Abstract
Nicotine replacement therapy (NRT) is often used to maintain smoking cessation. However, concerns exist about the safety of long term NRT use in ex-smokers and its concurrent use in smokers. In this study, we determined the effect of nicotine administration on 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK)-induced lung tumors in A/J mice. Female mice were administered a single dose of NNK (10 μmol) and 0.44 μmol/ml nicotine in the drinking water. Nicotine was administered 2 weeks prior to NNK, 44 weeks after NNK, throughout the experiment, or without NNK treatment. The average weekly consumption of nicotine-containing water was 15 ± 3 mls/mouse, resulting in an estimated daily nicotine dose of 0.9 μmol (0.15 mg) per mouse. Nicotine administration alone for 46 weeks did not increase lung tumor multiplicity (0.32 ± 0.1 tumor/mouse versus 0.53 ± 0.1 tumors/mouse). Lung tumor multiplicity in NNK-treated mice was 18.4 ± 4.5 and was not different than for mice consuming nicotine before or after NNK administration, 21.9 ± 5.3 and 20.0 ± 5.4 tumors per mouse, respectively. Lung tumor multiplicity in animals consuming nicotine both before and after NNK administration was 20.4 ± 5.4. Tumor size and progression of adenomas to carcinomas was also not affected by nicotine consumption. In addition, nicotine consumption had no effect on the level of O6-methylguanine in the lung of NNK-treated mice. These negative findings in a commonly used model of human lung carcinogenesis should lead us to question the interpretation of the many in vitro studies that find nicotine stimulates cancer cell growth.
Keywords: Nicotine, NNK, A/J mouse, O6-methylguanine
Introduction
Tobacco use results in more than 400,000 deaths annually in the United States; 157,000 of these are due to lung cancer (1,2). The use of nicotine replacement therapy (NRT) to aid smoking cessation efforts would significantly decrease the number of tobacco related deaths (3). However, concerns exist about the safety of long-term nicotine use in ex-smokers as well as its concurrent use with smoking. It has been suggested that nicotine is a driver of cancer growth, the “estrogen of lung cancer” (4). Nicotine is a ligand for the nicotinic acetylcholine receptor (nAChR) and has been shown to increase cell proliferation, inhibit apoptosis and enhance angiogenesis and stimulate cancer cell growth (5–7). Therefore, the effect of nicotine on tobacco-induced lung cancer is of concern to the public health community.
In animals, nicotine alone is not a carcinogen (8). A two year study of rats chronically exposed to inhaled nicotine did not result in any increased frequency of tumors in any tissue (9). A small number of lung tumors were induced in hamsters exposed to nicotine in the presence of hypoxia (10). More recently, nicotine has been reported to promote tumor growth and metastasis in cancer xenograft models (5,11–13). However, animal co-carcinogenesis studies with nicotine have produced mixed results, some studies show evidence for co-carcinogenicity and others have shown no effect or a protective effect of nicotine (8,12).
The effects of nicotine on cell proliferation, apoptosis and angiogenesis are mediated by nicotine’s interaction with the nAChR (6,7) and genome wide association study studies have implicated a gene locus (15q25) that encodes three nAChR subunits in lung cancer risk (14–16). Some investigators have suggested this association is a direct link to lung cancer, independent from any effect on nicotine addiction and smoking intensity (7,17). The possible direct link between nAChR and lung cancer has heightened the concern of FDA and public health officials in promoting long-term use of NRT (18). Nevertheless, a direct link has not been established. A meta analysis in non-smokers shows no association of the 15q25 locus with lung cancer and data from the Lung Health Study do not support a link between NRT and lung cancer (19,20). Also of note is a recent study in which chronic nicotine exposure, in contrast to short term exposure, impairs angiogenesis and down regulates the nAChR (21).
In contrast to the above concerns, nicotine has been suggested to protect smokers from tobacco induced carcinogenesis (22–24). Specifically, it has been hypothesized that nicotine competitively inhibits enzymes that catalyze the activation of the tobacco specific carcinogen, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK), since these enzymes also catalyze the metabolism of nicotine. The primary pathway of nicotine metabolism is cytochrome P450 (P450) 2A6 -catalyzed oxidation to the nicotine Δ5′(1′) iminium ion, and further oxidation to cotinine and trans 3′-hydroxycotinine (25–27). P450 2A6 is also a catalyst of NNK α-hydroxylation (28). α-Hydroxylation generates reactive intermediates that alkylate DNA to adducts that result in mutagenic bases, initiating the carcinogenic process (8). P450 2A6 is a poor catalyst of NNK α-hydroxylation, however the closely related extrahepatic enzyme, P450 2A13 is an excellent catalyst (28). P450 2A13, also an efficient catalyst of nicotine oxidation (26), is expressed in the human lung and likely contributes to the metabolic activation of NNK in smokers (29). Nicotine is not only a competitive inhibitor of P450 2A6 and P450 2A13 catalyzed reactions, it also irreversibly inactivates both enzymes during its metabolism (27). Therefore, nicotine metabolism in the lung may lead to a decrease in P450 2A13 catalyzed activation of NNK, decreasing DNA adduct formation and potentially protecting smokers from NNK carcinogenesis.
The A/J mouse is an excellent model in which to study modifiers of NNK induced lung carcinogenesis (30,31). In the mouse, nicotine and NNK are metabolized by the P450 2A6/2A13 ortholog, P450 2A5 (26). P450 2A5 present in both the lung and the liver catalyzes the bioactivation of NNK. In the mouse the pathway critical to NNK induced tumorigenesis is α-hydroxylation of the methylene carbon adjacent to the nitroso group (32,33). This pathway leads to DNA methylation, and the persistence of O6-methylguanine (O6mG) adducts results in lung tumorigenesis. There is a strong correlation between O6mG levels in the lung and the multiplicity of lung tumors in the NNK treated A/J mouse (33). Also, when a lung specific P450 reductase knockout mouse with no P450 activity in the lung is treated with NNK, both the number of lung tumors per mouse and the level of O6mG DNA adducts in the lung are significantly reduced relative to NNK-treated wild type animals (34). An inhibitor of P450 2A5 activity in the lung would be expected to have similar effects.
The study presented here was designed to test two hypotheses: one, that sustained exposure to nicotine prevents or delays tumor initiation in A/J mice treated with NNK, and two, that when tumor initiation occurs in this model, nicotine accelerates tumor growth by reducing apoptosis, promoting angiogenesis, and altering the tumor microenvironment. The effect of chronic nicotine administered in the drinking water on P450 2A5 activity, and NNK induced lung tumorigenesis was determined.
Materials and Methods
Chemicals, reagents and Diet
(S)-Nicotine hydrogen tartrate, NNK, coumarin, and other reagents were purchased from Sigma Aldrich (St. Louis MO). O6mG was a gift from Stephen Hecht (Masonic Cancer Center, University of Minnesota). Mouse diets (AIN-93G and AIN-93M) were purchased from Harlan Teklad (Madison, WI).
Animal Studies
Four week-old female A/J mice were obtained from the Jackson Laboratories (Bar Harbor, ME). Mice were housed under specific pathogen free conditions and allowed to acclimate for 7 days before experimental procedures. Experiments were conducted with approval from the University of Minnesota Institutional Animal Use and Care Committee. Husbandry practices and diet followed protocols described previously (35). Two experiments were carried out. The 1st was a 2 week study to determine the consumption of nicotine in the drinking water with and without saccharin. Saccharin has been used in previous studies to mask the taste of nicotine. Experiment 2 was carried out in two parts to determine the effect of chronic nicotine on NNK metabolism and DNA adduct formation and NNK-induced tumorigenesis.
Experiment 1
Female A/J mice, 5 weeks of age, were randomized into 6 groups of 5 mice each. Treated groups received nicotine hydrogen tartrate (100 or 200 μg/ml) in the drinking water with or without 2% saccharin as described (5). Fresh water with the appropriate concentration of nicotine and/or saccharin was provided twice weekly for two weeks, and water consumption for each cage was measured at the same intervals. Sodium potassium tartrate was used as a control for animals that did not receive nicotine. Nicotine disposal was in accordance to state and local regulations. Urine was collected daily by gently massaging the abdomen to stimulate urination. Urine was not obtained from every mouse each day. Mice were euthanized according to the guidelines of the American Veterinary Medical Association after two weeks and blood collected immediately post mortem by cardiac venipuncture. Plasma levels of cotinine were determined for each mouse and urine pooled by group was analyzed for cotinine.
Experiment 2
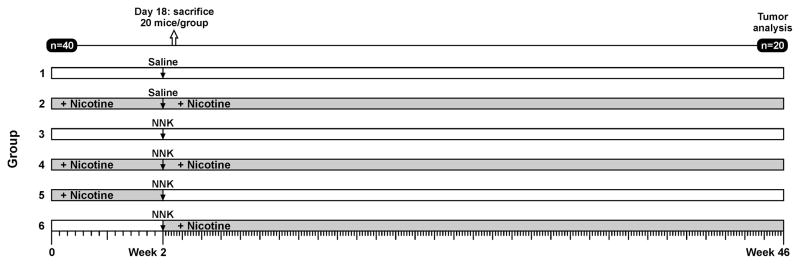
Groups of 40 mice (5 weeks of age, 5 mice per cage) were assigned to one of six experimental conditions as illustrated in Fig. 1. Nicotine hydrogen tartrate [200 μg (0.44 μmol)/ml] and sodium potassium tartrate were provided in drinking water as described above. Water consumption per cage per week was measured and consumption per mouse was estimated based on the number of mice per cage. After 2 weeks, each mouse in groups 3–6 were administered 2 mg (10 μmol) NNK in 0.1 ml of phosphate buffered saline as a single intraperitoneal injection (36). Mice that were not injected with NNK (groups 1 and 2) received an intraperitoneal injection of 0.1 ml phosphate buffered saline solution. Immediately following the administration of NNK or saline, nicotine-containing drinking water was provided to animals in group 6 and was replaced with non-nicotine containing water for animals in group 5. Groups 2, 4 and 6 were provided nicotine containing water for the remainder of the experiment. Blood and urine were collected as above for the first two weeks. Subsequently, blood and urine was collected from each animal in the nicotine consuming groups at least once a month. Twenty mice from each group were euthanized 96 h after the NNK injection. Blood was collected immediately post mortem by cardiac venipuncture and liver and lung tissues were harvested and frozen on dry ice and stored at −80°C until analysis for P450 2A5-catalyzed metabolism and O6-mG levels. The remaining mice were maintained for 44 weeks, at which time they were euthanized. Blood was collected immediately post mortem by cardiac venipuncture.
Figure 1.
Experimental Protocol to assess the effect of chronic nicotine consumption on the initiation and progression of NNK-induced lung tumorigenesis in the A/J mouse. Female mice were administered nicotine (0.44 μmol/ml) in the drinking water as their sole source of water; throughout the study (groups 2 and 4), prior to NNK administration (group 5) or after NNK administration (group 6). Groups 1 and 3 did not receive nicotine and group 5 did not receive nicotine after week 2. Four days following NNK or saline treatment 20 of the 40 mice in each group were euthanized for the determination of DNA adduct levels and P450 2A5 activity.
Tumor multiplicity and classification
Tumor multiplicity was determined grossly as described (35). Briefly, immediately upon sacrifice, lungs were rinsed with cold phosphate buffered saline solution, excised en bloc, and tumors counted using a dissecting microscope. Tumors were scored based on location (lung lobe) and the widest tumor diameter (<0.5 mm; 0.5–1.0 mm, 1.1–2.0 mm, >2 mm). The entire pulmonary tree from five animals and a hemisection from five animals in Groups 1 and 2 were flash frozen in liquid nitrogen and stored at −80°C for further enzyme and tumor analysis. The remaining sections were fixed by immersion in 10% neutral buffered formalin for 24 h, and subsequently transferred to 70% ethanol for long-term preservation. For histopathology evaluation, lung sections were embedded in paraffin blocks. Three step-sections, each 150 μm apart, were obtained from the blocks and stained with hematoxylin and eosin for microscopic analysis. Tumors were categorized according to criteria of the Mouse Models of Human Cancers Consortium (37). Briefly, alveolar hyperplasia was diagnosed by an increase in the number of cuboidal or columnar cells in an alveolus without cellular atypia. Adenomas were well-circumscribed, <5 mm diameter areas of proliferative cuboidal to columar cells lining an alveolus. Adenomas with dysplasia (pre-invasive lesions) showed marked cellular atypia and/or squamous metaplasia. Lesions that were >5 mm diameter and showed invasion into adjacent airways, blood vessels, or alveoli were classified as carcinomas.
Statistics
Descriptive statistics were used to enumerate water consumption, tumor multiplicity and progression (total tumor number, size distribution, and pathologic classification). Data were analyzed using 2-tailed Student’s T-test and one-way ANOVA. To account for variance in lung lobes examined due to fragmentation and loss during processing, data were normalized per lung lobe. Significance was set at p<0.05. Poisson regression models also were used to examine the effect of group on tumor multiplicity, the distribution of tumor types, and tumor diameters, after adjusting for plasma levels of nicotine metabolites.
Lung and Liver P450 2A5 metabolism and Lung O6mG levels
Lung and liver microsomes were prepared as described previously (38). Half the lung or liver was used, and the microsomal pellet was resuspended in a final volume of 0.2 ml. Coumarin 7-hydroxylation activity, used to access P450 2A5 activity, was quantified as previously described (39). Microsomes (5–20 μl) were incubated with 20 μM coumarin and a NADPH generating system (0.4 mM NADP, 10 mM glucose-6-phosphate, 0.4 units/ml glucose phosphate dehydrogenase) in 50 mM Tris, pH 7.4 for 10 to 20 min at 37°C. The reaction was stopped with 20 μl 15% TCA. DNA was isolated from half a lung (60–100 mg tissue) using the PUREGENE DNA Purification Kit (Qiagen, Valencia, CA). O6-mG levels were determined as previously described (40). The urine (1–5 μL) and plasma (25 μL) were analyzed for nicotine, cotinine and trans 3′-hydroxycotinine by liquid chromatography tandem mass spectrometry (LC/MS/MS) as previously described (41).
Results
Consumption of nicotine in the drinking water
In a two week pilot study, mice were provided nicotine in the drinking water with or without saccharin (group 1A/B, controls; group 2A, 0.22 μmol/ml nicotine; group 3A, 0.44 μmol/ml nicotine; group 2B, 0.22 μmol/ml nicotine with 2% saccharin; group 3B, 0.44 μg/ml nicotine with 2% saccharin). The urinary concentrations of cotinine varied widely across the days of collection. Cotinine values ranged from 80 to 3820 ng/ml and appeared to be independent of both saccharin supplementation and nicotine concentration. Plasma cotinine concentrations ranged from 3 to 45 ng/ml and were higher in animals consuming saccharin (group 2, 7 ± 4 ng/ml; group 3, 12 ± 8 ng/ml; group 2B, 19 ± 18 ng/ml; group 3B 22 ± 13 ng/ml). However, saccharin did not appear to significantly influence average water consumption, which ranged from 1.6 to 2.2 ml/mouse/day. The differences observed in cotinine plasma concentrations are likely due to differences in the time of nicotine consumption. Therefore, saccharin was not used in the tumorigenesis experiment.
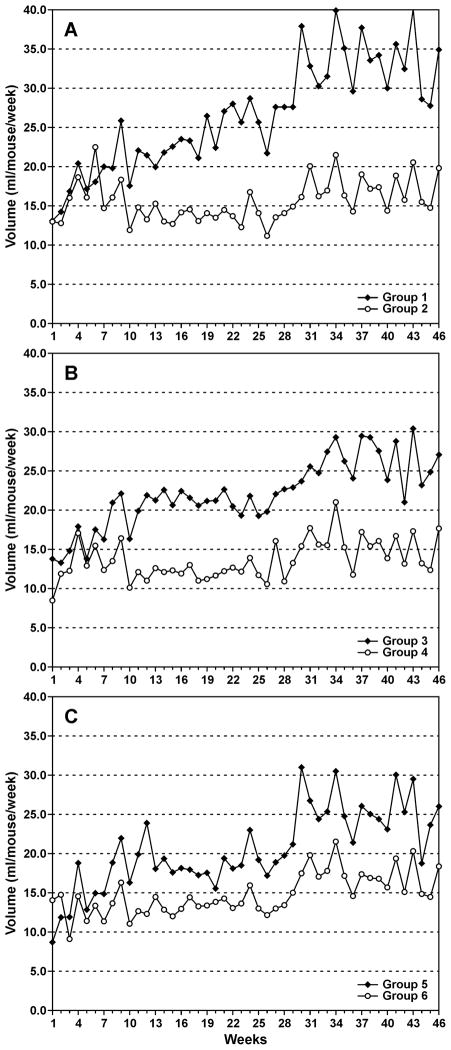
For the first 4 weeks of the tumorigenesis study there was no difference in water intake between nicotine consuming and non-nicotine consuming groups (Fig. 2A–C). However, water consumption was significantly decreased in the groups consuming nicotine over the next 42 weeks. The difference was less pronounced in the NNK treated animals compared to saline controls (Fig. 2A versus 2B or 2C). None of the animals displayed clinical signs of dehydration. The average weekly water consumption per mouse over weeks 2 to 46 in the nicotine consuming animals was 15 ± 3 ml/mouse. Therefore, the estimated daily dose of nicotine per mouse was 0.9 μmol (0.15 mg) per day, a significantly higher dose per kg than the approximately 20 mg/day consumed by a 70 kg one pack a day smoker.
Figure 2.
(A–C) Average weekly water consumption per mouse by group (described in Figure 1). Water consumption for each cage was measured twice per week.
Urinary nicotine, cotinine and trans-3′-hydroxycotinine concentrations for weeks 1–2 and month 5 of nicotine consumption, presented in Table 1, are consistent with this high dose of nicotine. There was no difference in urinary nicotine, cotinine or trans 3′-hydroxycotinine concentrations among the groups and the mean values for months 2 through 10 were not significantly different than those at 5 months (data not shown). As in the 2 week study urinary cotinine concentrations varied greatly across animals. The variation was somewhat less after several weeks of consumption. The urinary concentrations of nicotine were as much as 6-fold lower than cotinine and were also quite variable, ranging from 22 to 10,500 ng/ml. This is likely due to the time of urine collection relative to nicotine consumption and the relatively fast metabolism of nicotine in the mouse. The concentration of the primary cotinine metabolite, trans 3′-hydroxycotinine was 4 to 10 times greater than cotinine.
Table 1.
Concentration of nicotine, cotinine, and trans-3′-hydroxycotinine in the urine of nicotine consuming micea
| Group | Treatmentb | Time | Nicotine (ng/ml) | Cotinine (ng/ml) | trans 3′-Hydroxycotinine (ng/ml) | |||
|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Mean | Range | |||
| 2 | Nicotine 0–46 weeks/saline | 1–2 weeksc (n= 26) | 1360 ± 1040 | 65 – 3570 | 1260 ± 1240 | 116 – 4700 | 12200 ± 9010 | 1600 – 34000 |
| 5 month (n=14) | 1270 ± 1170 | 217 – 3620 | 4400 ± 3200 | 450 – 10600 | 27900 ± 9820 | 17100 – 49600 | ||
| 4 | Nicotine 0–46 weeks/NNK | 1–2 weeks (n = 24) | 1900 ± 2550 | 53 – 7700 | 4790 ± 5860 | 70 – 17500 | 18900 ± 13500 | 4300 – 48000 |
| 5 months (n=15) | 2170 ± 2760 | 156 – 10,500 | 5700 ± 4300 | 930 – 16000 | 42900 ± 19400 | 16600 – 74400 | ||
| 5 | Nicotine 0–2 weeks/NNKa | 1–2 weeks (n=25) | 980 ± 930 | 22 – 2870 | 3520 ± 6220 | 150 – 3120 | 17000 ± 10500 | 2920 – 37500 |
| 5 months | ndd | nd | nd | |||||
| 6 | Nicotine 2–46 weeks/NNKb | 1–2 weeks | nd | nd | nd | |||
| 5 months (n= 20) | 840 ± 714 | 62 – 2560 | 5910 ± 4140 | 820 – 14700 | 37800 ± 19400 | 9750 – 83400 | ||
Urine obtained from individual mice was analyzed by LC/MS/MS, values are provided for two time points for individual mice from which urine was collected.
The protocol is as illustrated in Fig. 1, beginning at 5 weeks of age female A/J mice (Groups 2,4,5) were provided 0.44 μmol/ml nicotine in the drinking water, after 2 weeks animals in Groups 4, 5 and 6 were administered a single dose of NNK (10 μmol), nicotine was discontinued for Group 5 and initiated in Group 6 at the time of the NNK injection
Urine was collected from a single mouse between 7 and 14 days of nicotine consumption the remaining samples were from a single collection per mouse from 2 to 7 days.
nd, not determined, animals were not consuming nicotine at this time
The plasma concentrations of nicotine, cotinine and trans-3′-hydroxycotinine were determined at the two termination times, 18 days (96 h after NNK or saline injection) and 46 weeks (Table 2). Plasma nicotine levels were low, typically less than 1 ng/ml. Nine animals in group 4, day 18, had plasma nicotine values greater than any animal in the other two groups, with the highest value equal to 11 ng/ml. It is unclear why the concentrations of cotinine and nicotine were higher in this group at this time of plasma collection. The mouse with the highest nicotine plasma value also was the animal with the highest cotinine and trans 3′-hydroxycotinine values, consistent with more recent and/or higher consumption of nicotine. As with the urine values, the variation in plasma nicotine concentrations was likely due to the time of last nicotine consumption. Although circulating nicotine values were low at the single time points analyzed, the detection of nicotine concentrations as high as 11 ng/ml confirms that peak nicotine levels were at least 20 times higher.
Table 2.
Plasma nicotine, cotinine, and trans-3′-hydroxycotinine concentrations
| Group | Treatmenta | Time | Nicotine (ng/ml) | Cotinine (ng/ml) | trans 3′-Hydroxycotinine (ng/ml) | |||
|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Mean ng/ml | Range | |||
| 2 | Nicotine 0–46 weeks/saline | Day 18 (n=20) | 0.61 ± 0.5 | 0.2 – 2.4 | 40 ± 45 | 7 – 198 | 34 ± 21 | 13 – 109 |
| Week 46 (n=19) | 0.40 ± 0.46 | 0.1 – 1.9 | 19 ± 20 | 3 – 72 | 48 ± 36 | 6 – 111 | ||
| 4 | Nicotine 0–46 weeks/NNK | Day 19 (n=20) | 2.3 ± 1.5 | 0.3 – 11 | 118 ± 139 | 19 – 618 | 40 ± 32 | 6 – 120 |
| Week 46 (n=18) | 0.66 ± 0.53 | 0.5 – 2.4 | 31 ± 23 | 12 – 84 | 45 ± 19 | 23 – 78 | ||
| 6 | Nicotine 2–46 weeks/ NNKa | Day 18 (n=20) | 0.65 ± 0.76 | 0.1 – 2.5 | 32 ± 33 | 1 – 123 | 15 ± 14 | 0 – 45 |
| Week 46 (n=20) | 0.26 ± 0.28 | 0.1 – 1.1 | 29 ± 19 | 6 – 53 | 62 ± 28 | 28 – 105 | ||
The protocol is illustrated in Fig. 1 and described in Table 1. Mice in Groups 2 and 4 were consuming nicotine in the drinking water from day 1 to the day of blood collection, animals in Group 6 began consuming nicotine on day 14. Twenty mice in each group were euthanized on day 18 and the remaining mice (18–20) were euthanized at 46 weeks, the termination of the tumorigenesis protocol. Blood was collected immediately post mortem by cardiac venipuncture. Plasma was isolated and analyzed by LC/MS/MS for nicotine and its metabolites.
O6mG levels and P450 2A5 activity
To determine the effect of nicotine on the metabolic activation of NNK, O6mG levels were quantified 96 h following NNK treatment. A 96 h time point was used since a linear relationship between tumor multiplicity and lung DNA O6mG levels exists at this time (33). There was no effect of nicotine consumption on O6mG levels in the lung. The level of O6mG in mice administered only NNK (group 3, n = 10) was 16 ± 5.7 pmol O6mG/μmol guanine compared to 14 ± 1.9 for animals consuming nicotine throughout the experiment (group 4, n= 10). Consistent with this finding was the observation that nicotine consumption did not affect either lung or liver P450 2A5 activity. P450 2A5, a coumarin 7-hydroxylase, is a key catalyst of the metabolism of NNK to the reactive species that generates O6mG (28). In hepatic microsomes from control mice (group 1), the rate of coumarin 7-hydroxylation was 6.4 ± 4.4 pmol/min/mg (n= 10) and in nicotine consuming mice (group 2) it was 5.4 ± 1.8 pmol/min/mg (n=10). In pulmonary microsomes, the rates were 8.7 ± 3.9 pmol/min/mg (n=6, group 1) and 7.7 ± 3.4 pmol/min/mg (n= 6, group 2).
Effect of nicotine on NNK induced lung tumorigenesis
The administration of chronic nicotine in the drinking water did not result in an increase in lung tumor multiplicity or size relative to untreated animals (Table 3, group 1 and 2). As expected all groups administered a single dose of NNK had a significantly increased incidence of lung tumors, the average multiplicity was <1 in mice not treated with NNK and 18.4 – 21.9 in NNK-treated mice (Poisson analysis p<0.0001, Table 3). Similar differences were observed for tumor distribution. However, there was no significant difference in tumor multiplicity or the distribution of tumor numbers by size whether animals were consuming nicotine or not (group 3 versus groups 4, 5, or 6). The concentrations of nicotine metabolites in plasma of individual animals were not significant variables when included in a regression model of the effect of group on tumor size, multiplicity distribution.
Table 3.
Effect of chronic nicotine consumption on NNK induced lung tumors multiplicity and size in A/J micea
| Group | N | Treatmenta | Percent of mice with tumors | Tumors per mouseb (Mean ± SD)
|
||||
|---|---|---|---|---|---|---|---|---|
| total | Diameter (mm)
|
|||||||
| <0.5 | 0.5 – 1.0 | 1.0 – 2.0 | >2 | |||||
| 1 | 19 | No nicotine/saline | 31 | 0.53 ± 0.1 | 0.05 | 0.32 | 0.11 | 0.05 |
| 2 | 19 | Nicotine 0–46 weeks/saline | 26 | 0.32 ± 0.1 | 0.00 | 0.21 | 0.05 | 0.05 |
| 3 | 18 | No nicotine/NNK | 100 | 18.4 ± 4.5 | 0.50 | 6.50 | 10.1 | 1.39 |
| 4 | 18 | Nicotine 0–46 weeks/NNK | 100 | 20.4 ± 5.4 | 0.28 | 7.89 | 11.3 | 0.94 |
| 5 | 19 | Nicotine 0–2 weeks/NNKb | 100 | 21.9 ± 5.3 | 0.80 | 7.90 | 11.8 | 1.40 |
| 6 | 20 | Nicotine 2–46 weeks/NNKb | 100 | 20.0 ± 5.4 | 0.55 | 5.80 | 12.3 | 1.30 |
The protocol is illustrated in Fig. 1. Nicotine (0.44 μmol/ml) was administered in the drinking water for the time intervals indicated and NNK (2 μmol) or saline was administered by interperitoneal injection at 2 weeks. Twenty mice in each group were euthanized on day 18 for DNA adduct analysis and the remaining mice (18–20) were euthanized at 46 weeks. One or two premature deaths occurred in Groups 2–5, details are provided in Table 4. Due to a logistical error only 19 animals were analyzed in Group 1.
The number of total tumors per mouse ranged from 6 to 41.
The tumors in the mice of each group were categorized as adenomas, adenomas with dysplasia or carcinomas. The incidence (percent of mice with tumors) and the multiplicity of each tumor type are presented in Table 4. There was no significant difference in either incidence or multiplicity for any of the tumor categories between NNK treated mice that consumed no nicotine and those that consumed nicotine (group 3 versus groups 4, 5 or 6). There was a slightly higher but non-significant difference in carcinoma incidence in group 4 and 6, versus group 3 or 5. However, there was no parallel decrease in either adenomas or adenomas with dysplasia, which is inconsistent with increased progression to carcinoma. Based on the data variance, we estimate that 80 mice per group would be required to detect a significant (p <0.05) difference of this magnitude between these groups.
Table 4.
Histopathological analysis of tumors in A/J mice receiving NNK with or without nicotinea
| Group | Treatment | Incidence (percent of mice) | Multiplicity (Average per Mouse ± SD) | ||||
|---|---|---|---|---|---|---|---|
| Adenoma | Adenoma with dysplasia | Carcinoma | Adenoma | Adenoma with dysplasia | Carcinoma | ||
| 1 (n=14) | No nicotine/saline | 7 | 7 | 0 | 0.07 ± 0.27 | 0.07 ± 0.27 | 0.0 |
| 2 (n = 15) | Nicotine 0–46 weeks/saline | 8 | 0 | 15 | 0.08 ± 0.28 | 0.0 | 0.15 ± 0.40 |
| 3 (n= 18) | No nicotine/NNK | 83 | 56 | 28 | 3.4 ± 2.4 | 0.83 ± 0.92 | 0.44 ± 0.78 |
| 4 (n = 18) | Nicotine 0–46 weeks/NNK | 89 | 61 | 44 | 4.4 ± 2.7 | 1.0 ± 1.1 | 0.67 ± 0.91 |
| 5 (n = 19) | Nicotine 0–2 weeks/NNK | 95 | 63 | 28 | 4.8 ± 3.5 | 1.0 ± 0.94 | 0.37 ± 0.68 |
| 6 (n = 20) | Nicotine 2–46 weeks/NNK | 85 | 65 | 50 | 4.4 ± 2.6 | 0.8 ± 0.70 | 0.70 ± 0.80 |
Treatments were as described in Fig. 1 and Table 3. Histological analysis was not carried out on lungs from 5 mice in Groups 1 and 2. Premature deaths occurred in Groups 2–5 as follows: Group 2, one death, week 3, cause of death – unknown, no microscopic analysis of tissues; Group 3, one death week 5 cause of death – unknown and one death at week 29 cause of death – disseminated lymphoma, pulmonary adenomas present; Group 4, one death week 43 cause of death – respiratory distress, adenocarcinoma with multifocal pulmonary adenomas, bronchiolar epithelial hyperplasia, alveolar histiocytosis and hemorrhage and one death at week 37 after NNK injection. Cause of death – dorsal skin tumor (a large non-malignant hematoma) pulmonary adenomas present; Group 5, one death at week 11 euthanized due to “labored breathing” no microscopic analysis of tissues.
Discussion
Nicotine has been suggested to be a promoter of lung cancer. This suggestion is based on numerous in vitro studies and several short term xenograft studies (5–7,11,12). In the study presented here we saw no effect of chronic nicotine consumption on the incidence, multiplicity or progression of NNK-induced lung tumors in the A/J mouse. This was true whether nicotine was consumed before or after NNK administration. In this model system, which has been used extensively to study NNK carcinogenesis, nicotine did not affect either the initiation or progression of lung tumors. A recent study by Maier et al also reported that nicotine administered in the drinking water had no effect on lung tumorigenesis in two additional mouse models (42).
Nicotine metabolism in the mouse and in humans is qualitatively similar. Metabolism is catalyzed by closely related enzymes, P450 2A5 and P450 2A6, and the major metabolites in both species are cotinine and trans 3′-hydroxycotinine (25,43). In smokers urine, the proportion of nicotine to cotinine to trans 3′-hydroxycotinine is typically 1 to 1.5 to 4 (25). However, in the A/J mouse the average proportions of these three compounds was 1 to 3 to 14, consistent with the greater catalytic efficiency of the mouse enzyme, P450 2A5 compared to its human ortholog CYP2A6 (26). A high efficiency of nicotine metabolism has also been reported in other mouse strains (43,44).
As we initiated our study, Davis et al reported that nicotine, administered as three weekly interperitoneal injections [1 mg (4.8 μmol)/kg], increased both the number and size of NNK-induced tumors in the A/J mouse. This was a small study with a number of limitations. The weekly dose of nicotine used in their study, 0.36 μmol/mouse (assuming an average weight of 25 g) was almost 20- fold lower than the average weekly dose of nicotine consumed in our study, 6.6 μmol/mouse (15 ml per week 0.44 μmol nicotine/ml, Fig. 2). Administering nicotine by injection may result in a higher peak nicotine concentration, than when nicotine is consumed in the drinking water. However, the mice would have experienced this nicotine concentration for less than 1 h three days a week. No measure of plasma or urinary nicotine or cotinine was reported. The number of NNK induced tumors reported for nicotine treated and untreated animals was 16 ± 3 and 10 ± 3, n=8 mice per group. This is a small number of mice for which to detect a significant difference in tumor number. In the A/J mouse the variation in lung tumors per mouse is fairly large. In our study, it ranged from 6 to 41 in all NNK treated mice (n = 76) and the standard deviation for groups of 20 was 25%. In a recent study by Memmott et al, which used a similar NNK dosing protocol to that used by Davis the number of lung tumors per mouse in NNK treated animals ranged from 10 to 40 (n=15) (45).
The main limitation of our study is that due to the rapid metabolism of nicotine in the mouse, circulating nicotine levels were significantly lower than in smokers. However, the daily dose of nicotine per kg body weight is much higher than that of a smoker, and peak nicotine concentrations were at least 11 ng/ml, 20 times higher than circulating levels. The strength of the study is the chronic administration of nicotine and the length of administration. By following animals for 44 weeks after NNK administration we were able to assess the progression of adenomas to adenocarcinomas. As noted in the results (Table 3) there was a non-significant increased number of carcinomas in groups 4 and 6 compared to groups 3 and 5. There was no parallel decrease in adenomas or adenomas with dysplasia, consistent with this observation being due to chance.
In summary, there were three key outcomes of our studies on the effect of nicotine on tumorigenesis in the A/J mouse, a species which is highly susceptible to lung tumors: 1) Chronic nicotine consumption alone did not induce lung tumors. 2) Nicotine consumption up until the time of NNK administration did not decrease (or increase) tumor incidence and 3) chronic nicotine consumption had no significant effect on tumor incidence, multiplicity or progression. These negative findings in a commonly used model of human lung carcinogenesis should lead us to question the interpretation and relevance of in vitro and short term xenograft studies of nicotine’s effect on cancer cells. Nicotine is a ligand for the nAChR and therefore increased exposure to nicotine will trigger many downstream changes but what the effect of chronic nicotine exposure is on these pathways in a smoker or ex-smoker is not clear.
Acknowledgments
We thank Katherine Wickham for assisting in the analysis of nicotine and its metabolites in urine and plasma, Mitzi Lewellen for assistance in carrying out the animal studies, Josh Parker and Paula Overn for histology services, and Robin Bliss for statistical analysis. We also thank Stephen S. Hecht for useful discussions on the design and analysis of the tumorigenicity study.
Grant Support.
This study was supported by a grant from the Masonic Cancer Center and funds from the Animal Care and Research Program at the University of Minnesota and NIH (CA-84529). LC/MS/MS analysis was carried out in the Analytical Biochemistry Core, histology was carried out in the Comparative Pathology Shared Resource, and statistical analysis carried out in the Biostatistics and Bioinformatics Shared Resource of the Masonic Cancer Center, supported in part by CA-77598.
Reference List
- 1.CDC. Morbidity and Mortality Weekly Report 57. 2008. Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses --- United States, 2000–2004; pp. 1226–1228. [PubMed] [Google Scholar]
- 2.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–36. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 3.Apelberg BJ, Onicescu G, Avila-Tang E, Samet JM. Estimating the risks and benefits of nicotine replacement therapy for smoking cessation in the United States. Am J Public Health. 2010;100:341–48. doi: 10.2105/AJPH.2008.147223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spindel ER. Is nicotine the estrogen of lung cancer? Am J Respir Crit Care Med. 2009;179:1081–82. doi: 10.1164/rccm.200901-0013ED. [DOI] [PubMed] [Google Scholar]
- 5.Heeschen C, Jang JJ, Weis M, Pathak A, Kaji S, Hu RS, et al. Nicotine stimulates angiogenesis and promotes tumor growth and atherosclerosis. Nat Med. 2001;7:833–39. doi: 10.1038/89961. [DOI] [PubMed] [Google Scholar]
- 6.Oloris SC, Frazer-Abel AA, Jubala CM, Fosmire SP, Helm KM, Robinson SR, et al. Nicotine-mediated signals modulate cell death and survival of T lymphocytes. Toxicol Appl Pharmacol. 2010;242:299–309. doi: 10.1016/j.taap.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Improgo MR, Scofield MD, Tapper AR, Gardner PD. The nicotinic acetylcholine receptor CHRNA5/A3/B4 gene cluster: dual role in nicotine addiction and lung cancer. Prog Neurobiol. 2010;92:212–26. doi: 10.1016/j.pneurobio.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hecht SS. Tobacco carcinogens, their biomarkers, and tobacco-induced cancer. Nature Rev Cancer. 2003;3:733–44. doi: 10.1038/nrc1190. [DOI] [PubMed] [Google Scholar]
- 9.Waldum HL, Nilsen OG, Nilsen T, Rorvik H, Syversen V, Sanvik AK, et al. Long-term effects of inhaled nicotine. Life Sci. 1996;58:1339–46. doi: 10.1016/0024-3205(96)00100-2. [DOI] [PubMed] [Google Scholar]
- 10.Schuller HM, McGavin MD, Orloff M, Riechert A, Porter B. Simultaneous exposure to nicotine and hyperoxia causes tumors in hamsters. Lab Invest. 1995;73:448–56. [PubMed] [Google Scholar]
- 11.Jarzynka MJ, Guo P, Bar-Joseph I, Hu B, Cheng SY. Estradiol and nicotine exposure enhances A549 bronchioloalveolar carcinoma xenograft growth in mice through the stimulation of angiogenesis. Int J Oncol. 2006;28:337–44. [PMC free article] [PubMed] [Google Scholar]
- 12.Davis R, Rizwani W, Banerjee S, Kovacs M, Haura E, Coppola D, et al. Nicotine promotes tumor growth and metastasis in mouse models of lung cancer. PLoS ONE. 2009;4:e7524. doi: 10.1371/journal.pone.0007524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al Wadei HA, Plummer HK, III, Schuller HM. Nicotine stimulates pancreatic cancer xenografts by systemic increase in stress neurotransmitters and suppression of the inhibitory neurotransmitter gamma-aminobutyric acid. Carcinogenesis. 2009;30:506–11. doi: 10.1093/carcin/bgp010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amos CI, Wu X, Broderick P, Gorlov IP, Gu J, Eisen T, et al. Genome-wide association scan of tag SNPs identifies a susceptibility locus for lung cancer at 15q25.1. Nat Genet. 2008;40:616–22. doi: 10.1038/ng.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hung RJ, McKay JD, Gaborieau V, Boffetta P, Hashibe M, Zaridze D, et al. A susceptibility locus for lung cancer maps to nicotinic acetylcholine receptor subunit genes on 15q25. Nature. 2008;452:633–37. doi: 10.1038/nature06885. [DOI] [PubMed] [Google Scholar]
- 16.Thorgeirsson TE, Geller F, Sulem P, Rafnar T, Wiste A, Magnusson KP, et al. A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature. 2008;452:638–42. doi: 10.1038/nature06846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spitz MR, Amos CI, Dong Q, Lin J, Wu X. The CHRNA5-A3 region on chromosome 15q24–25.1 is a risk factor both for nicotine dependence and for lung cancer. J Natl Cancer Inst. 2008;100:1552–56. doi: 10.1093/jnci/djn363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuehn BM. FDA considering data on long-term use of nicotine replacement therapy products. JAMA. 2010;304:2580. doi: 10.1001/jama.2010.1804. [DOI] [PubMed] [Google Scholar]
- 19.Galvan A, Dragani TA. Nicotine dependence may link the 15q25 locus to lung cancer risk. Carcinogenesis. 2010;31:331–33. doi: 10.1093/carcin/bgp282. [DOI] [PubMed] [Google Scholar]
- 20.Murray RP, Connett JE, Zapawa LM. Does nicotine replacement therapy cause cancer? Evidence from the Lung Health Study. Nicotine Tob Res. 2009;11:1076–82. doi: 10.1093/ntr/ntp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Konishi H, Wu J, Cooke JP. Chronic exposure to nicotine impairs cholinergic angiogenesis. Vasc Med. 2010;15:47–54. doi: 10.1177/1358863X09106326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown B, Avalos J, Lee C, Doolittle D. The effect of tobacco smoke, nicotine, and cotinine on the mutagenicity of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) Mutat Res. 2001;494:21–29. doi: 10.1016/s1383-5718(01)00174-7. [DOI] [PubMed] [Google Scholar]
- 23.Richter E, Tricker AR. Nicotine inhibits the metabolic activation of the tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in rats. Carcinogenesis. 1994;15:1061–64. doi: 10.1093/carcin/15.5.1061. [DOI] [PubMed] [Google Scholar]
- 24.Richter E, Tricker AR. Effect of nicotine, cotinine and phenethyl isothiocyanate on 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) metabolism in the Syrian golden hamster. Toxicology. 2002;179:95–103. doi: 10.1016/s0300-483x(02)00321-9. [DOI] [PubMed] [Google Scholar]
- 25.Hukkanen J, Jacob P, III, Benowitz NL. Metabolism and disposition kinetics of nicotine. Pharmacol Rev. 2005;57:79–115. doi: 10.1124/pr.57.1.3. [DOI] [PubMed] [Google Scholar]
- 26.Murphy SE, Raulinaitis V, Brown KM. Nicotine 5′-oxidation and methyl oxidation by P450 2A enzymes. Drug Metab Dispos. 2005;13:1166–73. doi: 10.1124/dmd.105.004549. [DOI] [PubMed] [Google Scholar]
- 27.von Weymarn LB, Brown KM, Murphy SE. Inactivation of CYP2A6 and CYP2A13 during nicotine metabolism. J Pharmacol Exp Ther. 2006;316:295–303. doi: 10.1124/jpet.105.091306. [DOI] [PubMed] [Google Scholar]
- 28.Jalas JR, Hecht SS, Murphy SE. Cytochrome P450 enzymes as catalysts of metabolism of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK), a tobacco-specific carcinogen. Chem Res Toxicol. 2005;18:95–110. doi: 10.1021/tx049847p. [DOI] [PubMed] [Google Scholar]
- 29.Zhang X, D’Agostino J, Wu H, Zhang QY, von Weymarn L, Murphy SE, et al. CYP2A13: variable expression and role in human lung microsomal metabolic activation of the tobacco-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone. J Pharmacol Exp Ther. 2007;323:570–78. doi: 10.1124/jpet.107.127068. [DOI] [PubMed] [Google Scholar]
- 30.Malkinson AM. Primary lung tumors in mice as an aid for understanding, preventing, and treating human adenocarcinoma of the lung. Lung Cancer. 2001;32:265–79. doi: 10.1016/s0169-5002(00)00232-4. [DOI] [PubMed] [Google Scholar]
- 31.Hecht SS. Biochemistry, biology, and carcinogenicity of tobacco-specific N-nitrosamines. Chem Res Toxicol. 1998;11:559–603. doi: 10.1021/tx980005y. [DOI] [PubMed] [Google Scholar]
- 32.Hecht SS, Jordan KG, Choi CI, Trushin N. Effects of deuterium substitution on the tumorigenicity of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol in A/J mice. Carcinogenesis. 1990;11:1017–20. doi: 10.1093/carcin/11.6.1017. [DOI] [PubMed] [Google Scholar]
- 33.Peterson LA, Hecht SS. O6-Methylguanine is a critical determinant of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone tumorigenesis in A/J mouse lung. Cancer Res. 1991;51:5557–64. [PubMed] [Google Scholar]
- 34.Weng Y, Fang C, Turesky RJ, Behr M, Kaminsky LS, Ding X. Determination of the role of target tissue metabolism in lung carcinogenesis using conditional cytochrome P450 reductase-null mice. Cancer Res. 2007;67:7825–32. doi: 10.1158/0008-5472.CAN-07-1006. [DOI] [PubMed] [Google Scholar]
- 35.Kassie F, Anderson LB, Scherber R, Yu N, Lahti D, Upadhyaya P, et al. Indole-3-carbinol inhibits 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone plus benzo(a)pyrene-induced lung tumorigenesis in A/J mice and modulates carcinogen-induced alterations in protein levels. Cancer Res. 2007;67:6502–11. doi: 10.1158/0008-5472.CAN-06-4438. [DOI] [PubMed] [Google Scholar]
- 36.Hecht SS, Morse MA, Amin S, Stoner GD, Jordan KG, Choi CI, et al. Rapid single-dose model for lung tumor induction in A/J mice by 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone and the effect of diet. Carcinogenesis. 1989;10:1901–04. doi: 10.1093/carcin/10.10.1901. [DOI] [PubMed] [Google Scholar]
- 37.Nikitin AY, Alcaraz A, Anver MR, Bronson RT, Cardiff RD, Dixon D, et al. Classification of proliferative pulmonary lesions of the mouse: recommendations of the mouse models of human cancers consortium. Cancer Res. 2004;64:2307–16. doi: 10.1158/0008-5472.can-03-3376. [DOI] [PubMed] [Google Scholar]
- 38.Wong HL, Murphy SE, Wang M, Hecht SS. Comparative metabolism of N-nitrosopiperidine and N-nitrosopyrrolidine by rat liver and esophageal microsomes and cytochrome P450 2A3. Carcinogenesis. 2003;24:291–300. doi: 10.1093/carcin/24.2.291. [DOI] [PubMed] [Google Scholar]
- 39.von Weymarn LB, Felicia ND, Ding X, Murphy SE. N-Nitrosobenzylmethylamine α-hydroxylation and coumarin 7-hydroxylation by rat esophageal microsomes and cytochrome P450 2A3 and 2A6 enzymes. Chem Res Toxicol. 1999;12:1254–61. doi: 10.1021/tx990128y. [DOI] [PubMed] [Google Scholar]
- 40.Upadhyaya P, Lindgren BR, Hecht SS. Comparative levels of O6-methylguanine, pyridyloxobutyl-, and pyridylhydroxybutyl-DNA adducts in lung and liver of rats treated chronically with the tobacco-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone. Drug Metab Dispos. 2009;37:1147–51. doi: 10.1124/dmd.109.027078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bloom AJ, Hinrichs AL, Wang JC, von Weymarn LB, Bierut LJ, Goate A, et al. The Contribution of Common CYP2A6 Alleles to Variation in Nicotine Metabolism Among European Americans. Pharmacogenet Genomics. 2011 doi: 10.1097/FPC.0b013e328346e8c0. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maier CR, Hollander C, Dogan I, Dennis PA. Nicotine does not enhance lung tumorigenesis in K-Ras-driven mouse models of lung cancer. Cancer Prev Res. 2011 doi: 10.1158/1940-6207.CAPR-11-0365. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raunio H, Pokela N, Puhakainen K, Rahnasto M, Mauriala T, Auriola S, et al. Nicotine metabolism and urinary elimination in mouse: in vitro and in vivo. Xenobiotica. 2008;38:34–47. doi: 10.1080/00498250701708539. [DOI] [PubMed] [Google Scholar]
- 44.Siu EC, Tyndale RF. Characterization and comparison of nicotine and cotinine metabolism in vitro and in vivo in DBA/2 and C57BL/6 mice. Mol Pharmacol. 2007;71:826–34. doi: 10.1124/mol.106.032086. [DOI] [PubMed] [Google Scholar]
- 45.Memmott RM, Mercado JR, Maier CR, Kawabata S, Fox SD, Dennis PA. Metformin prevents tobacco carcinogen--induced lung tumorigenesis. Cancer Prev Res (Phila) 2010;3:1066–76. doi: 10.1158/1940-6207.CAPR-10-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]