Abstract
Plasmodium vivax is causing increasingly more cases of severe malaria worldwide. Among 25 cases in India during 2010–2011, associated conditions were renal failure, thrombocytopenia, jaundice, severe anemia, acute respiratory distress syndrome, shock, cerebral malaria, hypoglycemia, and death. Further studies are needed to determine why P. vivax malaria is becoming more severe.
Keywords: Plasmodium vivax, acute kidney injury, hemodialysis, malaria, parasites, India
India is a major contributor to the worldwide distribution of Plasmodium vivax malaria (1). Severe and complicated malaria is usually caused by the P. falciparum parasite, but P. vivax, usually considered a benign parasite that causes disease resulting in low case-fatality rates, can also occasionally cause severe disease. Reported severe manifestations of P. vivax include cerebral malaria, liver dysfunction, acute kidney injury, severe anemia, acute respiratory distress syndrome, shock, abnormal bleeding, and multiple organ failure (2–10). The mechanism of P. vivax–associated acute kidney injury and its effective management remain unclear. In addition, little information is found in the literature to explain the recent increase in incidence of acute kidney injury and the shift toward multiple complications, specifically in India (11). This scarcity of data prompted us to review cases at the Institute of Kidney Diseases and Research Centre–Institute of Transplantation Sciences, Civil Hospital, Ahmedabad, India.
The Study
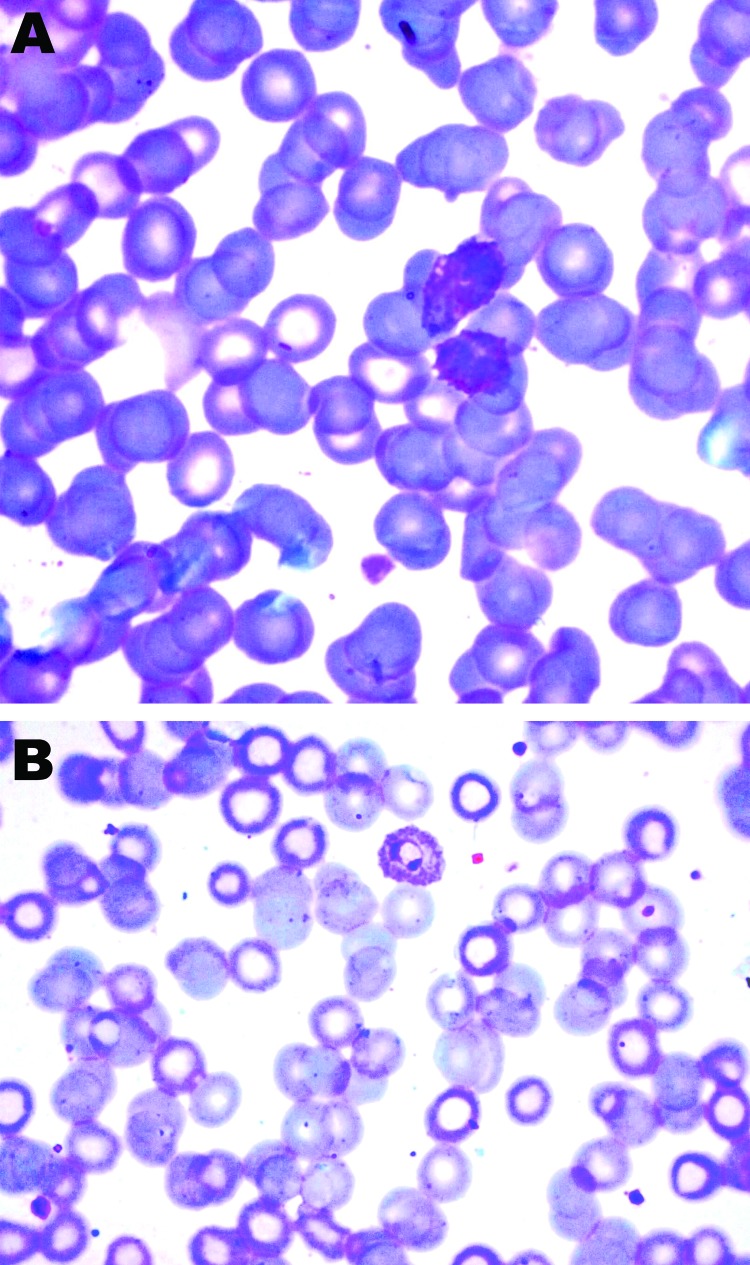
We conducted a prospective study during 2010–2011 to describe clinical characteristics, laboratory parameters, prognostic factors, and outcomes for 25 Civil Hospital patients who required hemodialysis for acute kidney injury associated with P. vivax monoinfection. P. vivax monoinfection was diagnosed by direct visualization of the parasite in Giemsa-stained peripheral blood films (Figure 1) and rapid diagnostic test results (negative for histidine-rich protein 2 of P. falciparum and positive for P. vivax–specific lactate dehydrogenase). The severity of illness was assessed by using the Acute Physiology and Chronic Health Evaluation (APACHE II), Sequential Organ Failure Assessment (SOFA), Multiple Organ Dysfunction Score (MODS), and Glasgow Coma Scale. Smear evaluation included reading 200–500 fields with the oil immersion objective lens for >20 minutes by an expert. If the initial smear examination was negative for P. falciparum, additional smears were reviewed within 6–24 hours to rule out mixed infection. Patients with other concurrent illness or P. falciparum mixed infections were excluded from the study. After a diagnosis was established and treatment was initiated, the parasitologic response was monitored. Other causes of acute kidney injury, fever, and jaundice (i.e., dengue viral infection, leptospirosis, sepsis, typhus, enteric fever, and viral hepatitis and drug reactions) were excluded by history and relevant investigations.
Figure 1.
Schizonts (A) and ring form (B) of Plasmodium vivax, Ahmedabad, India, 2010–2011. Original magnification ×1,000.
Acute kidney injury was defined as serum creatinine >3 mg/dL and urine output <400 mL/24 hours with normal kidney size according to ultrasonography. The patients were treated with antimalarial drugs (artesunate and doxycycline [n = 25], quinine [n = 2]); fluid replacement and supportive measures were instituted as needed. Intravenous ceftriaxone was given initially until a bacterial infection (e.g., Salmonella infection) was excluded. Renal replacement therapy was initiated before overt symptoms and signs of acute kidney injury developed (10,11). Hemodialysis was initiated for fluid overload, hyperkalemia, clinical evidence of uremia, metabolic acidosis, blood urea nitrogen >100 mg/dL, and creatinine >4–5 mg/dL or rapidly increasing. Intermittent hemodialysis (n = 24) was provided on alternate days through a temporary dialysis catheter, and continuous renal replacement therapy was provided for 1 hemodynamically unstable patient. Renal replacement therapy continued until the patient’s kidney function improved (increase in urine output or progressive decline in creatinine).
Blood transfusion was reserved for patients with hemoglobin <7 g/dL. Exchange transfusion was performed for patients with parasite density >10%, end-stage organ failure complications, and serum bilirubin >25 mg/dL. Renal biopsy was performed when oliguria, heavy proteinuria, or hematuria persisted for >3 weeks.
Of the 202 malaria patients in whom acute kidney injury was treated, 177 (87.7%) cases of total malaria with acute kidney injury were caused by P. falciparum and 25 (12.3%) by P. vivax. Baseline characteristics of the study patients are shown in Table 1. Comparison of patients who survived or died is shown in Table 2. Initial clinical features were fever (100%), nausea or vomiting (84%), oliguria (60%), abdominal pain or tenderness (40%), jaundice (40%), dyspnea (32%), diarrhea (12%), altered sensorium (4%), and convulsions (4%). The time between onset of symptoms and admission to the hospital for acute kidney injury was 7–15 days (median 11 days). At admission, cultures of blood, sputum, and urine were negative for microorganisms for all patients. The following complications were observed: renal failure (100%), thrombocytopenia (64%), thrombocytopenia <50,000 cells/μL (40%), hyponatremia (52%) (usually asymptomatic), jaundice (bilirubin >3 mg/dL) (40%), severe anemia (hemoglobin <7 gm/dL) (40%), acute respiratory distress syndrome (16%), shock (12%), cerebral malaria (4%), hypoglycemia (4%), and death (12%).
Table 1. Baseline values for 25 Plasmodium vivax patients with acute kidney injury, Ahmedabad, India, 2010–2011*.
| Characteristic | Value |
|---|---|
| Age, y | 30.1 ± 12.3 |
| Hypotension not resolving after receipt of fluid, no. (%) | 3 (12) |
| Mechanical ventilation, no. (%) | 4 (16) |
| Lactate dehydrogenase, U/L | 1267 ± 462 |
| APACHE 2 score | 17.4 ± 3.8 (9–27) |
| SOFA score | 8.4 ± 2.8 (4–14) |
| MODS score | 7.9 ± 2.8 (4–14) |
| GCS score | 14.3 ± 1.14 (12–15) |
| Hemoglobin, gm/L | 8.02 ± 1.6 |
| Hematocrit, % | 24.6 ± 4.9 |
| Leukocytes, cells/mm3 | 9,002.8 ± 3,098 |
| Platelets, cells/μL | 108,680 ± 91,606 |
| Total bilirubin, mg/dL | 5.6 ± 7.6 |
| Direct bilirubin, mg/dL | 4.1 ± 6.2 |
| Indirect bilirubin, mg/dL | 1.5 ± 2.1 |
| Alanine aminotransferase, U/L | 66 ± 45.5 |
| Sodium, mmol/L | 130 ± 6.8 |
| Creatinine, mg/dL | 7.37 ± 2.6 |
| Blood urea, mg/dL | 140.4 ± 59 |
| No. hemodialysis sessions | 5.1 ± 3.5 |
*Values are mean ± SD (range) except as indicated. APACHE, Acute Physiology and Chronic Health Evaluation; SOFA, Sequential Organ Failure Assessment; MODS, Multiple Organ Dysfunction Score; GCS, Glasgow Coma Scale.
Table 2. Comparison of 25 Plasmodium vivax patients with acute kidney injury, Ahmedabad, India, 2010–2011*.
| Characteristic | Survived, n = 22 | Died, n = 3 | p value |
|---|---|---|---|
| Age, y | 27.7 ± 9.9 | 47.3 ± 17.5 | 0.058 |
| Hypotension not resolving after receipt of fluid, no. (%) | 0 | 3 (100) | 0.0001 |
| Mechanical ventilation, no. (%) | 1 (4.5) | 3 (100) | 0.0001 |
| Lactate dehydrogenase, U/L | 1126.3 ± 243.2 | 2300 ± 360.5 | 0.001 |
| APACHE 2 score | 16.4 ± 2.61 (9–23) | 25.3 ± 1.52 (24–27) | 0.001 |
| SOFA score | 7.73 ± 2.3 (4–11) | 13.3 ± 1.15 (12–14) | 0.001 |
| MODS score | 7.23 ± 2.26 (4–10) | 13 ± 1.0 (12–14) | 0.001 |
| GCS score | 14.5 ± 1.01 (12–15) | 12.3 ± 0.57 (12–13) | 0.013 |
| Hemoglobin, gm/L | 8.0 ± 1.71 | 8.13 ± 0.70 | 0.96 |
| Hematocrit, % | 24.5 ± 5.2 | 25.6 ± 2.3 | 0.78 |
| Leuckocytes, cells/mm3 | 9,175.9 ± 3,110 | 7,733.3 ± 3,300 | 0.49 |
| Platelets, cells/μL | 113,409 ± 96,618 | 74,000 ± 2,5159 | 0.90 |
| Total bilirubin, mg/dL | 6.1 ± 8 | 2.56 ± 0.75 | 0.72 |
| Direct bilirubin, mg/dL | 4.46 ± 6.58 | 1.76 ± 0.40 | 0.60 |
| Indirect bilirubin, mg/dL | 1.64 ± 2.23 | 0.80 ± 0.34 | 0.90 |
| Alanine aminotransferase, U/L | 66.9 ± 47.8 | 59.3 ± 29.1 | 0.96 |
| Sodium, mmol/L | 130.5 ± 7.17 | 126.6 ± 2.3 | 0.23 |
| Creatinine, mg/dL | 7.36 ± 2.7 | 7.5 ± 2.17 | 0.66 |
| Blood urea, mg/dL | 147.7 ± 57.5 | 87 ± 48.8 | 0.08 |
| No. hemodialysis sessions | 5.3 ± 3.7 | 3.33 ± 1.15 | 0.23 |
*Values are mean ± SD (range) except as indicated. APACHE, Acute Physiology and Chronic Health Evaluation; SOFA ,Sequential Organ Failure Assessment; MODS, Multiple Organ Dysfunction Score; GCS, Glasgow Coma Scale.
Urinalysis showed muddy brown granular casts or epithelial cell casts; trace protein; and absence of dysmorphic red cells, heavy protein, and leukocytes. None of the patients were deficient in glucose 6-phosphate dehydrogenase activity in erythrocytes. The mean APACHE II, SOFA, MODS, and Glasgow Coma scores were higher for patients who died than those who survived (Table 2). SOFA and MODS scores <12 were associated with a low mortality rate (22 patients, 0 deaths), whereas scores >12 indicated a worse outcome (3 patients, 3 deaths). APACHE II score <24 was associated with a low mortality rate (22 patients, 0 deaths), whereas score >24 indicated a worse outcome (3 patients, 3 deaths) (p<0.008).
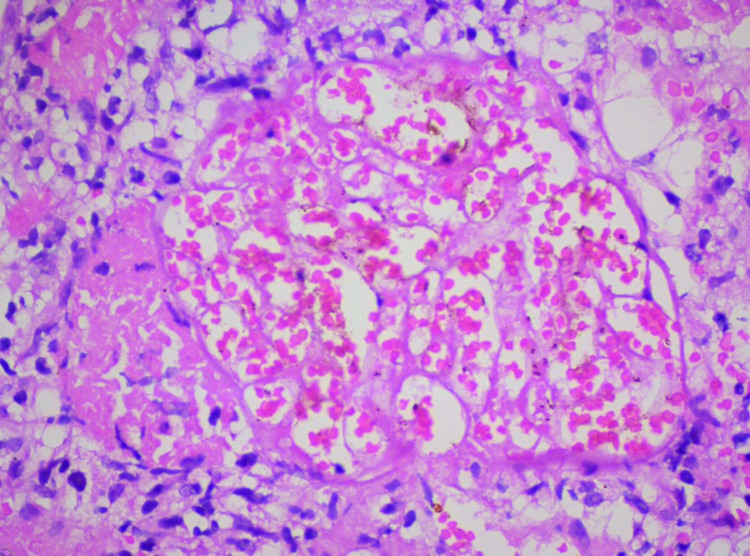
Cerebral malaria occurred in 1 patient, who died. Blood component transfusion was given to 7 (28%) patients. Exchange transfusion was given to 1 (4%), who survived. For all patients, initial rehydration failed to lead to renal recovery. Most patients no longer needed dialysis after 2 weeks, and renal function returned in 3 weeks. Renal biopsies, performed for 4 patients, detected patchy cortical necrosis in 3 (Figure 2) and acute tubular necrosis in 1. A total of 19 (76%) patients completely recovered with normal renal function (creatinine <1.4 mg/dL [reference 0.7–1.4 mg/dL]), 3 (12%) did not recover completely (creatinine 1.5–3 mg/dL) and continued to receive conservative treatment, and 3 (12%) died. Factors related to acute kidney injury were heavy parasitemia (48%), hyperbilirubinemia (40%), volume depletion (40%), intravascular hemolysis (100%), and sepsis (12%).
Figure 2.
Renal biopsy sample showing patchy cortical necrosis, hematoxylin and eosin staining, Ahmedabad, India, 2010–2011 Original magnification ×400.
Conclusions
Our study highlights the possibility that P. vivax can cause acute kidney injury. There is no direct pathogenic linkage between P. vivax and acute kidney injury. Hence, despite the association, cause-and-effect relationships remain doubtful. However, the following can contribute to acute kidney injury: heavy parasitemia, volume depletion, hyperbilirubinemia, intravascular hemolysis, renal ischemia, sepsis, disseminated intravascular coagulation, cytoadherence to endothelial cells, and microvascular sequestration (2,10,11,12,13). Bilirubin and hemoglobin were useful for predicting P. vivax–induced nephropathy (9). Because co-infection with P. vivax and P. falciparum protects patients from severe malaria, mixed infection is unlikely in patients with severe malaria (2,9,14).
In our study, APACHE II score >24 and SOFA and MODS scores >12 were associated with higher mortality rates. These scores can be used for prognosis for patients with malaria and acute kidney injury and can help us better categorize patients for better management and improved outcomes. One limitation of our study is that PCR confirming P. vivax monoinfection was not performed routinely.
Acute cortical necrosis is rare in patients with acute kidney injury from malaria (15). The possible pathogenic factors are renal damage through renal hypoperfusion or endothelial injury through release of various circulating substances (intravascular hemolysis and sepsis). P. vivax should be suspected in patients with acute kidney injury who have prolonged oligoanuria. P. vivax can lead to serious, potentially life-threatening complications, such as acute kidney injury. Further studies are needed to determine why P. vivax infections are becoming more severe.
Biography
Dr Kute is an assistant professor at the Institute of Kidney Diseases and Research Center and the Dr H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India. His research interests include acute kidney injury in tropical diseases and diabetic nephropathy.
Footnotes
Suggested citation for this article: Kute VB, Trivedi HL, Vanikar AV, Shah PR, Gumber MR, Patel HV, et al. Plasmodium vivax malaria–associated acute kidney injury, India, 2010–2011. Emerg Infect Dis [serial on the Internet]. May 2012 [date cited]. http://dx.doi.org/10.3201/eid1805.111442
References
- 1.Joshi H, Prajapati SK, Verma A, Kang’a S, Carlton JM. Plasmodium vivax in India [review]. Trends Parasitol. 2008;24:228–35. 10.1016/j.pt.2008.01.007 [DOI] [PubMed] [Google Scholar]
- 2.Anstey NM, Russell B, Yeo TW, Price RN. The pathophysiology of vivax malaria. Trends Parasitol. 2009;25:220–7. 10.1016/j.pt.2009.02.003 [DOI] [PubMed] [Google Scholar]
- 3.Kochar DK, Saxena V, Singh N, Kochar SK, Kumar SV, Das A. Plasmodium vivax malaria. Emerg Infect Dis. 2005;11:132. 10.3201/eid1101.040519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kochar DK, Das A, Kochar SK, Saxena V, Sirohi P, Garg S, et al. Severe Plasmodium vivax malaria: a report on serial cases from Bikaner in northwestern India. Am J Trop Med Hyg. 2009;80:194–8. [PubMed] [Google Scholar]
- 5.Kochar DK, Singh P, Agarwal P, Kochar SK, Pokharna R, Sareen PK. Malarial hepatitis. J Assoc Physicians India. 2003;51:1069–72. [PubMed] [Google Scholar]
- 6.Singh H, Parakh A, Basu S, Rath B. Plasmodium vivax malaria: is it actually benign? J Infect Public Health. 2011;4:91–5. 10.1016/j.jiph.2011.03.002 [DOI] [PubMed] [Google Scholar]
- 7.Sonkar SK, Uniyal R, Sonkar GK. Three unusual presentations of Plasmodium vivax malaria. Trop Doct. 2011;41:240–1. 10.1258/td.2011.110220 [DOI] [PubMed] [Google Scholar]
- 8.Choi HJ, Lee SY, Yang H, Bang JK. Retinal haemorrhage in vivax malaria. Trans R Soc Trop Med Hyg. 2004;98:387–9. 10.1016/j.trstmh.2003.12.002 [DOI] [PubMed] [Google Scholar]
- 9.Chung BH, Lee SW, Lee SE, Hwang TJ, Shin HS. Predictors of Plasmodium vivax malaria–induced nephropathy in young Korean men. Nephron Clin Pract. 2008;110:c172–7. 10.1159/000167023 [DOI] [PubMed] [Google Scholar]
- 10.Prakash J, Singh AK, Kumar NS, Saxena RK. Acute renal failure in Plasmodium vivax malaria. J Assoc Physicians India. 2003;51:265–7. [PubMed] [Google Scholar]
- 11.Das BS. Renal failure in malaria. J Vector Borne Dis. 2008;45:83–97. [PubMed] [Google Scholar]
- 12.Jha V, Chugh KS. Acute kidney injury in malaria. In: Ronco C, Bellomo R, Kellum J, editors. Critical care nephrology. 2nd ed. Philadelphia (PA): Saunders Elsevier; 2009. p. 850–5. [Google Scholar]
- 13.Carvalho BO, Lopes SC, Nogueira PA, Orlandi PP, Bargieri DY, Blanco YC, et al. On the cytoadhesion of Plasmodium vivax–infected erythrocytes. J Infect Dis. 2010;202:638–47. 10.1086/654815 [DOI] [PubMed] [Google Scholar]
- 14.Luxemburger C, Ricci F, Raimond D, Bathet S, White NJ. The epidemiology of severe malaria in an area of low transmission in Thailand. Trans R Soc Trop Med Hyg. 1997;91:256–62. 10.1016/S0035-9203(97)90066-3 [DOI] [PubMed] [Google Scholar]
- 15.Chugh KS, Jha V, Sakhuja V, Joshi K. Acute renal cortical necrosis—a study of 113 patients. Ren Fail. 1994;16:37–47. 10.3109/08860229409044846 [DOI] [PubMed] [Google Scholar]