Abstract
Objectives
To describe how members of the older general public deliberate with one another in finding solutions to the dilemma of involving decisionally incapable persons in dementia research.
Design, Setting, and Participants
160 persons aged 50+ who participated in an all-day deliberative democracy (DD) session on the ethics of surrogate consent for dementia research. The DD day consisted of both extensive, interactive education with experts in clinical research and ethics, as well as small group deliberations.
Measurements
Audiotaped small group deliberations were transcribed and analyzed, and the main thematic elements were coded.
Results
During deliberation, participants acknowledged the limitations of advanced research directives and discussed ways to improve their use. Although there was consensus about the necessity of surrogate consent, the participants recognized potential pitfalls and looked for ways to safeguard the process. Participants supporting surrogate consent for research emphasized societal and individual benefit, the importance of assent, and trust in surrogates and the oversight system. Other participants felt that the high risk of some research scenarios was not sufficiently offset by benefits to patients or society.
Conclusions
Members of the older general public are able to make use of in-depth education and peer deliberation to provide reasoned and informed opinions on the ethical use of surrogate consent for dementia research. The public’s approach to surrogate consent is one of cautious pragmatism: an overall trust in science and future surrogates with awareness of the potential pitfalls, suggesting that their trust cannot be taken for granted.
Keywords: surrogate consent, dementia, deliberative democracy
Alzheimer’s disease (AD) is incurable, devastating, and highly prevalent. The clinical research necessary to make progress against AD, however, poses the dilemma of involving patients with substantial cognitive impairment who lack the ability to provide informed consent.(1, 2) The dilemma is magnified when the research is invasive and burdensome, with unpredictable risks.(3–5) Despite several decades of debate in the U.S., no clear policy exists regarding the involvement of adults with decisional impairments in clinical research.(6) AD research centers(7, 8) research ethics review boards(9, 10), and dementia experts and advocates(11) vary considerably in their viewpoints, policies and practices in dealing with this ethical issue.
Several studies have suggested that there is considerable support for surrogate consent for dementia research.(12–15) But most of these studies have been traditional cross-sectional surveys and do not provide insights into the underlying basis for these opinions. Given the historical, ethical, and scientific complexities of the topic, understanding the underlying reasons for such opinions would provide insights into their validity.(16)
We have been investigating the views of the general public regarding surrogate consent for dementia research using democratic deliberation (DD). The practice of DD is built on normative theory that regards citizens’ views as important and necessary sources of public policy. The goal is to obtain considered opinions of citizens that result from a fair, respectful, and transparent interchange of viewpoints based on thorough education and peer deliberation; such opinions can then inform democratic policy-making.(17, 18) DD is increasingly recognized as useful for soliciting public opinion on controversial policies.(19) For example, the Agency for Healthcare Research and Quality is currently conducting a large scale study of democratic deliberation to inform comparative effectiveness research(20) and the U.S. Presidential Commission for the Study of Bioethical Issues has recommended democratic deliberation to inform bioethics policy debates.(21)
In our deliberative study, members of the older general public participated in a day long session of in-depth education and peer deliberation concerning the ethics of surrogate consent for dementia research.(16) We found broad initial support for a policy of surrogate consent for research that significantly increased after deliberation.(22) We also found through detailed qualitative analysis that the quality of deliberation in our DD sessions was quite good and that participants learned and used new information, were respectful and collaborative, and were able to “reason together” to arrive at societal policy recommendations.(23) In this article, we explore the major themes of deliberation among our participants as they discuss and debate the ethics of surrogate consent for dementia research.
METHODS
A comprehensive account of the theoretical basis and methodological procedures for this study has been published elsewhere.(16) The study was reviewed by the University of Michigan’s Institutional Review Board and deemed exempt from federal regulations.
Participants
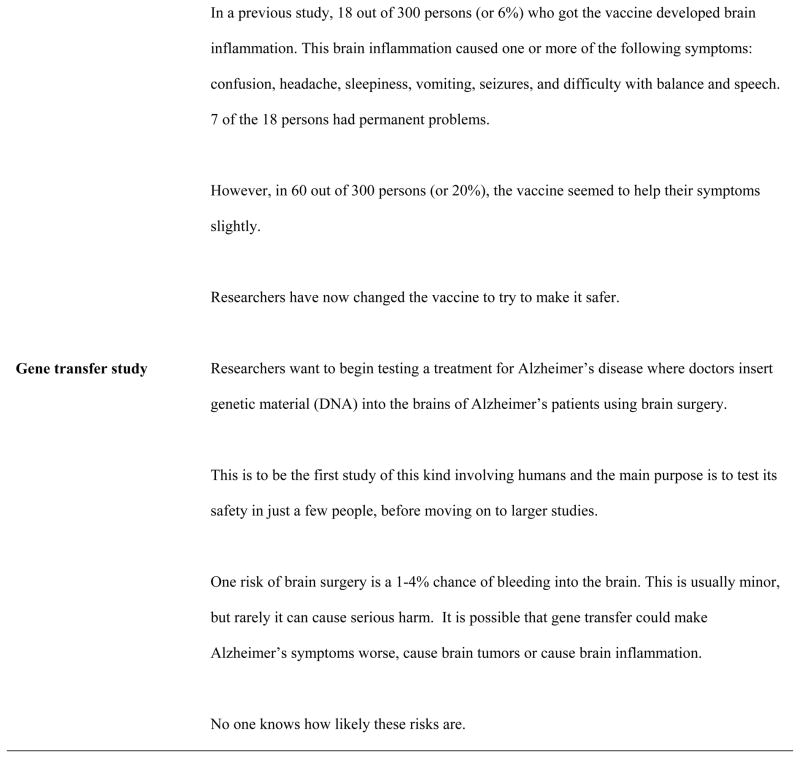
160 members of the general public (≥50 years old) who had been randomized (n=212, 75% attendance rate) into the deliberation arm of a 3-arm study (total n=503, recruited via random digit dialing within a 50-mile radius of Ann Arbor, MI) attended an all-day deliberative session. Other arms included an education-only group (receiving educational materials but not attending DD sessions, n=141) and a control group (no intervention, n=150). Since only the DD group participated in deliberations, only their data are presented in this paper (see Table 1).
Table 1.
Participant characteristics, n=160.
| Demographics | n (%)a or Mean±SD |
|---|---|
| Female | 97 (61) |
| Age (years) | 63±8 |
| What is your current marital status? | |
| Single | 13 (8) |
| Married | 103 (64) |
| Divorced | 26 (16) |
| Widowed | 17 (11) |
| Are you Hispanic or Latino/Latina? | |
| Yes | 1 (1) |
| What is your race? | |
| White | 143 (89) |
| Black or African-American | 16 (10) |
| Other | 1 (1) |
| What is the highest level of education you have completed? | |
| Less than college | 81 (51) |
| College | 39 (24) |
| More than college | 40 (25) |
| In general, how do your finances work out at the end of a typical month? | |
| Some money left over | 110 (69) |
| Just enough to make ends meet | 37 (23) |
| Not enough to make ends meet | 8 (5) |
| Do you have any relationship with an Alzheimer’s patient? | |
| Primary Caregiver/Decision-maker | 46 (29) |
| Close to someone with AD | 70 (44) |
| No relation | 43 (27) |
Some percentages do not add to 100 because not all participants answered the question.
Procedures
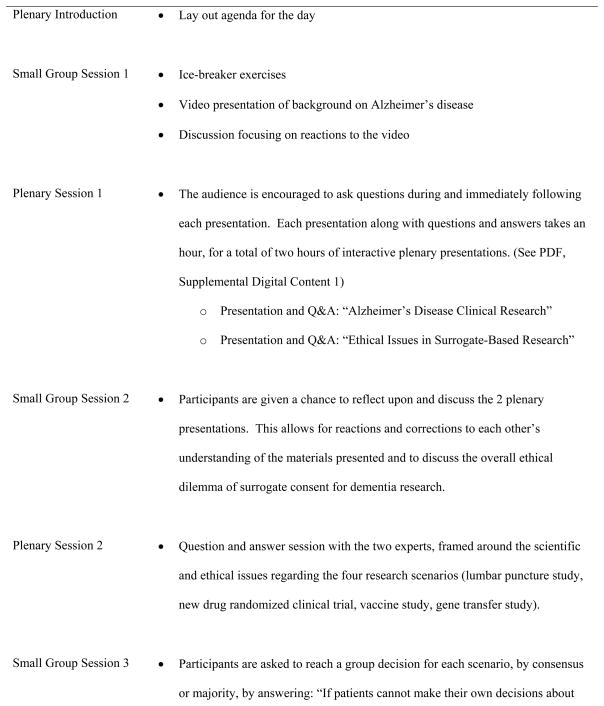
On the day of the DD session, the attendees were randomly assigned in groups of 5–7 persons per table. There were 27 tables (in two cohorts); each table was led by a trained facilitator.(16) Participants were informed that the group discussions at each table would be recorded. The procedures for the day are outlined in Figure 1.
Figure 1. Sequence and content of the DD session daya.
aTo maintain balanced expert responses to all questions, the two experts (AD clinical researcher and bioethicist) are available and travel together from table to table to answer questions throughout the day. Breaks and meal times are not shown.
The deliberative session involved three small group sessions. The first small group session was primarily designed to “warm up” the group to the process of group discussion, including an ice breaker exercise and general reactions to an informational video on Alzheimer’s disease (AD). That small group session was not analyzed for this paper.
The second small group session immediately followed an extensive educational session by experts in AD clinical research and in research ethics (see PDF, Supplemental Digital Content 1). During this session, the participants were asked to engage in general discussion about the presentations and also about the ethical dilemma of involving decisionally impaired dementia patients in clinical research.
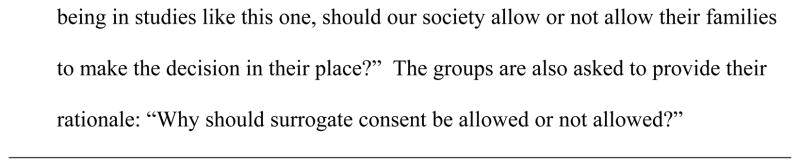
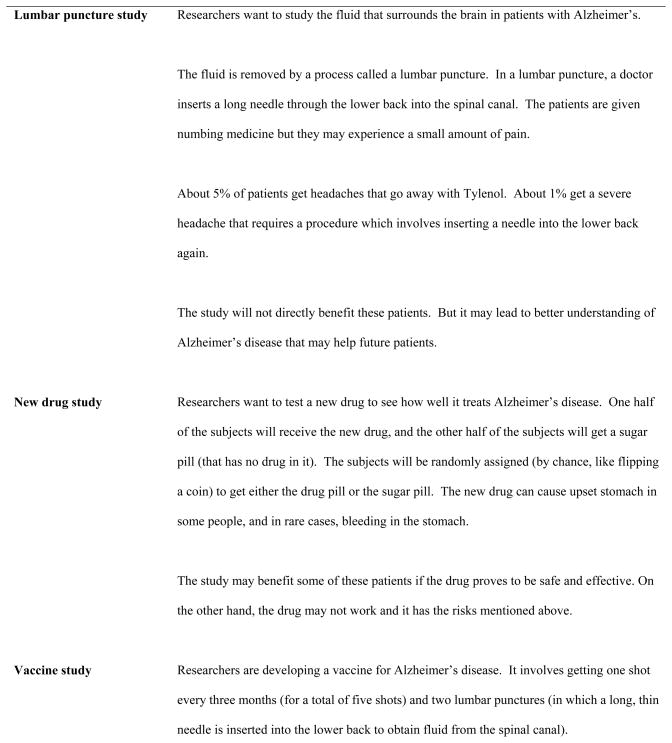
In the third small group session, participants were asked to evaluate four research scenarios: a study requiring a lumbar puncture, a clinical trial of a new drug, a vaccine study, and a study requiring the insertion of genetic material directly into the brain of a subject (see Figure 2).
Figure 2.
Four Alzheimer disease clinical research scenarios discussed during deliberation.
Participants were to provide recommendations regarding whether our society should have a policy of family surrogate consent for studies such as the ones described, and to reach a group decision, by consensus or majority. The participants were also asked to provide rationales for their recommendations.
Analyses
All group discussion recordings were transcribed. Twelve group transcriptions were selected to be coded: six were randomly chosen from the groups that agreed by majority or unanimous vote – that society should allow surrogate consent for all four scenarios (n=18), and six were randomly chosen from groups where there was at least one research scenario (by consensus or majority) for which the group would not allow surrogate consent (n=8) or where there was a tie vote (n=1).
To examine the substance of group conversations we developed a coding scheme using a systematic and iterative method common to qualitative analysis,(24) building on codes used in a previous study and identifying new codes relevant to this study.(25) Coding was conducted by two team members independently using NVivo qualitative software. Prior to analysis, coding discrepancies were discussed and resolved by three team members (AS, RdV, KR). Theme saturation was reached after coding transcripts of 9 of the 12 groups and our analysis is based on these 9 groups’ transcripts. These 9 groups were fairly evenly split between groups that would allow surrogate consent for all 4 scenarios (n=5) versus those who would not allow surrogate consent in at least one scenario (n=4). After coding was completed, each group’s transcript was systematically reviewed for the most commonly occurring themes and relevant quotes were identified.
RESULTS
Small Group Deliberation: General Discussion about Surrogate Consent
There was a striking pattern to the participant discussions during small group session 2, which focused on general issues related to surrogate consent. Although they learned through the expert presentations that few people complete research advance directives, participants nevertheless found such directives attractive, and discussed ways to improve their use. However, this discussion also inevitably included the limitations of advance directives. The discussions on advance directives generally led to the conclusion that such directives could not by themselves solve the ethical dilemma of involving incapacitated persons in dementia research.
Improving Advance Directives
Participants discussed several ways to increase the use of advance directives. Some suggested encouraging individuals to complete advance directives as soon as they were diagnosed with dementia: “I keep coming back to the advanced directive. What if every person who is early … diagnosed with early Alzheimer’s …What if they are immediately asked if they would consent?” (F45—participants are identified by gender and ID number). Other participants suggested that public awareness for the need for research advance directives could be raised through education: “It has to be education. It has to be lobbying efforts after the education. Most people aren’t going to react unless it personally happens to them.” (F50) Many participants suggested that research advance directives could be incorporated into other documents such as living wills, heath care durable powers of attorney, or even driver’s licenses.
Limitations of Advance Directives
Despite the attractiveness of advance directives, the participants recognized that education and other efforts to increase their use may not be sufficient. One participant pointed out a number of reasons why she (despite being at risk for dementia) and many others fail to complete advance directives:
F15: The reason the numbers are so low is because human beings by nature do not wish to think about our end times. I mean I have both parents gone from two different dementias. I don’t have it yet. I’ve thought about it. Right now, I don’t have the money to get it done. It has to be done with an attorney. I have to pick competent people.
Others pointed out the difficulty of anticipating the future when completing advance directives—both the content of future research as well as knowing what one’s wishes might be in the future: “Sometimes peoples’ thoughts change with time, and with the amount of pain they’re in or whatever” (M27) and “You don’t know the content of a study that might not be done until twenty years later. How could you know the content?”(M49) Another participant compared it to signing a Do Not Resuscitate (DNR) order in advance: “We all think we’re going to do that when we get to the end of our life, but none of us really wants to die and we don’t know …We might change our mind at the last minute, you know?”(F48)
Participants also pointed out that relying on advance directives may have negative consequences for future research since few people complete them.
M63: If you limit it only to people who have advanced directives… there’s a great likelihood that we’re going to really limit the amount of research that can be done.
Challenges of Surrogate Consent
Having recognized the limitations of advance directives, there emerged a consensus that some form of surrogate consent is necessary:
F23: In order to advance knowledge about Alzheimer’s, by definition, surrogate consent has to happen. It has to happen.
F31: But if the answer is “no,” that surrogates can’t give consent, then there is no hope for ever getting anywhere. So the answer has to be in my mind, “yes.”
However, participants did not unquestioningly accept a policy of surrogate consent. Instead, they pointed out many challenges and potential abuses of such a policy. Participants were concerned about whether surrogates would be competent, knowledgeable, know the patient’s wishes, or have the patient’s best interests in mind.
M26: Do they really understand that I wanted to do that? How forceful or how open was I with that statement and that choice? Are they informed of the research study and what it entails?
M34: When you’re dealing with family members, not every family member may have that subject at heart. Do you know what I’m saying?…And a lot of them are just not smart enough… They’re not smart enough, educated enough, you know…
Many participants worried that surrogates may not have the best reasons for enrolling AD patients in research: “Would it be in the best interest of the person or is it monetary for them? Are they thinking of something else?” (F57)
It is clear that participants do not have unrealistic and rosy views of surrogate consent. They see the many challenges, even as they recognize that surrogate consent is necessary to move dementia research forward.
Safeguarding surrogate consent
Also, much like their discussion regarding advance directives, many participants went beyond a simple discussion of the pros and cons of surrogate consent, to seek solutions to improve and safeguard the process.
F44: So it seems as though we almost have no choice but to have some form of surrogate consent, and our challenge is … How do we make it work? How do we build protections for, you know, the Alzheimer’s victim … the patients …
Participants discussed potential policies that would mandate safeguards such as third party oversight or some sort of vetting process to evaluate the competence, intentions, and appropriateness of the surrogate.
M21: Let’s have some standards about who can and who can’t be a surrogate and for what reasons.
F30: Allowing surrogate consent with certain safeguards in place…such as the person who is the surrogate is assessed. You know, you can do interview assessments that will tell you, you know …Using diplomatic questions that will allow you to obtain information …as to whether the person really not only understands what they’re potentially saying “yes” to, but also whether they do have the best interest of the person at heart.
M63: I think policymakers should consider the competency of the surrogate making this decision. There should be some sort of a test, some sort of questionnaire…
Small Group Deliberation: Specific Research Scenarios
In small group session 3, participants were asked to evaluate four specific research scenarios of varying risks and benefit and to decide whether society should have a policy that allows surrogate consent for each scenario.
Lower risk scenarios
In the lumbar puncture and drug study scenarios, low risk was the most commonly cited criterion for voting to allow a policy of surrogate consent. However, risk was not the only deciding factor. Participants also emphasized as important considerations societal benefit and the necessity of research, potential individual benefit (drug study), the importance of patient assent, and the value of monitoring for adverse events.
Societal and individual benefit
The participants distinguished between societal and individual benefits, and saw both as considerations:
M34: I’d like to say one thing. Another reason why I say “allow” is because it says right here, “The study will not directly benefit the patient,” right? But what it will do … It will lead to better understanding …understanding of the disease itself.
F50: My way of looking at this is that it’s one step in the chain towards a cure.
The drug study scenario had the additional appeal of potential direct benefit to AD patients who may enroll in such studies:
F65: If a person does have Alzheimer’s and the drug actually is a positive drug and it works, the person doing the test will actually benefit from it.
F31: There is an additional reason. There’s a chance it might help.
Importance of assent/dissent
Another important issue for participants was the concept of assent: even if the surrogates give permission, if AD patients refuse to participate, they have the final word.
M21: As I understand it, if at any point in the process the patient says, “I don’t want to do that.” “I don’t want to do it any more,” or “I don’t want to do it,” to begin with, then the answer is already “no.” No matter what the surrogate says, if the patient says “no,” the answer is “no.”
For many participants understanding assent was critical to their approval of surrogate consent. One participant stated in a later higher risk scenario, that her appreciation of the concept of assent was her “lightbulb” moment, when she became comfortable with surrogate consent (F23).
Value of monitoring adverse effects
Some participants who voted to allow surrogate consent mentioned the importance of close monitoring of subjects in research studies:
F39: I know when I was in one study, I had to report morning and night and answer all these questions. You know, very specific questions. So it’s pretty well-monitored for safety reasons. So that’s another reason I would allow it.
Higher risk scenarios
For the vaccine and gene transfer studies, not unexpectedly, the issue of risk was highly salient for participants. When voting whether to allow surrogate consent in these studies, it often came down to whether the level of risk was sufficiently offset by potential benefits.
Risks not offset by benefits
For participants who opted not to allow surrogate consent in the higher risk scenarios, they felt that there were simply not sufficient benefits either to patients or to society to make up for the high risks.
F30: I feel that way from a societal point of view too because we can’t …. I mean each individual human life is important, and it has value… You still have to value the individual human life. Otherwise, you’re on that slippery slope where you start evaluating human life and you end up with things like the horror stories that he told us about.
F56: I just think the risk/benefit ratio is not good. The chance of it helping anybody is pretty low.
However, for some participants, their concern was mainly a deep discomfort with surgical intervention into the brain.
F24: …any time you put foreign material into the brain, you are risking all kinds of problems in my opinion.
F42: I would not allow this. This just seems like spooky old school, creepy, witch doctor-type surgery.
Benefits to patient or society
For participants who would allow surrogate consent, the higher risk was offset by potential benefits to patient or society.
M20: What it might be is the fact that this is the first step towards something really promising. This may not be the end-all cure, but if we try this and it looks like this is actually having an effect, maybe now we can focus more research on this. In the end, we’ll have a much huger positive impact.
F39: Yeah. Slightly helping …You know having someone be able to get dressed in the morning on their own can be huge for that person’s state of mind and for the people who care for that person…Who knows? Maybe they’re getting more improved, less side effects … You never know unless you allow somebody to make the choice to be a research patient.
Trust in the oversight system
During the session day, participants were presented with information about historical research abuses and current protections to prevent these abuses (see PDF, Supplemental Digital Content 1). We found that prior to the study, most participants had been unaware of the human subject protections system. The participants appealed to this new knowledge in supporting a policy of surrogate consent:
M36: That comes from pressures from society on how we behave. Like Tuskegee or any one of those experiments… There were a lot of things going on then that were acceptable that are not acceptable today… They’re just not tolerated.
F41: I guess I have faith in how it was described earlier in how it went through these different boards and getting the study approved. I mean I put a lot of faith in that system… there aren’t those Nazi doctors and some of those other things that we saw earlier. So, therefore, I have my confidence in that there aren’t going to be butchers out there cutting open peoples’ heads …
Trust in surrogates
Trust in surrogates was another salient theme for participants who voted to allow surrogate consent in the higher risk scenarios.
M17: I would allow it and, once again, placing your trust in the surrogate being someone who loves you, somebody who has your best interest at heart and …may know what you would have wanted.
F48: We can trust our surrogate, like you said, so whatever the test is, they will …They are the rational minds, and they’ll look it over and decide if this is something that they’re willing to put you through.
Societal versus individual perspective
Participants who voted to allow surrogate consent in the higher risk scenarios also moved beyond a simple risk/benefit calculation to articulate the distinction between societal policy and the individual choices of surrogates:
M36: By voting “nay” against surrogate empowerment, what you’re essentially doing is voting “no” on every other family. You’re putting yourself in a position of impacting every family who has an Alzheimer’s patient. On the other hand, by giving the surrogate power in all cases, then it becomes a singular family issue, or a singular person issue.
DISCUSSION
Several studies have shown that there is considerable layperson support for allowing surrogate consent for dementia research.(12–14, 26) Among our participants, we found that the older general public strongly supports a policy of surrogate consent for dementia research and that this support increased after in-depth education and peer deliberation; for example, at baseline, support for a policy of surrogate consent for a dementia research protocol involving gene transfer neurosurgery increased from 56% to 68% after deliberation.(22) Our thematic analysis of participants’ deliberations provides important insights into what this overall support means.
The attitude reflected in the deliberations can best be described as “cautious pragmatism.” The participants reasoned their way through the complex ethical issues, aware of both the pros and cons of policy options, while maintaining their focus on practical solutions. They were strongly attracted by the potential of advance directives and tried to remedy their inherent shortcomings. These ideas included not only the expected “public campaign” type solutions but also the idea of obtaining a directive very early on in the course of dementia, which has recently become a focus of discussion.(27)
The participants’ acceptance of the need for surrogate consent for dementia research was not an unthinking or idealized endorsement. They clearly recognized the potential pitfalls of such a policy and focused on providing practical safeguards. Their approach was, in effect, “trust but verify”—surrogate consent implies a trust in the surrogates to do the right thing, but procedures should be in place that maximize the likelihood that they can do the job of a surrogate. For example, the idea of conducting a screening interview, or even a capacity assessment, of the potential surrogates may in fact be justifiable (especially for high risk studies) on the grounds that although most adults when acting on their own behalf may deserve the presumption of capacity, when they are acting on behalf of others for decisions that are not inherently in their interest, the weight of that presumption can be less.
In their deliberation over specific research scenarios, we found that the participants, not surprisingly, weighed potential benefits against the risks of harm inherent in research protocols. But the details of their deliberations reveal that the participants were able to incorporate new materials into their reasoning process. They were able to distinguish between societal and individual benefits, use concrete examples of how research monitoring works, use the idea that a person might be incompetent to provide informed consent and yet be able to express meaningful preferences through assent or dissent, and understand that historical abuses have led to an extensive research oversight system. They also evaluated the implications of policy, e.g., they recognized that a policy that disallows surrogate consent is “essentially… voting ‘no’” for all families whereas a policy which allows it makes research participation “a singular family or a singular person issue.”
There are, however, important limitations to our analysis. First, the DD sessions require a considerable time commitment and there is likely unavoidable self-selection. For example, the high level of trust that most participants showed in the human subject protections system may reflect the fact that people who are willing to attend DD sessions are more likely to engage with “the system.” Second, we used only 9 of the 27 transcripts for our qualitative analysis, allowing for the possibility that these were not representative of all session participants. However, after coding seven groups, we were not uncovering new codes, and coding of an additional two groups confirmed saturation. Third, we stratified our coding to have an over-representation of groups that had voted against allowing surrogate consent for at least one research scenario, and this may have led to under-representation of pro-research viewpoints.
Despite these limitations, the results of our analysis are clear. It is possible to elicit highly informed and reasoned public opinions regarding the ethics of surrogate consent for dementia research and these opinions can inform the creation of policy. The public’s generally positive view of surrogate consent should not, however, be taken as unalloyed, idealistic trust in science. Rather, the public appears willing to support a policy of surrogate consent, all the while recognizing the potential pitfalls of entrusting the scientific process (which includes an oversight mechanism) and future surrogates to do the right thing. This trust, based on a cautious pragmatism, will likely be dynamic, open to fluctuations that depend on how responsibly our society manages the involvement of vulnerable, incapacitated subjects in research.
Supplementary Material
Acknowledgments
Supported by NIH R01AG029550 and the Greenwall Foundation Faculty Scholars Award in Bioethics.
Footnotes
Disclosures:
Dr. De Vries is funded by NIA grant 1 RO1 AG029550.
Kerry Ryan reports no competing interests.
Aimee Stanczyk reports no competing interests.
Dr. Appelbaum receives royalties from the publication of Professional Manual, The MacArthur Competence Assessment Tool for Clinical Research (MacCAT-CR); Assessing Competence To Consent To Treatment: A Guide for Physicians and Other Health Professionals; and Informed Consent: Legal Theory and Clinical Practice, 2nd ed. He is funded by NIA grants 1 RO1 AG029550 (4/01/2008-06/30/2011) and 1 RO1 AG027986 (9/1/2007-6/30/2011); NCI grant 1 R01 CA107295 (07/01/06-06/30/11); NCRR grant 1 UL1 RR024156-01 (09/30/06-06/30/16); NINR grant 1RC1 NR011612-01 (09/28/09-07/31/11); NHGRI grant 1P20HG005535-01 (04/01/10-03/31/13); and the Robert Wood Johnson Foundation Program on Public Health and Law (03/31/11-5/31/12); and was recently funded by NIMH grant R01 MH075023 (3/1/2008-8/31/2010). He holds an equity interest in COVR, Inc. (violence risk prediction software).
Laura Damschroder received travel reimbursement and honorarium for plenary talk at the Robert Wood Johnson Foundation; was recently funded by NIA grant 1 RO1 AG029550.
Dr. Knopman serves on a Data Safety Monitoring Board for Lilly Pharmaceuticals, and is an investigator for clinical trials sponsored by Elan Pharmaceuticals, Forest Pharmaceuticals and Baxter Healthcare. He is deputy editor of Neurology, and receives compensation for editorial activities.
Dr. Scott Kim receives royalties from the publication of the book Evaluation of Capacity to Consent to Treatment and Research; is funded by NIMH grant R01-MH075023 (09/01/2005 – 08/31/2010), NIA grant R01-AG029550 (09/15/2007-06/30/2011) and R01 AG028827 (09/01/2006 – 06/30/2009), and the Greenwall Foundation (07/01/2006 – 06/30/2009).
References
- 1.Kim SYH, Caine ED, Currier GW, et al. Assessing the competence of persons with Alzheimer’s disease in providing informed consent for participation in research. Am J Psychiatry. 2001;158:712–717. doi: 10.1176/appi.ajp.158.5.712. [DOI] [PubMed] [Google Scholar]
- 2.Okonkwo O, Griffith HR, Belue K, et al. Medical decision-making capacity in patients with mild cognitive impairment. Neurology. 2007;69:1528–1535. doi: 10.1212/01.wnl.0000277639.90611.d9. [DOI] [PubMed] [Google Scholar]
- 3.Orgogozo JM, Gilman S, Dartigues JF, et al. Subacute meningoencephalitis in a subset of patients with AD after Abeta42 immunization. Neurology. 2003;61:46–54. doi: 10.1212/01.wnl.0000073623.84147.a8. [DOI] [PubMed] [Google Scholar]
- 4.Tuszynski MH, Thal L, Pay M, et al. A phase 1 clinical trial of nerve growth factor gene therapy for Alzheimer disease. Nat Med. 2005;11:551–555. doi: 10.1038/nm1239. [DOI] [PubMed] [Google Scholar]
- 5.Kolata G. The New York Times. Aug 18, 2010. Doubt on tactic in Alzheimer’s battle; p. A14. [Google Scholar]
- 6.Saks ER, Dunn LB, Wimer J, et al. Proxy consent to research: the legal landscape. Yale J Health Policy Law Ethics. 2008;8:37–92. [PubMed] [Google Scholar]
- 7.Cahill M, Wichman A. Research involving persons with cognitive impairments: Results of a survey of Alzheimer disease research centers in the United States. Alzheimer Dis Assoc Disord. 2000;14:20–27. doi: 10.1097/00002093-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Karlawish JHT, Knopman D, Clark CM, et al. Informed consent for Alzheimer’s disease clinical trials: a survey of clinical investigators. IRB. 2002;24:1–5. [PubMed] [Google Scholar]
- 9.Gong MN, Winkel G, Rhodes R, et al. Surrogate consent for research involving adults with impaired decision making: survey of Institutional Review Board practices. Crit Care Med. 2010;38:2146–2154. doi: 10.1097/CCM.0b013e3181f26fe6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bravo G, Dubois MF, Wildeman SM, et al. Research with decisionally incapacitated older adults: practices of Canadian research ethics boards. IRB. 2010;32:1–8. [PubMed] [Google Scholar]
- 11.Black BS, Rabins PV, Sugarman J, et al. Seeking assent and respecting dissent in dementia research. Am J Geriatr Psychiatry. 2010;18:77–85. doi: 10.1097/JGP.0b013e3181bd1de2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wendler D, Martinez RA, Fairclough D, et al. Views of potential subjects toward proposed regulations for clinical research with adults unable to consent. Am J Psychiatry. 2002;159:585–591. doi: 10.1176/appi.ajp.159.4.585. [DOI] [PubMed] [Google Scholar]
- 13.Kim SYH, Kim HM, McCallum C, et al. What do people at risk for Alzheimer’s disease think about surrogate consent for research? Neurology. 2005;65:1395–1401. doi: 10.1212/01.wnl.0000183144.61428.73. [DOI] [PubMed] [Google Scholar]
- 14.Karlawish J, Rubright J, Casarett D, et al. Older adults’ attitudes toward enrollment of non-competent subjects participating in Alzheimer’s research. Am J Psychiatry. 2009;166:182–188. doi: 10.1176/appi.ajp.2008.08050645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim SY, Kim HM, Langa KM, et al. Surrogate consent for dementia research: a national survey of older Americans. Neurology. 2009;72:149–155. doi: 10.1212/01.wnl.0000339039.18931.a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim S, Wall I, Stanczyk A, et al. Assessing the public’s views in research ethics controversies: deliberative democracy and bioethics as natural allies. J Empir Res Hum Res Ethics. 2009;4:3–16. doi: 10.1525/jer.2009.4.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fishkin JS. The voice of the people. New Haven, CT: Yale Univ Press; 1997. [Google Scholar]
- 18.Freeman S. Deliberative democracy: a sympathetic comment. Philosophy & Public Affairs. 2000;29:371–419. [Google Scholar]
- 19.Mitton C, Smith N, Peacock S, et al. Public participation in health care priority setting: A scoping review. Health Policy. 2009;91:219–228. doi: 10.1016/j.healthpol.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 20.US Congress: American Recovery and Reinvestment Act. Washington: GPO; 2009. [Google Scholar]
- 21.Presidential Commission for the Study of Bioethical Issues: New Directions: The Ethics of Synthetic Biology and Emerging Technologies. Final Report. 2010 Retrieved from http://www.bioethics.gov/
- 22.Kim SYH, Kim HM, Knopman DS, et al. Effect of public deliberation on attitudes toward surrogate consent for dementia research. Neurology. doi: 10.1212/WNL.0b013e31823648cb. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Vries R, Stanczyk AE, Ryan KA, et al. A framework for assessing the quality of democratic deliberation: Enhancing deliberation as a tool for bioethics. J Empir Res Hum Res Ethics. doi: 10.1525/jer.2011.6.3.3. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bourgeault I, Dingwall R, De Vries R, editors. Qualitative Methods in Health Research. Thousand Oaks, CA: Sage; 2010. Section C: Collecting and analyzing data; pp. 287–555. [Google Scholar]
- 25.De Vries R, Stanczyk A, Wall IF, et al. Assessing the quality of democratic deliberation: A case study of public deliberation on the ethics of surrogate consent for research. Soc Sci Med. 2010;70:1896–1903. doi: 10.1016/j.socscimed.2010.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim SYH, Uhlmann RA, Appelbaum PS, et al. Deliberative assessment of surrogate consent in dementia research. Alzheimers Dement. 2010;6:342–350. doi: 10.1016/j.jalz.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim S, Karlawish J, Kim H, et al. Preservation of the capacity to appoint a proxy decision maker: implications for dementia research. Arch Gen Psychiatry. 2011;68:214–220. doi: 10.1001/archgenpsychiatry.2010.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.