Abstract
Overweight and obese patients with osteoarthritis (OA) experience more OA pain and disability than patients who are not overweight. This study examined the long-term efficacy of a combined pain coping skills training (PCST) and lifestyle behavioral weight management (BWM) intervention in overweight and obese OA patients. Patients (N=232) were randomized to a 6-month program of: 1) PCST + BWM; 2) PCST-only; 3) BWM-only; or 4) standard care control. Assessments of pain, physical disability (Arthritis Impact Measurement Scales [AIMS] physical disability, stiffness, activity, and gait), psychological disability (AIMS psychological disability, pain catastrophizing, arthritis self-efficacy, weight self-efficacy), and body weight were collected at four time points (pretreatment, post-treatment, and 6 months and 12 months after the completion of treatment). Patients randomized to PCST+ BWM demonstrated significantly better treatment outcomes (average of all three post-treatment values) in terms of pain, physical disability, stiffness, activity, weight self-efficacy, and weight when compared to the other three conditions (p’s <.05). PCST+BWM also did significantly better than at least one of the other conditions (i.e., PCST-only, BWM-only, or standard care) in terms of psychological disability, pain catastrophizing, and arthritis self-efficacy. Interventions teaching overweight and obese OA patients pain coping skills and weight management simultaneously may provide the more comprehensive long-term benefits.
Keywords: osteoarthritis, pain, coping, physical disability, overweight, obese
Pain is the key concern for the greater than 27 million US adults suffering from osteoarthritis (OA) [21; 16; 29]. Being overweight or obese is associated with a 4- to 5- fold increased risk of knee OA [2], OA pain severity, and OA disability [35; 47; 19; 51]. Overweight and obese OA patients are advised to lose weight to reduce pain and disability [52; 31]. However, OA pain can interfere with successful weight loss behaviors (i.e., increasing physical activity, reducing caloric consumption) [40; 4; 14; 11; 43]. An intervention to improve overweight and obese OA patients’ ability to cope with their pain and manage their weight may have additive benefits, but such an approach has not been investigated.
There are good reasons to believe that overweight and obese OA patients may benefit from a behavioral intervention combining both pain coping and weight loss strategies. First, these patients can experience increased pain when initiating exercise, leading to exercise avoidance and/or failure to reach target heart rate training range [41; 17]. Skills designed to cope with pain during exercise and to decrease exercise avoidance may provide benefit. Second, these patients may experience acute pain relief (or mood relief) from eating highly caloric foods, leading to additional weight gain [40; 4; 14]. Training in pain coping teaches patients skills that can serve as alternatives to eating for pain or mood relief. Third, pain flares challenge the maintenance of pain coping skills and weight management strategies. Skills to increase coping with pain flares [27] may decrease their negative impact on weight management.
Previous studies involving pain coping skills training (PCST) for normal weight OA patients have demonstrated efficacy [23; 24; 22; 26]. PCST emphasizes pain as a biopsychosocial experience, using cognitive and behavioral techniques to improve pain coping. PCST benefits in overweight and obese OA patients with pain may be enhanced by the addition of lifestyle behavioral weight management (BWM) strategies. Lifestyle BWM programs emphasize gradual weight loss through addressing behavioral and psychosocial lifestyle factors influencing weight management [8]. Comprehensive BWM programs have demonstrated efficacy for reducing weight in people who are overweight or obese though they have not been evaluated for OA specifically. Components of lifestyle BWM have been utilized with overweight and obese OA patients with pain, demonstrating moderate changes in weight, pain, and disability [37; 9; 34; 38; 18; 42; 13]. Past intervention work has not explicitly addressed how OA maladaptive pain coping efforts may interfere with weight management or fully applied state-of-the-art lifestyle BWM strategies, as that work has largely focused on dietary restriction and exercise. Furthermore, long-term treatment outcomes have not been evaluated.
The aim of this study was to compare the long-term effects of a combined PCST and BWM protocol to either protocol alone or a standard care condition on overweight and obese OA patients’ pain, physical disability, and psychological disability, and weight. The combined protocol, compared to either treatment alone or a standard care condition, was hypothesized a priori to: achieve greater reductions in pain (specified a priori as the primary outcome), physical disability, and psychological disability as well as body weight. Because OA is a chronic disease, this study was designed to examine the long-term treatment effects of intervention and thus the average of each outcome over the 12-months after completion of treatment (post-treatment, 6 months and 12 months follow up) was examined.
Methods
Participants & Procedures
Participants for this randomized clinical trial were recruited through the Rheumatology, Orthopedic Surgery, Internal Medicine, Family Medicine, and Pain Management clinics at Duke University Medical Center (DUMC), through flyers posted in the community and from advertisements in local newspapers. Most (90%) participants were recruited through the community and from advertisements in local newspapers, and 10% were recruited from DUMC clinics via physician referral. All study procedures and materials were approved by the DUMC Institutional Review Board. All participants in this study were recruited between January 2004 and February 2008 providing written informed consent prior to any study procedures.
To determine if they were eligible for the study, all participants were asked about their pain, were weighed, received bilateral knee radiographs, and met with a study rheumatologist, physician’s assistant, or nurse who conducted a medical history and a physical examination. Participants were included if: 1) they reported knee pain on most days of the month for at least the prior 6 months; 2) were over the age of 18; 3) were overweight or obese (BMI greater than or equal to 25 and less than or equal to 42); 4) met the American College of Rheumatology criteria for OA and had radiographic evidence of OA affecting one or both knees (knee x-rays were graded by an experienced reader) on the basis of the Kellgren-Lawrence grading system (0–4; [28]); 5) had no other major weight bearing joint affected by OA; 6) OA of the knee(s) was considered the medical condition that contributed most to limitations in their daily function as assessed by the healthcare provider; and 7) were able to read and speak English.
Participants were excluded if they: 1) had a significant medical condition that increased their risk of a significant adverse health event during physical activity (e.g., myocardial infarction in the previous six months, abnormal blood pressure response to exercise, etc.); 2) had another known organic disease that would contraindicate safe participation in the study (e.g., cancer); 3) had a non-OA inflammatory arthropathy or another arthritic disorder (e.g., rheumatoid arthritis); 4) used oral corticosteroids regularly; or 5) were participating in a regular exercise or weight loss program. During the consent process, all participants were told about each of the possible conditions they could be randomized to participate in, including standard care. After consent, all participants completed a baseline assessment visit that included a series of questionnaires to assess pain, physical disability, including stiffness and activity, and psychological disability including pain catastrophizing and self-efficacy. Participants completed laboratory gait measurements and provided demographic and medical information.
After completing the baseline assessments, a data technician unfamiliar with the research protocol used a random allocation computer software program to assign participants in blocks (minimum = 27, maximum = 39) to one of four treatment conditions: 1) Pain Coping Skills Training alone (PCST-only); 2) Behavioral Weight Loss alone (BWM-only); 3) PCST with Behavioral Weight Loss (PCST+BWM); or 4) Standard Care Control. No stratification variables were used. A research assistant communicated randomization results to participants. A total of seven cohorts were randomized with 6 to 10 participants randomized into each condition. Following the 24 week treatment period, all participants in treatment conditions received a maintenance phone call 1 time a month for 6-months. Participants completed an in person post-treatment assessment immediately following the 24 week treatment period, a 6-month follow-up, and a 12-month follow-up. Post-treatment assessments were conducted by research assistants who were blind to the participant’s treatment condition. One reportable adverse event occurred during the study; a participant randomized to PCST+BWL fell off of the treadmill during the study exercise session which resulted in superficial wounding. No other reportable adverse events occurred. Non-reportable adverse events occurred in each condition and included instances such as participant being injured outside of a study session or having an illness such as a cold which prevented them from exercising for a period of time.
Pain Coping Skills Training (PCST)
PCST was delivered over the course of 24 weeks. During the first 12 weeks, 60-minute group sessions were held weekly. For the last 12 weeks, 60-minute group sessions were held every other week. PCST was delivered by clinical psychologists with prior PCST experience (1 to 5 years) who were systematically trained by a senior clinical psychologist who is an expert in pain coping skills training having over 20 years of experience using these methods in chronic pain populations. A manualized session by session outline was created that was specific to this study. Training included role playing, listening to the protocol delivered on audiotape, and observation of PCST being delivered in a group format. Psychologists delivering the treatment for this protocol met for supervision weekly with the senior psychologist; audiotapes of session were reviewed to evaluate the concurrence between the session delivery and the intervention protocol, and role playing for the next session were conducted. Four psychologists led the PCST groups during the course of the study. The PCST intervention was designed to 1) decrease maladaptive pain catastrophizing; and 2) enhance participants’ ability to control and decrease pain by increasing use of adaptive coping strategies (e.g., distraction, relaxation, and changing activity patterns). To introduce PCST, a simplified version of Melzack and Wall’s gate control model of pain [33] was used to show that pain is affected by thoughts, feelings, and behaviors. Pain coping strategies were described as skills that can be mastered through home practice. Participants were trained in three attention diversion methods: relaxation, imagery, and distraction. Activity-rest cycling and pleasant activity scheduling were used to reduce pain and enable participants to pace and increase their activity level. Cognitive-restructuring was used to help participants recognize the relationships between thoughts, feelings and behavior. This technique was also used to identify pain catastrophizing and other irrational, maladaptive thoughts and to replace these with alternative, rational coping thoughts. Participants were encouraged to practice skills learned and given homework assigments during the time in between sessions. During the six biweekly sessions in the second half of the intervention period, maintenance of PCST was emphasized, coping skills were reviewed, and difficulties encountered were identified. Methods for coping with common problems (e.g., helplessness in response to pain flare up) were reviewed, monitoring for early warning signs of setbacks in coping efforts were discussed, and participants were assisted in developing a plan for coping with such problems. PCST is based on previous work in studies of patients with arthritis pain and has been validated in prior studies in OA patients [23; 24].
Behavioral Weight Management (BWM)
During the first 12 weeks, 60 minute group sessions were held weekly. Additionally, three 90-minute supervised exercises sessions were held each week of the first 12 weeks. During the last 12 weeks, 60-minute group sessions were held every other week; there were no supervised exercise sessions. BWM was delivered by psychologists with a specialty in behavioral medicine and prior experience in behavioral weight management protocols (1 to 6 years). Systematic training and supervision in the BWM protocol was done by a senior clinical psychologist with prior experience in behavioral weight management. A manualized session by session outline was created specifically for this study. Training was similar to that used for the PCST groups and included role playing, listening to the protocol delivered on audiotape, and observation of BWM being delivered in a group format. Psychologists delivering the treatment for the BWM protocol met for supervision weekly with the senior psychologist; audiotapes of session were reviewed to evaluate concurrence between delivery and the intervention protocol, and role playing with the content for the next session was conducted. Five psychologists led the PCST groups during the course of the study. The exercise sessions were conducted by an exercise physiologist with experience in patients with chronic diseases such as OA. Study supervision of the exercise physiologists was provided by a separate senior clinical health psychologist with over 20 years of experience in exercise training of patients with chronic diseases.
The BWM weekly group session information was based primarily on the comprehensive and empirically validated LEARN Program for Weight Management [8]. Each participant was given a copy of the LEARN manual [8], which focuses on five elements related to weight loss: lifestyle, exercise, attitudes, relationships, and nutrition and contains 16 weekly sessions. The content of most of the group sessions was based on the weekly topic(s). In addition, participants received Appetite Awareness Training [7] for two sessions, which emphasized the importance of attending to internal hunger and fullness cues. The overall goal of the LEARN program is a weight loss of 1 to 2 pounds (i.e., 0.45 to 0.92 kilograms) a week achieved by gradually decreasing calorie and fat intake through permanent lifestyle changes. Initial calorie goals were set at 1200 daily for women and 1500 daily for men. These goals were adjusted based on individual progress. Weight was recorded at each weekly session. Participants were required to keep weekly food diaries and these diaries were reviewed at the beginning of each meeting.
Supervised group exercise training ranges were based on maximum heart rate achieved during an exercise treadmill test. Participants were assigned training ranges equivalent to 70% maximum heart rate reserve. Each exercise session was started with a 10 minute warm-up period, with general flexibility and isometric strengthening of postural muscles. Aerobic training session consisted of stationary bicycling progressing from an intensity and duration from 55% of heart rate reserve for 15 minutes to 70% of heart rate reserve for 30 minutes. Participants progressed to the use of other aerobic exercise machines (e.g., treadmill) to achieve these goals as preferred and tolerated. Exercise sessions concluded with 10 minutes of cool-down consisting of light stretching and deep breathing exercises. Individual plans for maintenance were developed to ensure that participants could continue their new activity patterns.
PCST+BWM
Participants randomized to the PCST+BWM condition concurrently received the PCST and BWM protocols described above. That is, during the first 12 weeks, participants attended 120 minutes of group sessions that first presented the BWM protocol and then the PCST protocol. During the first 12 weeks, participants also attended three 90-minute supervised exercises sessions each week. During the last 12 weeks, participants attended 120 minutes of group sessions held every other week that first presented the BWM protocol and then the PCST protocol. All PCST+BWM groups were delivered by clinical psychologists referenced above. The same psychologist delivered both PCST and BWM in any given cohort. Training and supervision were uniform with the description provided above with additional attention given to only presenting the protocol material specific to the session being conducted (i.e., PCST or BWM).
Standard Care Control
The standard care control condition was designed to serve as a routine treatment control. Patients assigned to this condition continued to receive their routine care. They did not receive PCST or BWM. They were requested to complete all measures at time intervals corresponding with the beginning and end of the active interventions and the follow-up assessments.
Maintenance Calls
After the 24-week active intervention phase, participants in all treatment conditions received six monthly maintenance calls focused on reinforcing the use of skills learned during the intervention. Phone calls were scheduled to be approximately 20 minutes long and were structured to include a review of skills, discussion of skill use, how skills were or could be applied in problem situations, and goal setting for the upcoming month. Phone calls were recorded and a number of calls were reviewed by the supervising psychologist and periodically reviewed during supervision sessions.
Measures
Osteoarthritis Diagnosis
The diagnosis of knee OA was based on the American College of Rheumatology clinical classification criteria of knee OA. Radiographic assessment of both knees was used to confirm the OA diagnosis. A fixed-flexion posteroanterior knee radiograph was taken with the SynaFlex™ X-ray positioning frame (Synarc, San Francisco, CA). With this platform, the feet were externally rotated 10 degrees, the knees and thighs touched the vertical platform anteriorly, and the X-ray beam was angulated 10 caudally. Skyline views of both patellae were taken with the participant in the seated position, knees bent, and the beam angled from the feet toward the knees. One of the study rheumatologists graded each x-ray on the basis of Kellgren-Lawrence criteria [28]. The most severe of the two knees’ Kellgren-Lawrence scores (range 1–4) was used to designate an individual’s severity in this study, with higher scores indicating greater disease severity.
Pain, Physical Disability, and Psychological Disability
The Arthritis Impact Measurement Scales (AIMS) [32] was used to measure pain, physical disability, and psychological disability. The AIMS is a widely used 45-item, self-report questionnaire designed to measure health status in arthritis participants that provides three summary scales: pain, physical disability, and psychological disability. Summary scales range from 0 to 10, with higher scores indicating greater pain or disability. The Western Ontario and McMaster Osteoarthritis Index (WOMAC; [6]), a multidimensional assessment tool, was also used to measure pain as well as stiffness and physical functioning activities. The WOMAC index used in this study was a visual analog scale that consisted of three subscales assessing pain (5 items), stiffness (2 items), and physical functioning activities (17 items). The range of scores on each subscale was between 0 and 100, with higher scores reflecting a worse condition. The reliability and validity of both the AIMS and the WOMAC have been supported by previous research [6; 3; 20].
Gait Velocity
Gait velocity was also used to assess physical disability. Three-dimensional kinematic data were collected using the EvaRT motion analysis system (Motion Analysis, Inc., Santa Rosa, CA) as subjects walked along a 30-meter walkway at normal and fast speeds. Velocity was measured initially using two wireless infrared photocell timing devices (Brower Timing Systems, Draper, Utah) positioned 5 meters apart and the participant’s target walking velocity for each speed was determined. Velocity was also calculated from reflective markers placed on the subjects sacrum (reflective markers were used to collect kinematic data for a separate part of this study). The EvaRT software was used to track the reflective markers and condition the data. The raw data were smoothed using a 4th order, recursive Butterworth filter with a 6Hz cutoff frequency. Three trials at each speed in which all markers were identified and the subject had clean contact with the force plate (kinetic data were collected for a separate part of the study) were averaged to the velocity sample used in this analysis.
Pain Catastrophizing
Catastrophizing was assessed using the Catastrophizing Scale of the Coping Strategies Questionnaire (CSQ; [44]) This scale contains six items that ask participants to rate the frequency with which they engage in catastrophizing when they experience pain using a six-point scale on which 0 = “never” and 6 = “always”. The CSQ Catastrophizing Scale has been shown to have good internal reliability as well as a high degree of stability over time [44].
Self-Efficacy for Arthritis and Weight Control
Two self-efficacy scales were used. First, the Arthritis Self-Efficacy Scale (ASES) [30] was used to assess participants’ perceived abilities to perform behaviors that would control arthritis. This measure is comprised of three subscales: self-efficacy for pain control, self efficacy for physical function, and self-efficacy other arthritis symptoms. Participants are asked to indicate their responses on a Likert-type 10–100 scale (10 = “very uncertain”; 100 = “very certain”). A total self efficacy score created by adding together scores on each subscale of this instrument. Second, the Weight Efficacy Life-Style Questionnaire (WELSQ; [10]), a 20-item scale used to assess participants’ self-efficacy to control their weight by resisting eating across five situations (i.e., positive emotions, negative emotions, food availability, social context, physical discomfort), was used. Items are rated on a 0–9 scale where 0 = “not confident in my inability to resist desire to eat” and 9 = “very confident in ability to resist desire to eat.” The sum of the ratings for all items provides a global measure with higher scores reflecting greater self-efficacy for resisting eating. The WELSQ has demonstrated good reliability and validity [10].
Weight & Body Mass Index (BMI)
Weight was measured to the nearest 0.1 kg with without shoes in the standing position. Height was measured to the nearest 1 cm. BMI was calculated by dividing weight (in kg) by height (in m2).
Power Analysis
Power computations were made based on an expectation of 60 participants in each group, 15% attrition, and contrasts comparing the PCST+BWM group to the remaining three groups. We assumed that the correlation between the baseline covariates and a given follow-up measure would be r = .5. Assuming an alpha of .05, a reduction in the error term of (square root of [1–.50]) = .71 (because of the baseline covariate), we estimated that we would have 80% power to detect an effect size of approximately d = .55 for a given outcome, where d is the standardized difference between group means.
Statistical Analyses
All analyses adhered to the intent-to-treat principle. The primary analysis was carried out using mixed repeated measures model, as available with SAS PROC MIXED (SAS 9.1, Cary, NC). Mixed models have the desirable feature of using all available data in the analysis, irrespective of whether some data points are missing for a given participant. Separate models were estimated for each outcome. The follow-up measurement (serial measures of the outcome from the 2nd through 4th measurement occasion) was the response variable and is referred to as the post-treatment level. Modeling all measurement occasions in this fashion allows us to understand the course of the outcomes over the entire year of follow-up: thus the analysis evaluates not only the immediate impact of treatment but also the maintenance of those effects over a one-year period. In addition, including the full complement of measurement occasions enables the mixed model to preserve the cases that had one or more missing data points during the follow-up. The predictor side of the models included the baseline level of the corresponding outcome variable, treatment group, age, gender, race, disease severity, time, and the treatment by time interaction. It is recommended that covariates be chosen based on their substantive basis and not on test of differences[15]; we included age, gender, race, and disease severity in all models based on their associations with the study outcomes in prior work [19; 46]. The inclusion of covariates in a randomized trial improves the precision of the treatment estimates and improves the power of the tests of the treatment effect[15]. Age, gender, race, and disease severity were included in all models because past work has suggested they have significant relationships with the study outcomes. Continuous variables were centered at their means, while the time variable was “centered” at the immediate post-treatment measurement occasion. We examined several covariance structures using fit statistics and determined that the compound symmetry structure was a reasonable choice. Thus a model was fitted of the form:
In addition to improving the precision of the treatment effect estimates, using the baseline level of the outcome as an adjustment covariate also has important implications for which model terms are of the most interest. In the case of a conventional repeated measures analysis of variance, where the baseline measure is included on the response side of the model, the effect of primary interest is the time by treatment interaction term. In contrast, in the present model the term of primary interest is the main effect for treatment. A main effect for treatment is interpreted as the effect of that treatment averaged over the three post-treatment time periods (i.e., treatment and maintenance). We used Dunnett’s procedure to compare the averaged effect of the PCST+BWM to the remaining groups. This aim of this study was to compare the benefits of PCST+BWM to each treatment alone and a standard care condition; thus, the reference group for all models was PCST+BWM. Of secondary interest is the time by treatment interaction, which addresses the question of whether the groups differ on change during the second, third, and fourth measurement occasion. A non-significant time by treatment interaction suggests that the changes over the post-treatment follow-up period cannot be distinguished from sampling error. If interactions terms were not statistically significant, they were removed from the model and the model was re-estimated with only the main effects terms.
Results
Sample Characteristics
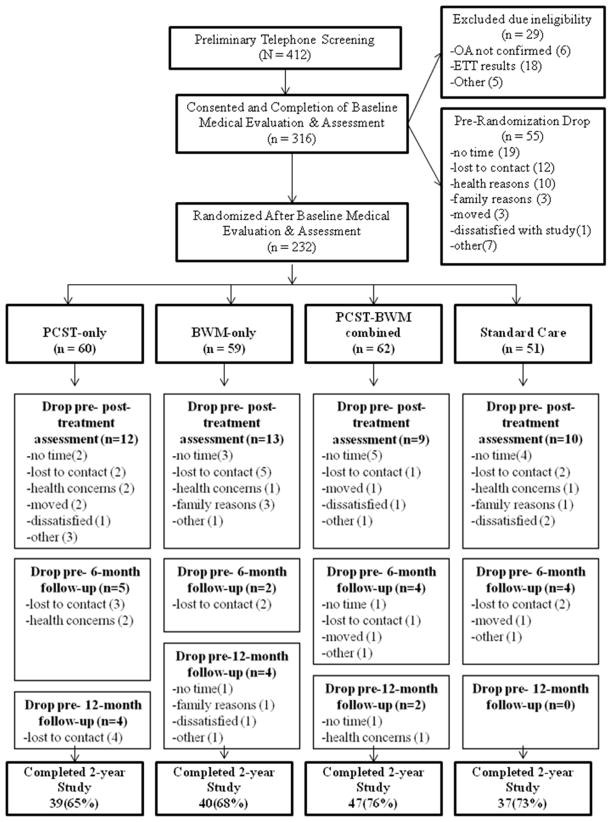
Two-hundred and thirty-two participants (aged 20–85) met study criteria and were randomized into the study. The primary reasons for participant exclusion were failure to be medically fit for exercise based on results of the exercise treadmill test, participant declining due to time constraints, participants lost to contact after baseline evaluation and assessment, and participant declining study participation due to other health problems (Figure 1). Participants in this study were on average 58 (SD=10) years old, 79% were female, and self-reported to be 62% white, 356% black, 1% American Indian or Alaskan Native and 2% reported “other” race. The treatment groups did not differ with respect to age, gender, race, education, or OA disease severity (Table 1).
Figure 1.
Flowchart of trial.
Table 1.
Patient Characteristics for Treatment Groups
| Characteristics | PCST-only (n = 60) | BWM-only (n = 59) | PCST + BWM (n = 62) | Standard Care (n = 51) | Total (N=232) |
|---|---|---|---|---|---|
| Age years, mean (SD) | 58.13(11.25) | 58.27(11.02) | 57.47(9.43) | 57.94(10.09) | 57.95(10.41) |
| Male, n(%) | 20(33%) | 12(20%) | 5(8%) | 11(22%) | 48(21%) |
| Education n(%) | |||||
| Less than high school | 2(3%) | 0(0%) | 3(5%) | 0(0%) | 5(2%) |
| High school graduate | 8(13%) | 4(7%) | 8(13%) | 6(12%) | 26(12%) |
| Some college | 15(25%) | 10(17%) | 14(23%) | 19(37%) | 58(25%) |
| College graduate | 19(32%) | 25(42%) | 22(37%) | 8(16%) | 74(32%) |
| At least some graduate school | 16(27%) | 20(34%) | 13(22%) | 18(35%) | 67(29%) |
| Nonwhite, n(%)a | 23(38%) | 20(34%) | 25(40%) | 20(39%) | 88(38%) |
| KL score, m(sd) | 2.48(1.01) | 2.38(1.12) | 2.38(1.05) | 2.34(1.05) | 2.40(1.06) |
Note. PCST = pain coping skills training. BWM = behavioral weight loss KL = Kellgren-Lawrence.
The racial composition of the samples was White = 143 (62%); Black=80 (35%); American Indian or Alaskan Native = 1(1%); Reported “Other” = 4(2%).
Adherence
Seventy percent (N=163) of all randomized participants completed the 2-year study; 69 (30%) dropped out before completing the entire 2-year study protocol. Twenty-four participants (6 from PCST-only, 10 from BWM-only, 4 from PCST+BWM, 4 from standard care) dropped out of the study after randomization but before treatment due to: lack of time for study (n=8), being lost to contact (n=3), health reasons (n=4), family reasons (n=2), moving (n=1), dissatisfied with study (n=2), or other or unknown (n=4). Participant dropouts at other study intervals were as follows: 20 participants dropped out prior to the post-treatment assessment (6 from PCST-only, 3 from BWM-only, 5 from PCST+BWM, 6 from standard care); 15 participants dropped out prior to the 6-month follow-up assessment (5 from PCST-only, 2 from BWM-only, 4 from PCST+BWM only, 4 from standard care); 10 participants dropped out prior to the 12-month post-treatment assessment (4 from PCST-only, 4 from BWM-only, 2 from PCST+BWM only, 0 from standard care). Participants were classified as a dropout if they asked to not be contacted for any future study activities or if study staff were unable to contact them by telephone or postal mail. Any participant who was not a study dropout was classified as completing the study. Participants who were not classified as a dropout were contacted and asked to complete all assessments even if they missed a prior assessment. All randomized participants were included in the data analysis following the intent-to-treat principle. Dropout rates did not vary significantly across treatment conditions (chi-square = 2.0; p = 0.57). Figure 1 depicts the reasons that participants gave for study dropout in detail by each treatment group. Study dropouts did not differ from study completers on baseline measures of physical or psychological disability, self-efficacy, or pain catastrophizing (p’s = 0.36–0.65). Participants who dropped out had higher baseline AIMS pain scores (p = 0.02) and weight (p = 0.03). Among participants who did not drop out post-randomization and who attended at least one intervention session, participants randomized to the PCST-only condition attended a mean of 66% (median = 72%; inter-quartile range [IRQ] = 56%–83%) of their in-person intervention sessions, participants randomized to the BWM-only condition attended a mean of 65% (median = 72%; IRQ = 53%–83%) of their in-person intervention sessions and 64% (median = 72%; IRQ = 53%–81%) of the exercise sessions, and participants randomized to the PCST+BWM condition attended a mean of 74% (median = 83%; IRQ = 67%–89%) of their in-person intervention sessions and 72% (median = 75%; IRQ = 65%–85%) of their exercise sessions. Thirty participants randomized to an active intervention condition did not attend any intervention sessions (PCST-only = 10, BWM-only = 13, PCST+BWM = 7). When participants missed intervention sessions, they were contacted by phone to inquire about reasons for missing session, provide them with the session information, and to encourage them to read the materials and engage in home practice.
Study Outcomes
Mixed model results showed that the overall time effect was significant for weight, BMI, physical disability, self-efficacy, pain catastrophizing but not for pain, psychological disability, and gait. These results are presented below and in Table 2. In no cases did we find a significant time by treatment interaction. This term was therefore removed from all analyses.
Table 2.
Treatment outcomes adjusted for age, gender, ethnicity, and disease severity.
| Outcome | Effect of Treatment | Baseline Value | Post Treatment Average | Dunnett’s Test Adjusted P | Estimated Difference Between PCST+BWM and Each Other Condition | |
|---|---|---|---|---|---|---|
| F Value | Pr>F | M(95%CI) | M(95%CI) | M(95%CI) | ||
| AIMS Pain | 4.22 | .007 | ||||
| PCST+BWM* | 5.8(5.3–6.2) | 4.0(3.7–4.3) | ||||
| BWM-only | 5.3(4.9–5.7) | 4.7(4.3–5.1) | .01 | .73(.18–1.3) | ||
| PCST-only | 5.6(5.2–6.0) | 4.4(4.1–4.8) | .22 | .41(−.16–1.0) | ||
| Standard Care | 5.5(4.9–6.1) | 4.7(4.3–5.1) | .02 | .70(.10–1.3) | ||
| WOMAC Pain | 7.01 | .0002 | ||||
| PCST+BWM* | 47.7(42.1–53.3) | 27.2(23.9–30.4) | ||||
| BWM-only | 42.6(37.7–47.5) | 35.5(31.9–39.0) | .002 | 8.3(2.5–14.1) | ||
| PCST-only | 42.8(42.1–53.3) | 34.5(30.8–38.2) | .01 | 7.3(1.3–13.3) | ||
| Standard Care | 43.4(37.4–49.5) | 38.0(34.1–41.8) | .0002 | 10.8(4.6–16.9) | ||
| AIMS Physical | 13.4 | <.0001 | ||||
| PCST+BWM* | 1.7(1.4–1.9) | 1.0(0.8–1.1) | ||||
| BWM-only | 1.8(1.1–1.7) | 1.5(1.3–1.6) | <.0001 | 0.5(0.3–0.8) | ||
| PCST-only | 1.6(1.3–1.8) | 1.5(1.3–1.6) | <.0001 | 0.5(0.3–0.7) | ||
| Standard Care | 1.6(1.2–1.9) | 1.4(1.2–1.6) | <.0001 | 0.4(0.2–0.7) | ||
| WOMAC Stiffness | 5.30 | .0017 | ||||
| PCST+BWM* | 61.5(55.6–67.3) | 35.4(31.2–39.6) | ||||
| BWM-only | 50.7(44.6–56.7) | 45.7(41.2–50.2) | .004 | 10.3(2.8–17.7) | ||
| PCST-only | 54.7(48.3–61.1) | 44.5(39.7–49.2) | .02 | 9.0(1.4–16.8) | ||
| Standard Care | 53.2(46.0–60.7) | 46.4(41.3–51.3) | .004 | 10.9(3.2–18.8) | ||
| WOMAC Activity | 11.84 | <.0001 | ||||
| PCST+BWM* | 47.7(42.2–53.1) | 25.1(22.1–28.3) | ||||
| BWM-only | 44.3(39.5–49.0) | 36.0(32.6–39.3) | <.0001 | 10.8(5.3–16.2) | ||
| PCST-only | 46.2(41.1–51.3) | 35.2(31.8–38.6) | .0001 | 10.0(4.4–15.6) | ||
| Standard Care | 46.1(39.7–52.5) | 37.5(33.9–41.2) | <.0001 | 12.4(6.5–18.2) | ||
| Normal Velocitya | 1.7 | .17 | ||||
| PCST+BWM* | 1.1(1.1–1.2) | 1.2(1.1–1.2) | ||||
| BWM-only | 1.1(1.1–1.2) | 1.2(1.1–1.2) | .89 | −.01(−.06–.03) | ||
| PCST-only | 1.1(1.0–1.1) | 1.1(1.1–1.2) | .41 | −.04(−.10–.01) | ||
| Standard Care | 1.1(1.1–1.2) | 1.2(1.1–1.2) | .98 | −.01(−.05–.04) | ||
| Fast Velocitya | .50 | .68 | ||||
| PCST+BWM* | 1.5(1.4–1.6) | 1.6(1.5–1.6) | ||||
| BWM-only | 1.6(1.5–1.6) | 1.5(1.5–1.6) | .92 | .02(−.04–.08) | ||
| PCST-only | 1.5(1.4–1.6) | 1.5(1.5–1.6) | .98 | −.01(−.07–.05) | ||
| Standard Care | 1.5(1.4–1.6) | 1.5(1.5–1.6) | .62 | .03(−.02–.10) | ||
| AIMS Psychological | 2.22 | .09 | ||||
| PCST+BWM* | 2.7(2.3–3.2) | 2.2(2.0–2.4) | ||||
| BWM-only | 2.9(2.5–3.4) | 2.5(2.2–2.7) | .30 | .23(−0.1–.06) | ||
| PCST-only | 2.9(2.6–3.9) | 2.6(2.4–2.8) | .05 | 0.4(0.1–0.7) | ||
| Standard Care | 3.0(2.6–3.4) | 2.5(2.3–2.8) | .16 | 0.3(−0.1–0.6) | ||
| Pain Catastrophizing | 3.6 | .02 | ||||
| PCST+BWM* | 7.4(5.5–9.3) | 3.8(3.0–4.6) | ||||
| BWM-only | 6.6(4.8–8.2) | 5.6(4.7–6.5) | .008 | 1.8(.40–3.2) | ||
| PCST-only | 7.2(5.5–8.9) | 4.9(4.0–5.8) | .19 | 1.1(−.38–2.6) | ||
| Standard Care | 6.9(4.9–8.9) | 5.4(4.4–6.3) | .04 | 1.5(.04–3.0) | ||
| Self-Efficacy Total | 11.34 | <.0001 | ||||
| PCST+BWM* | 207.6(195.0–220.2) | 243.25(236.3–250.1) | ||||
| BWM-only | 199.7(186.1–213.3) | 222.3(214.7–229.8) | .0002 | −21.0(−33.3 – −8.7) | ||
| PCST-only | 201.4(188.3–214.5) | 225.7(217.7–233.7) | .004 | −17.5(−30.4 – −4.7) | ||
| Standard Care | 198.6(184.9–212.4) | 213.0(204.7–221.2) | <.0001 | −30.3(−43.4 – −17.2) | ||
| Weight Self-Efficacy | 6.9 | .0002 | ||||
| PCST+BWM* | 5.26(4.7–5.8) | 6.5(5.7–6.3) | ||||
| BWM-only | 5.53(5.0–6.0) | 5.9(5.6–6.2) | .003 | −.57(−.98–−.16) | ||
| PCST-only | 5.41(5.0–5.8) | 6.0(5.7–6.2) | .02 | −.47(.91–−.05) | ||
| Standard Care | 4.91(4.4–5.4) | 5.7(5.4–6.0) | .0001 | −.77(−1.2–−.33) | ||
| Weight | 15.7 | <.0001 | ||||
| PCST+BWM* | 204.2(196.1–212.4) | 197.2(195.0–199.5) | ||||
| BWM-only | 203.5(195.0–212.1) | 203.3(200.8–205.8) | .0014 | 6.08(2.0–10.1) | ||
| PCST-only | 212.9(203.8–222.1) | 207.8(205.1–210.5) | <.0001 | 10.61(6.3–14.9) | ||
| Standard Care | 203.5(199.1–219.0) | 207.5(204.7–210.3) | <.0001 | 10.32(5.9–15.0) | ||
| BMI | 13.3 | <.0001 | ||||
| PCST+BWM* | 34.1(33.0–35.2) | 32.7(32.3–33.1) | ||||
| BWM-only | 33.5(32.4–34.7) | 33.9(33.5–34.3) | .0004 | 1.20(0.5–2.0) | ||
| PCST-only | 34.4(33.3–35.5) | 34.3(33.8–34.8) | <.0001 | 1.62(0.8–2.4) | ||
| Standard Care | 34.1(32.8–35.4) | 34.5(34.0–35.0) | <.0001 | 1.79(1.0–2.6) | ||
Pain
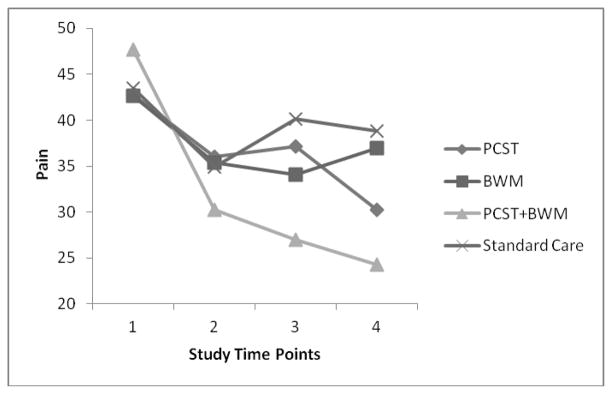
For the AIMS pain scale, participants in the combined PCST+BWM condition exhibited the lowest post-treatment levels of pain; this was followed by the PCST-only condition (next lowest), followed by BWM-only and the standard care conditions. Dunnett’s procedure showed that the PCST+BWM condition differed significantly from the BWM-only and standard care conditions, but not from the PCST-only condition. A similar pattern emerged for the WOMAC pain outcome, again with participants in the PCST-BWM condition showing the lowest post-treatment levels of pain followed by PCST-only, and then the BWM-only and standard care conditions. In this case, however, the PCST-BWM condition differed from all of the other three conditions. See Figure 2.
Figure 2.
WOMAC Pain scores at pre-treatment, post-treatment, 6-months post-treatment, and 12-months post treatment by randomization condition
Physical Disability
For the AIMS physical disability scale, participants in the combined PCST+BWM condition exhibited the lowest post-treatment levels of physical disability; standard care condition, the next lowest, followed by the BWM-only and PCST-only conditions. PCST+BWM condition differed significantly from each of the other three conditions. For the WOMAC stiffness scale, participants in the PCST+BWM condition exhibited the lowest post-treatment levels of stiffness, followed by PCST-only, then BWM-only, and then the standard care condition. The PCST+BWM condition differed significantly from the other three conditions. For the WOMAC physical function activity scale, again, participants in the PCST+BWM condition demonstrated the lowest levels of activity impairment followed by PCST-only, BWM-only, and then standard care. Again, PCST+BWM condition differed significantly from the other three conditions. When examining group means over the course of the study for gait velocity (i.e., average of normal and fast speeds), there were no significant time by treatment group effects or interactions.
Psychological Disability
Participants in the combined PCST+BWM condition exhibited the lowest post-treatment levels of psychological disability, followed by BWM-only and standard care, and then PCST-only. PCST+BWM condition differed significantly from the PCST-only condition but was not significantly different from BWM-only or standard care.
Pain catastrophizing
Participants in the combined PCST+BWM condition demonstrated the lowest post-treatment levels of pain catastrophizing; the next lowest scores were in the PCST-only group, followed by standard care, and then BWM-only. PCST+BWM conditioned differed significantly from BWM-only and standard care, but not from PCST-only.
Self-efficacy for arthritis and weight management
For arthritis self-efficacy, participants in the PCST+BWM condition demonstrated the highest post-treatment levels of arthritis management self-efficacy, followed by PCST-only, BWM-only, and finally standard care. PCST+BWM condition differed significantly from PCST-only, BWM-only, and standard care. For weight management self-efficacy, the combined PCST+BWM condition exhibited the highest post-treatment levels of weight-management self-efficacy, followed sequentially by PCST-only, BWM-only, and standard care. PCST+BWM condition differed significantly from PCST-only, BWM-only and standard care.
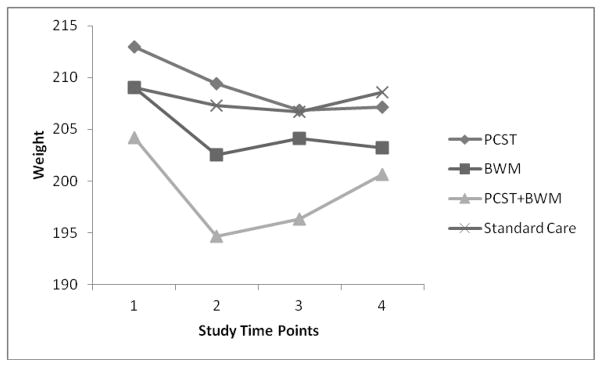
Weight and BMI
For weight (see Figure 3), participants in the combined PCST+BWM condition achieved the lowest post-treatment weight (average weight loss of 7.0 pounds during the 2-year period) followed by BWM-only and then PCST-only and standard care. Again, the PCST+BWM condition differed significantly from all other groups. For BMI, participants in the combined PCST+BWM demonstrated the lowest post-treatment BMI levels; BWM-only was the next lowest, followed by PCST-only and standard care. PCST+BWM condition differed significantly from each of the other three conditions. To note, participants randomized to the PCST+BWM condition had lost on average 5% of their weight at post-treatment and were able to on average maintain approximately 50% of this loss over the 2-year follow-up period.
Figure 3.
Weight at pre-treatment, post-treatment, 6-months post-treatment, and 12-months post treatment by randomization condition
Discussion
This study examined the combined effects of PCST and a lifestyle BWM program (i.e., PCST+BWM) compared to either treatment alone and a standard care control condition in overweight and obese OA patients. Participants randomized to the PCST+BWM condition showed long-term improvements in pain, physical disability, psychological disability, and weight when compared to the other groups. To our knowledge, this study is the first of OA patients to demonstrate that a behavioral intervention that simultaneously addresses pain and weight is more effective in improving pain and other outcomes than behavioral interventions that address pain or weight alone. Strengths of this study included long-term examination of a number of OA-related outcomes, the comparison of four conditions, the fact that it is the first study to apply PCST specifically to overweight and obese OA patients with pain, use of radiographic x-ray to confirm OA diagnosis, and use of intent-to-treat, mixed repeated measures model analyses that permit use of all available data.
One of the most important findings was that participants in the PCST+BWM condition demonstrated significantly greater reductions in pain than participants in PCST-only, BWM-only, and standard care conditions. Analysis of data collected with the WOMAC pain scale showed that participants in the PCST+BWM condition improved significantly more than all of the other groups, while analysis of data collected with the AIMS pain scale demonstrated differences from the BWM-only and standard care conditions. It is generally assumed that weight loss is the key for pain reduction in overweight and obese OA patients. However, our results that participants in the PCST+BWM condition evidenced greater long-term reductions in pain than participants in the BWM-only condition challenge this assumption. Past work in overweight and obese OA patients has found decreased pain resulting from interventions aimed only at weight loss [36; 38]; our findings suggest that PCST combined with BWM may result in even greater pain reduction.
Another important finding was that participants in the PCST+BWM condition were most likely to demonstrate greater decreases in weight compared to the other three conditions. While others have found that BWM programs can reduce weight [37; 9; 34; 38; 18; 42; 13], our finding suggests that training in pain coping along with weight management may be a critical component for longer-term weight management for OA patients. Participants randomized to the PCST+BWM condition had lost on average 5% of their weight at post-treatment and were able to on average maintain approximately 50% of this loss over the 2-year follow-up period. Identifying factors related to failed weight management in overweight and obese patient samples has been challenging [50]. Our results suggest that pain coping skills training may address factors influential in weight management (e.g., pain, arthritis self-efficacy) not addressed in traditional BWM programs. Consistent with this idea, more than 40% of morbidly obese OA patients gained or failed to lose weight while participating in a trial of lifestyle BWM that did not include pain management [48]. Our pre-to post-treatment data (not shown) suggest that 84% of patients in the PCST+BWM condition lost weight immediately following treatment. Finally, over the 24-month study timeline the patients in the standard care condition gained about as much weight as patients in the PCST+BWM lost. This pattern is important because it suggests that our intervention not only led to weight loss, but also prevented gradual weight gain that occurs over time.
Overweight and obese OA patients who were randomized to the PCST+BWM condition also demonstrated decreased physical disability, decreased stiffness, and increased activity compared to patients in the other conditions. These results underscore the notion that for overweight and obese OA patients, the application of PCST+BWM leads to benefits not seen with a weight management program alone.
Pain catastrophizing, one of the most important pain-related cognitions, was significantly decreased in patients in the PCST+BWM condition compared to patients receiving BWM-only. Pain catastrophizing refers to the tendency to focus on and magnify pain sensations, and to feel helpless in the face of pain [49]. Overweight and obese OA patients experience higher levels of OA pain and disability and may be particularly likely to engage in pain catastrophizing. Reducing pain catastrophizing is critical because it has been associated with weight management challenges (i.e., increased eating [45], decreased activity [12]). PCST-only worked as well as PCST+BWM on this particular measure indicating that being overweight or obese does not preclude some of the benefits of PCST.
Patients in the PCST+BWM condition showed significant improvements in arthritis self-efficacy compared to each of the other three conditions. Self-efficacy is the belief that one has the ability to successfully perform a behavior to achieve a desired outcome [5]. Patients reporting higher versus lower levels of arthritis self-efficacy have been shown to rate pain stimuli as less unpleasant and have a greater pain tolerance [25]; overweight and obese OA patients with higher arthritis self-efficacy may be more able to tolerate OA pain that results from increased activity or pain flares, decreasing their likelihood to engage in behaviors that challenge weight management (i.e., inactivity, overeating) in response to pain.
Patients in the PCST+BWM condition also demonstrated significant increases in weight management self-efficacy when compared to the other three conditions. Weight management self-efficacy is assessed by asking patients to rate their confidence in their ability to resist the desire to eat across different situations (e.g., when experiencing negative emotions, physical discomfort). Patients in the PCST+BWM condition reported significant increases in their confidence that they could resist eating across these common and often challenging eating situations.
There were no differences between PCST+BWM and the other conditions on gait outcomes. Although the present study found that PCST+BWM produced significant improvements in self reports of physical disability on the AIMS, this treatment combination did not produce significant improvements in gait outcomes. Based on prior studies showing the self reported physical disability correlates with gait markers [39], one might expect that gait findings would be obtained in the present study. Interestingly, a prior study examining the effects of weight loss on gait mechanisms by combining a sample patients who received varying treatments (i.e., exercise, diet, a control group) found that weight loss, irrespective of treatment condition, was associated with significant changes in gait [34]. This suggests that it is may be weight loss per se, rather than effects specific to a particular intervention protocol that might explain mprovements in gait. Additionally, there may be other gait assessments (i.e., joint kinematics, ground reaction forces) which may be more sensitive to changes produced by our behavioral interventions. For example, obese patients undergoing a mean weight loss of 13.5% body weight have shown significant reductions in knee joint loading, lower axial impulse, and the internal knee abductor moment [1]. Finally, although gait velocity is a reliable indicator of radiological OA severity [51], it may not be sensitive to behavioral intervention changes but gait-related assessments that can be considered more reflective of everyday activities (e.g., timed walking) might be. This possibility is consistent with our findings that PCST+BWM resulted in decreased physical disability in our self-report measures that assessed activities of daily living (e.g., walking a block). The multiple factors effecting disability and treatment of disability in this population are continuing to be investigated.
The current study has several limitations. First, it was limited to patients who were overweight or obese and does not provide information on whether these behavioral interventions would provide benefits to morbidly obese (BMI ≥ 40) OA patients. Future work should examine the efficacy of a combined PCST and BWM protocol for morbidly obese OA patients. Next, patients in this study were required to attend 18 weekly group sessions over 24 weeks, and in conditions with an exercise component, 3 weekly exercise sessions for 12 weeks. Future work should investigate methods of delivering PCST and BWM that are less time and resource intensive (e.g., phone or web-based, home-based exercise). Next, the relatively high level of education (i.e., 61% having at least a college degree) in this sample may indicate that participants had psychosocial resources to participate in a time intensive program that may not be found in a more general sample of patient. Additionally, participants were largely recruited from community advertisements (90%) and not from direct physician referral which may have influenced some of their characteristics (e.g., OA disease severity). Future work should aim to recruit a more general sample of patients with regard to education and recruitment source to examine whether or not similar findings emerge.
The results of this study indicate that significant benefits are provided by simultaneously training overweight and obese OA patients to increase the effectiveness of their pain coping skills and manage their weight. Over the course of two years, PCST+BWM provided both pain and weight-related benefits to overweight and obese OA patients not evidenced in PCST-only, BWM-only, or a standard care condition. These findings raise the interesting possibility of a synergistic effect created by combining interventions that teach overweight and obese OA patients to cope with their pain as well as manage their weight. It may be that PCST gives patients pain coping skills, which enhance their ability to comply with the needed lifestyle changes to lose weight (i.e., increasing activity, decreasing eating).
Acknowledgments
This study is known as OA Life. This publication was made possible by grant number P01 AR50245 from the National Institutes of Health. We would like to thank the numerous staff and faculty at Duke University Medical Center who worked on this study and as well as the patients who participated in this study; both of without whom it would not have been possible to conduct.
Footnotes
No conflict of interest is reported by the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Aaboe J, Bliddal H, Messier SP, Alkjaer T, Henriksen M. Effects of an intensive weight loss program on knee joint loading in obese adults with knee osteoarthritis. Osteoarthritis Cartilage. 2011 doi: 10.1016/j.joca.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1988;128:179–89. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 3.Anderson JJ, Felson DT, Meenan RF, Williams HJ. Which traditional measures should be used in rheumatoid arthritis clinical trials? Arthritis Rheum. 1989;32:1093–9. doi: 10.1002/anr.1780320907. [DOI] [PubMed] [Google Scholar]
- 4.Anseloni VC, Weng HR, Terayama R, Letizia D, Davis BJ, Ren K, Dubner R, Ennis M. Age-dependency of analgesia elicited by intraoral sucrose in acute and persistent pain models. Pain. 2002;97:93–103. doi: 10.1016/s0304-3959(02)00010-6. [DOI] [PubMed] [Google Scholar]
- 5.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 6.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 7.Brown AJ, Smith LT, Craighead LW. Appetite awareness as a mediator in an eating disorders prevention program. Eat Disord. 2010;18:286–301. doi: 10.1080/10640266.2010.490118. [DOI] [PubMed] [Google Scholar]
- 8.Brownell K. The LEARN Program for Weight Management. Dallas: The LifeStyle Company; 2000. [Google Scholar]
- 9.Christensen R, Astrup A, Bliddal H. Weight loss: the treatment of choice for knee osteoarthritis? A randomized trial. Osteoarthritis Cartilage. 2005;13:20–7. doi: 10.1016/j.joca.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59:739–44. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- 11.Der Ananian C, Wilcox S, Watkins K, Saunders R, Evans AE. Factors associated with exercise participation in adults with arthritis. J Aging Phys Act. 2008;16:125–43. doi: 10.1123/japa.16.2.125. [DOI] [PubMed] [Google Scholar]
- 12.Elfving B, Andersson T, Grooten WJ. Low levels of physical activity in back pain patients are associated with high levels of fear-avoidance beliefs and pain catastrophizing. Physiother Res Int. 2007;12:14–24. doi: 10.1002/pri.355. [DOI] [PubMed] [Google Scholar]
- 13.Foy CG, Lewis CE, Hairston KG, Miller GD, Lang W, Jakicic JM, Rejeski WJ, Ribisl PM, Walkup MP, Wagenknecht LE. Intensive lifestyle intervention improves physical function among obese adults with knee pain: findings from the Look AHEAD trial. Obesity (Silver Spring) 2011;19:83–93. doi: 10.1038/oby.2010.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gluck ME, Geliebter A, Hung J, Yahav E. Cortisol, hunger, and desire to binge eat following a cold stress test in obese women with binge eating disorder. Psychosom Med. 2004;66:876–81. doi: 10.1097/01.psy.0000143637.63508.47. [DOI] [PubMed] [Google Scholar]
- 15.Harrell FE. Regression Modeling Strategies. New York: Springer; 2001. [Google Scholar]
- 16.Hochberg MC. Radiographic features and functional status in rheumatoid arthritis. Arthritis Rheum. 1989;32:1340–1. doi: 10.1002/anr.1780321028. [DOI] [PubMed] [Google Scholar]
- 17.Hootman JM, Macera CA, Ainsworth BE, Addy CL, Martin M, Blair SN. Epidemiology of musculoskeletal injuries among sedentary and physically active adults. Med Sci Sports Exerc. 2002;34:838–44. doi: 10.1097/00005768-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Jenkinson CM, Doherty M, Avery AJ, Read A, Taylor MA, Sach TH, Silcocks P, Muir KR. Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial. BMJ. 2009;339:b3170. doi: 10.1136/bmj.b3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jordan JM, Luta G, Renner JB, Linder GF, Dragomir A, Hochberg MC, Fryer JG. Self-reported functional status in osteoarthritis of the knee in a rural southern community: the role of sociodemographic factors, obesity, and knee pain. Arthritis Care Res. 1996;9:273–8. doi: 10.1002/1529-0131(199608)9:4<273::aid-anr1790090412>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 20.Katz PP, Pasch LA, Wong B. Development of an instrument to measure disability in parenting activity among women with rheumatoid arthritis. Arthritis Rheum. 2003;48:935–43. doi: 10.1002/art.10990. [DOI] [PubMed] [Google Scholar]
- 21.Kazis LE, Meenan RF, Anderson JJ. Pain in the rheumatic diseases. Investigation of a key health status component. Arthritis Rheum. 1983;26:1017–22. doi: 10.1002/art.1780260811. [DOI] [PubMed] [Google Scholar]
- 22.Keefe FJ, Blumenthal J, Baucom D, Affleck G, Waugh R, Caldwell DS, Beaupre P, Kashikar-Zuck S, Wright K, Egert J, Lefebvre J. Effects of spouse-assisted coping skills training and exercise training in patients with osteoarthritic knee pain: a randomized controlled study. Pain. 2004;110:539–49. doi: 10.1016/j.pain.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 23.Keefe FJ, Caldwell DS, Williams DA, Gil KM, Mitchell D, Robertson C, Martinez S, Nunley J, Beckham JC, Crisson JD, Helms M. Pain coping skills training in the management of osteoarthritic knee pain: A comparative study. Behavior Therapy. 1990;21:49–62. [Google Scholar]
- 24.Keefe FJ, Caldwell DS, Williams DA, Gil KM, Mitchell D, Robertson C, Martinez S, Nunley J, Beckham JC, Helms M. Pain coping skills training in the management of osteoarthritic knee pain — II: Follow-up results. Behavior Therapy. 1990;21:435–47. [Google Scholar]
- 25.Keefe FJ, Lefebvre JC, Maixner W, Salley AN, Jr, Caldwell DS. Self-efficacy for arthritis pain: relationship to perception of thermal laboratory pain stimuli. Arthritis Care Res. 1997;10:177–84. doi: 10.1002/art.1790100305. [DOI] [PubMed] [Google Scholar]
- 26.Keefe FJ, Somers TJ. Psychological approaches to understanding and treating arthritis pain. Nat Rev Rheumatol. 2010;6:210–6. doi: 10.1038/nrrheum.2010.22. [DOI] [PubMed] [Google Scholar]
- 27.Keefe FJ, Van Horn Y. Cognitive-behavioral treatment of rheumatoid arthritis pain: maintaining treatment gains. Arthritis Care Res. 1993;6:213–22. doi: 10.1002/art.1790060408. [DOI] [PubMed] [Google Scholar]
- 28.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32:37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 31.March L, Amatya B, Osborne RH, Brand C. Developing a minimum standard of care for treating people with osteoarthritis of the hip and knee. Best Pract Res Clin Rheumatol. 2010;24:121–45. doi: 10.1016/j.berh.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Meenan RF, Gertman PM, Mason JH. Measuring health status in arthritis. The arthritis impact measurement scales. Arthritis Rheum. 1980;23:146–52. doi: 10.1002/art.1780230203. [DOI] [PubMed] [Google Scholar]
- 33.Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–9. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 34.Messier SP, Gutekunst DJ, Davis C, DeVita P. Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2005;52:2026–32. doi: 10.1002/art.21139. [DOI] [PubMed] [Google Scholar]
- 35.Messier SP, Loeser RF, Hoover JL, Semble EL, Wise CM. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehabil. 1992;73:29–36. [PubMed] [Google Scholar]
- 36.Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, Ettinger WH, Jr, Pahor M, Williamson JD. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50:1501–10. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 37.Messier SP, Loeser RF, Mitchell MN, Valle G, Morgan TP, Rejeski WJ, Ettinger WH. Exercise and weight loss in obese older adults with knee osteoarthritis: a preliminary study. J Am Geriatr Soc. 2000;48:1062–72. doi: 10.1111/j.1532-5415.2000.tb04781.x. [DOI] [PubMed] [Google Scholar]
- 38.Miller GD, Nicklas BJ, Davis C, Loeser RF, Lenchik L, Messier SP. Intensive weight loss program improves physical function in older obese adults with knee osteoarthritis. Obesity (Silver Spring) 2006;14:1219–30. doi: 10.1038/oby.2006.139. [DOI] [PubMed] [Google Scholar]
- 39.Nebel MB, Sims EL, Keefe FJ, Kraus VB, Guilak F, Caldwell DS, Pells JJ, Queen R, Schmitt D. The relationship of self-reported pain and functional impairment to gait mechanics in overweight and obese persons with knee osteoarthritis. Arch Phys Med Rehabil. 2009;90:1874–9. doi: 10.1016/j.apmr.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raymond NC, de Zwaan M, Faris PL, Nugent SM, Achard DM, Crosby RD, Mitchell JE. Pain thresholds in obese binge-eating disorder subjects. Biol Psychiatry. 1995;37:202–4. doi: 10.1016/0006-3223(94)00244-w. [DOI] [PubMed] [Google Scholar]
- 41.Rejeski WJ, Ettinger WH, Jr, Martin K, Morgan T. Treating disability in knee osteoarthritis with exercise therapy: a central role for self-efficacy and pain. Arthritis Care Res. 1998;11:94–101. doi: 10.1002/art.1790110205. [DOI] [PubMed] [Google Scholar]
- 42.Riecke BF, Christensen R, Christensen P, Leeds AR, Boesen M, Lohmander LS, Astrup A, Bliddal H. Comparing two low-energy diets for the treatment of knee osteoarthritis symptoms in obese patients: a pragmatic randomized clinical trial. Osteoarthritis Cartilage. 2010;18:746–54. doi: 10.1016/j.joca.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 43.Rosemann T, Kuehlein T, Laux G, Szecsenyi J. Factors associated with physical activity of patients with osteoarthritis of the lower limb. J Eval Clin Pract. 2008;14:288–93. doi: 10.1111/j.1365-2753.2007.00852.x. [DOI] [PubMed] [Google Scholar]
- 44.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 45.Somers TJ, Keefe FJ, Carson JW, Pells JJ, Lacaille L. Pain catastrophizing in borderline morbidly obese and morbidly obese individuals with osteoarthritic knee pain. Pain Res Manag. 2008;13:401–6. doi: 10.1155/2008/652453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Waters SJ, Riordan PA, Blumenthal JA, Mckee DC, LaCaille L, Tucker JN, Schmitt D, Caldwell DS, Kraus VB, Sims EL, Shelby RA, Rice JR. Pain Catastrophizing and Pain-Related Fear in Osteoarthritis Patients: Relationships to Pain and Disability. J Pain Symptom Manag. 2009;37:863–72. doi: 10.1016/j.jpainsymman.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spector TD, Hart DJ, Doyle DV. Incidence and progression of osteoarthritis in women with unilateral knee disease in the general population: the effect of obesity. Ann Rheum Dis. 1994;53:565–8. doi: 10.1136/ard.53.9.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Still CD, Benotti P, Wood GC, Gerhard GS, Petrick A, Reed M, Strodel W. Outcomes of preoperative weight loss in high-risk patients undergoing gastric bypass surgery. Arch Surg. 2007;142:994–8. doi: 10.1001/archsurg.142.10.994. discussion 9. [DOI] [PubMed] [Google Scholar]
- 49.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 50.Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology. 2007;132:2226–38. doi: 10.1053/j.gastro.2007.03.051. [DOI] [PubMed] [Google Scholar]
- 51.Zeni JA, Jr, Higginson JS. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: a result of altered walking speed? Clin Biomech (Bristol, Avon) 2009;24:372–8. doi: 10.1016/j.clinbiomech.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16:137–62. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]