ABSTRACT
BACKGROUND
Risk behaviors tend to cluster, particularly among smokers, with negative health effects. To optimize patients’ health and wellbeing, health care providers ideally would assess and intervene upon the multiple risks with which patients may present.
OBJECTIVE
This study examined medical students’ skills in assessing and treating multiple risk behaviors.
DESIGN
Using a randomized experimental design, medical students’ counseling interactions were evaluated with a standardized patient presenting with sexual health concerns and current tobacco use with varied problematic drinking status (alcohol-positive or alcohol-negative).
PARTICIPANTS
One hundred and fifty-six third-year medical students.
MAIN MEASURES
Student and standardized patient completed measures evaluated student knowledge, attitudes, and clinical performance.
KEY RESULTS
Overall, most students assessed tobacco use (85%); fewer assessed alcohol use (54%). Relative to the alcohol-negative case, students seeing the alcohol-positive case were less likely to assess sexually transmitted disease history (80% vs. 91%, p = 0.042), or patients’ readiness to quit smoking (41% vs. 60%, p = 0.025), and endorsed greater attitudinal barriers to tobacco treatment (p = 0.030). Patient satisfaction was significantly lower for the alcohol-positive than the alcohol-negative case; clinical performance ratings moderated this relationship.
CONCLUSIONS
When presented with a case of multiple risks, medical students performed less effectively and received lower patient satisfaction ratings. Findings were moderated by students’ overall clinical performance. Paradigm shifts are needed in medical education that emphasize assessment of multiple risks, new models of conceptualizing behavior change as a generalized process, and treatment of the whole patient for optimizing health outcomes.
KEY WORDS: multiple risk behaviors, medical education, training, standardized patients, alcohol, tobacco, sexual health
Risk behaviors, such as tobacco, alcohol misuse, and unsafe sexual practices often co-occur. Smokers, in particular, have poor behavioral profiles with about 90% engaging in multiple risks,1–4 and among individuals with alcohol problems, an estimated 56% also use tobacco.5 Both binge drinking and tobacco use during early adolescence predict higher levels of sexual risk taking into late adolescence, including early sexual intercourse, infrequent condom use, and sexually transmitted disease (STD) risk.6
Multiple risk behaviors have an additive or synergistic negative influence on health. With tobacco and alcohol use, the risk of head and neck cancers is multiplied.7,8 Smoking increases the risk of adverse cardiovascular events in women treated with combined hormonal contraceptives.9 Tobacco use also increases the risk of cervical cancer, infertility, painful and irregular menses, and early menopause.10
Health care providers are an important resource for health promotion. Physician advice doubles the likelihood of patients quitting smoking11, reduces problematic drinking12, and decreases the number of days that heavy drinking and unprotected sex occur13. Excess risks lead to excess costs, and effectively treating two behaviors in an individual reduces medical costs by about $2000 per year14. To optimize the health and wellbeing of patients, health care providers ideally would assess and intervene upon the multiple risks with which patients present. With alcohol and tobacco, observational studies have documented that continued smoking is associated with worse alcohol treatment outcomes15, while quitting smoking predicts improved sobriety16–19. Counter to clinical concerns that intervening on smoking may compromise sobriety, a meta-analysis of 19 randomized controlled trials with clients in addictions treatment or recovery found tobacco treatment interventions were associated with a 25% increased likelihood of long-term abstinence from alcohol and illicit drugs20.
Medical student performance provides an indication of how well medical schools are preparing future doctors. We previously found that third-year medical students were skilled at identifying patients’ tobacco use and tailored their interventions based on patients’ readiness to quit21. The current randomized controlled study extends this work to evaluate student performance with a standardized patient with sexual health concerns and current tobacco use that varied on problematic drinking status (alcohol-positive or alcohol-negative). The patient case was designed to be realistic in the cluster of issues presented and provide an evaluation of the approach to multiple risks. To our knowledge, this is the first study to examine student physician attitudes and behaviors in treating tobacco dependence among smokers presenting with multiple risks.
METHOD
Setting
The study occurred at the University of California, San Francisco (UCSF) School of Medicine. The curriculum covered sexual risk behaviors, tobacco use, and alcohol use in separate training blocks delivered by different faculty groups (Textbox 1).
Textbox 1. Medical School Curriculum Content on Sexual Risk Behaviors, Tobacco, & Alcohol
Procedures
The study was conducted in November/December 2010 during the mini-clinical performance examination (mini-CPX), a required, formative SP assessment conducted mid-way through the third year. SPs can simulate clinical situations realistically and consistently and have been employed in many medical schools to teach and evaluate clinical skills22,23.
During the mini-CPX, each student saw three SPs in 17-minute encounters and completed a 10-minute online written exercise (interstation exercise) immediately following each encounter. In one case, a 28-year-old woman concerned about a recent pregnancy scare and requesting a prescription for the birth control pill was a current smoker. The case presented the students with an opportunity to offer smoking cessation counseling.
Textbox 2 provides a brief description of the two study case versions. In one version, the patient reported limited alcohol use. In the other, the patient reported heavy alcohol use. If students failed to assess alcohol use, alcohol-positive patients were instructed to reveal their problematic alcohol use to ensure that the case versions were distinct.
Textbox 2. Standardized Patient Case Profile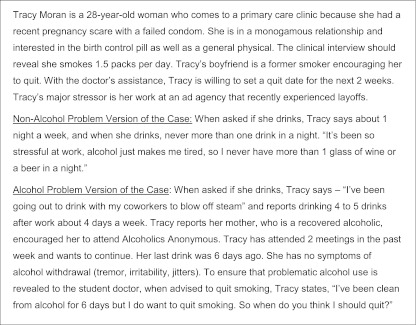
Students were randomly assigned to case version and not informed that two versions were used or that the case addressed smoking cessation. The three female actors portraying the case received 15 hours of training on case presentation, checklist completion, smoking health effects, and tobacco treatment research in patients with substance use problems. All three actors played both case versions on different days.
Sample
Participants were third-year medical students, mid-way through their core clerkships. During the mini-CPX orientation, the students were informed of the study described as an examination of student performance with disease assessment and prevention. The UCSF Institutional Review Board approved the study. All students were required to complete the SP case and interstation exercise as a routine part of the miniCPX; informed consent to analyze student responses and performance ratings was requested at the interstation exercise following the patient encounter. All measures were computer-administered with no missing data on any of the items.
Standardized Patient Completed Measures
A checklist evaluated student assessment of the patient’s sexual health history (3-items) and frequency and amount of alcohol use (1-item), credited only if the student initiated assessment of the patient’s alcohol use. Tobacco treatment (5-items), based on the 5-A’s framework24, credited students for: 1) asking about tobacco use and amount; 2) advising about the health benefits of quitting or health risks of smoking on hormonal birth control; 3) assessing readiness to quit smoking; 4) assisting with quitting (i.e., setting a quit date in 2 weeks, recommending cessation pharmacotherapy, encouraging coping strategies other than smoking for dealing with stress, referring to a smoking cessation quitline/program); and 5) arranging a follow-up visit. Tobacco treatment performance was evaluated as the percent correct out of 5 points, internal consistency Cronbach’s alpha = 0.77.
Clinical performance (11-items) was evaluated using an adaptation of the SEGUE Framework25. Using a 3-point rating scale of “strongly agree” (1.00), “agree” (0.75), and “disagree” (0), SPs evaluated students’ demonstrated empathy and respect, information gathering, active listening, exploration of the patient’s perspective, development of personal rapport, meeting of patient’s needs, and involvement of the patient in treatment planning (Cronbach’s alpha = 0.80 for the total scale score evaluated as the percent credited out of 11 possible points). The items in the SEGUE were designed to be low inference and objective, such that raters would be able to identify whether the behavior was performed or not, thereby eliminating the need for a middle rating of 0.50. The distinction between 0.75 and 1.00 on the scale is meant to capture the minority of students with exceptional performance on the item.
Patient satisfaction (1-item) assessed whether the patient would, based on her level of satisfaction, return to see this student physician again, coded as agree (1) or disagree (0). Narrative feedback provided by the SPs was open-ended, brief, and evaluative concerning students’ overall performance. This feedback was coded for thematic content by two study authors (KG and JJP) without knowledge of case version.
Student Completed Measures
Three multiple-choice items assessed students’ tobacco treatment knowledge of unassisted quit attempt success rates, smoking prevalence, and readiness to quit smoking among smokers with substance use problems. A fourth item had the students identify the patient’s stage of change. Attitudes toward treating tobacco dependence in smokers with addiction problems (four items) were assessed with a 5-point Likert scale ranging from strongly agree (1) to strongly disagree (0) (sample item: patients with alcohol or drug problems should work on their substance use issues before quitting smoking). The knowledge and attitudinal items had demonstrated sensitivity to training effects previously26.
Analyses
Descriptive analyses summarized survey responses. Differences in student performance were examined by patient case version. Initial analyses tested differences in measured variables by patient actor. When significant, partial correlations and logistic regressions were run to examine associations among the constructs controlling for patient actor, entered as a categorical variable and represented by dummy codes. In logistic regressions, the Wald statistic was used to assess the significance of a single variable or coefficient. Patient satisfaction was examined in relation to patient case version and clinical performance both in univariate analyses and in a mediation analysis. For the mediation analysis, we entered the variables in two separate steps and examined the influence of clinical performance on the change in standardized beta weights of patient case version in predicting patient satisfaction27.
RESULTS
Sample Descriptives
Of the 168 miniCPX students, 156 agreed to have their data used for the study (93% participation rate). The sample was 55% female, 26% of underrepresented minority, with a mean age of 27.3 years (SD = 2.7), and representative of the UCSF third-year medical school class (p > 0.50 for tests of comparison on measured demographics). Nearly half the sample (n = 75, 48%) interviewed the patient with alcohol problems. The three actors were assigned to both case versions equally with no difference in assignment, χ2(2) = 2.34, p = 0.310.
Behavioral Assessment and Interaction
Table 1 summarizes student performance in the counseling interaction overall and by case version. While most students (>80%) assessed the patient’s sexual health history and discussed options for birth control, students’ assessment of prior STDs (80% vs. 91%) and birth control use (88% vs. 98%) were significantly lower with the alcohol-positive rather than the alcohol-negative case. Just over half (54%) of students assessed alcohol use and amount without prompting by the patient, with no difference by case version.
Table 1.
Combined and Case-Specific Scoring for Standardized Patient Exam
| Case Version | Group comparison p-value | |||
|---|---|---|---|---|
| Alcohol Negative n = 81 | Alcohol Positive n = 75 | Overall N = 156 | ||
| Assessed history of sexually transmitted diseases | 91% | 80% | 86% | 0.042 |
| Assessed history of prior birth control use | 98% | 88% | 93% | 0.020 |
| Discussed options for birth control use | 89% | 81% | 85% | 0.167 |
| Asked patient about alcohol use and amount | 54% | 53% | 54% | 0.902 |
| Asked patient about tobacco use and amount | 85% | 84% | 85% | 0.838 |
| Advised patient of health benefits of quitting or the risks of using hormonal birth control while smoking | 88% | 81% | 85% | 0.274 |
| Assessed patient’s readiness to quit smoking | 60% | 41% | 51% | 0.025 |
| Assisted patient with quitting smoking* | 75% | 67% | 71% | 0.234 |
| Scheduled a follow up visit to re-evaluate patient’s tobacco use or quit attempt | 33% | 36% | 35% | 0.726 |
| Tobacco treatment summary score: M (SD) | 56% (0.28) | 51% (0.30) | 53% (0.29) | 0.247 |
| Clinical performance summary score: M (SD) | 84% (0.11) | 81% (0.13) | 83% (0.12) | 0.173 |
| Would return to see this doctor again | 95% | 84% | 90% | 0.023 |
*Credit for assistance included either setting a quit date within 2 weeks, recommending cessation pharmacotherapy, encouraging alternative coping strategies for stress and anxiety, or referring to a quit smoking program, quitline or other support group
Most students asked about tobacco use (85%), advised patients to quit (85%), and provided assistance with quitting (71%). Students encountering the alcohol-positive case, however, were significantly less likely to assess patients’ readiness to quit smoking than students working with the alcohol-negative case (41% vs. 60%). Controlling for patient actor effects in a logistic regression, case version remained a significant predictor of assessment of readiness to quit (Wald = 7.20, df = 1, p = 0.007). Few students arranged follow-up to assess progress with quitting smoking (35%). Students achieved a mean of 53% (SD = 0.29) of possible points for tobacco treatment interventions, with no difference by case version.
Student Tobacco Treatment Knowledge
Students averaged 42% correct (SD = 0.21; range: 0% to 100%) on the knowledge items. Greater knowledge was significantly correlated with tobacco treatment performance scores, r = 0.17, p = 0.034. Overall knowledge scores did not differ by patient case version: (48% [SD = 0.20] for the alcohol-positive case vs. 40% [SD = 0.21] for alcohol-negative, p = 0.124). Students seeing the alcohol-positive case, however, were less likely to view smokers with alcohol problems as comparable in readiness to quit to the general population, χ2(3) = 8.27, p = 0.041. Only 24% of students correctly identified the SP’s stage of change for quitting smoking as preparation (ready to quit within 30 days); 6% of students staged the patient in contemplation and 49% in precontemplation; 21% stated they did not know or assess the patient’s stage of change. Fewer students seeing the alcohol-positive case correctly staged the patient in preparation (19%) relative to the alcohol-negative case (30%), but the difference was not statistically significant, χ2(1) = 2.54, p = 0.111; there was no difference by patient actor. Failure to correctly identify patients as in preparation was associated with significantly lower tobacco treatment performance scores, M = 48% (SD = 0.29) vs. 69% (SD = .23), F(1,155) = 15.77, p < 0.001, and lower likelihood of working to set a quit date within 2 weeks, M = 18% vs. 34%, χ2(1) = 4.54, p = 0.033, relative to students who correctly staged the patient in preparation.
Student Attitudinal Barriers
The overall mean sum score for the attitudinal barrier items was 1.17 (SD = 0.66) out of 4, indicating low levels of agreement. Students encountering the alcohol-positive patient, however, had significantly greater agreement with the barriers to treatment (M = 1.29, SD = 0.68) than students encountering the alcohol-negative patient (M = 1.06, SD = .62), F(1,155) = 4.79, p = 0.030. Higher attitudinal barriers were significantly correlated with lower tobacco treatment performance (r = −0.17, p = 0.033) and poorer tobacco treatment knowledge (r = −0.20, p = 0.011).
Counseling Interaction
Students averaged 83% (SD = 0.11) on the clinical performance score, with highest scores on maintaining a respectful tone (M = 89%, SD = 0.14) and lowest on reviewing next steps with the patient (M = 71%, SD = 0.31). Clinical performance scores differed significantly by patient actor, F(2,155) = 67.24, p < 0.001. In a partial correlation, controlling for patient actor, clinical performance scores were significantly associated with case version (partial r = −0.26, p < 0.001) and indicated lower scores for the alcohol-positive patient. Clinical performance was not significantly correlated with tobacco treatment attitudes (partial r = −0.15, p = 0.068) or knowledge (partial r = 0.14, p = 0.080).
Patient Satisfaction
Patient satisfaction in reported willingness to return to see the student doctor differed significantly by actor, χ2(2) = 8.47, p = 0.015. In a logistic regression, controlling for actor, patient satisfaction was significantly lower for the alcohol-positive than the alcohol-negative case, Wald = 5.32, df = 1, p = 0.021. Controlling for patient actor, patient satisfaction also was significantly correlated with attitudinal barriers (r = −0.19, p = 0.016), tobacco treatment scores (r = 0.19, p = 0.021), and clinical performance (r = 0.49, p < 0.001), but not tobacco treatment knowledge (r = 0.04, p = 0.667).
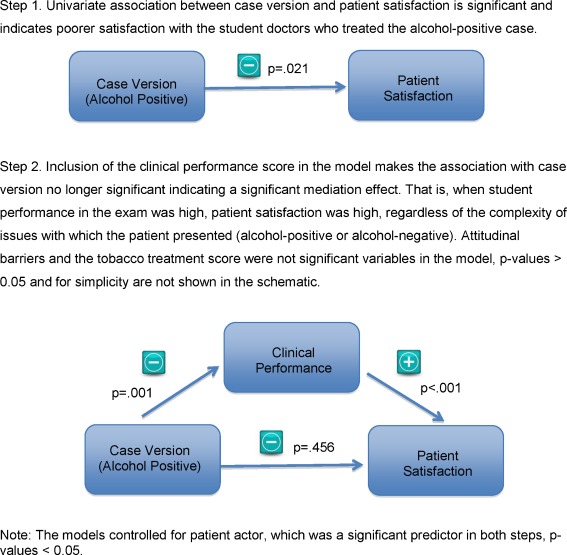
We explored mediators of the relationship between patient case version and patient satisfaction using logistic regression analysis (Fig. 1). The change in significance for case version as a predictor of patient satisfaction (step 1) with the inclusion of the clinical performance score (step 2) indicated a significant mediation effect. Attitudinal barriers and tobacco treatment scores did not add significantly to the mediation model, p-values > 0.05.
Figure 1.
Test of mediation in patient satisfaction with student physician.
Narrative Feedback
The actors’ narrative feedback from the patient perspective to the students revealed that 38% of students adequately addressed patients’ tobacco use. Students who did not adequately address patients’ tobacco use failed to demonstrate competency for treating tobacco dependence (9%), discouraged quitting during early alcohol recovery (3%), ran out of time (10%), or failed to address next steps with quitting (41%). Type of feedback provided did not vary by patient actor, χ2(8) = 8.99, p = 0.343. A chi-square test for differences by patient case version, however, was significant, χ2(4) = 11.57, p = 0.021, and indicated that students seeing the alcohol-positive case were more likely to run out of time (18% vs. 3%) and voice concerns about quitting smoking and alcohol simultaneously (6% vs. 0%) relative to students seeing the alcohol-negative case.
DISCUSSION
Health behavior change efforts are viewed as paramount for a sustainable health care system28. In an SP evaluation, just over half of our student sample was assessed for problematic alcohol use, far less than the proportion asking about tobacco. Students seeing the alcohol-positive case were less likely to ask about prior birth control and STD history. They also were less likely to identify that smokers with alcohol problems are as ready to quit smoking as the general population, and they endorsed more attitudinal barriers to treating tobacco dependence in smokers with substance use problems. Greater perceived barriers were associated with less attention to tobacco use with the patient. These findings suggest the need for training on assessment and management of the multiple risks with which patients present.
Notably, students’ screening rates for multiple risk behaviors were comparable to reports in the literature for surveys with general practitioners and recently trained and experienced family physicians29,30. On average, however, students addressed fewer than three of the recommended 5-A's of tobacco treatment. Tobacco treatment training specifically needs to emphasize the identification of patients ready to quit smoking and the provision of active interventions as less than one in four students in our study encouraged the patient to set a quit date. Attention to follow-up planning also is needed.
Although clinical performance ratings for communication were high for all students, patient satisfaction, expressed as willingness to continue treatment with the student doctor, was significantly lower for the alcohol-positive than the alcohol-negative case. Clinical performance ratings moderated the relationship between patient case version and patient satisfaction. That is, when student performance in the exam was high, patient satisfaction was high, regardless of the complexity of issues with which the patient presented (alcohol-positive or alcohol-negative).
The findings also likely reflect the systems problem of insufficient time to evaluate multiple issues in medical practice. It is noteworthy that 18% of students with the alcohol-positive case ran out of time, compared with only 3% of those with the alcohol-negative case. The miniCPX patient encounter was limited to 15 minutes, which mirrors the standard primary care visit in practice and likely is not adequate for addressing the multiple risks with which patients present. Analysis of 46,250 adult visits to primary care physicians from 1997–2005 in the National Ambulatory Medical Care Survey identified the median visit duration as 15 minutes; visits that provided appropriate behavioral counseling (in this case, for diet and exercise) averaged 2.6 to 4.2 minutes longer per risk behavior addressed.31 Training on effective time management and agenda setting is critical for facilitating students’ attention to multiple risks.
Students who saw the alcohol-positive case also were more likely to voice concerns about quitting smoking and alcohol concurrently than students who saw the alcohol-negative case. Provider training needs to cover the synergistic benefits of treating multiple risks and effective models for supporting, rather than overwhelming, patients with multiple behavior change goals.
The current study is limited to one training site, with a single SP encounter, and may not generalize to other programs. To our knowledge, the amount of curriculum time our medical school dedicated to behavioral risks is likely on average to other medical schools. Schools with a greater emphasis on behavioral health issues may expect better student performance. Tobacco-related knowledge and attitudes were assessed only following the patient encounter to avoid priming the students that the case was tobacco-related. It is possible, though unlikely given the randomized design, that student group differences found by patient case version were pre-existing. Assessment of student knowledge and attitudes for addressing sexual health and alcohol concerns would have been valuable; however, time constraints limited the number of items and areas that could be assessed. Strengths of the study include the 93% student participation rate and use of SPs, which allow for assessment of skills in a clinically realistic, natural learning setting in a standardized manner. Despite intensive training and supervision, patient actor differences were identified and controlled for in tests of associations.
In closing, it is worth noting that the curriculum for students in the current study covered assessment and treatment of sexual health concerns, tobacco, and alcohol in separate modular blocks rather than from an integrative model of health behavior change, and there was minimal communication between faculty leading the different areas. This siloed approach is characteristic of traditional medical training and behavioral research fields more broadly32. The study findings support the need for paradigm shifts in medical education, both in didactics and clinical practice opportunities, that emphasize assessment of multiple risks, new models of conceptualizing behavior change as a generalized process, and treatment of the whole patient for optimizing health outcomes.
Acknowledgements
This work was supported by the National Institute on Drug Abuse (#K23 DA018691 and #P50 DA09253), the State of California Tobacco-Related Disease Research Program (#17RT-0077), and the National Institute of Mental Health (#R01 MH083684). We thank Jewel Smally and Ann Homan for overseeing the patient-actors and survey data collection; Patricia Donnellan, MPH, Rachel Grana, PhD, Norval Hickman, PhD, MPH, Romina Kim, and Nicholas Orozco for assisting with training the standardized patient actors; the standardized patient actors Chloe Bronzan, Audra Wolfman, and Linnea George-Kupfer; and Kevin Delucchi, PhD, for his consultation on statistical analyses.
Conflicts of Interest
None disclosed.
References
- 1.Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. Am J Prev Med. 2004;27(2 Suppl):18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 2.Klesges RC, Eck LH, Isbell TR, Fulliton W, Hanson CL. Smoking status: effects on the dietary intake, physical activity, and body fat of adult men. Am J Clin Nutr. 1990;51(5):784–9. doi: 10.1093/ajcn/51.5.784. [DOI] [PubMed] [Google Scholar]
- 3.Pronk NP, Anderson LH, Crain AL, et al. Meeting recommendations for multiple healthy lifestyle factors. Prevalence, clustering, and predictors among adolescent, adult, and senior health plan members. Am J Prev Med. 2004;27(2 Suppl):25–33. doi: 10.1016/j.amepre.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 4.Kendzor DE, Costello TJ, Li Y, et al. Race/ethnicity and multiple cancer risk factors among individuals seeking smoking cessation treatment. Cancer Epidemiol Biomark Prev. 2008;17(11):2937–45. doi: 10.1158/1055-9965.EPI-07-2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA. 2000;284(20):2606–10. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 6.Wu J, Witkiewitz K, McMahon RJ, Dodge KA. A parallel process growth mixture model of conduct problems and substance use with risky sexual behavior. Drug Alcohol Depend. Oct 1;111(3):207–214. [DOI] [PMC free article] [PubMed]
- 7.Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48(11):3282–7. [PubMed] [Google Scholar]
- 8.Xu WH, Zhang XL, Gao YT, et al. Joint effect of cigarette smoking and alcohol consumption on mortality. Prev Med. 2007;45(4):313–9. doi: 10.1016/j.ypmed.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burkman R, Schlesselman JJ, Zieman M. Safety concerns and health benefits associated with oral contraception. Am J Obstet Gynecol. 2004;190(4 Suppl):S5–22. doi: 10.1016/j.ajog.2004.01.061. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services. Women and Smoking—A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2001
- 11.Bao Y, Duan N, Fox SA. Is some provider advice on smoking cessation better than no advice? An instrumental variable analysis of the 2001 National Health Interview Survey. Health Serv Res. 2006;41(6):2114–35. doi: 10.1111/j.1475-6773.2006.00592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557–68. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- 13.Velasquez MM, Sternberg K, Johnson DH, Green C, Carbonari JP, Parsons JT. Reducing sexual risk behaviors and alcohol use among HIV-positive men who have sex with men: a randomized clinical trial. J Consult Clin Psychol. 2009;77(4):657–67. doi: 10.1037/a0015519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edington DW. Emerging research: a view from one research center. Am J Health Promot. 2001;15(5):341–9. doi: 10.4278/0890-1171-15.5.341. [DOI] [PubMed] [Google Scholar]
- 15.Frosch DL, Shoptaw S, Nahom D, Jarvik ME. Associations between tobacco smoking and illicit drug use among methadone-maintained opiate-dependent individuals. Exp Clin Psychopharmacol. 2000;8(1):97–103. doi: 10.1037/1064-1297.8.1.97. [DOI] [PubMed] [Google Scholar]
- 16.Bobo JK, McIlvain HE, Lando HA, Walker RD, Leed-Kelly A. Effect of smoking cessation counseling on recovery from alcoholism: findings from a randomized community intervention trial. Addiction. 1998;93(6):877–87. doi: 10.1046/j.1360-0443.1998.9368779.x. [DOI] [PubMed] [Google Scholar]
- 17.Shoptaw S, Jarvik ME, Ling W, Rawson RA. Contingency management for tobacco smoking in methadone-maintained opiate addicts. Addict Behav. 1996;21(3):409–12. doi: 10.1016/0306-4603(95)00066-6. [DOI] [PubMed] [Google Scholar]
- 18.Hughes JR. Possible effects of smoke-free inpatient units on psychiatric diagnosis and treatment. J Clin Psychiatry. 1993;54(3):109–14. [PubMed] [Google Scholar]
- 19.Kohn CS, Tsoh JY, Weisner CM. Changes in smoking status among substance abusers: baseline characteristics and abstinence from alcohol and drugs at 12-month follow-up. Drug Alcohol Depend. 2003;69(1):61–71. doi: 10.1016/S0376-8716(02)00256-9. [DOI] [PubMed] [Google Scholar]
- 20.Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. J Consult Clin Psychol. 2004;72(6):1144–56. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- 21.Prochaska JJ, Teherani A, Hauer KE. Medical students’ use of the stages of change model in tobacco cessation counseling. J Gen Intern Med. 2007;22(2):223–7. doi: 10.1007/s11606-006-0040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Furman GE. The role of standardized patient and trainer training in quality assurance for a high-stakes clinical skills examination. Kaohsiung J Med Sci. 2008;24(12):651–5. doi: 10.1016/S1607-551X(09)70031-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jerant A, Kravitz RL, Azari R, et al. Training residents to employ self-efficacy-enhancing interviewing techniques: randomized controlled trial of a standardized patient intervention. J Gen Intern Med. 2009;24(5):606–13. doi: 10.1007/s11606-009-0946-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fiore MC, Jaen CR, Baker TB.Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service 2008
- 25.Makoul G. The SEGUE Framework for teaching and assessing communication skills. Patient Educ Couns. 2001;45(1):23–34. doi: 10.1016/S0738-3991(01)00136-7. [DOI] [PubMed] [Google Scholar]
- 26.Prochaska JJ, Fromont SC, Leek D, et al. Evaluation of an evidence-based tobacco treatment curriculum for psychiatry residency training programs. Acad Psychiatry. 2008;32(6):484–92. doi: 10.1176/appi.ap.32.6.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 28.Schroeder SA. We Can Do Better — Improving the Health of the American People. N Engl J Med. 2007;357:1221–8. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 29.Haley N, Maheux B, Rivard M, Gervais A. Lifestyle health risk assessment. Do recently trained family physicians do it better? Can Fam Physician. 2000;46:1609–16. [PMC free article] [PubMed] [Google Scholar]
- 30.Maheux B, Haley N, Rivard M, Gervais A. Do physicians assess lifestyle health risks during general medical examinations? A survey of general practitioners and obstetrician-gynecologists in Quebec. CMAJ. 1999;160(13):1830–4. [PMC free article] [PubMed] [Google Scholar]
- 31.Chen LM, Farwell WR, Jha AK. Primary care visit duration and quality: does good care take longer? Arch Intern Med. 2009;169(20):1866–72. doi: 10.1001/archinternmed.2009.341. [DOI] [PubMed] [Google Scholar]
- 32.Prochaska JO. Multiple Health Behavior Research represents the future of preventive medicine. Prev Med. 2008;46(3):281–5. doi: 10.1016/j.ypmed.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 33.Hudmon KS, Corelli RL, Chung E, et al. Development and implementation of a tobacco cessation training program for students in the health professions. J Cancer Educ Fall. 2003;18(3):142–9. doi: 10.1207/S15430154JCE1803_07. [DOI] [PubMed] [Google Scholar]