Abstract
OBJECTIVE
To determine whether all-cause and cardiovascular disease (CVD) death rates declined between 1997 and 2006, a period of continued advances in treatment approaches and risk factor control, among U.S. adults with and without diabetes.
RESEARCH DESIGN AND METHODS
We compared 3-year death rates of four consecutive nationally representative samples (1997–1998, 1999–2000, 2001–2002, and 2003–2004) of U.S. adults aged 18 years and older using data from the National Health Interview Surveys linked to National Death Index.
RESULTS
Among diabetic adults, the CVD death rate declined by 40% (95% CI 23–54) and all-cause mortality declined by 23% (10–35) between the earliest and latest samples. There was no difference in the rates of decline in mortality between diabetic men and women. The excess CVD mortality rate associated with diabetes (i.e., compared with nondiabetic adults) decreased by 60% (from 5.8 to 2.3 CVD deaths per 1,000) while the excess all-cause mortality rate declined by 44% (from 10.8 to 6.1 deaths per 1,000).
CONCLUSIONS
Death rates among both U.S. men and women with diabetes declined substantially between 1997 and 2006, reducing the absolute difference between adults with and without diabetes. These encouraging findings, however, suggest that diabetes prevalence is likely to rise in the future if diabetes incidence is not curtailed.
Diabetes has been associated with an average 10 years of life lost for individuals diagnosed during middle age (1). Fortunately, numerous evidence-based interventions exist, ranging from glycemic and cardiovascular disease (CVD) risk factor control to early screening for diabetes complications (2). These have been paralleled by population-wide improvements in glycemic control, CVD risk factors, and rates of several diabetes complications (3–5). Despite these improvements, it remains unclear whether longevity has increased uniformly among diabetic populations. Studies in specific diabetic cohorts in Framingham, Minnesota, and North Dakota suggest mortality declined during the 1990s (6–8). Analyses of consecutive cohorts of the U.S. population from the 1970s through the 1990s, however, found that all-cause and CVD death rates declined among diabetic men but not diabetic women (9,10). However, no national studies have examined mortality trends among the U.S. diabetic population since the 1990s, and the intervening years have been a period of continued advances in treatment approaches and risk factor levels. Newly available mortality follow-up data linked to the National Health Interview Survey (NHIS) provide a unique opportunity to determine whether CVD and all-cause mortality has improved among the U.S. population during recent decades as well as whether the excess mortality associated with diabetes has declined (11,12).
RESEARCH DESIGN AND METHODS
The NHIS is an ongoing survey of the health status, health care access, and behaviors of the U.S. civilian noninstitutionalized population conducted by the National Center for Health Statistics (NCHS) (11). The NHIS uses multistage probability sampling to select approximately 41,000 households and 107,000 individuals each year. The annual response rate of NHIS between 1997 and 2004 ranged from 87 to 92%. Here, we used data from 242,383 (approximately 30,000 per year) adults aged 18 years and older (one randomly selected from each family to receive additional NHIS questions) from the survey years 1997–2004 whose data were linked to the National Death Index, a computer database of all deaths in the U.S. compiled by the NCHS (12). Approximately 89% of all participants’ data (range of 86–93% across survey years) were considered adequate for accurate linkage (12). All NHIS surveys undergo human subjects oversight and participants give informed consent. More detailed descriptions of the NHIS design have been published elsewhere (11).
Measurements
Interviewers assessed diabetes status by asking participants if a doctor or other health professional had ever told them that they had diabetes or sugar diabetes and the number of years since diagnosis. In addition, respondents were queried for age, race/ethnicity, sex, education, family income, history of CVD, and self-reported height and weight, which were used to compute BMI (kg/m2). Income was used to compute the poverty index ratio, an index of income assessed in relation to need, with a score of 1 representing the official federal poverty threshold, a score of <1 indicating a relative level of poverty, and a score of >1 representing income as a multiple of the poverty level. Mortality, including causes of death, was determined from the National Death Index, which was linked with the NHIS (12). The participants’ vital status was available from the time of the survey 1997–2004 through 31 December 2006 (up to 10 years). Underlying causes of death were classified according to the codes of the International Classification of Diseases, Ninth Revision including those coded 390 to 448 classified as CVD deaths (ICD-10 codes 100–178).
Statistical analyses
Our primary objective examined whether death rates in later samples of persons with diabetes were different from those of earlier samples. Secondary objectives examined whether changes in mortality over time differed between the diabetic and nondiabetic cohorts and between various age, sex, race, and socioeconomic subgroups of the diabetic population.
We grouped the survey participants into four consecutive 2-year samples (1997–1998, 1999–2000, 2001–2002, and 2003–2004) and calculated death rates (deaths per person-years) for a maximum of 3 years of follow-up. Participants’ data were censored at the time (quarter year) of death or after 3 years if still alive. Death rates were age-standardized to the projected year 2000 U.S. population. We used χ2 tests and ANOVA to determine whether demographic and health characteristics of the population changed across surveys. We examined the normality distribution of residuals to confirm the appropriateness of ANOVA. We compared survival distributions between the samples according to diabetes status and key covariates using life table analysis and log rank tests. We then used Cox proportional hazards analysis to compare death rates between earlier and later samples among the diabetic population, nondiabetic population, and among various subgroups of the diabetic population. We also compared death rates between individuals with and without diabetes. To examine the potential bias that would exist if later cohorts are diagnosed earlier in the natural history of diabetes, we excluded those with less than 2 years of diabetes duration from the most recent sample. Survey weights were applied to make study estimates representative of the U.S. civilian noninstitutionalized adult population with diabetes. In addition, survey weights were adjusted to account for potential nonresponse bias associated with age, sex, or race/ethnicity. Results were considered significant if P < 0.05, and analyses were conducted with SUDAAN version 10.0.1 to account for the complex NHIS design (13).
RESULTS
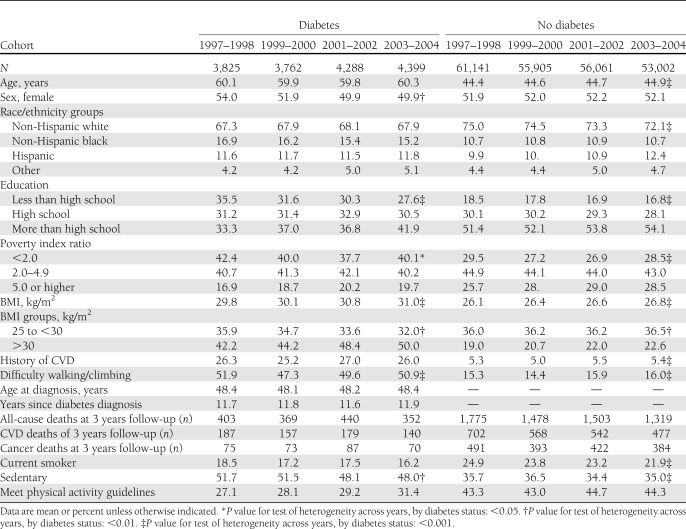
Table 1 describes the characteristics of the U.S. population according to diabetes status across the four consecutive 2-year NHIS samples. Among the population with diabetes, there are consistent increases over time in the levels of education, income, and obesity and a decrease in the proportion of smokers, sedentary behavior, and difficulty walking. There were no significant changes in age, race/ethnicity, history of CVD, or diabetes duration. Demographic trends over time were similar for the nondiabetic population, except that there was also a slight increase in age and the number of Hispanics.
Table 1.
Characteristics of the U.S. adults with and without diabetes according to 2-year study cohorts, 1997–2004
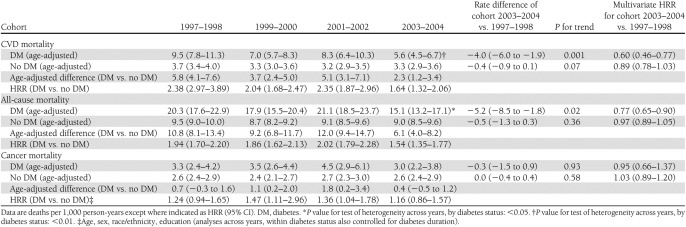
Among the population with diagnosed diabetes, 3-year CVD death rates declined by 4.0 deaths per 1,000 person-years from the 1997–1998 sample (9.5 per 1,000 person-years) to the 2003–2004 sample (5.6 per 1,000 person-years) (P for trend < 0.01) (Table 2). In multivariate analyses adjusting for age, sex, race/ethnicity, and diabetes duration, diabetic adults in the most recent sample (2003–2004) had 40% lower CVD (hazard rate ratio [HRR], 0.60 [95% CI 0.46–0.77]) mortality and 23% lower all-cause mortality (0.77 [0.65–0.90]) than people in the earliest sample (1997–1998) (P < 0.05 for each). There were no significant changes in the rates of cancer mortality among persons either with or without diabetes. In sensitivity analyses excluding those with less than 2 years of diabetes duration from the most recent sample, there was essentially no difference in the rate ratios associated with later cohorts.
Table 2.
All-cause and CVD mortality rates (deaths per 1,000 person-years) according to cohort and diabetes status
CVD death rates declined among the nondiabetic population as well, but the magnitude of decline was weaker (from 3.7 to 3.3 deaths per 1,000; HRR 0.89 [95% CI 0.78 to 1.03], P for trend = 0.07) than that observed for diabetic adults and there was not a significant decline in all-cause mortality (P = 0.36). As a result, the excess CVD death rate associated with diabetes (i.e., compared with those without diabetes) declined from 5.8 to 2.3 deaths per 1,000, and the all-cause death rate difference between people with and without diabetes declined from 10.8 to 6.1 deaths per 1,000.
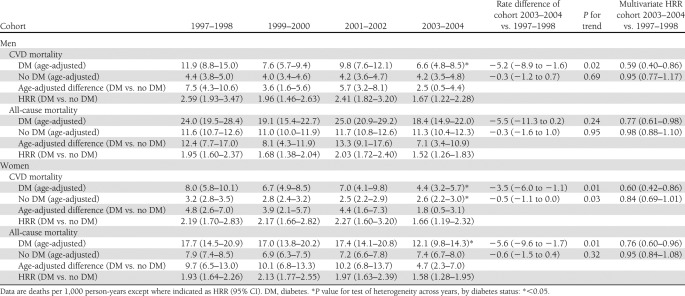
All-cause and CVD death rates in the diabetic population declined among both men and women (Table 3). However, there was a slightly greater magnitude of decline among men (5.2 deaths per 1,000 decline for men vs. 3.5 per 1,000 for women; P = 0.02 for interaction term) . These trends for both men and women again paralleled less dramatic reductions in the nondiabetic population, resulting in reductions in the excess CVD mortality from 7.5 to 2.5 deaths per 1,000 for diabetic men and from an excess 4.8 to 1.8 deaths per 1,000 women.
Table 3.
All-cause and CVD mortality rates according to cohort and diabetes status and sex
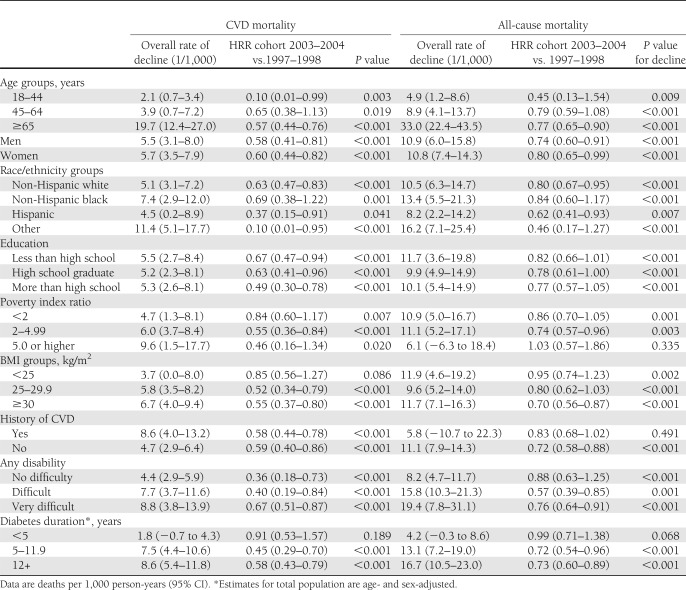
Stratified analyses indicated that reductions in all-cause and CVD mortality were observed relatively uniformly across the population (Table 4). HRRs of decline were similar across groups, but absolute rates of decline tended to be greater in that subgroup with high initial rates, such as older adults and people with long-duration diabetes. Of note, however, was the high relative reduction in CVD and all-cause mortality among young adults with diabetes (age 18–44 years).
Table 4.
Rates of decline (deaths per 1,000 person-years) and multivariate HRRs for all-cause mortality associated with cohort status among specific subgroups of the diabetic population
CONCLUSIONS
This analysis of nationally representative samples of adults with and without diabetes reveals impressive reductions in CVD and all-cause mortality between 1997 and 2006. The rates of improvement among those with diabetes have exceeded those of the nondiabetic population, resulting in more than a 50% reduction of the excess death rates that have been repeatedly attributed to diabetes. Although excess mortality risk remains high—about 2 deaths per 1,000 due to CVD and about 6 all-cause deaths—this excess risk is now considerably lower than previous reports and consistent with improvements in several risk factors, complications, and indicators of medical care and representative of gradual, ongoing improvement in health for people with diagnosed diabetes (3–5,14).
Improvements were observed approximately equally in women and men, which contrasts with earlier analyses. Previous studies in the U.S. and Finland have suggested that the declines in mortality were stronger among men than women (9,10,15). Although no explanation for that finding was confirmed, differences in risk factor management and pathophysiology between diabetic men and women were both cited as possible factors (16). The present analyses suggest, however, that previous sex-related differences in trends may have dissipated over time. The rate of decline in death was as great among women as men, and this finding was maintained after adjusting for differences in demographic factors, comorbidity, and time since diagnosis of disease.
Our findings of improved life expectancy support recent regional studies in the U.S., including North Dakota, Framingham, and Minnesota, as well as population-based studies in Ontario, Denmark, Scotland, Norway, and Finland (6–8,17,18). These trends parallel other improvements in levels of risk factors and rates of complications among the overall U.S. diabetic population (3,5,19,20). In addition, steady improvements in quality and organization of care, self-management behaviors, and medical treatments, including pharmacological treatment of hyperlipidemia and hypertension, could each have contributed to reductions in death rates (21). Incidence of lower extremity amputation, end-stage renal disease, and CVD hospitalization have each declined steadily (22). Reductions in mortality are likely to be influenced by multiple factors, however, and thus may lag behind declines in specific risk factors. The possibility of such lags in secular trends is a reminder that, since improvements in smoking prevalence and blood pressure levels may have slowed during the past decade (23), a flattening of death rates in the near future is still conceivable and should be evaluated.
Although the NHIS provides the largest nationally representative cohort data with diagnosed diabetes, our findings are limited by reliance on self-report to define diabetes; at least 20% of cases with diabetes are undiagnosed (13). Because the fraction of diabetes cases that remain undiagnosed may be decreasing, later cohorts of diabetes could be enriched with people who had their diabetes detected earlier, possibly contributing to lower mortality. In addition, individuals with diabetes who were unaware of their condition would have been misclassified into the nondiabetic group. Because this group is likely to have an increased death rate relative to people without diabetes, the excess mortality risk associated with diabetes is likely to be an underestimate. To examine this, we conducted sensitivity analyses in which we excluded those with less than 2 years of diabetes duration from the most recent sample. This had little difference in our findings, indicating that the reductions in death rates across the samples appears not to be explained by earlier diagnosis. There was also little difference in the prevalence of clinically significant CVD or functional impairment (i.e., difficulty walking) across samples. Nevertheless, to rule out a bias due to earlier detection in later samples, studies will need to compare death rates from cohorts that include individuals with undiagnosed diabetes, for which few studies exist. However, our analyses have the advantage of having a larger cohort of people with diabetes (about 2,000 cases per year), along with a national probability sampling methodology, making it the most representative contemporary examination of death rates among the U.S. diabetic population.
Although our analyses indicate encouraging reduction in mortality and, indirectly, continued success in diabetes care, these findings have ironic implications for the future U.S. diabetes burden. Death rates, along with earlier detection of undiagnosed diabetes and incidence of new diabetes cases, are the principal determinants of future diabetes prevalence and the disease and economic burden that follows. Recently published models indicate thatdeclining mortality among people with diabetes can lead to a substantial increase in prevalence (24,25). Studies from national registries in Denmark, Sweden, and provincial registries in Canada portray a similar picture, wherein the death rate has declined sufficiently so that prevalence is likely to continue to increase even if incidence trends flatten (18,26). Thus, the excess mortality associated with diabetes, though declining, will be spread among a considerably greater proportion of the population. Ultimately, this means that the need for vigilant efforts to prevent vascular and neuropathic complication and early mortality associated with diabetes along with efforts to reduce diabetes incidence will continue to be major demands into the future.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
E.W.G. conceptualized the study, designed the analysis, and wrote the manuscript. Y.J.C. conducted the analysis. S.S. contributed to and reviewed the analysis and reviewed the manuscript. C.C. and L.G. contributed to data acquisition and reviewed and edited the manuscript. S.G. reviewed and edited the manuscript. L.B. contributed to statistical analysis and reviewed and edited the manuscript. E.W.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
A slide set summarizing this article is available online.
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the Centers for Disease Control and Prevention.
See accompanying commentary, p. 1204.
References
- 1.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA 2003;290:1884–1890 [DOI] [PubMed] [Google Scholar]
- 2.Li R, Zhang P, Barker LE, Chowdhury FM, Zhang X. Cost-effectiveness of interventions to prevent and control diabetes mellitus: a systematic review. Diabetes Care 2010;33:1872–1894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999–2008. Diabetes Care 2011;34:1337–1343 [DOI] [PMC free article] [PubMed]
- 4.Preis SR, Pencina MJ, Hwang SJ, et al. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham Heart Study. Circulation 2009;120:212–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gregg EW, Albright AL. The public health response to diabetes—two steps forward, one step back. JAMA 2009;301:1596–1598 [DOI] [PubMed] [Google Scholar]
- 6.Thomas RJ, Palumbo PJ, Melton LJ, 3rd, et al. Trends in the mortality burden associated with diabetes mellitus: a population-based study in Rochester, Minn, 1970–1994. Arch Intern Med 2003;163:445–451 [DOI] [PubMed] [Google Scholar]
- 7.Tierney EF, Cadwell BL, Engelgau MM, et al. Declining mortality rate among people with diabetes in North Dakota, 1997–2002. Diabetes Care 2004;27:2723–2725 [DOI] [PubMed] [Google Scholar]
- 8.Preis SR, Hwang SJ, Coady S, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation 2009;119:1728–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gregg EW, Gu Q, Cheng YJ, Narayan KM, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med 2007;147:149–155 [DOI] [PubMed] [Google Scholar]
- 10.Gu K, Cowie CC, Harris MI. Diabetes and decline in heart disease mortality in US adults. JAMA 1999;281:1291–1297 [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Design and estimation for the National Health Interview Survey, 1995–2004. Vital Health Stat 2 2000;130:1–31 [PubMed] [Google Scholar]
- 12.The National Health Interview Survey (1986–2004) Linked Mortality Files, mortality follow-up through 2006: Matching Methodology, May 2009 [article online], 2009. Hyattsville, MD, National Center for Health Statistics. Office of Analysis and Epidemiology. Available from http://www.cdc.gov/nchs/data/datalinkage/matching_methodology_nhis_final.pdf Accessed 8 February 2012
- 13.SUDDAN 10. RTI International, Research Triangle Park, NC. Available from http://www.rti.org/sudaan Accessed 8 February 2012
- 14.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med 2007;356:2388–2398 [DOI] [PubMed] [Google Scholar]
- 15.Barengo NC, Katoh S, Moltchanov V, Tajima N, Tuomilehto J. The diabetes-cardiovascular risk paradox: results from a Finnish population-based prospective study. Eur Heart J 2008;29:1889–1895 [DOI] [PubMed] [Google Scholar]
- 16.Rivellese AA, Riccardi G, Vaccaro O. Cardiovascular risk in women with diabetes. Nutr Metab Cardiovasc Dis 2010;20:474–480 [DOI] [PubMed] [Google Scholar]
- 17.Hoehner CM, Williams DE, Sievers ML, Knowler WC, Bennett PH, Nelson RG. Trends in heart disease death rates in diabetic and nondiabetic Pima Indians. J Diabetes Complications 2006;20:8–13 [DOI] [PubMed] [Google Scholar]
- 18.Lipscombe LL, Hux JE. Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995–2005: a population-based study. Lancet 2007;369:750–756 [DOI] [PubMed] [Google Scholar]
- 19.Burrows NR, Li Y, Geiss LS. Incidence of treatment for end-stage renal disease among individuals with diabetes in the U.S. continues to decline. Diabetes Care 2010;33:73–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geiss L, Engelgau M, Pogach L, et al. A national progress report on diabetes: successes and challenges. Diabetes Technol Ther 2005;7:198–203 [DOI] [PubMed] [Google Scholar]
- 21.Saaddine JB, Cadwell B, Gregg EW, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Ann Intern Med 2006;144:465–474 [DOI] [PubMed] [Google Scholar]
- 22.National Diabetes Surveillance System. [article online], 2008. Atlanta, GA, Centers for Disease Control and Prevention. Available from http://www.cdc.gov/diabetes/statistics/index.htm Accessed 11 March 2009
- 23.Wang J, James C, Gregg EW, Geiss L. Long-term and recent progress in blood pressure levels among U.S. adults with diagnosed diabetes, 1988–2008. Diabetes Care 2011;34:1579–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and high risk for diabetes using A1c criteria in the U.S. population in 1988–2006. Diabetes Care 2010;33:562–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr 2010;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K, Steering Group of the National Diabetes Register The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia 2008;51:2187–2196 [DOI] [PubMed] [Google Scholar]