Abstract
Objective
Fear of movement has important clinical implications for individuals with osteoarthritis. This study aimed to establish a brief fear of movement scale for use in osteoarthritis. Items from the Tampa Scale for Kinesiophobia (TSK) were examined.
Methods
The English version of the TSK was examined in a community-based sample (N=1,136) of individuals with osteoarthritis of the hip or knee. Exploratory and confirmatory factor analyses were used to determine the number and content of the dimensions of fear of movement. Factorial invariance was tested across subgroups of gender, race, education, and osteoarthritis severity. Convergent validity with measures of pain, physical functioning, and psychological functioning was examined.
Results
Factor analyses identified a single factor 6-item scale that measures activity avoidance due to pain-related fear of movement (confirmatory factor analysis indices of model fit: RMSEA=.04; SRMR=.01; CFI=.99; TLI=.99). The 6-item scale demonstrated factorial invariance across gender, race, levels of education, and osteoarthritis severity suggesting that this scale performs consistently across diverse groups of individuals with osteoarthritis. Convergent validity with measures of pain (β=.30 to .41), physical functioning (β=.44 to .48), and psychological functioning (β=.36 to .37) was also demonstrated.
Conclusion
The brief fear of movement scale identified in this study provides a promising and valid approach for assessing fear of movement in individuals with osteoarthritis. This brief scale demonstrated several important strengths including a small number of items, sound psychometric properties, and consistent performance across diverse groups of individuals with osteoarthritis.
Fear of movement, or kinesiophobia, is described as a debilitating fear of physical movement and activity that an individual believes will cause pain, injury, or re-injury1. Fear of movement has been studied in diverse patient populations (e.g., chronic low back pain, chronic fatigue syndrome) and has been associated with increased pain, physical disability, and psychological disability2. Recent experimental data suggest that pain-related fear of movement and avoidance can be acquired through associative learning3. In patients with osteoarthritis (OA), maintaining a sufficient level of daily activity is critical to managing pain and disability associated with the disease4, but individuals who experience fear of movement may be hesitant to initiate or engage in daily activity.
Fear of movement has important clinical implications for individuals with OA5–9 and is increasingly a target of interventions aimed at reducing OA-related disability10,11. Several studies have demonstrated the negative impact of fear of movement on individuals with OA5–9. In a recent study6 in knee OA, fear of movement was significantly associated with greater psychological disability and slower gait speed after accounting for demographic and medical variables. Another study7 in OA indicated that fear of movement explained a significant proportion of variance in physical disability after controlling for pain and radiographic findings.
The lack of a validated fear of movement scale for OA, measurement problems, and the length of existing scales limit the widespread assessment of fear of movement in OA. Because the validity of a measure is dependent on the specific population being examined12, determining the appropriate structure and content of a fear of movement scale for OA is necessary. Findings from other samples of patients with persistent pain may not apply to OA. Beliefs about pain and movement may differ across populations and healthcare providers’ recommendations regarding physical activity could vary based on medical diagnosis13. Fear of movement scales designed for other populations (e.g., chronic pain, accident-related injury) may not be appropriate for use in OA. Disease-related pain due to OA usually occurs gradually over time, does not necessarily occur in response to a specific event or accident, and may worsen over time due to disease progression.
The present study was conducted to establish a brief fear of movement scale for use in OA. Items from the most widely used measure of fear of movement, the Tampa Scale for Kinesiophobia (TSK)14, were examined. The measurement properties of the TSK have been evaluated in patients with chronic and acute back pain15–23, fibromyalgia16,17,24, and musculoskeletal pain13,19. Two relatively small studies have examined the properties of the TSK in OA7,25, but these studies reported conflicting findings. Heuts and colleagues7 used confirmatory factor analysis to compare various structures of the TSK in individuals with OA and found a two factor structure. However, several TSK items did not perform well and exhibited low factor loadings. In another OA sample, Mielenz et al.25 found a one factor solution for the TSK. Item response theory analyses showed that one item (item 13) that was retained in the Heuts et al.7 study performed poorly and the authors recommended dropping it from the scale. Given conflicting findings across these two studies, the TSK dimensions and items appropriate for use in OA remain unclear.
The present study included a large (N=1,136) community-based sample of African American and White men and women with OA of the hip or knee. This study examined the number and content of the dimensions of the TSK in an OA sample, identified a brief fear of movement scale for use in OA, and tested the convergent validity of the identified fear of movement scale.
Materials and Methods
Participants
This study included participants in the Johnston County Osteoarthritis (JoCo OA) Project, a longitudinal, population-based study of the onset and progression of OA in a semirural North Carolina county. The JoCo OA project is the largest population-based, longitudinal study in the U.S. to monitor the occurrence and natural history of knee OA among African American and white men and women. Details about project methods are provided elsewhere26,27. The original JoCo OA Project cohort (1991–1998) was selected to be representative of the civilian, noninstitutionalized, English-speaking African American and white population aged >45 years who were residents of Johnston County for at least one year. A cohort enrichment occurred between 2003–200428. The sample for this analysis was derived from individuals from both these recruitments who participated in the second follow-up of the study (conducted 2006–2010). The current sample included 1,136 participants who had radiographic knee or hip OA and completed the TSK.
Measures
OA Grade
Knee radiographs were obtained in standard format with foot map positioning and assessed by a single radiologist (JBR) for Kellgren-Lawrence (K/L) grade using a standard knee atlas29. K/L grades for the tibiofemoral joint were defined as follows: 0=no OA, 1=questionable OA, 2=mild OA, 3=moderate OA, and 4=severe OA29. Participants with films suggesting underlying inflammatory arthropathy were eliminated from this analysis. Knee OA was defined as K/L grade of >2 in at least one knee. Hip OA was derived from anteroposterior pelvis films, also using the K/L scoring system, with OA defined as K/L grade>2 in at least one hip.
Fear of Movement
The TSK14 was examined to provide a brief fear of movement scale that is valid and reliable in people with OA. The original TSK is a self-report measure assessing the fear of injury/re-injury due to movement. The instrument consists of 17 items scored on a 4-point scale from “strongly agree” to “strongly disagree.”
Pain
Pain was assessed with three measures: a) The short form of the McGill Pain Questionnaire (SF-MPQ)30 contains 11 questions referring to the sensory dimension of pain and four related to the affective dimension. Each descriptor is ranked on a four point scale (0=none to 3=severe). This variable is referred to as Pain Description (Cronbach’s alpha in this sample=.66). b) Pain intensity was measured on an 11-point numeric pain rating scale (0–10), with higher numbers indicating higher pain. The numeric pain rating has been found to be a reliable and valid measure of pain intensity31. c) Pain was assessed with the pain subscale of the Western Ontario and McMasters Universities Osteoarthritis Index (WOMAC)32. The WOMAC is a well-established scale designed to assess pain, stiffness, and function in lower extremity OA. The total range of scores on the pain subscale is 0–20 with higher scores indicating higher pain (Cronbach’s alpha in this sample=.94).
Physical Functioning
Physical function was assessed with two measures. a) The WOMAC physical function scale32 can range from 0–68 with higher scores indicating greater problems with physical functioning (Cronbach’s alpha in this sample=.98). b) The Health Assessment Questionnaire (HAQ)33 is a measure of disability in arthritis. The HAQ includes 20 activities of daily living questions grouped into eight categories. Level of difficulty over the previous week is recorded (0=no difficulty to 3=unable to do). Cronbach’s alpha was .95 in this sample.
Psychological function
Two measures assessed psychological function. a) The five-item psychological function subscale of the Arthritis Impact Measurement Scales34 measured anxiety and tension (AIMS-anxiety). Cronbach’s alpha was .85 in this sample. b) Depressive symptoms were measured with the Center for Epidemiological Studies-Depression scale (CES-D)35. This 20-item scale assesses how often depressive symptoms have occurred in the past week (Cronbach’s alpha in this sample=.76).
Statistical Analysis
To examine the TSK factor structure, the sample was randomly divided into two equally sized subsamples. The two subsamples did not differ significantly (p >.10) on demographic, medical, or study variables. Exploratory factor analysis (EFA) was conducted in the first subsample. EFA provides more information about item performance than confirmatory factor analysis (CFA) and is preferred when the number of factors is unclear36. Maximum likelihood EFA was conducted with oblique quartimin rotation37 when more than one factor was extracted38. CFA was conducted in the second subsample to examine the fit of the model identified using EFA in the first subsample. EFA and CFA were conducted using Mplus 5.139. Several indices were used to examine model fit: root mean square error of approximation (RMSEA), the standardized root mean square residual (SRMSR), the comparative fit index (CFI), the Tucker-Lewis Index (TLI), and the Consistent Akaike Information Criterion (CAIC). Factorial invariance across subgroups of gender, race, education, and OA grade was examined in the total sample using the procedures recommended by Dimitrov40. Multiple regression analyses were conducted for the full sample to examine convergent validity.
Results
Participants
Participants had a mean age of 71.54 (SD=9.14) years and an average education of 13.64 (SD=4.13) years. The sample was 68.7% women and 31.3% men. Over half (59.1%) of participants were married. The sample was 71.7% White and 28.3% African American. Forty-five percent of participants had knee OA, 33% had hip OA, and 22% had both hip and knee OA. Participants with knee OA had the following OA grades in the worse severity knee: 1=4.2%, 2=34%, 3=29.2%, and 4=32.7%. Participants with hip OA had the following OA grades: 1=26.5%, 2=66.2%, 3=5.0%, and 4=2.3%.
Item descriptive statistics
Table 1 displays descriptive statistics for the 17 TSK items. Items were approximately normally distributed with the exception of item 6 (skew=1.01). For item 6, 10% (n=110) of participants indicated that the item did not apply to them. Among the remaining participants, 44% strongly disagree, 31% disagree, 11% agree, and 4% strongly agree.
Table 1.
TSK item descriptive Statistics (N=1,136)
| #a | Item | Mean (SD) | Median | Range |
|---|---|---|---|---|
| 1 | I am afraid that I may injure myself if I exercise | 1.91 (.78) | 2.00 | 1 – 4 |
| 2 | If I were to try to overcome it, my pain would increase | 2.05(.74) | 2.00 | 1 – 4 |
| 3 | My body is telling me that I have something dangerously wrong | 2.21(.91) | 2.00 | 1 – 4 |
| 4 | My pain would probably be relieved if I were to exercise b | 2.37(.81) | 2.00 | 1 – 4 |
| 5 | People are taking my medical condition seriously enough | 2.73(.89) | 3.00 | 1 – 4 |
| 6 | My accident has put my body at risk for the rest of my life c | 1.72(.84) | 2.00 | 1 – 4 |
| 7 | Pain always means I have injured my body | 1.92(.64) | 2.00 | 1 – 4 |
| 8 | Just because something aggravated my pain does not mean it’s dangerous b | 2.75(.65) | 3.00 | 1 – 4 |
| 9 | I am afraid that I might injure myself accidently | 2.12(.80) | 2.00 | 1 – 4 |
| 10 | Simply being careful that I do not make unnecessary movements is the safest thing I can do to prevent pain from worsening | 2.53 (.88) | 3.00 | 1 – 4 |
| 11 | I wouldn’t have this much pain if there wasn’t something potentially dangerous going on in my body | 1.93(.69) | 2.00 | 1 – 4 |
| 12 | Although my condition is painful, I would be better off if I were physically active b | 2.59(.91) | 3.00 | 1 – 4 |
| 13 | Pain lets me know when to stop exercising so that I don’t injure myself | 2.83(.68) | 3.00 | 1 – 4 |
| 14 | It’s really not safe for a person with a condition like mine to be physically active | 1.91(.73) | 3.00 | 1 – 4 |
| 15 | I can’t do all the things normal people do because it’s too easy to get injured | 2.03(.79) | 2.00 | 1 – 4 |
| 16 | Even though something is causing a lot of pain, I don’t think it’s actually dangerous b | 2.64(.69) | 3.00 | 1 – 4 |
| 17 | No one should have to exercise when he/she is in pain | 2.42(.69) | 2.00 | 1 – 4 |
The original TSK item numbers are retained for consistency and to allow for ease of comparison with other studies.
Items 4,8,12, and 16 are reversed scored.
For item 6, n=110 participants did not answer the item and indicated that the question did not apply to them.
Exploratory Factor Analysis (EFA)
EFA was conducted in the first subsample (N=568) with all 17 TSK items. While four eigenvalues exceeded the Kaiser-Guttman criteria41 of 1.0 (5.07, 2.16, 1.34, and 1.23), the scree test42 suggested a two-factor solution. We first extracted a two-factor solution as suggested by the scree test. The data were then under and over-factored by extracting one and three-factor solutions. Fit indices for each model are displayed in Table 2. The two-factor solution demonstrated mediocre fit. Examination of factor loadings for the two-factor extraction showed that item 6 failed to load on a single factor (loadings=.33 and .20; communality=.19) and loadings did not improve in the one and three-factor extractions. Consistent with prior TSK studies7,16,17,19,25,43 the four reverse scored items (4, 8, 12, and 16) failed to load on a single factor and exhibited low communalities (.01 to .07) in all three factor extractions.
Table 2.
Indices of fit for exploratory factor analysis (EFA) in the first subsample of participants (N=568)
| Model | Consistent Akaike Information Criterion (CAIC) | Root Mean Square Error of Approximation (RMSEA) | Standardized Root Mean Square Residual (SRMSR) | Comparative Fit Index (CFI) | Tucker-Lewis Index (TLI) |
|---|---|---|---|---|---|
| 17 Items | |||||
| One factor | 18354.21 | .12 | .10 | .70 | .66 |
| Two factors | 17889.52 | .08 | .05 | .87 | .83 |
| Three factors | 17803.22 | .07 | .04 | .91 | .87 |
| 12 Items | |||||
| One factor | 13672.22 | .11 | .07 | .84 | .81 |
| Two factors | 13456.81 | .08 | .04 | .93 | .90 |
| Three factors | 13401.01 | .07 | .03 | .96 | .93 |
| 6 Items | |||||
| One factor | 6358.36 | .13 | .03 | .95 | .92 |
| 5 Items | |||||
| One factor | 5612.32 | .09 | .02 | .98 | .96 |
After dropping item 6 and the four reverse scored items, we reran the EFA. For the remaining 12 TSK items, the Kaiser-Guttman criteria41 and the scree test42 suggested a two factor solution. We examined a two-factor solution and then under and over-factored by extracting one and three-factors. Indices of model fit are displayed in Table 2. The two factor solution demonstrated fair fit. The results of the two-factor extraction are displayed in Table 3. Multiple studies conducted in other pain populations7,16,17,19,21,43 have found that TSK items comprise an Activity Avoidance factor and a Harm/Somatic Focus factor. Table 3 displays items in this order for ease of comparison with prior studies. Of the Activity Avoidance items, items 13 and 17 had low loadings (≤.31) and low communalities (≤.21). The four Harm/Somatic Focus items failed to load on a single factor. Items 3 and 5 loaded on the second factor, while items 7 and 11 loaded more highly on the first factor. When one and three-factors were extracted, factor loadings did not improve. The three-factor solution was clearly over-factored, as only one item (Item 1) loaded on the third factor.
Table 3.
Exploratory factor analysis (EFA) in the first subsample of participants (N=568)
| Item # | TSK 12 Items | TSK 6 Items | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Factor 1 loading | Factor 2 loading | Communality | Factor Loading | Communality | ||
| Activity Avoidance Items | ||||||
| 1 | I am afraid that I may injure myself if I exercise | .73 | .01 | .54 | .75 | .56 |
| 2 | If I were to try to overcome it, my pain would increase | .67 | .04 | .47 | .68 | .46 |
| 9 | I am afraid that I might injure myself accidentally | .72 | −.04 | .49 | .70 | .49 |
| 10 | Simply being careful that I do not make unnecessary movements is the safest thing I can do to prevent pain from worsening | .51 | .23 | .41 | .59 | .35 |
| 13 | Pain lets me know when to stop exercising so that I don’t injure myself | .24 | .30 | .21 | ||
| 14 | It’s really not safe for a person with a condition like mine to be physically active | .82 | −.02 | .66 | .82 | .67 |
| 15 | I can’t do all the things normal people do because it’s too easy to get injured | .89 | −.03 | .76 | .87 | .75 |
| 17 | No one should have to exercise when he/she is in pain | .31 | −.04 | .09 | ||
| Harm/Somatic Focus Items | ||||||
| 3. | My body is telling me that I have something dangerously wrong | .06 | .79 | .67 | ||
| 5 | People are taking my medical condition seriously enough | −.08 | .68 | .42 | ||
| 7 | Pain always means I have injured my body | .39 | −.20 | .13 | ||
| 11 | I wouldn’t have this much pain if there wasn’t something potentially dangerous going on in my body | .54 | .14 | .37 | ||
| Variance accounted for by factor | 39.6% | 12.2% | 62.1% | |||
| Cronbach’s alpha for factor items | .85 | .54 | .87 | |||
| Descriptive Statistics: | ||||||
| Mean | 12.68 | |||||
| Standard Deviation | 3.72 | |||||
| Median | 13.00 | |||||
| Range | 6–24 | |||||
Based on the two-factor solution with 12 items, we dropped the two Activity Avoidance items (13 and 17) that exhibited poor factor loadings and communalities. We also dropped the four Harm/Somatic Focus items (3, 5, 7, and 11) because these items failed to load on the same factor, and two of the items (7 and 11) had fairly low factor loadings and communalities (see Table 3). The six remaining items from the TSK were then examined. For the remaining six items, the Kaiser-Guttman criteria41 and the scree test42 suggested a one-factor solution. The results of the one-factor extraction are displayed in Table 3. All six items exhibited adequate factor loadings and communalities. Fit indices indicated close model fit (see Table 2), with the exception of RMSEA (=.13), which was high. Modification indices provided by Mplus 5.1 were examined due to the high RMSEA. Modification indices suggested that the unique variances of similarly worded items 14 and 15 were correlated, which resulted in a high RMSEA value. To further explore the impact of overlapping items 14 and 15 on model fit, we conducted an additional EFA dropping the weaker of the two items (item 14). Indices of model fit were improved (see Table 2) and all five items exhibited adequate factor loadings and communalities. However, the six item scale was retained in all subsequent analyses because both items 14 and 15 had high factor loadings and communalities.
Confirmatory Factor Analysis (CFA)
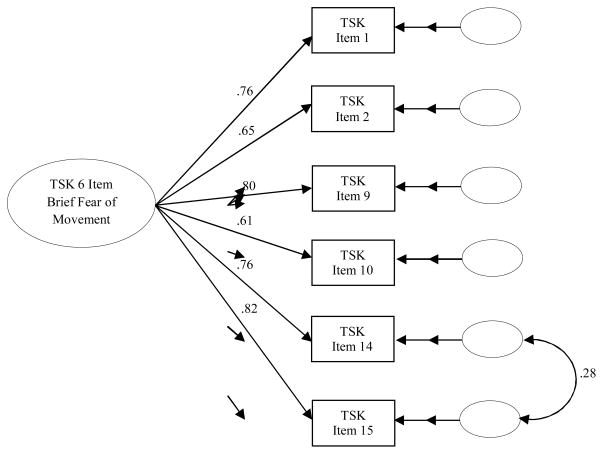
CFA was conducted in the second subsample (N=568) to examine the single factor structure with six TSK items identified using EFA in the first subsample. Figure 1 displays the factor loadings and unique variances for the CFA. All indices of fit indicated close model fit (CAIC=6541.67; RMSEA=.04; SRMR=.01; CFI=.99; TLI=.99). Based on EFA results, the CFA model allowed the unique variances of items 14 and 15 to correlate.
Figure 1.
Confirmatory factor analysis for TSK 6 Item in the second subsample (N=568)
Factorial Invariance
Factorial invariance was examined across subgroups of gender, race, education, and OA grade in the total sample. The procedure recommended by Dimitrov40 uses a multi-stage forward approach for testing factorial invariance across groups based on chi-square difference tests and examination of change in CFI between nested models. Invariance is accepted if the chi-square difference test is not significant (α=.05) and the CFI does not decrease by ≥.0144. A logical sequence of increasingly restrictive nested models is examined to test measurement and structural invariance. The sequence begins with an unconstrained model (Model 0). Measurement invariance is examined at three levels: metric (Model 1: factor loadings are invariant), scalar (Model 2: item intercepts are invariant), and item uniqueness (Model 3: item residuals are invariant). Structural invariance (Model 4) tests for invariant factor variances with invariant factor loadings.
For gender, comparison of models showed that factor loadings were invariant across men and women (Model 1 vs. Model 0: χ2=6.77, df=6, p=.34; ΔCFI<.001). Results showed scalar invariance for all items but one; item 14 had a slightly higher intercept for men compared to women (1.90 vs. 1.79, respectively). Partial scalar invariance was confirmed after re-running the model with the intercept for item 14 allowed to vary (Model 2 vs. Model 1: χ2=6.94, df=4, p=.14; ΔCFI=−.001). Analyses showed invariance of item uniqueness (Model 3 vs. Model 2:χ2 =8.19, df=6, p=.22; ΔCFI<.001) and structural invariance across men and women (Model 4 vs. Model 2: χ2=1.47, df=1, p=.23; ΔCFI<.001).
Analyses for race showed that factor loadings were invariant across African American and White participants (Model 1 vs. Model 0: χ2=3.79, df=6, p=.71; ΔCFI=.001). Scalar invariance was demonstrated for all items but one; item 9 had a slightly higher intercept for White participants compared to African American participants (2.16 vs. 1.99, respectively). Partial scalar invariance was confirmed after re-running the model with the intercept for item 9 allowed to vary (Model 2 vs. Model 1: χ2=7.79, df=4, p=.10; ΔCFI=−.001). Analyses showed invariance of item uniqueness (Model 3 vs. Model 2: χ2=8.45, df=6, p=.21; ΔCFI=−.001) and structural invariance across African American and White participants (Model 4 vs. Model 2:χ2=0.04, df=1, p=.84; ΔCFI<.001).
For education (≤high school education vs. >high school education), comparison of models showed that factor loadings (Model 1 vs. Model 0: χ2=6.21, df=6, p=.40; ΔCFI=−.001) and item intercepts (Model 2 vs. Model 1: χ2=9.27, df=5, p=.10; ΔCFI=−.001) were invariant across level of education. Invariance of item uniqueness was found for all items but one; item 15 was found to have greater residual variance in those with ≤high school education compared to those with >high school education (.18 vs. .11, respectively). Partial invariance of item uniqueness was confirmed after re-running the model with the residual variance of item 15 allowed to vary (Model 3 vs. Model 2: χ2=6.91, df=5, p=.23; ΔCFI=−.001). Comparison of models showed structural invariance across levels of education (Model 4 vs. Model 2: χ2=0.38, df=1, p=.54; ΔCFI<.001).
Analyses for OA Grade (≤2 mild OA vs. ≥3 moderate to severe OA) showed that factor loadings (Model 1 vs. Model 0: χ2=9.17, df=6, p=.16; ΔCFI<.001) and item intercepts (Model 2 vs. Model 1: χ2=6.97, df=5, p=.22; ΔCFI=−.001) were invariant across OA grade. Analyses also showed invariance of item uniqueness (Model 3 vs. Model 2: χ2=8.98, df=6, p=.17; ΔCFI=−.001) and structural invariance across OA grade (Model 4 vs. Model 2: χ2=0.04, df=1, p=.84;ΔCFI<.001).
Convergent Validity
Table 4 displays correlations and 95% confidence intervals for correlations between the 6-item Brief Fear of Movement Scale and participant characteristics. Multiple regression analyses examined convergent validity of the Brief Fear of Movement Scale while controlling for participant characteristics (see Table 5). Moderate positive associations were found between fear of movement and measures of pain and stiffness (β=.30 to .41). The strongest associations were found between higher scores on the Brief Fear of Movement Scale and higher scores on measures of physical functioning (β=.44 to .48). Moderate positive associations were found between fear of movement and measures of psychological function (β=.36 to .37).
Table 4.
Correlations examining relationships between participant characteristics and the TSK 6-item Brief Fear of Movement Scale (N=1,136)
| TSK 6 Item Brief Fear of Movement Scale
|
||
|---|---|---|
| Pearson’s and point-biserial correlations | 95% CI for correlation | |
| Age (in years) | .21 | .15 to .27 |
| Education (in years) | −.29 | −.34 to −.23 |
| Gender (0=Male, 1=Female) | .08 | .02 to .14 |
| Race (0=White, 1=African American) | .09 | .03 to.15 |
| Marital status (0=Not married, 1=Married) | −.14 | −.20 to −.09 |
| Worse knee OA grade | .20 | .14 to .25 |
| Worse hip OA grade | .17 | .12 to .23 |
Note: All correlations significant at p<.05.
Table 5.
Multiple regression analysis examining convergent validity of the TSK 6-item Brief Fear of Movement Scale (N=1,136)
| Final standardized β | p | Squared semi-partial r | |
|---|---|---|---|
| Dependent Variable: McGill Pain Description | |||
| Age (years) | −.06 | .05 | .003 |
| Education (years) | −.04 | .18 | .002 |
| Gendera | .06 | .05 | .003 |
| Raceb | −.01 | .75 | .0001 |
| OA gradec | .06 | .06 | .003 |
| TSK 6-item Brief Fear of Movement Scale | .30 | <.001 | .08 |
| Dependent Variable: McGill Pain Intensity | |||
| Age (years) | −.07 | .007 | .006 |
| Education (years) | −.04 | .21 | .001 |
| Gender | .10 | <.001 | .01 |
| Race | −.02 | .42 | .0001 |
| OA grade | .16 | <.001 | .03 |
| TSK 6-item Brief Fear of Movement Scale | .41 | <.001 | .16 |
| Dependent Variable: WOMAC Pain | |||
| Age (years) | −.15 | <.001 | .03 |
| Education (years) | −.07 | .01 | .006 |
| Gender | .08 | .002 | .009 |
| Race | −.03 | .27 | .001 |
| OA grade | .23 | <.001 | .07 |
| TSK 6-item Brief Fear of Movement Scale | .40 | <.001 | .16 |
| Dependent Variable: WOMAC Stiffness | |||
| Age (years) | −.10 | .001 | .01 |
| Education (years) | −.08 | .01 | .006 |
| Gender | .08 | .004 | .008 |
| Race | −.005 | .87 | <.0001 |
| OA grade | .22 | <.001 | .06 |
| TSK 6-item Brief Fear of Movement Scale | .34 | <.001 | .11 |
| Dependent Variable: WOMAC Function | |||
| Age (years) | −.08 | .006 | .008 |
| Education (years) | −.08 | .006 | .008 |
| Gender | .10 | <.001 | .01 |
| Race | −.001 | .96 | <.0001 |
| OA grade | .21 | <.001 | .06 |
| TSK 6-item Brief Fear of Movement Scale | .44 | <.001 | .20 |
| Dependent Variable: Health Assessment Questionnaire (HAQ) | |||
| Age (years) | .09 | .001 | .01 |
| Education (years) | −.06 | .03 | .005 |
| Gender | .18 | <.001 | .05 |
| Race | −.02 | .48 | .0005 |
| OA grade | .14 | <.001 | .03 |
| TSK 6-item Brief Fear of Movement Scale | .48 | <.001 | .25 |
| Dependent Variable: Center for Epidemiologic Studies Depression Scale (CES-D) | |||
| Age (years) | −.10 | .001 | .01 |
| Education (years) | −.09 | .003 | .008 |
| Gender | .09 | .001 | .009 |
| Race | .03 | .26 | .001 |
| OA grade | −.02 | .48 | .0004 |
| TSK 6-item Brief Fear of Movement Scale | .37 | <.001 | .12 |
| Dependent Variable: Arthritis Impact Measurement Scale (AIMS) Anxiety/Tension | |||
| Age (years) | −.16 | <.001 | .03 |
| Education (years) | .03 | .28 | .001 |
| Gender | .17 | <.001 | .03 |
| Race | −.02 | .51 | .0004 |
| OA grade | −.06 | .06 | .004 |
| TSK 6-item Brief Fear of Movement Scale | .36 | <.001 | .12 |
Gender coded as 0=men, 1=women
Race coded as 0=White, 1=African American
OA grade coded as 0=worse hip or knee OA grade mild (i.e., ≤ 2), 1=worse hip or knee OA grade moderate to severe (i.e., ≥ 3)
Discussion
The present study identified and evaluated a brief fear of movement scale for use in OA. Exploratory and confirmatory factor analyses identified a Brief Fear of Movement Scale for OA that includes six items from the TSK14 that capture activity avoidance due to pain-related fear of movement. The Brief Fear of Movement Scale performed consistently across diverse groups of individuals as demonstrated by factorial invariance across gender, race, education, and OA grade. The scale also demonstrated relationships with measures of pain, physical functioning, and psychological functioning indicating that this scale has convergent validity. Taken together, these results indicate that the Brief Fear of Movement Scale provides a valid approach for assessing fear of movement in OA.
An important finding from this work is that the Brief Fear of Movement Scale showed invariance across subgroups of gender, race, education level, and OA grade. Results showed that the structure (factor variances and loadings) of the measure was consistent across the subgroups examined. While slight differences in item intercepts and uniqueness were found in several cases, the small number and magnitude of these differences suggested that this measure performs consistently across subgroups40. These results indicate that the Brief Fear of Movement Scale developed in this work can be used in diverse groups of individuals with OA.
The Brief Fear of Movement Scale demonstrated convergent validity with measures of pain, physical functioning, and psychological functioning. The strongest relationships were found between fear of movement and measures of physical function. These findings are consistent with prior studies that have demonstrated a negative impact of fear of movement on functioning in individuals with OA5–9. The Brief Fear of Movement Scale shared approximately 25% of its variance with measures of physical functioning. The Brief Fear of Movement Scale exhibited moderate relationships with pain and psychological functioning, which is consistent with past studies in OA6,7. Finally, the Brief Fear of Movement Scale demonstrated weak associations with OA grade, which is consistent with other work suggesting that fear of movement is important to assess in addition to disease severity5–9.
For the Brief Fear of Movement Scale, we dropped the four reverse scored TSK items, item 6, and items 13 and 17 from the Activity Avoidance factor. This study and numerous studies of the TSK7,16,17,19,25,43 have found that the four reverse scored items fail to correlate with other TSK items. Item 6 was dropped because our data suggested that this item might be inappropriate for use in individuals with OA and it failed to correlate with other TSK items. Items 13 and 17 did not load with other TSK items and performed poorly in the analyses. Mielenz et al.25 also reported problems with item 13 in a study of OA and concluded that item 13 had little in common with other TSK items. Item 17 has exhibited low factor loadings in prior studies21,24,45–47, and was among the more poorly performing items in analysis conducted by Mielenz et al.25
We chose to drop the four harm/somatic focus TSK items from the Brief Fear of Movement Scale because these items did not load on a single factor and exhibited fairly low loadings. If future measures include these items, users should be made aware that these four items may not form a single factor. In this study, two items (3 and 5) focused on the seriousness of pain loaded together on a factor, but the two remaining items showed higher loadings on the activity avoidance factor. Additional studies are needed to determine whether these four items capture information that is indicative of fear of movement in individuals with OA. It is possible that the content of these items may be more suggestive of a tendency to catastrophize about pain24, rather than fear of movement.
While this study included a large community based sample of individuals with OA, findings need to be viewed within the particular circumstances of this study. First, this study included a single assessment, which prohibits testing reliability of the scale over time or sensitivity to changes in disease or function over time. Second, all of the variables examined for convergent validity were assessed using self-report measures, which raises possible concerns over common method bias in the estimation of these relationships. Third, these data were collected as part of a population-based study of the onset and progression of OA. Hypotheses and analyses examining the psychometric properties and convergent validity of the Brief Fear of Movement Scale were conducted post hoc. Finally, the study sample included individuals with OA who were living in North Carolina. Additional studies are needed to determine whether these results generalize to individuals living in other geographic regions and to populations with other types of disease related pain.
Fear of movement is an important target for reducing disability in individuals with OA5–10. Having a valid measure for assessing fear of movement in OA has important clinical implications. Once identified, pain-related fear of movement could be treated using in vivo exposure techniques. Vlaeyen et al.48–50 have developed in vivo exposure techniques that enable patients with pain to learn that they can successfully experience and habituate to movements or activities that they might normally avoid. These techniques have been found to be effective in decreasing pain and disability in patients with other persistent pain conditions and could be adapted for use in individuals with OA.
The Brief Fear of Movement Scale identified in this study provides a promising and valid approach for assessing fear of movement in OA. This brief scale demonstrated several important strengths including a small number of items, sound psychometric properties, and consistent performance across diverse groups. Future longitudinal and experimental studies are needed to further examine the scale’s stability over time and its sensitivity to change.
Significance and Innovation.
Fear of movement has important clinical implications for individuals with osteoarthritis including increased pain, physical disability, and psychological disability. It is increasingly a target of interventions aimed at reducing osteoarthritis-related disability.
The lack of a validated fear of movement scale for osteoarthritis, measurement problems, and the length of existing scales limit the widespread assessment of fear of movement in osteoarthritis clinical and research settings.
The present study identified and evaluated a Brief Fear of Movement Scale for use in osteoarthritis based on the most widely used fear of movement scale, the Tampa Scale for Kinesiophobia (TSK).
The Brief Fear of Movement Scale identified in this study demonstrated several important strengths including a small number of items (i.e. six items), sound psychometric properties, and consistent performance across diverse groups of individuals with osteoarthritis.
Acknowledgments
Grant Support: Centers for Disease Control and Prevention/Association of Schools of Public Health S043, S1733, and S3486; Multipurpose Arthritis and Musculoskeletal Diseases Center grant 5-P60-AR-30701 and the Multidisciplinary Clinical Research Center grant P60-AR49465 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and National Institute of Mental Health Grant R01 MH64034
Footnotes
Conflicts of Interest:
None
References
- 1.Vlaeyen JWS, KoleSnijders AMJ, Rotteveel AM, Ruesink R, Heuts P. The role of fear of movement (re)injury in pain disability. Journal of Occupational Rehabilitation. 1995 Dec;5(4):235–252. doi: 10.1007/BF02109988. [DOI] [PubMed] [Google Scholar]
- 2.Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000 Apr;85(3):317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 3.Meulders A, Vansteenwegen D, Vlaeyen JWS. The acquisition of fear of movement-related pain and associative learning: A novel pain-relevant human fear conditioning paradigm. Pain. 2011 Nov;152(11):2460–2469. doi: 10.1016/j.pain.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Dekker J, Tola P, Aufdemkampe G, Winckers M. NEGATIVE AFFECT, PAIN AND DISABILITY IN OSTEOARTHRITIS PATIENTS - THE MEDIATING ROLE OF MUSCLE WEAKNESS. Behaviour Research and Therapy. 1993 Feb;31(2):203–206. doi: 10.1016/0005-7967(93)90073-4. [DOI] [PubMed] [Google Scholar]
- 5.Damsgard E, Thrane G, Anke A, Fors T, Roe C. Activity-related pain in patients with chronic musculoskeletal disorders. Disability and Rehabilitation. 2010;32(17):1428–1437. doi: 10.3109/09638280903567877. [DOI] [PubMed] [Google Scholar]
- 6.Somers TJ, Keefe FJ, Pells JJ, et al. Pain Catastrophizing and Pain-Related Fear in Osteoarthritis Patients: Relationships to Pain and Disability. Journal of Pain and Symptom Management. 2009 May;37(5):863–872. doi: 10.1016/j.jpainsymman.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heuts P, Vlaeyen JWS, Roelofs J, et al. Pain-related fear and daily functioning in patients with osteoarthritis. Pain. 2004 Jul;110(1–2):228–235. doi: 10.1016/j.pain.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 8.Morone NE, Karp JF, Lynch CS, Bost JE, El Khoudary SR, Weiner DK. Impact of Chronic Musculoskeletal Pathology on Older Adults: A Study of Differences between Knee OA and Low Back Pain. Pain Medicine. 2009 May-Jun;10(4):693–701. doi: 10.1111/j.1526-4637.2009.00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steultjens MPM, Dekker J, Bijlsma JWJ. Avoidance of activity and disability in patients with osteoarthritis of the knee - The mediating role of muscle strength. Arthritis and Rheumatism. 2002 Jul;46(7):1784–1788. doi: 10.1002/art.10383. [DOI] [PubMed] [Google Scholar]
- 10.Williams NH, Amoakwa E, Burton K, et al. Activity Increase Despite Arthritis (AIDA): design of a Phase II randomised controlled trial evaluating an active management booklet for hip and knee osteoarthritis ISRCTN24554946. Bmc Family Practice. 2009 Sep 4;10 doi: 10.1186/1471-2296-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Veenhof C, Koke AJA, Dekker J, et al. Effectiveness of behavioral graded activity in patients with osteoarthritis of the hip and/or knee: A randomized clinical trial. Arthritis & Rheumatism-Arthritis Care & Research. 2006 Dec 15;55(6):925–934. doi: 10.1002/art.22341. [DOI] [PubMed] [Google Scholar]
- 12.Portney LGWM. Foundations of Clinical Research: Applications to Practice. 2. Upper Saddle River, NJ: Prentice Hall Health; 2000. [Google Scholar]
- 13.Lundberg M, Styf J, Jansson B. On what patients does the Tampa Scale for Kinesiophobia fit? Physiotherapy Theory and Practice. 2009;25(7):495–506. doi: 10.3109/09593980802662160. [DOI] [PubMed] [Google Scholar]
- 14.Miller RKS, Tood D. The Tampa Scale for Kinesiophobia. 1991. [Google Scholar]
- 15.Geisser ME, Haig AJ, Theisen ME. Activity avoidance and function in persons with chronic back pain. Journal of Occupational Rehabilitation. 2000 Sep;10(3):215–227. [Google Scholar]
- 16.Roelofs J, Goubert L, Peters ML, Vlaeyen JWS, Crombez G. The Tampa Scale for Kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. European Journal of Pain. 2004 Oct;8(5):495–502. doi: 10.1016/j.ejpain.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Goubert L, Crombez G, Van Damme S, Vlaeyen JWS, Bijttebier P, Roelofs J. Confirmatory factor analysis of the Tampa scale, for Kinesiophobia - Invariant two-factor model across low back pain patients and fibromyalgia patients. Clinical Journal of Pain. 2004 Mar-Apr;20(2):103–110. doi: 10.1097/00002508-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Houben RMA, Leeuw M, Vlaeyen JWS, Goubert L, Picavet HSJ. Fear of movement/injury in the general population: Factor structure and psychometric properties of an adapted version of the Tampa Scale for Kinesiophobia. Journal of Behavioral Medicine. 2005 Oct;28(5):415–424. doi: 10.1007/s10865-005-9011-x. [DOI] [PubMed] [Google Scholar]
- 19.Roelofs J, Sluiter JK, Frings-Dresen MHW, et al. Fear of movement and (re)injury in chronic musculoskeletal pain: Evidence for an invariant two-factor model of the Tampa Scale for Kinesiophobia across pain diagnoses and Dutch, Swedish, and Canadian samples. Pain. 2007 Sep;131(1–2):181–190. doi: 10.1016/j.pain.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 20.Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: A shortened version of the Tampa scale for kinesiophobia. Pain. 2005 Sep;117(1–2):137–144. doi: 10.1016/j.pain.2005.05.029. [DOI] [PubMed] [Google Scholar]
- 21.French DJ, France CR, Vigneau F, French JA, Evans RT. Fear of movement/(re)injury in chronic pain: A psychometric assessment of the original English version of the Tampa scale for kinesiophobia (TSK) Pain. 2007 Jan;127(1–2):42–51. doi: 10.1016/j.pain.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 22.Swinkels-Meewisse E, Swinkels R, Verbeek ALM, Vlaeyen JWS, Oostendorp RAB. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Manual Therapy. 2003 Feb;8(1):29–36. doi: 10.1054/math.2002.0484. [DOI] [PubMed] [Google Scholar]
- 23.Swinkels-Meewisse IEJ, Roelofs J, Verbeek ALM, Oostendorp RAB, Vlaeyen JWS. Fear of movement/(re)injury, disability and participation in acute low back pain. Pain. 2003 Sep;105(1–2):371–379. doi: 10.1016/s0304-3959(03)00255-0. [DOI] [PubMed] [Google Scholar]
- 24.Burwinkle T, Robinson JP, Turk DC. Fear of movement: Factor structure of the Tampa Scale of Kinesiophobia in patients with fibromyalgia syndrome. Journal of Pain. 2005 Jun;6(6):384–391. doi: 10.1016/j.jpain.2005.01.355. [DOI] [PubMed] [Google Scholar]
- 25.Mielenz TJ, Edwards MC, Callahan LF. First item response theory analysis on Tampa Scale for Kinesiophobia (fear of movement) in arthritis. Journal of Clinical Epidemiology. 2010 Mar;63(3):315–320. doi: 10.1016/j.jclinepi.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of Hip Symptoms and Radiographic and Symptomatic Hip Osteoarthritis in African Americans and Caucasians: The Johnston County Osteoarthritis Project. Journal of Rheumatology. 2009 Apr;36(4):809–815. doi: 10.3899/jrheum.080677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jordan JMHC, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic kee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;(34):172–180. [PubMed] [Google Scholar]
- 28.Allen KD, Chen J-C, Callahan LF, et al. Associations of Occupational Tasks with Knee and Hip Osteoarthritis: The Johnston County Osteoarthritis Project. Journal of Rheumatology. 2010 Apr;37(4):842–850. doi: 10.3899/jrheum.090302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kellgren JHLJ, Bier F. Genetic factors in generalized oste-arthrosis. Ann Rheum Dis. 1963;(22):237–255. doi: 10.1136/ard.22.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melzack R. THE SHORT-FORM MCGILL PAIN QUESTIONNAIRE. Pain. 1987 Aug;30(2):191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 31.Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001 Nov;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 32.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. VALIDATION-STUDY OF WOMAC - A HEALTH-STATUS INSTRUMENT FOR MEASURING CLINICALLY IMPORTANT PATIENT RELEVANT OUTCOMES TO ANTIRHEUMATIC DRUG-THERAPY IN PATIENTS WITH OSTEO-ARTHRITIS OF THE HIP OR KNEE. Journal of Rheumatology. 1988 Dec;15(12):1833–1840. [PubMed] [Google Scholar]
- 33.Ramey DR, Raynauld JP, Fries JF. The health assessment questionnaire 1992: status and review. Arthritis care and research: the official journal of the Arthritis Health Professions Association. 1992 Sep;5(3):119–129. doi: 10.1002/art.1790050303. [DOI] [PubMed] [Google Scholar]
- 34.Meenan RF, Gertman PM, Mason JH. MEASURING HEALTH-STATUS IN ARTHRITIS - ARTHRITIS IMPACT MEASUREMENT SCALES. Arthritis and Rheumatism. 1980;23(2):146–152. doi: 10.1002/art.1780230203. [DOI] [PubMed] [Google Scholar]
- 35.Radloff LS. THE CENTER FOR EPIDEMIOLOGIC STUDIES DEPRESSION SCALE A SELF REPORT DEPRESSION SCALE FOR RESEARCH IN THE GENERAL POPULATION. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 36.RLG . Factor analysis. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- 37.Jennrich RI, Sampson PF. ROTATION FOR SIMPLE LOADINGS. Psychometrika. 1966;31(3):313–313. doi: 10.1007/BF02289465. [DOI] [PubMed] [Google Scholar]
- 38.Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999 Sep;4(3):272–299. [Google Scholar]
- 39.Muthen LKMB. Mplus: statistical analysis with latent variables. User’s guide. Los Angeles, CA: Muthen & Muthen; 2005. [Google Scholar]
- 40.Dimitrov DM. Testing for Factorial Invariance in the Context of Construct Validation. Measurement and Evaluation in Counseling and Development. 2010 Jul;43(2):121–149. [Google Scholar]
- 41.Guttman L. SOME NECESSARY CONDITIONS FOR COMMON-FACTOR ANALYSIS. Psychometrika. 1954 Jun;19(2):149–161. [Google Scholar]
- 42.Cattell RB. The scree test for the number of factors. Multivariate Behav Res. 1966;1:254–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- 43.Clark MA, Kori S, Brockel J. Kinesiophobia and chronic pain: psychometric characteristics and factor analysis of the Tampa Scale. Paper presented at: American Pain Society. 1996:Abstract 77. [Google Scholar]
- 44.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling. 2002;9(2):233–255. [Google Scholar]
- 45.Wong WS, Kwok HY, Luk KDK, et al. FEAR OF MOVEMENT/(RE)INJURY IN CHINESE PATIENTS WITH CHRONIC PAIN: FACTORIAL VALIDITY OF THE CHINESE VERSION OF THE TAMPA SCALE FOR KINESIOPHOBIA. Journal of Rehabilitation Medicine. 2010 Jul;42(7):620–629. doi: 10.2340/16501977-0575. [DOI] [PubMed] [Google Scholar]
- 46.Visscher CM, Ohrbach R, van Wijk AJ, Wilkosz M, Naeije M. The Tampa Scale for Kinesiophobia for Temporomandibular Disorders (TSK-TMD) Pain. 2010 Sep;150(3):492–500. doi: 10.1016/j.pain.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 47.Vlaeyen JWS, Kolesnijders AMJ, Boeren RGB, Vaneek H. FEAR OF MOVEMENT (RE)INJURY IN CHRONIC LOW-BACK-PAIN AND ITS RELATION TO BEHAVIORAL PERFORMANCE. Pain. 1995 Sep;62(3):363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 48.de Jong JR, Vlaeyen JWS, Onghena P, Cuypers C, den Hollander M, Ruijgrok J. Reduction of pain-related fear in complex regional pain syndrome type I: The application of graded exposure in vivo. Pain. 2005 Aug;116(3):264–275. doi: 10.1016/j.pain.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 49.Vlaeyen JWS, de Jong J, Geilen M, Heuts P, van Breukelen G. Graded exposure in vivo in the treatment of pain-related fear: a replicated single-case experimental design in four patients with chronic low back pain. Behaviour Research and Therapy. 2001 Feb;39(2):151–166. doi: 10.1016/s0005-7967(99)00174-6. [DOI] [PubMed] [Google Scholar]
- 50.Vlaeyen JWS, de Jong J, Geilen M, Heuts P, van Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: Further evidence on the effectiveness of exposure in vivo. Clinical Journal of Pain. 2002 Jul-Aug;18(4):251–261. doi: 10.1097/00002508-200207000-00006. [DOI] [PubMed] [Google Scholar]