The burden of diabetes is enormous and escalating at an alarming rate (1–3). Nearly 26 million Americans have the disease, including over 10% of the total adult population and over 25% of the population aged 65 years and older. While most of those individuals have type 2 diabetes, nearly 1 million Americans have type 1 diabetes. An additional 79 million American adults have prediabetes, which, when added to those with diabetes, suggests that nearly half of the adult population currently has impaired glucose metabolism (1). If present trends continue, as many as one in three American adults will be diagnosed with diabetes by 2050; the majority of cases will include older adults and racial and ethnic minorities (4).
The high prevalence of diabetes, especially among the aging population, comes at a considerable economic cost. In 2007, diabetes and prediabetes accounted for approximately $218 billion in direct medical costs and lost productivity in the U.S. (5). Health care expenditures for individuals with diabetes are 2.3 times greater than expenditures for those without diabetes, and diabetes complications account for a significant proportion of those costs (5). Diabetes significantly increases the risk of cardiovascular events and death, and is the leading cause of end-stage renal disease, blindness, and nontraumatic lower-limb amputations in the U.S. (1). Despite medical advances significantly decreasing the risk of complications and associated mortality, the trajectory of these declines has been blunted by the overall increase in the number of people afflicted with diabetes.
Decades of intensive research have resulted in vastly improved understanding of the pathophysiology and impact of diabetes, as well as a host of new and improved therapies. The translation of this research into practice has led to reductions in chronic complications and mortality in people with diabetes (6). Yet, as the incidence and prevalence of both type 1 and type 2 diabetes continue to escalate, the need for innovative research and associated evidence-based care and prevention is increasingly vital to protect the public health and to help control the surging costs of diabetes-related health care.
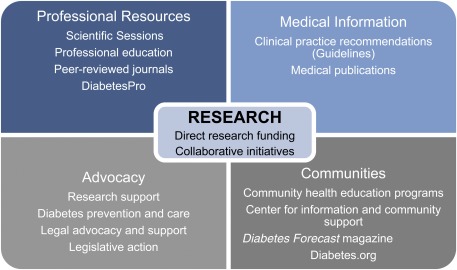
The American Diabetes Association (ADA) is committed to improving the lives of all those with or at risk for the disease, irrespective of the disease type, age, or ethnic origin of the individual with the disease. Our vision is a life free of diabetes and its burdens. Research holds the key to understanding and combating this illness, and stemming the rising tide of the epidemic. However, the importance of the ADA as an organization is seen not only in its commitment to research funding, but also in showcasing new research findings in the most prestigious scientific meeting and the leading scientific journals dedicated to diabetes in the world, synthesis and interpretation of research into position statements and standards of care, efforts to translate research findings to community-based practice, and advocacy to foster more research. All of these activities together lead to translation of the research from the bench to the clinic and to better outcomes for people with diabetes (Fig. 1). In this article, we will describe these activities and their impact on the field of diabetes research, prevention, care, and public health.
Figure 1.
Research is central to many of the key mission activities at the ADA. The ADA directly supports research through the research program, but scientific and medical research in general is also a critical component for many of the other activities that the organization engages in to support people with diabetes, including professional publications and meetings, medical information, community programs, and advocacy.
RESEARCH AT THE ADA
Research is at the core of the ADA’s efforts to serve its constituency of individuals with diabetes and those at risk for the disease. The association has a long history of research support and engagement. The first direct ADA research grants were awarded in 1952. In the late 1970s, the ADA’s research funding was centralized into a grant program modeled after that of the National Institutes of Health (NIH), with operational and scientific oversight housed in the national office. The program is guided by two national volunteer committees: the Research Policy Committee, which advises on research strategy, portfolio management, and special programs, and the Research Grant Review Committee, a panel of independent, volunteer scientific and medical experts in a broad array of disciplines who review and prioritize all applications for the ADA research support.
Since the inception of the research grant program, the ADA has invested more than $600 million in diabetes research, funding nearly 4,000 individual projects. In 2011 alone, the ADA committed $34.6 million to research and supported more than 400 ongoing projects at 139 leading research institutions across the U.S. A recent analysis of the ADA-funded investigators illustrates the positive impact associated with these efforts.
In a representative cohort of investigators supported in fiscal year 2005, fully 98% remained dedicated to diabetes research through 2011. These individuals were extremely productive, with the average ADA award directly resulting in approximately six peer-reviewed primary publications. They became leaders in the diabetes scientific community, with more than a third of investigators assuming a leadership position (e.g., directors, chairs, chiefs) during that timeframe, and nearly half receiving scientific achievement awards. Moreover, and perhaps most importantly, 85% of the investigators received additional funding for their research in the 5 years subsequent to their award. These findings indicate that the ADA research funding provided the foundation for researchers to successfully compete for further research dollars, thus increasing the prospect of meaningful contributions to scientific knowledge.
THE ADA RESEARCH STRATEGY
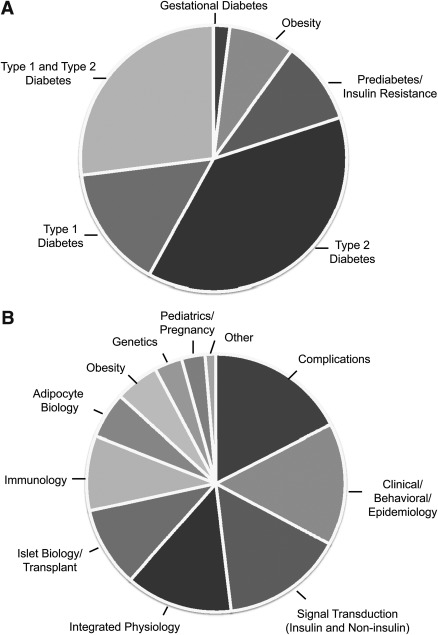
The ADA supports research across the broad spectrum of diabetes and related disease states (e.g., obesity, prediabetes, type 2 diabetes, type 1 diabetes, gestational diabetes mellitus [Fig. 2A]) and topic areas (e.g., diabetes complications, cell biology, integrated physiology, epidemiology [Fig. 2B]). Funding decisions are based primarily on scientific merit as assessed during a rigorous peer-review process. The intent behind this funding strategy is first and foremost to serve all people affected by diabetes and its complications. It is increasingly recognized that although type 1 and type 2 diabetes have distinct etiologies, they share many common underlying cellular processes (e.g., inflammation, immune responses, β-cell failure) and are associated with the same diabetes-related complications. By addressing all aspects of the disease, it is likely that research supported through these grants will impact knowledge of treatment and prevention of diabetes generally.
Figure 2.
The ADA research program supports research across the broad spectrum of diabetes types and research topic areas (proportions of 2011 allocations in dollars). A: The majority of the research portfolio is dedicated to research that is relevant to type 1 and type 2 diabetes, but gestational diabetes mellitus, obesity, and insulin-resistant states are also represented. B: The topic areas represented in the program.
Another key aspect of the ADA research strategy is to provide a complementary, rather than redundant, source of funding for diabetes researchers. Many of the ADA grant opportunities support areas of high need (early investigators, innovative projects) that may not otherwise be funded or for which bridging/start-up funding may be necessary to compete for future grant support by large federal organizations, such as the NIH. The high success rate of ADA investigators obtaining subsequent funding exemplifies the success of this approach. From the analysis of ADA researchers discussed above, an initial investment of ∼$56 million from the ADA research program translated into ∼$412 million in subsequent research support to these investigators from other sources within 5 years. This not only fills an important need in the research community, but also supports the Association’s mission to fund the most promising and innovative areas of investigation.
EXPANDING THE FIELD OF DIABETES RESEARCH
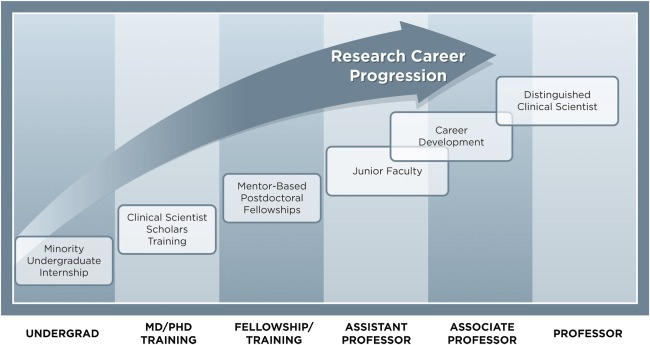
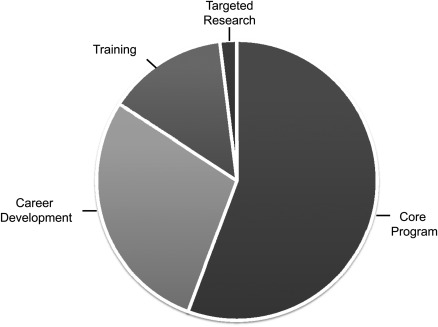
With increasingly limited federal budgets and greater competition for diabetes research dollars, early investigators have been disproportionately impacted (7), thus limiting opportunities for career development. Whereas the average age of newly independent investigators receiving an initial RO1 from the NIH is reportedly 42 years of age (8), research shows that the ages between 30 and 40 years can be the most productive in a researcher’s career (9,10). Unfortunately, in today’s environment, many early-career scientists have difficulty efficiently transitioning to independent research careers and as a result are choosing paths other than academic research. Those who do choose to pursue academic research spend a disproportionate amount of time applying for grants, which, in many cases, do not adequately support their research. This detracts from their ability to fully capitalize on original and uninhibited scientific inquiries and approaches during this critical time. The ADA research program strives to bridge this gap through a number of specific grant mechanisms targeting early investigators, who are either in research training (i.e., fellowship or postdoctoral positions) or in an early academic career stage (Fig. 3). In 2011, approximately a third of the annual research budget was allocated to these funding opportunities (Fig. 4).
Figure 3.
Training and career development grant opportunities. The ADA offers grant opportunities for training and career development that cover the spectrum of academic career stages. Approximately 38% of the budget of the program in 2011 was dedicated to training and career development awards.
Figure 4.
Portfolio distribution of awards supported by the ADA in 2011 (proportions of 2011 allocations in dollars). The majority of the portfolio is dedicated to support of Core Program awards including basic, clinical/translational, and innovation projects. Approximately a quarter of the budget supported career development awards, followed by training grants and targeted research.
This funding is specifically intended to support the ADA’s mission to maintain talent in the field of diabetes research, provide a foundation for career progression, and build a strong scientific case for subsequent federal funding for their work. Thus far, the ADA has successfully accomplished each of these objectives, with 98% of researchers supported through the career development program staying in the field of diabetes research, 87% of them receiving federal funding for their work, and 82% receiving a promotion in the 5 years subsequent to their award. Yet despite these successes, it is clear that more is needed to attract and retain talented researchers in the field of diabetes research and to ensure that they have the necessary resources to conduct truly transformational research.
To this end, the Association is currently undertaking a capital campaign to support a new and innovative award program, the Pathway program. The intent of this program is to further expand the field of diabetes research by supporting exceptional scientists performing innovative and transformational research. This program will be available to individuals who have been identified as having extraordinary potential to make significant contributions and are early in their independent research careers, or are undertaking a significant change in their research focus. These awards will encourage the exploration of new ideas and multidisciplinary approaches to diabetes research. The recipients will benefit from a substantial financial commitment over a longer period of time than is traditionally offered. To further increase the likelihood of success and progress, this program will also provide flexibility in the use of the funds, extensive individualized mentorship from distinguished researchers, and frequent opportunities and incentives for interaction and collaboration. Through this effort, the ADA will help launch the next generation of diabetes researchers, while accelerating scientific discoveries that will positively impact people with diabetes. Importantly, this program is incremental and will augment the existing programs.
INNOVATION AND TRANSLATION
The Association encourages innovative and translational research through a number of specific programs targeting these areas. Risk tolerance is a necessary component of supporting highly innovative and truly translational research as it is difficult a priori to definitively determine the likelihood of success in these areas. However, in the cases where projects are successful, there is an enhanced probability of moving the field ahead rapidly and significantly. The Association’s innovation grant mechanisms support ideas with solid theoretical foundations and a high probability to impact patients with diabetes, but without a requirement for significant preliminary data or previous proof of concept. Numerous successes have resulted from this program, including identification of potential biomarkers and innovative new approaches for combating the autoimmune response in type 1 diabetes (11).
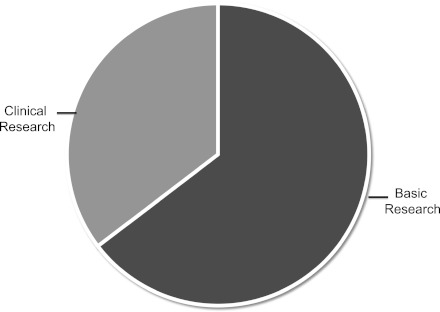
Traditionally, the ADA research program provided a majority of its funding to basic science research. However, as the program has matured, it has become clear that translational research, at both the bench-to-clinic and clinic-to-community interfaces, is critical for improving patient outcomes. As a result, the Association has made a concerted effort to increase the proportion of translational and clinical grants that are awarded and, in the last 5 years, has increased this proportion of clinical work in the portfolio to ∼35% (Fig. 5). This shift in emphasis facilitates more laboratory-to-human translation, exploratory clinical work, clinic-to-community translation, and patient-centered outcomes research.
Figure 5.
Portfolio distribution of basic and clinical research at the ADA in 2011 (proportions of 2011 allocations in dollars). The proportion of clinical and translational research supported by the Association has increased over the last 5 years and now makes up approximately a third of the overall portfolio. The majority of the portfolio is dedicated to basic research.
STRATEGIC RESEARCH PRIORITY AREAS
While the majority of ADA research dollars are allocated to investigator-initiated research over a wide range of topic areas, a percentage of the portfolio is used to support targeted and collaborative research initiatives in strategically important areas. Most targeted research funding is subsidized by collaborative sponsorships with individual donors, other funders of diabetes research, or industry partners. These opportunities are announced in specific requests for applications throughout the year. Recent examples of targeted initiatives include grants that have supported novel research on diabetes care delivery, studies examining the neurohormonal control of metabolism, and clinical and translational efforts to understand the impact of hypoglycemia. Larger federal research initiatives, often originating with the NIH, have also been supported with ADA research contributions—most notably the Diabetes Prevention Trial–Type 1 (DPT-1), the Diabetes Prevention Program (DPP), the Hyperglycemia and Adverse Pregnancy Outcome Study (HAPO), and the Veterans Affairs Diabetes Trial (VADT).
Although targeted research is not strictly limited to the following areas, these topics serve as strategic priorities to guide targeted and collaborative activities.
Type 2 diabetes prevention
Early identification of impaired glucose tolerance, coupled with weight loss and physical exercise interventions, can delay the onset of type 2 diabetes significantly. The ADA was a critical collaborative partner in the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)-sponsored DPP, which demonstrated that lifestyle modification or treatment with metformin can delay the incidence of developing diabetes by 58% and 31%, respectively. Findings indicated that even modest weight loss can significantly minimize risk (12). In addition, a recent analysis of 10-year follow-up data from the DPP showed that both lifestyle intervention and metformin treatment were highly cost-effective treatments for patients with prediabetes (13).
Despite this strong evidence, diabetes prevention is often not emphasized or practiced. Reasons for this may include lack of awareness in the general population of the seriousness of the attendant risks of diabetes, insufficient clinical efforts to screen patients, limited availability of prevention programs, and societal barriers to adherence to healthy behavior. In the DPP, ∼11% of participants in the control group progressed to type 2 diabetes each year (12). However, the DPP participants were selected as a particularly high-risk cohort, with most having combined impaired glucose tolerance and impaired fasting glucose. For the 79 million individuals in the U.S. with the broader spectrum of prediabetes, reliable and straightforward means for distinguishing those who will progress to diabetes from those who will not are needed to most efficiently target resources. Further studies characterizing the pathways that underlie the development of the disease are necessary for identification of novel risk factors and early biomarkers that could predict progression and facilitate identification of the population in need of preventative treatment. Studies aimed at translating research-based prevention programs into clinical and community-based practice, and studies examining cost-effective and novel means of delivering prevention are also necessary. Due to the size and trajectory of the problem, the potential benefits that could result from subsequent prevention strategies are enormous.
Type 1 diabetes prevention
Analogous prerequisites for widespread prevention of type 2 diabetes also apply to prevention of type 1 diabetes: the identification of those in the general population that are at highest risk and the identification of the best therapies and the point at which interventions are appropriate and effective. Since the identification of an autoimmune origin of type 1 diabetes, investigators have been examining ways to modulate the immune system to prevent (or reverse) the autoimmune process and preserve or restore β-cell function in patients at risk for or early in the course of type 1 diabetes. However, promising findings in research with animal models have often failed to translate to human cases of diabetes (14). Large-scale federally supported clinical research initiatives, including Type 1 Diabetes TrialNet and the Immune Tolerance Network, provide important resources for the diabetes community to examine new approaches and therapies. Additional research defining the underlying pathways and identifying potential treatment strategies, coupled with active integration with these resources, is essential for progress. Once effective prevention strategies are identified, it will be critical to facilitate widespread clinical translation to advance prevention efforts.
Complications
Although the etiologies differ, both type 1 and type 2 diabetes can result in many of the same acute and chronic complications. Cardiovascular disease accounts for the majority of mortality in patients with type 2 diabetes. Recent large trials, originally presented at the ADA Scientific Sessions in 2008, have failed to demonstrate that intensive glycemic control strategies can necessarily reduce this burden (15–17). Although control of other cardiovascular risk factors continues to be a mainstay of prevention, a greater understanding of the link between disordered glycemic control and the development of cardiovascular disease remains an important research objective.
Research is also needed to address chronic microvascular complications of neuropathy, nephropathy, retinopathy, as well as hypoglycemia and severe hyperglycemic states, which also represent a significant proportion of the morbidity and costs of diabetes. The identification of populations of patients with diabetes that are particularly resistant or highly susceptible to the development of these complications may provide important clues to the genetic and metabolic precursors. Systems biology approaches examining genetic and metabolic profiles, and the interfaces between pathways, may provide a more global understanding of the commonalities and distinct effects of hyperglycemia on various organ systems. Once the physiological pathways involved in these processes are identified, they must be carefully dissected to elucidate new targets for the development of therapeutic agents.
The ADA has and will continue to work in collaboration with other organizations, including industry partners, JDRF, the National Kidney Foundation, and others, to address critical complications research needs. Through support of specific grant opportunities and collaborative projects, the ADA will continue to provide support for research in these areas. Planned work group and consensus reports on hypoglycemia and chronic kidney disease emphasize the importance that the ADA places on understanding the complexity of the molecular and cellular processes underlying these complications, and the output from such activities will provide further guidance for future investigations in these areas.
Diabetes care in subpopulations
Comparing the effects of therapies or treatment strategies in diverse and representative patient populations can identify particular benefits or specific risks in various stages of disease, in demographic subgroups (e.g., ethnicity, age, sex), and in the context of particular comorbid conditions. The landmark Action to Control Cardiovascular Risk in Diabetes (ACCORD), Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE), and VADT studies found that individualizing treatment for patients is critical to delivering the best and most appropriate care and that more data are needed in specific populations to inform these decisions (15–17). Unfortunately, many of the large-scale clinical studies that examine the effects of therapies do not capture large proportions of these patient populations. One example is the older adult population, one that is highly impacted by diabetes, but relatively understudied. The ADA recently hosted an older adult consensus conference examining the specific considerations and needs of this population. The outcomes of the conference, including research priorities, will be published to guide the community as the ADA addresses this and other important subgroups. With expanding numbers of therapeutic choices, a clear understanding of the benefits and risks associated with the available therapies is extremely important for clinicians to deliver the best possible care to their patients and for patients to make informed shared decisions about their treatment.
Community translation
The ADA’s support for translational research and programs extends beyond the clinical setting. The Association understands the need to address awareness, behavioral and environmental barriers, and disparities in the community where people work and live. Modification of antecedents, including 1) awareness of prediabetes or diabetes status; 2) knowledge of diabetes physiology, etiology, complications, risk factors, and health behaviors (e.g., diet, exercise, and seeking health care); 3) attitudes pertaining to health status; and 4) intentions and self-efficacy to improve behaviors, has been directly linked to decreased incidence of diabetes and complications (18–21). Unlike clinical settings, where time, support, and access are often limited, community-based programs can provide culturally and age-appropriate education and tools designed to modify those antecedents and, in turn, delay or prevent the onset of diabetes, or reduce risks of its complications (22,23).
To maximize the positive impact and cost-effectiveness, the ADA is currently undertaking rigorous outcomes research on its own community programs to effectively target its resources and to complement published findings on community interventions. Moreover, the ADA research program has and will continue to fund external research to identify novel and innovative approaches to community-based interventions.
MEASURING IMPACT
With continuing economic pressures and constrained federal budgets, the ADA has experienced an increase in demand for diabetes research dollars, reflected in the steady growth in applications received each year. While increased volume results in ever higher-quality research being supported, it also presents challenges in meeting the funding demands of the diabetes research community. The Association is committed to meeting these challenges through strong stewardship of its current support, developing innovative new programs to address critical needs, and through careful measurement and frequent adjustments to strategies to maintain direct progress toward goals. Impact assessments will evaluate progress against the following strategic long-term metrics: By 2015 there will be an increase in ADA award recipients who receive subsequent federal funding, an increase in total federal funding for diabetes research, and an increase in ADA research funding. To support these goals, the organization will increase career development resources for ADA grant recipients to better enable them to successfully compete for federal research dollars, will work to attract new talent to the field, and will expand the core research program to support high-quality and innovative basic, clinical, and translational science across the full spectrum of diabetes research.
The Association will continue to collect annual data to capture meaningful antecedents of successful attainment of the longer-term goals, including retention and advancement of principal investigators in diabetes research, peer-reviewed publications, patents, and subsequent federal funding. Using these findings, the ADA research programs can be strengthened and modified to ensure progress toward the prevention, treatment, and ultimate cure of diabetes.
The success of research is critically important to reach the Association’s strategic goals. Meaningful research outcomes have and will continue to advance the field by expediting the identification of those with diabetes before the onset of complications, reducing disparities among those at high risk, ensuring the best clinical care, preventing diabetes-related mortality, and guiding the development and refinement of both programmatic and funding strategies.
DISSEMINATION OF RESEARCH INFORMATION
Another key requirement for research progress is rapid and broad dissemination of research results throughout the research community and to the public, something the ADA is well placed to accomplish. Each year, the ADA’s annual Scientific Sessions serves as the largest meeting of diabetes researchers and clinicians in the world. The Scientific Sessions is the prime venue for the presentation of cutting-edge clinical diabetes research findings including results from the Diabetes Control and Complications Trial (DCCT), ACCORD, ADVANCE, VADT, Targeting Inflammation using Salsalate for Type-2 Diabetes (TINSAL-T2D), and HAPO trials, just to name a few. For critical or emerging areas of research, the Association also hosts consensus conferences and special scientific meetings to gather experts for discussion and debate. The outcomes of these meetings are disseminated to the scientific community to identify gaps, guide research priorities, and improve clinical practice. The Diabetes and Cancer consensus conference provides an illustrative example of the intent and impact of these meetings. Following the publication of epidemiological data suggesting a potential association between treatments for hyperglycemia and the development of cancer (24–27), the ADA, in collaboration with the American Cancer Society, organized an expert conference to review the evidence and develop a comprehensive consensus statement that was subsequently published in Diabetes Care (28). This statement addressed key questions regarding the relationship between diabetes and cancer and highlighted areas where additional research would be required.
The ADA was also the forerunner in clinical diabetes guidelines, initiating development in the 1980s—a practice subsequently adopted by many other organizations representing a wide range of fields within public health. The Association’s flagship clinical practice recommendation, “Standards of Medical Care in Diabetes,” has been revised and published annually for 24 years. Additionally, each year the Association develops and publishes topic-specific position statements; recent examples include diabetes and driving and transitions of care for youth with diabetes. Evidence from basic, clinical, epidemiological, cost-effectiveness, and translational research underpins these clinical practice recommendations. Recommendations are rated with an evidence-based grading system that describes the strength of the evidence underlying each recommendation (29).
To provide high-quality, peer-reviewed scientific information to the diabetes research and medical community, the ADA also publishes four journals, Diabetes, Diabetes Care, Clinical Diabetes, and Diabetes Spectrum, which cover top clinical and basic research advances. Collectively, in 2011 these journals reached more than 40,000 subscribers in print and generated more than 7.2 million online visits. Diabetes and Diabetes Care publish primary research findings and have impact factors of 8.9 and 7.1, respectively, making them the highest ranking journals exclusively publishing diabetes research.
The ADA scientific and medical resources are also disseminated in the community, and patient education materials that the Association develops are distributed through awareness campaigns, community-based programs, and a national call center. The Association has a long history of community-based programs in populations who have the greatest need for sustained support and education. These programs specifically target high-risk ethnic minority communities, nonminority individuals at risk for diabetes, new patients with type 2 diabetes, and youth with type 1 diabetes. Associated resources include community-based education, support groups, health fairs, youth camps, school advocacy, and health communication materials. Research underpins each of these services and informational resources. For example, the recently revised Diabetes Risk Test, a simple but accurate screening tool designed to improve awareness of prediabetes or diabetes risk, is a validated self-assessment tool based on academic researchers’ analyses of data from the National Health and Nutrition Examination Survey, the premier ongoing study of the nation’s health (30).
The evidence supporting the Association’s clinical practice recommendations and community programs also serves as the foundation of advocacy regarding discrimination, health legislation, and policies. The ADA advocacy efforts are instrumental in preventing discrimination and assuring health care coverage for those with diabetes. Importantly, the ADA is also a key advocate for increased federal diabetes research support. The ADA’s grasp of the impact of diabetes and its commitment to the vital role of research emboldens its appeals for federal research support (through NIH, Centers for Disease Control and Prevention, and other federal agencies) to address and reduce the public health burden of the disease.
In summary, our vision—a life free of diabetes and all its burdens—may be achieved through continued dedication to support for diabetes research and active involvement and collaboration in the community. The ADA is making progress in realizing this vision through innovative research, advocacy for additional research funding, and the dissemination of key research findings, all of which lead to rapid and meaningful clinical translation. While the diabetes epidemic continues to progress, the ADA recognizes the crucial role that research plays in slowing its momentum.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
V.A.F., M.S.K., T.D., and R.E.R. contributed to the concept, writing, and review of the manuscript.
The authors would like to acknowledge Megan Rowan, MPH, American Diabetes Association, and Matt Petersen, American Diabetes Association, for their insightful comments and editorial assistance in developing the manuscript. The authors also would like to thank Alvin Powers, MD, and Elizabeth Seaquist, MD, the current and immediate past chairs of the Research Policy Committee, for their vision and leadership of the ADA research activities, and all of the past and present members of the Research Policy Committee and Research Grant Review Committee for their invaluable contributions to the research program over the years.
References
- 1.Centers for Disease Control and Prevention National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 2.Bell RA, Mayer-Davis EJ, Beyer JW, et al. ; SEARCH for Diabetes in Youth Study Group Diabetes in non-Hispanic white youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S102–S111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geiss LS, Pan L, Cadwell B, Gregg EW, Benjamin SM, Engelgau MM. Changes in incidence of diabetes in U.S. adults, 1997-2003. Am J Prev Med 2006;30:371–377 [DOI] [PubMed] [Google Scholar]
- 4.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr 2010;8:29–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Aff (Millwood) 2010;29:297–303 [DOI] [PubMed] [Google Scholar]
- 6.Geiss L, Engelgau M, Pogach L, et al. A national progress report on diabetes: successes and challenges. Diabetes Technol Ther 2005;7:198–203 [DOI] [PubMed] [Google Scholar]
- 7.Vastag B. Increasing R01 competition concerns researchers. J Natl Cancer Inst 2006;98:1436–1438 [DOI] [PubMed] [Google Scholar]
- 8.Our commitment to supporting the next generation [article online], 2012. Available from http://nexus.od.nih.gov/all/2012/02/03/our-commitment-to-supporting-the-next-generation/. Accessed 6 April 2012
- 9.Falagas ME, Ierodiakonou V, Alexiou VG. At what age do biomedical scientists do their best work? FASEB J 2008;22:4067–4070 [DOI] [PubMed] [Google Scholar]
- 10.Matthews KR, Calhoun KM, Lo N, Ho V. The aging of biomedical research in the United States. PLoS One 2011;6:e29738. [DOI] [PMC free article] [PubMed]
- 11.Zhao Y, Jiang Z, Zhao T, et al. Reversal of type 1 diabetes via islet β cell regeneration following immune modulation by cord blood-derived multipotent stem cells. BMC Med 2012;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knowler WC, Barrett-Connor E, Fowler SE, et al. ; Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herman WH, Edelstein SL, Ratner RE, et al. ; The Diabetes Prevention Program Research Group The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes Care 2012;35:723–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roep BO, Atkinson M, von Herrath M. Satisfaction (not) guaranteed: re-evaluating the use of animal models of type 1 diabetes. Nat Rev Immunol 2004;4:989–997 [DOI] [PubMed] [Google Scholar]
- 15.Duckworth W, Abraira C, Moritz T, et al. ; VADT Investigators Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–139 [DOI] [PubMed] [Google Scholar]
- 16.Patel A, MacMahon S, Chalmers J, et al. ; ADVANCE Collaborative Group Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 17.Gerstein HC, Miller ME, Byington RP, et al. ; Action to Control Cardiovascular Risk in Diabetes Study Group Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DePalma MT, Rollison J, Camporese M. Psychosocial predictors of diabetes management. Am J Health Behav 2011;35:209–218 [DOI] [PubMed] [Google Scholar]
- 19.Nozaki T, Morita C, Matsubayashi S, et al. Relation between psychosocial variables and the glycemic control of patients with type 2 diabetes: a cross-sectional and prospective study. Biopsychosoc Med 2009;3:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chisholm V, Atkinson L, Donaldson C, Noyes K, Payne A, Kelnar C. Predictors of treatment adherence in young children with type 1 diabetes. J Adv Nurs 2007;57:482–493 [DOI] [PubMed] [Google Scholar]
- 21.Akimoto M, Fukunishi I, Kanno K, et al. Psychosocial predictors of relapse among diabetes patients: a 2-year follow-up after inpatient diabetes education. Psychosomatics 2004;45:343–349 [DOI] [PubMed] [Google Scholar]
- 22.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community. The DEPLOY Pilot Study. Am J Prev Med 2008;35:357–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pullen-Smith B, Carter-Edwards L, Leathers KH. Community health ambassadors: a model for engaging community leaders to promote better health in North Carolina. J Public Health Manag Pract 2008;14(Suppl.):S73–S81 [DOI] [PubMed] [Google Scholar]
- 24.Hemkens LG, Grouven U, Bender R, et al. Risk of malignancies in patients with diabetes treated with human insulin or insulin analogues: a cohort study. Diabetologia 2009;52:1732–1744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jonasson JM, Ljung R, Talbäck M, Haglund B, Gudbjörnsdòttir S, Steineck G. Insulin glargine use and short-term incidence of malignancies—a population-based follow-up study in Sweden. Diabetologia 2009;52:1745–1754 [DOI] [PubMed] [Google Scholar]
- 26.Colhoun HM; SDRN Epidemiology Group Use of insulin glargine and cancer incidence in Scotland: a study from the Scottish Diabetes Research Network Epidemiology Group. Diabetologia 2009;52:1755–1765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Currie CJ, Poole CD, Gale EA. The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia 2009;52:1766–1777 [DOI] [PubMed] [Google Scholar]
- 28.Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and cancer: a consensus report. Diabetes Care 2010;33:1674–1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Diabetes Association Standards of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl. 1):S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bang H, Edwards AM, Bomback AS, et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med 2009;151:775–783 [DOI] [PMC free article] [PubMed] [Google Scholar]