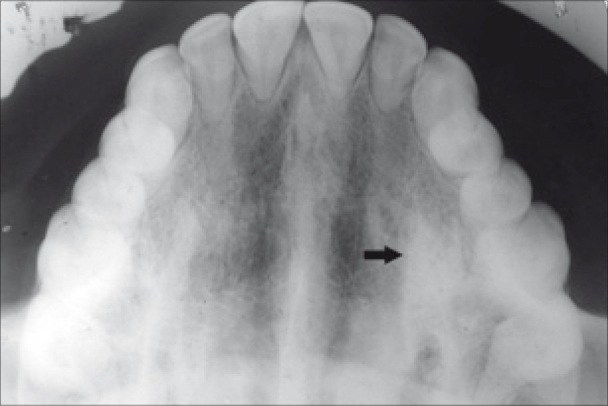
Region of well defined radio-opacity in the region of 25 and 26
Surgical procedure
Under local anesthesia, buccal and palatal flaps were raised, giving crevicular incisions in 24, 25, and 26 regions [Figures 5 and 6]. A second vertical incision was placed on the distal of the first premolar and a full thickness flap was raised to allow for adequate exposure of the surgical site. The bony mass was excised with the help of a Kirkland chisel which has one end that is a back-action chisel and the other end is a straight chisel [Figures 7 and 8]. Care was taken to excise the lesion keeping a periphery of healthy tissue around the lesion. The straight end of the Kirkland chisel was used to refine the bone margin of the surgical site and to round off any sharp edges. Thorough scaling and root planing coupled with removal of the granulation tissue followed by irrigation of the surgical site with saline were performed. Margins of the flap were trimmed to achieve good approximation and the flap was sutured with black silk sutures [Figure 9]. The specimen was put in a bottle containing 10% formalin solution and sent for histopathological examination. The healing was uneventful, and the sutures were removed after 10 days [Figure 10]. The case was followed-up for a period of one year, and there was no sign of recurrence [Figures 11 and 12].
Figure 5.

Sulcular incision given
Figure 6.
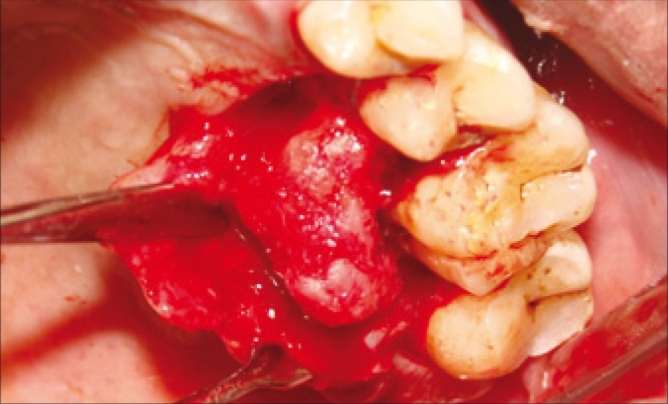
Flap raised using vertical incision
Figure 7.
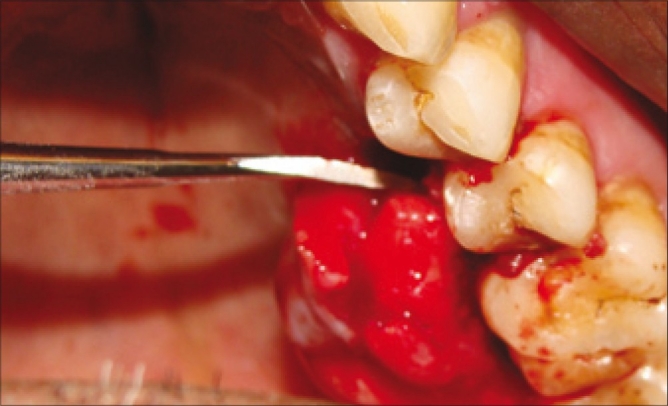
Excision of bony lesion with Kirkland chisel
Figure 8.
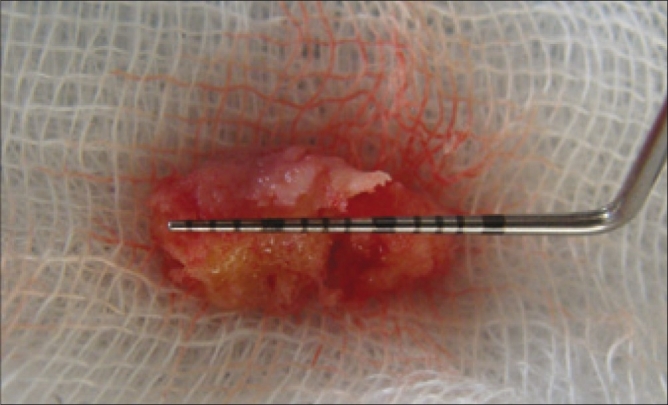
Excised bony lesion
Figure 9.

Sutures placed
Figure 10.

Post-op ten days
Figure 11.

Post-op one month
Figure 12.

Post-op one year
Histopathology
Section showed parakeratinized stratified squamous epithelium; sub epithelially a rim of normal connective tissue was seen around the rete ridges. Deeper connective tissue showed plump mesenchymal cells with prominent nuclei leading to formation of bony trabeculae. The lesional tissue showed numerous delicately arranged trabeculae with the osteocytes, but was devoid of osteoblastic rimming. The bony trabeculae were mature with resting lines. The inter-trabecular tissue showed marrow spaces pre-dominantly made up of adipose tissue, presence of few arterioles and capillaries [Figures 13 and 14]. Histopathologically, the lesion was diagnosed as peripheral (mature) osteoma, which is also referred to as “Ivory Osteoma”.
Figure 13.
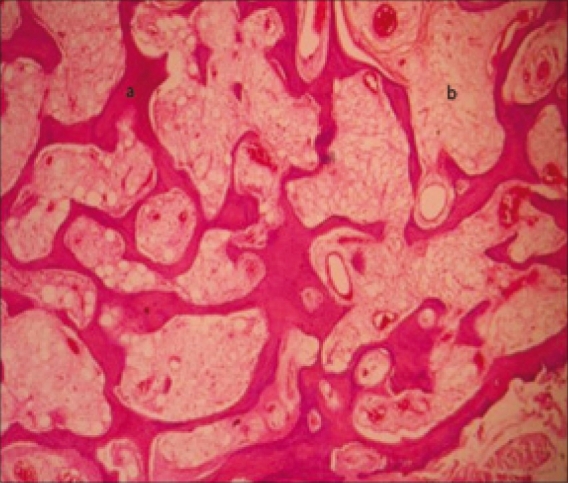
(a) Trabeculae with osteocytes (b) Adipose cells
Figure 14.
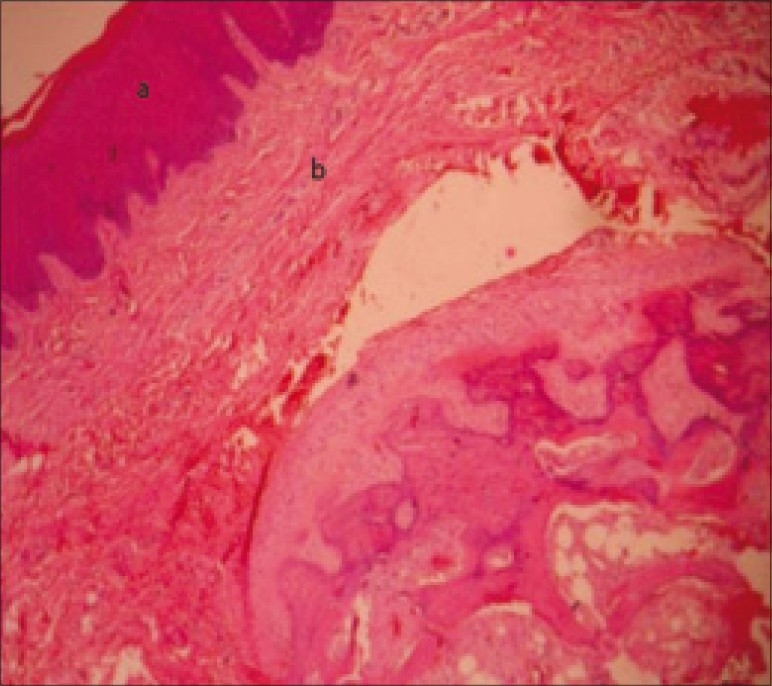
(a) Parakeratinized stratified squamous epithelium (b) Connective tissue
DISCUSSION
Osteomas are benign osteogenic lesions with very slow growth. They may arise from proliferation of either cancellous or compact bone. They can be central, peripheral, or extra skeletal.[1] In gnathic bones, osteoma can appear in bone's surface, as mushroom-like masses pedunculated or sessile (periosteum osteoma), or located in medullary space (endosteum osteoma). These lesions are usually asymptomatic, but may proliferate in medullary bone (endosteal) or on the bone surface as a polypoid or sessile mass (periosteal).[6] Reactive bone growth from infection, trauma, or vascular malformation may produce lesions simulating an osteoma. These lesions may arise at any age but with a distinct predilection for elderly adults and they are twice more common in male than in female.
As a pathologic entity, osteoma is difficult to differentiate radiographically from other lesions with pronounced ossifications. Exostosis, which is the term generally applied for well demarcated and extremely opaque bony lesion, osteosclerosis and similar alterations of the bone are always discussed alongside osteomas. The other differential diagnosis include enostosis, cementoma, complex odontome, fibrous dysplasia, osteochondroma, Paget's disease, peripheral ossifying fibroma, a reactive focal lesion; periosteal osteoblastoma, osteoid osteoma, and paraosteal osteosarcoma that present as painful masses of rapid growth.[7–9] Though the exact etiology is not known, it may be suggested, in this case that trauma from foreign body lodgment as afore mentioned might have been the trigger for this proliferative response.
CONCLUSION
Osteomas are slow growing benign osteogenic lesions arising from the proliferation of either cancellous or compact bone. They are usually asymptomatic and have a low recurrence rate. Simple excision of the lesion in its entirety is the treatment of choice in symptomatic lesions. The association of osteoma with Gardner's syndrome must always be kept in mind before deciding the treatment plan.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Nabeshima K, Marutsuka K, Shimao Y, Uehara H, Kodama T. Osteoma of the frontal sinus complicated by intracranial mucocele. Pathol Int. 2003;53:227–30. doi: 10.1046/j.1320-5463.2003.01459.x. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhry SI, Tappuni AR, Challacombe SJ. Multiple maxillary and mandibular exostoses associated with multiple dermatofibromas: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:319–22. doi: 10.1016/s1079-2104(00)70096-5. [DOI] [PubMed] [Google Scholar]
- 3.Neville BW, Damm D. Patologia oral e maxillofacial. Rio de Janeiro: GuanabaraKoogan; 1998. [Google Scholar]
- 4.Longo F, Califano L, De Maria G, Ciccarelli R. Solitary osteoma of the mandibular ramus: Report of a case. J Oral Maxillofac Surg. 2001;59:698–700. doi: 10.1053/joms.2001.23408. [DOI] [PubMed] [Google Scholar]
- 5.Lin CJ, Lin YS, Kang BH. Middle turbinate osteoma presenting with ipsilateral facial pain, epiphora, and nasal obstruction. Otolaryngol Head Neck Surg. 2003;128:282–3. doi: 10.1067/mhn.2003.29. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: A study of 10 new cases and analysis of the literature. J Oral Maxillofac Surg. 1994;52:467–70. doi: 10.1016/0278-2391(94)90342-5. [DOI] [PubMed] [Google Scholar]
- 7.Sayan NB, Uçok C, Karasu HA, Günhan O. Peripheral osteoma of the oral and maxillofacial region: A study of 35 new cases. J Oral Maxillofac Surg. 2002;60:1299–301. doi: 10.1053/joms.2002.35727. [DOI] [PubMed] [Google Scholar]
- 8.Johann AC, Freitas JB, Aguiar MC, de Araujo NS, Mesquita RA. Peripheral osteoma of the mandible: Case report and review of the literature. J Craniomaxillofac Surg. 2005;33:276–81. doi: 10.1016/j.jcms.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 9.8th ed. Philadelphia PA: Elsevier Saunders International; Robbins and Cotrans athologic basis of disease. [Google Scholar]


