Abstract
Background
There is accumulating epidemiologic evidence that exposure to traffic-related air pollutants, including particulate matter (PM) and polyaromatic hydro carbons (PAHs), plays a role in etiology and prognosis of a large scale of illnesses, although the role of specific causal agents and underlying mechanisms for different health outcomes remains unknown.
Objective
Our general objective was to assess the relations between personal exposure to traffic exhausts, in particular ambient PM2.5 and PAHs, and the occurrence of DNA strand breaks by applying personal monitoring of PM and biomarkers of exposure (urinary 1-hydroxypyrene-glucuronide, 1-OHPG) and effect (urinary 8-hydroxydeoxyguanosine, 8-OHdG and DNA strand breaks).
Methods
We recruited 91 traffic conductors and 53 indoor office workers between May 2009 and June 2011 in Taipei City, Taiwan. We used PM2.5 personal samplers to collect breathing-zone particulate PAHs samples. Spot urine and blood samples after work shift of 2 consecutive days were analyzed for 1-OHPG, 8-OHdG and DNA strand breaks, respectively. Statistical methods included linear regression and mixed models.
Results
Urinary 8-OHdG levels and the occurrence of DNA strand breaks in traffic conductors significantly exceeded those in indoor office workers in mixed models. Particulate PAHs levels showed a positive association with urinary 1-OHPG in the regression model (β = 0.056, p = 0.01). Urinary 1-OHPG levels were significantly associated with urinary 8-OHdG levels in the mixed model (β = 0.101, p = 0.023). Our results provide evidence that exposure to fine particulates causes DNA damage. Further, particulate PAHs could be biologically active constituents of PM2.5 with reference to the induction of oxidative DNA damages.
Introduction
Traffic emissions include large quantities of carbon dioxide (CO2), carbon monoxide (CO), hydrocarbons (HC), nitrogen oxides (NOx), particulate matter (PM), and mobile source air toxics (MSATs), such as benzene, formaldehyde, acetaldehyde, 1,3-butadiene, and lead (where leaded gasoline is still in use). In addition, secondary by-products, such as ozone and secondary aerosols, such as nitrates and inorganic and organic acids, contribute to traffic-related air pollution [1]. There is accumulating epidemiologic evidence that exposure to traffic-related air pollutants plays a role in etiology and prognosis of a large scale of illnesses, including asthma, impaired lung function, allergy, adverse birth outcomes, cardiovascular disease and cancer, although the role of specific causal agents and underlying mechanisms for different health outcomes remains unknown [1].
Traffic is an increasingly important source of PM, especially fine PM with an aerodynamic diameter  2.5 µm (PM2.5). Fine particles (PM2.5) can penetrate easily into respiratory tract and reach circulatory system, and be more toxic than coarse particles [2]. There is extensive epidemiologic evidence of the associations between both short- and long-term exposure to PM2.5 and the risk of respiratory and cardiovascular diseases, and adverse pregnancy outcomes.
2.5 µm (PM2.5). Fine particles (PM2.5) can penetrate easily into respiratory tract and reach circulatory system, and be more toxic than coarse particles [2]. There is extensive epidemiologic evidence of the associations between both short- and long-term exposure to PM2.5 and the risk of respiratory and cardiovascular diseases, and adverse pregnancy outcomes.
Traffic is also the most important source of polycyclic aromatic hydrocarbons (PAHs) in urban ambient air [3], [4]. PAHs are ubiquitous constituents of urban airborne particles and are of major health concern mainly due to their well-known carcinogenic and mutagenic properties.
Biomarkers of exposure and outcome could be useful both in the quantification of the relations of interests as well as in providing insight into the specific causal agents and underlying biological mechanism.
Metabolites of pyrene in human urine can be measured as 1-hydroxypyrene (1-OHP) after deconjugation of the glucuronide with beta-glucuronidase or directly as 1- hydroxypyrene-glucuronide (1-OHPG) without deconjugation. Since 1-OHPG is approximately 5-fold more fluorescent than 1-OHP, it may provide a more sensitive biomarker for assessing exposure to pyrene in mixtures of PAHs [5], [6]. Furthermore, the relation between total PAHs and pyrene was highly correlated in the urban environment [7]. Thus, Urinary 1-OHPG has been used as a biomarker of exposure to PAHs [6], [8], [9].
Urinary 8-OHdG levels and DNA strand breaks could serve as biomarkers of early effects of exposure to PM, because there is evidence that exposure to ambient particulate matter (PM) induces oxidative stress, genotoxicity, and carcinogenicity [10]. Previous studies suggest that PM interacts with biological systems through direct generation of reactive oxygen species (ROS) from the surface of particles, organic chemicals, transition metals or other agitated processes in bodies and further contributes to the oxidative stress process [10], [11]. Besides, oxidative stress is defined as an imbalance between free radical production and antioxidant capacity resulting in excess oxidative products [12]. The spectrum of DNA-related oxidative products includes strand breaks, AP (apurinic/apyrimidinic) sites, and oxidized bases. With the latter group, attention has been focused on 8-OHdG, a major product with a clear mutagenic potential, which has been commonly used as a biomarker of oxidative stress in studies on ambient air pollution [9], [13]–[16]. On the other hand, DNA strand breaks can be measured by the comet assay and represent an early and critical step in chemical carcinogenesis [17].
Most previous epidemiological studies have based exposure assessment on data collected at stationary monitoring stations, which may introduce both random and systematic error in exposure assessment of individuals [18]. Furthermore, only a few studies that have collected personal PM mass or its components as measures of exposure have explored the related DNA damage effects [14]–[16].
Our general objective was to assess the relations between personal exposure to traffic exhausts, in particular ambient PM2.5 and PAHs, and the occurrence of DNA strand breaks. We assessed the personal exposure to ambient air PM2.5 concentration and the amount of PAHs bound to PM2.5, urinary 1-OHPG levels as a biomarker of exposure to PAHs, and urinary 8-OHdG concentration and the occurrence of DNA strand breaks as biomarker of effect. In order to best elaborate the relations of interest in existing environmental conditions, we selected our study population from the Taipei City traffic conductors who represent probably the most highly exposed population in Taiwan.
Methods
Study Population
We recruited 91 traffic conductors as the exposed group and 53 indoor office workers as the reference group aged 20 to 63 years between April 2009 and June 2011 in Taipei City, Taiwan. All subjects were free of cancer and pulmonary disease and all of them had been working in their current job position for at least 3 months.
Ethics Statement
This study was approved by the Institutional Review Board of the National Health Research Institutes in Taiwan, and written informed consent from participants was obtained prior to study enrollment.
Data Collection
The participants underwent health examinations and completed a self-administered questionnaire about demographic information, lifestyle habits, as well as history of previous and current diseases. Personal monitors were used to assess the PM2.5 concentration in the breathing zone for all particulates during the daily work shift. Post-shift urine and blood samples were collected from participants on 2 consecutive days.
Air Sampling
The subjects were monitored for 9–10 hours per day equal to their working hours. Personal breathing-zone air samples were collected from the study subjects by battery-operated personal air-sampling pumps. The personal exposure monitors with a 2.5 µm impactor (The Personal Environmental Monitor, PEM; SKC Inc., Catalog No. 761–230, PA, USA) cut size was used in line with a Gilian GilAir 5 pump (Sensidyne Inc., Clearwater, FL) calibrated at a flow rate of 2 L/min. Particle samples were collected on Teflon filter (Biotech Line, Lynge, Denmark). Before and after sampling, the filters were weighed on a Micro Balance MT5 from Mettler-Toledo (Glostrup, Denmark) after conditioning for 24 h in a temperature- and relative humidity-controlled room. The mass collected in the filter was divided by the air volume sampled to calculate the gravimetric PM2.5 concentration.
Quantification of PAHs in PM
The PAH analyses of air samples were conducted using methods of Tsai et al. [19]. Total particulate PAHs levels were determined as the sum of following 22 individual species: naphthalene, acenaphthylene, acenaphthene, fluorene, phenanthrene, anthracene, fluoranthene, pyrene, cyclopenta[c,d]pyrene, benz[a]anthracene, chrysene, benzo[b]fluoranthene, benzo[k]fluoranthene, benzo[e]pyrene, benzo[a]pyrene, perylene, indeno[1,2,3-cd] pyrene, dibenz[a,h]anthracene, benzo[b]chrysene, benzo[ghi]perylene, coronene, and dibenzo[a,e]pyrene. Recovery efficiencies determined by spiking known amounts of PAHs through the GC-MS analytic process ranged from 80% to 110%. The limit of detection of the 22 PAH compound fell to the range 19–386 pg/m3. Analyses of field blanks found no significant contamination (i.e., GC/MS integrated area < detection limit).
Analysis of Urine Samples for 1-OHPG and 8-OHdG
The urine samples were collected within half an hour after the end of a work-shift. We divided the urine samples into several small volume aliquot and stored at −80°C freezer until analysis.
Urinary 1-OHPG was measured using the assay developed by Strickland et al. [5]. The recovery of the assay was 91%. The coefficient of variation of the assay was less than 5% during the period of sample analysis. The limit of detection was 0.05 ng/ml. Urinary 8-OHdG concentrations were measured using a liquid chromatography/MS/MS as described elsewhere [20]. A detection limit of 5.7 ng/L was obtained using seven repeated analyses of deionized water. The coefficients of variation in interday and intraday tests were <5%. Mean recovery of 8-OHdG in urine was 99%–102%. Each subject’s urinary 1-OHPG and 8-OHdG concentrations were normalized to urine creatinine.
Single-cell Gel Electrophoresis (Comet assay)
The blood samples were collected in EDTA tubes within half an hour after the end of work-shifts. Blood (2 ml) from each subject was immediately stabilized with 2 ml of a 20∶80 (v/v) mixture of dimethyl sulfoxide (DMSO) and RPMI 1640 cell culture medium [21]. Aliquots of these samples were progressively frozen to −80°C for later analysis.
Comet assay procedure was performed according to manufacturer’s protocol (Trevigen, Gaithersburg, MD). Comet assay kits, reagents and slides were purchased from Trevigen (Gaithersburg, MD). In brief, we mixed 50 µl thawed blood with 500 µl molten LMAgarose (at 37°C), and 50 µl mixture was immediately pipetted onto CometSlide™. Slides were left at 4°C in the dark in refrigerator for 10 min. The slides were immersed in prechilled lysis solution. After 1 h in the dark at 4°C, the slides were immersed in freshly prepared Alkaline Solution (300 mM NaOH, 1mM EDTA, pH>13) for 1 hour and then electrophoresed (300 mA, 30 min). The process of the electrophoresis was performed in a cold room to diminish background damage. Once electrophoresis was completed, the slides were immersed twice in deionized water for 10 min each, then in 70% ethanol for 5 min. Samples were stored at room temperature in the dark with desiccant prior to scoring. We quantified the DNA damage of 100 randomly selected leukocytes (50 cells from each duplicate well) after staining with 20 µl SYBR Green, using Pixera Penguin 150CL Cooled CCD digital camera systems (Pixera, USA) attached to a fluorescent microscope (Olympus, Japan). The percentage of DNA in tail (%T) was used as a measure of DNA damage and computed using the Komet Software version 5.5 (Kinetic Imaging Ltd, Liverpool, UK).
Negative and positive control cells purchased from Trevigen (Trevigen, Gaithersburg, MD) were included in the assay as a quality control. The percentage of DNA in tail for the negative and positive controls were <10% and >30%, respectively. Samples were coded and run along with quality control samples in the same bench.
Statistical Methods
The levels of PM2.5, particulate PAHs, urinary 1-OHPG, urinary 8-OHdG and DNA strand breaks were compared between the exposed and reference groups by Mann-Whitney U test. The distribution of urinary 1-OHPG, urinary 8-OHdG and DNA strand breaks by order of day within the exposed and reference groups were compared using Wilcoxon signed rank test. Multiple linear regression models were used to assess the relations between PM2.5 levels, particulate PAHs and urinary 1-OHPG adjusting for the covariates (such as age, gender, education level, smoking habit, season of data collection and exposure status).
Mixed-model repeated measures analysis (Proc mixed) was used to investigate the relations between urinary 1-OHPG, 8-OHdG and DNA strand breaks after adjusting for fixed covariates. These models treated the subjects as random effect and model selections were based on Akaike’s Information Criterion. The compound symmetry and variance components were constructed as the covariance structures. The dependent variables were transformed by the natural logarithm. Residual and influence analyses were conducted. To calculate the predictive value of an X unit increase in one of the predictors, the following formula was used: [exp(model estimate* X) − 1] * 100. A two-sided p-value <0.05 was considered statistically significant. All statistical analyses were performed using SAS (version 9.1.3; SAS Institute Inc., Carry, NC, USA.).
Results
Study Population
Characteristics of the study population were compared between the exposed and reference groups (table 1). The mean age was 49.2 years (SD 9.17) in the exposed group and 42.9 years (SD 8.86) in the reference group. The exposed group had a lower percentage of women and a lower educational level than the reference group. The most common season for data collection was spring for the exposed group, but spring and winter for the reference group. The distributions of lifestyle factors, such as smoking habit, drinking alcohol and cooking habit, were similar between the exposed and reference groups.
Table 1. Characteristic of subjects in exposed and reference groups.
| Exposed group | Reference group | ||||
| Variables | (N = 91) | (N = 53) | p-valuea | ||
| N | % | N | % | ||
| Age (years) (Mean±SD)b | 49.19± | 9.17 | 42.85± | 8.86 | <0.001 |
| Gender | |||||
| Male | 68 | 74.7 | 12 | 22.6 | |
| Female | 23 | 25.3 | 41 | 77.4 | |
| BMI (Kg/m2) (Mean±SD) b | 25.11± | 3.55 | 29.06± | 6.60 | <0.001 |
| Educational level | <0.001 | ||||
| High school | 57 | 64.0 | 9 | 17.0 | |
| College | 32 | 36.0 | 44 | 83.0 | |
| Current smoker | 0.128 | ||||
| No | 70 | 76.9 | 47 | 88.7 | |
| Yes | 21 | 23.1 | 6 | 11.3 | |
| Drinking alcohol | 1.000 | ||||
| No | 74 | 83.1 | 43 | 82.7 | |
| Yes | 15 | 16.9 | 9 | 17.3 | |
| Vitamin supplement | 0.140 | ||||
| No | 39 | 43.3 | 30 | 57.7 | |
| Yes | 51 | 56.7 | 22 | 42.3 | |
| Cooking habit | 0.122 | ||||
| No | 51 | 59.3 | 22 | 44.0 | |
| Yes | 35 | 40.7 | 28 | 56.0 | |
| Season of data collectionc | 0.027 | ||||
| Spring | 48 | 52.7 | 20 | 37.7 | |
| Summer | 14 | 15.4 | 3 | 5.7 | |
| Fall | 11 | 12.1 | 12 | 22.6 | |
| Winter | 18 | 19.8 | 18 | 34.0 | |
χ2 test.
Student’s t test.
Fisher’s exact test.
Comparison of PM2.5 Level, Particulate PAHs, Urinary 1-OHPG, Urinary 8-OHdG and DNA Strand Breaks between the Exposed and Reference Groups
Table 2 shows that the distributions of PM2.5 exposure and particulate PAHs in the exposed and reference groups. The median levels of PM2.5 and particulate PAHs in the exposed group were higher than those in the reference group. Spearman correlation between PM2.5 and particulate PAHs levels was significantly positive in the traffic conductors (r = 0.42, p<0.01), but not in the indoor office workers (r = −0.08, p = 0.57) (data not shown).
Table 2. Concentrations of PM2.5 and particulate polycyclic aromatic hydrocarbons (PAHs) for the exposed and reference groups.
| Exposed group | Reference group | ||||
| Variables | (N = 91) | (N = 53) | p-valuea | ||
| Median(Q25-Q75) | N | Median(Q25-Q75) | N | ||
| External exposure | |||||
| PM2.5 (µg/m3) | 82.87 (63.11–134.15) | 91 | 70.82 (56.31–99.25) | 50 | 0.054 |
| Particulate PAHs(ng/m3) | 13.07(8.76–20.55) | 91 | 8.24 (6.87–8.76) | 50 | <0.001 |
Mann-Whitney U test.
Table 3 shows the concentrations of urinary 1-OHPG, urinary 8-OHdG and DNA strand breaks in the exposed and reference groups by order of day. There were no significant differences of urinary 1-OHPG, urinary 8-OHdG, and DNA strand breaks between 1st day and 2nd day in the exposed and reference groups. In terms of urinary 1-OHPG, 8-OHdG and DNA strand breaks, the median level in the exposed group was significantly higher than those in the reference group both in the first and second day.
Table 3. Concentrations of urinary 1-OHPG, 8-OHdG and DNA strand breaks in the exposed and reference groups by order of day.
| Exposed group | Reference group | |||||||||||
| Variables | 1st day | 2nd day | p-valuea | 1st day | 2nd day | p-valueb | p-valuec | p-valued | ||||
| Median(Q25-Q75) | N | Median(Q25-Q75) | N | Median(Q25-Q75) | N | Median(Q25-Q75) | N | |||||
| Biomarker of exposure | ||||||||||||
| Urinary 1-OHPG (µg/g creatinine) | 0.36 (0.21–0.58) | 83 | 0.33 (0.17–0.55) | 81 | 0.393 | 0.16 (0.08–0.23) | 47 | 0.18 (0.11–0.31) | 46 | 0.634 | <0.001 | 0.001 |
| Biomarkers of effect | ||||||||||||
| Urinary 8-OHdG (µg/g creatinine) | 3.67 (2.72–5.01) | 87 | 3.44 (2.66–4.30) | 83 | 0.494 | 2.53 (1.58–3.59) | 47 | 2.28 (1.53–3.50) | 46 | 0.133 | <0.001 | <0.001 |
| DNA strand breaks (%) | 14.95 (12.65–18.53) | 89 | 15.37 (12.85–19.63) | 82 | 0.314 | 9.26 (7.64–10.62) | 49 | 9.46 (8.02–11.20) | 47 | 0.536 | <0.001 | <0.001 |
Wilcoxon Signed rank test within exposed group.
Wilcoxon Signed rank test within reference group.
Mann-Whitney U test between exposed and reference group for the first day.
Mann-Whitney U test between exposed and reference group for the second day.
Relations between Environmental Exposure and Biomarker of Exposure
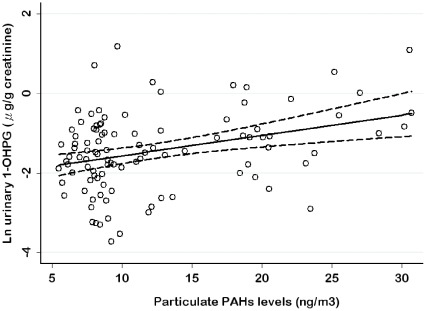
Table 4 presents associations between PM2.5 levels, particulate PAHs and urinary 1-OHPG levels in all workers and nonsmoking workers. In the adjusted model, there was no significant association between PM2.5 levels and urinary 1-OHPG levels in all workers and nonsmoking workers. In contrast, we found a significant positive association between particulate PAHs and urinary 1-OHPG in both groups of workers after adjusting for fixed covariates (p<0.05). That is, for a 10 ng/m3 increment of particulate PAHs level, a 75% increment in urinary 1-OHPG was observed among nonsmoking workers. Figure 1 illustrated a scatter plot of urinary 1-OHPG levels by particulate PAHs levels using regression models in nonsmoking workers after adjusting for other covariates with 95% confidence interval.
Table 4. Relations of PM2.5 exposure and particulate PAHs with urinary 1-OHPG by regression models.
| Ln urinary 1-OHPG(µg/g creatinine) | |||
| Variables | β | 95% CI | p-value |
| Total workers (N = 144) | |||
| Environmental exposurea | |||
| PM2.5 (µg/m3) | −0.0003 | −0.003 to 0.002 | 0.819 |
| Environmental exposurea | |||
| PM2.5 (µg/m3) | −0.0006 | −0.004 to 0.002 | 0.675 |
| Particulate PAHs (ng/m3) | 0.043 | 0.011 to 0.075 | 0.010 |
| Nonsmoking workers (N = 117) | |||
| Environmental exposureb | |||
| PM2.5 (µg/m3) | −0.0007 | −0.004 to 0.002 | 0.626 |
| Environmental exposureb | |||
| PM2.5 (µg/m3) | −0.001 | −0.004 to 0.002 | 0.503 |
| Particulate PAHs (ng/m3) | 0.056 | 0.014 to 0.098 | 0.010 |
Adjusted for age, gender, educational level, smoking habit, season of data collection, and group.
Adjusted for age, gender, educational level, season of data collection, and group.
Figure 1. The scatter plot of urinary 1-OHPG levels vs. particulate PAHs levels in nonsmoking workers.
Relations between Biomarkers of Exposure and Effect
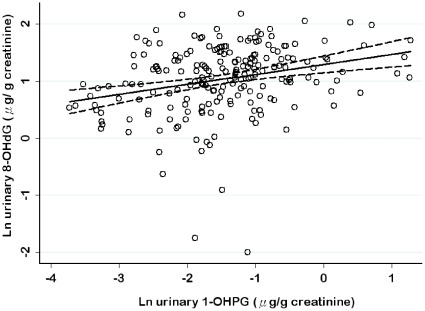
Table 5 presents the results of linear mixed models for determinants of urinary 1-OHPG, urinary 8-OHdG and DNA strand breaks in nonsmoking workers. After adjustments were made for other covariates, we found that an increase in urinary 1-OHPG was significantly related to an increase in urinary 8-OHdG (p<0.05). That is, for a 75% increment of urinary 1-OHPG levels, a 7.6% increment in urinary 8-OHdG levels was observed. The exposure at group level was a significant determinant of urinary 1-OHPG levels, urinary 8-OHdG levels and DNA strand breaks. However, urinary 1-OHPG and 8-OHdG levels were not significant determinants of DNA strand breaks. On the other hand, age was a significant determinant of urinary 8-OHdG levels and DNA strand breaks. Season was a significant determinant of urinary 8-OHdG levels. Females had on average higher levels of urinary 1-OHPG than males in the adjusted models. Figure 2 illustrated a scatter plot of urinary 8-OHdG levels by urinary 1-OHPG levels using mixed models in nonsmoking workers after adjustment for other covariates and presents graphically the lower and upper limits of the 95% confidence interval.
Table 5. Determinants of urinary 1-OHPG, 8-OHdG and DNA strand breaks in nonsmoking workers by mixed models (Noa = 234).
| Ln urinary 1-OHPG (µg/g creatinine) | Ln urinary 8-OHdG (µg/g creatinine) | Ln DNA strand breaks (%) | ||||
| Variables | β (95% CI) | p-value | β (95% CI) | p-value | β (95% CI) | p-value |
| Age (year) | 0.009 (−0.009 to 0.027) | 0.328 | 0.015 (0.003 to0.026) | 0.016 | −0.008 (−0.014 to −0.001) | 0.019 |
| Gender | ||||||
| Female (reference) | ||||||
| Male | −0.369 (−0.712 to −0.026) | 0.035 | −0.111 (−0.337 to 0.116) | 0.334 | 0.035 (−0.083 to 0.153) | 0.557 |
| Educational level | ||||||
| High school (reference) | ||||||
| College | −0.056 (−0.322 to 0.435) | 0.770 | 0.124 (−0.370 to 0.124) | 0.323 | 0.122 (−0.253 to 0.010) | 0.069 |
| Group | ||||||
| Control group (reference) | ||||||
| Exposed group | 0.634 (0.228 to 1.040) | 0.003 | 0.379 (0.108 to 0.649) | 0.007 | 0.621 (0.477 to 0.765) | <0.001 |
| Season | ||||||
| Winter (reference) | ||||||
| Spring | 0.125 (−0.222 to 0.472) | 0.477 | −0.256 (−0.483 to −0.029) | 0.027 | 0.023 (−0.097 to 0.143) | 0.701 |
| Summer | 0.080 (−0.457 to 0.616) | 0.769 | −0.506 (−0.857 to −0.156) | 0.005 | 0.051 (−0.143 to 0.245) | 0.603 |
| Fall | 0.083 (−0.385 to 0.550) | 0.727 | −0.237 (−0.542 to 0.067) | 0.125 | 0.094 (−0.065 to 0.253) | 0.242 |
| Ln 1-OHPG (µg/g creatinine) | 0.101 (0.014 to 0.187) | 0.023 | 0.007 (−0.036 to 0.051) | 0.732 | ||
| Ln 8-OHdG (µg/g creatinine) | −0.019 (−0.088to 0.050) | 0.587 | ||||
Abbreviations: number of observations (No).
Figure 2. The scatter plot of urinary 8-OHdG levels vs. urinary 1-OHPG levels in nonsmoking workers.
Discussion
Our results provide evidence that exposure to particulate PAHs in PM2.5 is a determinant of urinary 1-OHPG levels; urinary 1-OHPG could thus serve as a biomarker of ambient exposure to PAHs. Further, urinary 8-OHdG levels are related to urinary 1-OHPG levels and thus urinary 8-OHdG has potential to serve as a biomarker of effect. An increase of 10 ng/m3 in particulate PAHs was associated with a 75% increase in urinary 1-OHPG levels and a 75% increase in urinary 1-OHPG levels was associated with a 7.6% increase in urinary 8-OHdG levels. The results provide evidence that exposure to ambient air PM increases the occurrence of DNA damage, and exposure to particulate PAHs increases urinary 8-OHdG levels.
We hypothesized that particulate PAHs in PM could be a stronger determinant of urinary 8-OHdG compared with PM mass alone. Recent literature suggests that some chemical components of PM may have stronger effects than others and the differences in effect estimates across cities or seasons may be related to the chemical composition of particles [22], [23]. Particulate PAHs can be converted to PAH-quinones by cytochrome P450, epoxide hydrolase and dihydrodiol dehydrogenase [24], [25]. It has been reported that compounds having a quinone-structure are able to produce ROS in redox cycle [26], [27]. Laboratory-based in vitro or in vivo studies have consistently reported significant associations between 8-OHdG and PAHs. However, an early study found a dose-response relationship between PM2.5 -bound metal and urinary 8-OHdG among boiler markers at boiler making plants [14]. Wei et al. [16] reported that PM2.5 mass, PAHs and metal were significantly associated with an increased levels of urinary 8-OHdG after work-shift. Another panel study reported that the personal PM2.5 exposure was a predictor of 8-OHdG in lymphocytes with an 11% increase in 8-OHdG per 10 µg/m3 increase in PM2.5 concentration [15]. These studies showed that PM2.5 or its components could increase the burden of oxidative stress.
We found no associations between neither urinary 1-OHPG levels nor urinary 8-OHdG levels and DNA strand breaks, which was contrary to our hypothesis but in agreement with a previous study [28]. A recent study also reported that different PAH industries, such as graphite electrode, refractory, and coke oven, could contribute to genotoxic DNA damage and DNA damage was not unequivocally associated to PAH on the individual level most likely due to potential contributions of co-exposures [29]. Moreover, our finding of the exposed group status as an independent predictor of DNA strand breaks is consistent with an idea that traffic conductors could also be exposed to other unmeasured hazards, such as benzene and ozone. Taken together, these observations suggest that while particulate PAHs may have the potential to induce DNA strand breaks, other factors probably play a role in the response of the organism to environmental pollution.
Urinary 8-OHdG levels as not a significant predictor of DNA strand breaks indicated that 8-OHdG levels could play a minor role in the process of DNA strand breaks, and other spectrum of DNA damage could mainly contribute to increase the levels of DNA strand breaks. Actually, DNA damages based on alkaline single-cell gel electrophoresis include not only DNA strand breaks but also base modifications, as the oxidized purine bases (8-OHdG and others) and pyrimidine bases could be converted into additional DNA single strand breaks [17], [30]. Therefore, the origin of direct strand breaks and alkali-label sites that may include modified sugar and base residual is difficult to identify using alkaline comet assay. Apparently, this strongly depends on the DNA modifying agent.
There was a significant association between the ambient concentrations of PM2.5 and particulate PAHs exposure in the traffic conductors while such association was not present in the office workers. These differences between the occupational groups may be related to the outdoor and indoor locations that reflect different working conditions, as well as to differences in the dispersion of toxic substances between the outdoor and indoor workplace. PM2.5 levels and particulate PAHs levels of traffic conductors were lower than those in Taipei toll station workers (range from 87–346 µg/m3 for PM2.5 and 480–6026 ng/m3 for particulate PAHs) [7], [31]. This may be due to lower traffic intensities and different pattern of outdoor working activities between toll-station workers and traffic conductors.
As to the effect of age on urinary 8-OHdG, our study result was consistent with a previous finding of a significantly increasing trend in urinary 8-OHdG concentrations by increasing age [32]. Previously younger workers were reported to have higher levels of DNA strand breaks than older workers due to higher physical-activity loading on job [33], [34]. In the present study, the highest concentrations of urinary 8-OHdG were measured during the winter, which corresponds to higher levels of PAHs exposure in the winter than during other seasons [4]. Gender-related differences in urinary 1-OHPG levels could be explained by gender differences in endogenous metabolism of PAHs [35], [36].
Our study has some limitations. First, both traffic-related sources and other indoor sources contribute to the total exposure to PM and PAHs, and therefore, our exposure assessment was likely to underestimate personal PM2.5 and particulate PAHs exposures from traffic-related sources. Secondly, we did not assess exposure to other air pollutants, such as carbon monoxide, nitrogen dioxide and ozone. If these pollutants are associated with particulate matter, the estimated effects could be confounded. Last, genetic differences in PAH-metabolizing enzymes and DNA repair in the study population could affect the estimated effects. However, repeated measurement design in our study could decrease the influence of genetic background within-subject.
Our results provide new evidence that exposure to fine particulates may cause DNA damage by showing associations between measured ambient PAHs bound to PM2.5 and urinary 1-OHPG biomarkers as a biomarker of exposure and between urinary 1-OHPG and urinary 8-OHdG as a biomarker of DNA damage. In addition, our comparison of traffic conductors and office workers indicates that exposure to traffic exhausts could increase the amount of DNA strand breaks. These findings are consistent with the hypothesis that exposure to traffic exhausts increases carcinogenic and mutagenic processes in humans, which support results from previous epidemiologic studies [18], [37].
In summary, this is the first study to indicate that the elevated levels of particulate PAHs bound to PM2.5 could increase urinary 8-OHdG levels through the elevated levels of urinary 1-OHPG. These results provide an indication that air pollution PM could be associated with DNA damage, and particulate PAHs could be the biologically active constituent of PM with regarding to the induction of oxidative DNA damage.
Acknowledgments
We thank the Institute of Occupational Safety and Health for providing the personal aerosol sampler.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by the National Research Program for Genomic Medicine, Taiwan (grant no.: DOH97-TD-G-111-032, DOH98-TD-G-111-021, DOH99-TD-G-111-018 and NSC100-2325-B400-010). J.J. was supported by a grant from the Academy of Finland (SALVE Research Program). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Health Effects Institute. Health Effects Institute; 2010. Traffic-Related Air Pollution: A Critical Review of the Literature on Emissions, Exposure, and Health Effects. [Google Scholar]
- 2.Valavanidis A, Fiotakis K, Vlachogianni T. Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2008;26:339–362. doi: 10.1080/10590500802494538. [DOI] [PubMed] [Google Scholar]
- 3.Baek SO, Field RA, Goldstone ME, Kirk PW, Lester JN, et al. A review of atmospheric polycyclic aromatic hydrocarbons: Sources, fate and behavior. Water, Air, & Soil Pollution. 1991;60:279–300. [Google Scholar]
- 4.Tuominen J, Salomaa S, Pyysalo H, Skytta E, Tikkanen L, et al. Polynuclear aromatic compounds and genotoxicity in particulate and vapor phases of ambient air: effect of traffic, season, and meteorological conditions. Environ Sci Technol. 1988;22:1228–1234. doi: 10.1021/es00175a017. [DOI] [PubMed] [Google Scholar]
- 5.Strickland PT, Kang D, Bowman ED, Fitzwilliam A, Downing TE, et al. Identification of 1-hydroxypyrene glucuronide as a major pyrene metabolite in human urine by synchronous fluorescence spectroscopy and gas chromatography-mass spectrometry. Carcinogenesis. 1994;15:483–487. doi: 10.1093/carcin/15.3.483. [DOI] [PubMed] [Google Scholar]
- 6.Strickland P, Kang D, Sithisarankul P. Polycyclic aromatic hydrocarbon metabolites in urine as biomarkers of exposure and effect. Environ Health Perspect. 1996;104(Suppl 5):927–932. doi: 10.1289/ehp.96104s5927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsai PJ, Shih TS, Chen HL, Lee WJ, Lai CH, et al. Urinary 1-Hydroxypyrene as an Indicator for Assessing the Exposures of Booth Attendants of a Highway Toll Station to Polycyclic Aromatic Hydrocarbons. Environ Sci Technol. 2003;38:56–61. doi: 10.1021/es030588k. [DOI] [PubMed] [Google Scholar]
- 8.Kang D, Rothman N, Cho SH, Lim HS, Kwon HJ, et al. Association of exposure to polycyclic aromatic hydrocarbons (estimated from job category) with concentration of 1-hydroxypyrene glucuronide in urine from workers at a steel plant. Occup Environ Med. 1995;52:593–599. doi: 10.1136/oem.52.9.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai CH, Liou SH, Lin HC, Shih TS, Tsai PJ, et al. Exposure to traffic exhausts and oxidative DNA damage. Occup Environ Med. 2005;62:216–222. doi: 10.1136/oem.2004.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Risom L, Moller P, Loft S. Oxidative stress-induced DNA damage by particulate air pollution. Mutat Res. 2005;592:119–137. doi: 10.1016/j.mrfmmm.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez-Flecha B. Oxidant mechanisms in response to ambient air particles. Mol Aspects Med. 2004;25:169–182. doi: 10.1016/j.mam.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 12.Scandalios JG. Oxidative stress responses–what have genome-scale studies taught us? Genome Biol. 2002;3:10191–10196. doi: 10.1186/gb-2002-3-7-reviews1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chuang C-Y, Lee C-C, Chang Y-K, Sung F-C. Oxidative DNA damage estimated by urinary 8-hydroxydeoxyguanosine: influence of taxi driving, smoking and areca chewing. Chemosphere. 2003;52:1163–1171. doi: 10.1016/S0045-6535(03)00307-2. [DOI] [PubMed] [Google Scholar]
- 14.Kim JY, Mukherjee S, Ngo LC, Christiani DC. Urinary 8-hydroxy-2'-deoxyguanosine as a biomarker of oxidative DNA damage in workers exposed to fine particulates. Environ Health Perspect. 2004;112:666–671. doi: 10.1289/ehp.6827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorensen M, Autrup H, Hertel O, Wallin H, Knudsen LE, et al. Personal exposure to PM2.5 and biomarkers of DNA damage. Cancer Epidemiol Biomarkers Prev. 2003;12:191–196. [PubMed] [Google Scholar]
- 16.Wei Y, Han IK, Shao M, Hu M, Zhang OJ, et al. PM2.5 constituents and oxidative DNA damage in humans. Environ Sci Technol. 2009;43:4757–4762. doi: 10.1021/es803337c. [DOI] [PubMed] [Google Scholar]
- 17.Moller P. The alkaline comet assay: towards validation in biomonitoring of DNA damaging exposures. Basic Clin Pharmacol Toxicol. 2006;98:336–345. doi: 10.1111/j.1742-7843.2006.pto_167.x. [DOI] [PubMed] [Google Scholar]
- 18.Nafstad P, Haheim LL, Oftedal B, Gram F, Holme I, et al. Lung cancer and air pollution: a 27 year follow up of 16209 Norwegian men. Thorax. 2003;58:1071–1076. doi: 10.1136/thorax.58.12.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai PJ, Shieh HY, Lee WJ, Lai SO. Characteristics of Exposure Profiles for Workers Exposed to Airborne Dusts and Polycyclic Aromatic Hydrocarbons (PAHs) in the Carbon Black Manufacturing Industry. Journal of occupational health. 2001;43:118–128. [Google Scholar]
- 20.Hu CW, Wang CJ, Chang LW, Chao MR. Clinical-scale high-throughput analysis of urinary 8-oxo-7,8-dihydro-2'-deoxyguanosine by isotope-dilution liquid chromatography-tandem mass spectrometry with on-line solid-phase extraction. Clin Chem. 2006;52:1381–1388. doi: 10.1373/clinchem.2005.063735. [DOI] [PubMed] [Google Scholar]
- 21.Hininger I, Chollat-Namy A, Sauvaigo S, Osman M, Faure H, et al. Assessment of DNA damage by comet assay on frozen total blood: method and evaluation in smokers and non-smokers. Mutation Research/Genetic Toxicology and Environmental Mutagenesis. 2004;558:75–80. doi: 10.1016/j.mrgentox.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Bell ML, Ebisu K, Peng RD, Samet JM, Dominici F. Hospital admissions and chemical composition of fine particle air pollution. Am J Respir Crit Care Med. 2009;179:1115–1120. doi: 10.1164/rccm.200808-1240OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peng RD, Bell ML, Geyh AS, McDermott A, Zeger SL, et al. Emergency admissions for cardiovascular and respiratory diseases and the chemical composition of fine particle air pollution. Environ Health Perspect. 2009;117:957–963. doi: 10.1289/ehp.0800185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bonvallot V, Baeza-Squiban A, Baulig A, Brulant S, Boland S, et al. Organic compounds from diesel exhaust particles elicit a proinflammatory response in human airway epithelial cells and induce cytochrome p450 1A1 expression. American journal of respiratory cell and molecular biology. 2001;25:515–521. doi: 10.1165/ajrcmb.25.4.4515. [DOI] [PubMed] [Google Scholar]
- 25.Penning TM, Burczynski ME, Hung CF, McCoull KD, Palackal NT, et al. Dihydrodiol dehydrogenases and polycyclic aromatic hydrocarbon activation: generation of reactive and redox active o-quinones. Chem Res Toxicol. 1999;12:1–18. doi: 10.1021/tx980143n. [DOI] [PubMed] [Google Scholar]
- 26.Squadrito GL, Cueto R, Dellinger B, Pryor WA. Quinoid redox cycling as a mechanism for sustained free radical generation by inhaled airborne particulate matter. Free Radic Biol Med. 2001;31:1132–1138. doi: 10.1016/s0891-5849(01)00703-1. [DOI] [PubMed] [Google Scholar]
- 27.Xia T, Korge P, Weiss JN, Li N, Venkatesen MI, et al. Quinones and aromatic chemical compounds in particulate matter induce mitochondrial dysfunction: implications for ultrafine particle toxicity. Environ Health Perspect. 2004;112:1347–1358. doi: 10.1289/ehp.7167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marczynski B, Rihs HP, Rossbach B, Holzer J, Angerer J, et al. Analysis of 8-oxo-7,8-dihydro-2'-deoxyguanosine and DNA strand breaks in white blood cells of occupationally exposed workers: comparison with ambient monitoring, urinary metabolites and enzyme polymorphisms. Carcinogenesis. 2002;23:273–281. doi: 10.1093/carcin/23.2.273. [DOI] [PubMed] [Google Scholar]
- 29.Marczynski B, Pesch B, Wilhelm M, Rossbach B, Preuss R, et al. Occupational exposure to polycyclic aromatic hydrocarbons and DNA damage by industry: a nationwide study in Germany. Arch Toxicol. 2009;83:947–957. doi: 10.1007/s00204-009-0444-9. [DOI] [PubMed] [Google Scholar]
- 30.Collins A, Dusinska M, Franklin M, Somorovska M, Petrovska H, et al. Comet assay in human biomonitoring studies: reliability, validation, and applications. Environ Mol Mutagen. 1997;30:139–146. doi: 10.1002/(sici)1098-2280(1997)30:2<139::aid-em6>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 31.Lai CH, Liou SH, Shih TS, Tsai PJ, Chen HL, et al. Urinary 1-hydroxypyrene-glucuronide as a biomarker of exposure to various vehicle exhausts among highway toll-station workers in Taipei, Taiwan. Arch Environ Health. 2004;59:61–69. doi: 10.3200/AEOH.59.2.61-69. [DOI] [PubMed] [Google Scholar]
- 32.Mecocci P, MacGarvey U, Kaufman AE, Koontz D, Shoffner JM, et al. Oxidative damage to mitochondrial DNA shows marked age-dependent increases in human brain. Ann Neurol. 1993;34:609–616. doi: 10.1002/ana.410340416. [DOI] [PubMed] [Google Scholar]
- 33.Sallis JF. Age-related decline in physical activity: a synthesis of human and animal studies. Med Sci Sports Exerc. 2000;32:1598–1600. doi: 10.1097/00005768-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Tovalin H, Valverde M, Morandi MT, Blanco S, Whitehead L, et al. DNA damage in outdoor workers occupationally exposed to environmental air pollutants. Occup Environ Med. 2006;63:230–236. doi: 10.1136/oem.2005.019802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kure EH, Ryberg D, Hewer A, Phillips DH, Skaug V, et al. p53 mutations in lung tumours: relationship to gender and lung DNA adduct levels. Carcinogenesis. 1996;17:2201–2205. doi: 10.1093/carcin/17.10.2201. [DOI] [PubMed] [Google Scholar]
- 36.Merlo F, Andreassen A, Weston A, Pan CF, Haugen A, et al. Urinary excretion of 1-hydroxypyrene as a marker for exposure to urban air levels of polycyclic aromatic hydrocarbons. Cancer Epidemiol Biomarkers Prev. 1998;7:147–155. [PubMed] [Google Scholar]
- 37.Hwang BF, Lee YL, Jaakkola JJ. Air pollution and stillbirth: a population-based case-control study in Taiwan. Environ Health Perspect. 2011;119:1345–1349. doi: 10.1289/ehp.1003056. [DOI] [PMC free article] [PubMed] [Google Scholar]