ABSTRACT
BACKGROUND
Minority populations receive a lower quality healthcare in part due to the inadequate assessment of, and cultural adaptations to meet, their culturally informed healthcare needs. The seven million American Muslims, while ethnically and racially diverse, share religiously informed healthcare values that influence their expectations of healthcare. There is limited empirical research on this community’s preferences for cultural modifications in healthcare delivery.
OBJECTIVE
Identify healthcare accommodations requested by American Muslims.
METHODS
Using community-based participatory research (CBPR) methods, we partnered with four community organizations in the Greater Detroit area to design and conduct thirteen focus groups at area mosques serving African American, Arab American, and South Asian American Muslims. Qualitative content analysis utilized a framework team-based approach.
KEY RESULTS
Participants reported stigmatization within the healthcare system and voiced the need for culturally competent healthcare providers. In addition, they identified three key healthcare accommodations to address Muslim sensitivities: the provision of (1) gender-concordant care, (2) halal food and (3) a neutral prayer space. Gender concordance was requested based on Islamic conceptions of modesty and privacy. Halal food was deemed to be health-promoting and therefore integral to the healing process. Lastly, a neutral prayer space was requested to ensure security and privacy during worship.
CONCLUSIONS
This study informs efforts to deliver high-quality healthcare to American Muslims in several ways. We note three specific healthcare accommodations requested by this community and the religious values underlying these requests. Healthcare systems can further cultural sensitivity, engender trust, and improve the healthcare experiences of American Muslims by understanding and then attempting to accommodate these values as much as possible.
KEY WORDS: cultural modifications, Islam, minority health, healthcare delivery
BACKGROUND
Minority patient populations experience multiple challenges during clinical encounters, thus influencing the quality of care they receive.1,2 Differences between the patient and provider in language, cultural and medical values, as well as economic or social circumstances, may present obstacles. At a more macro-level, hospital-level services such as spiritual care departments and food services also influence the quality of the healthcare experience. Both the quality of patient–provider relationships and healthcare system services may then affect healthcare-seeking patterns and contribute to population-level healthcare disparities.
In discussions of healthcare quality, cultural competence and patient-centered care are championed as means to reduce healthcare disparities by improving how patients are cared for within the healthcare system. Cultural competence is a “set of congruent behaviors, attitudes, and policies that come together in a system, agency, or amongst professionals and enables them to work effectively in cross-cultural situations.”3,4 Integral to cultural competence is the “capacity to identify, understand, and respect the values and beliefs of others.”5 Cultural competence training improves provider attitudes toward minority patients, enhances cross-cultural communication skills, and fosters more stable therapeutic alliances.5 At a system-level, cultural competency programs along with patient-centered models of care ensure that patient values are respected and that medical complications stemming from cultural differences are reduced through reasonable healthcare accommodations.5,6
Little is known about healthcare disparities facing American Muslims and about the type of cultural tailoring of healthcare desired by this community. Although there are an estimated seven million Muslims in the US bound together by a shared religious tradition that informs cultural values around healthcare, the community is comprised of multiple ethnic groups that each have their own immigration history.7–10 Thus, the few empirical medical studies conducted within this community largely focus on specific subgroups and often overlook the influence of their shared religion in the patterning of health behaviors. To address this gap in knowledge, we delineate healthcare accommodations requested by American Muslims of different ethnic and national backgrounds and the values underpinning these requests. We define healthcare accommodations as adaptations made by the healthcare system in the manner or structure of healthcare delivery that respond to patient cultural or religious values. Understanding and addressing these patient values and needs may positively influence both healthcare experiences and future healthcare-seeking behaviors.
METHODS
Setting
We conducted this study in the greater metropolitan Detroit area, home to one of the longest-standing and largest populations of American Muslims in the United States, estimated to number around 200,000 persons.11–13
Design
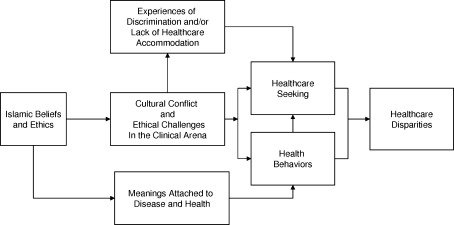
Our study utilized a conceptual model drawn from a series of models that considered the influences of culture and discrimination upon health behaviors and healthcare disparities (Fig. 1). Illustratively, Kleinman’s “cultural construction(s) of clinical reality” speaks to the illness experience being shaped by cultural factors governing perception, labeling, explanation, and valuation of the experience, and by processes embedded in family, social, and cultural bonds.14 Thus, illness is socio-culturally constructed. In this vein, Islam is tied to health through its influence upon Muslim culture, as religious values attach meaning to health and disease as well as health-related experiences and influence cultural practices that manifest in health and healthcare-seeking behaviors. Leiniger’s cultural care theory further notes that when patients experience healthcare that is incongruent to their values, the healthcare encounter becomes fraught with cultural conflicts and ethical dilemmas.15 Thus, Muslim patients may have religiously informed expectations of the healthcare encounter which if inadequately assessed or accommodated create poor clinical experiences or are perceived as discrimination. These experiences may then lead to delayed healthcare-seeking or altered health behaviors. Thus, as supported by the Institute of Medicine’s seminal report entitled “Unequal Treatment”, mistrust in the healthcare system, prior experiences of discrimination and lack of clinical accommodation affect patient health experiences and healthcare-seeking behaviors.16 We posit that these mechanisms also play a role in potential healthcare disparities amongst American Muslims.
Figure 1.
Synthesized conceptual model of the influence of islam upon muslim healthcare behaviors and healthcare disparities.
We used a community-based participatory research model and partnered with four community organizations in the area: two umbrella organizations representing 35 Muslim organizations including 25 mosques, an American Muslim policy institute, and an Arab community health organization. Representatives from these organizations, along with a multidisciplinary investigative team, comprised a steering committee that guided all phases of the project.17 This project was approved by the University of Michigan Institutional Review Board.
Sampling and Data Collection
Between December 2009 and March 2010, we conducted 13 focus groups with adults at seven mosques within the Greater Detroit-area chosen purposefully to achieve representation of both male and female Arab Americans, South Asian Americans, and African Americans. As our aim was to better understand the religious influences on healthcare, mosque-based recruitment was chosen as a proxy for self-identification with Islam and a base level of religiosity among participants. Each mosque governed the manner in which recruitment occurred; thus, a variety of methods including advertisements and announcements at mosques, flyers on community boards and listservs, and personal contact by mosque representatives were employed. Focus groups lasted approximately 1.5 hours and were segmented by gender and language (Arabic vs. English), and moderated by a multi-lingual, gender-concordant member of the investigative team. At the conclusion of the focus group, participants were asked to consider changes they would make in the healthcare setting to improve the Muslim healthcare experience and then to decide on the top three healthcare accommodations from the list generated.
Data Analysis
Interviews were audio-recorded and transcribed verbatim. As respondents mixed Arabic and English, Arabic terms were translated by a bilingual team member and verified for accuracy by a second bilingual team member. The one focus group conducted entirely in Arabic was translated by a professional translation company and verified for accuracy by a bilingual team member. Qualitative content analysis utilized a framework team-based approach facilitated by the QSR NVivo 8 software (QSR International, 2009). Common themes were identified by drawing on principles of grounded theory, including constant comparison of participant responses and inductive identification of themes from the data using a team-based approach. An iterative inductive coding process was utilized by four team members, and disagreements were resolved through consensus building team meetings. Two analysts (AK and KG) compiled a list of the top three accommodations selected by each focus group across healthcare settings. Where focus groups combined one or more accommodations into a single larger category, these were decoupled in order to correctly tally accommodations, and where different terms were used to denote the same accommodation, a singular term was used. The most commonly appearing accommodations were grouped thematically during team meetings while reviewing focus group transcripts for the rationale behind the accommodation requests. For further rigor, we reviewed transcripts to enumerate healthcare accommodations that were mentioned but did not make the top-three designation. The three most commonly mentioned healthcare accommodations which were also amongst the top-three accommodations are reported below (Table 1). The validity of our findings is enhanced by rigorous codebook development, the use of a group consensus process that included reflexive discussion of the data to develop findings, and by employing a multi-disciplinary research team including community members.
Table 1.
Healthcare Accommodations Most Commonly Identified in Focus Groups*
| Focus Group Number | Gender Concordant Care* | Halal Food† | Neutral Space for Prayer‡ | Muslim Social Services | Interpreters and other Language Resources |
|---|---|---|---|---|---|
| FG 1 | X | X | X | ||
| FG 2 | X | X | X | X | X |
| FG 3 | X | X | X | X | |
| FG 4 | X | X | X | X | X |
| FG 5 | X | X | X | ||
| FG 6 | X | X | X | X | |
| FG 7 | X | X | |||
| FG 8 | X | X | X | X | |
| FG 9 | X | X | X | ||
| FG 10 | X | X | X | ||
| FG 11 | X | ||||
| FG 12 | X | X | X | ||
| FG 13 | X | X | X | X | X |
| Totals | 12 | 12 | 11 | 6 | 4 |
*Healthcare accommodations are grouped thematically, and those reported in only 1 or 2 focus groups are not included.
*was noted as a top-three accommodation in 11/13 focus groups
† was noted as a top-three accommodation in 10/13 focus groups
‡ was noted as a top-three accommodation in 3/13 focus groups
RESULTS
Demographics
Table 2 provides an overview of the relevant characteristics of focus group participants. Seven female and six male focus groups were held with between four and twelve participants. Four groups contained predominately Arab participants, three hosted mainly South Asian respondents, and two comprised of only African American participants. The remaining four focus groups consisted of participants of two or more ethnicities.
Table 2.
Demographic Characteristics of Participants (N = 102)
| Demographic Characteristics | Frequency (%)* |
|---|---|
| Sex | |
| Female | 56 (54.9) |
| Age | |
| Mean (Range) | 44.69 (18-75) |
| Ethnicity | |
| Arab American/Arab | 43 (43) |
| South Asian | 23 (23) |
| African American/Black | 22 (22) |
| Islamic Denomination | |
| Sunni | 81 (81.8) |
| Shi’ite | 7 (7.1) |
| Education Level | |
| Bachelors or Above | 53 (54.1) |
| Some college | 27 (27.6) |
| High school diploma/GED or less | 18 (18.4) |
| Have Health Insurance | |
| Yes | 76 (78.4) |
*Row totals may not sum to 102 due to missing data
Cultural Competence
Healthcare accommodations, i.e. cultural adaptations that would make patients more comfortable in the healthcare setting, were discussed in the context of advancing patient-centered and culturally sensitive care. In nearly all of the focus group discussions, participants discussed the importance of cultural competency programming and used multiple terms interchangeably as they described the need for “cultural sensitivity,” “cultural awareness,” and “cultural sensitivity training.” Participants hoped that cultural competency programs would lead to (1) a greater understanding of Islam and Muslim culture, thus strengthening the patient–provider relationship as providers are more attuned to patient values and practices, and (2) improved Muslim experiences within the healthcare system as culturally sensitive adaptations would reduce barriers to, and challenges within, healthcare.
During these discussions, participants highlighted their experiences with providers who lacked knowledge about and respect for their Islamic faith. “A lot of doctors ask really basic things and you’re kind of like . . . they should already (know) that stuff…” one participant complained, while another added, “It’s not as if the patient . . . has to say . . . pay attention, I am a Muslim woman and I have this modesty issue. . . the nurse should be culturally sensitive.” Although participants felt that cultural competency was the responsibility of both providers and patients, there was a general expectation that providers should undergo cultural-sensitivity training to learn the basics, and patients can then teach particulars. By assigning responsibility for cultural competency to the healthcare system, participants felt relieved of the burden to educate their providers about Islam during every healthcare encounter.
Cultural competency efforts and patient-centered care are especially important because Muslim patients may feel unwelcome in the healthcare system. Illustratively, one participant stated, “doctors and nurses . . . everybody . . . looks at you like (a) stranger or like you will be a problem for them.” Another noted, “I think we all know of stories where due to someone having an accent or . . . appearing Muslim . . . that sometimes the doctors may be more blunt with you, or . . . belittle you, or not . . . give you the time of day.”
Participants stated that Muslim patients run the risk of being treated negatively by providers when requesting accommodations for their religious and cultural beliefs. One participant shared her experience with a male doctor who became upset after she expressed her preference for a female gynecologist. Another participant said her doctor became angry when she requested that he speak to her from behind the curtain as she was disrobed. At times, participants said, providers may not take requests for accommodations seriously, “think(ing) it’s a big joke . . . or a bunch of old-fashioned foolishness they don’t want to be bothered with.” Participants also noted an undercurrent of discrimination, noting that other groups receive religious considerations that they do not: “Why don’t (they) go the extra mile with . . . Muslims? . . . (Our) needs are very tiny . . . What’s the big deal?”
Participants noted that providers who acknowledge and respect their religious beliefs are more likely to be trusted and their recommendations adhered to. Summing up this theme, a participant shared:
When the nurse . . . tells you . . . I respect your religion . . . immediately, I will have trusted her. . . That’s half of the work of being a healthcare giver . . . to get the trust of the patient. When the patient trusts you…he will be compliant with care.
Priorities for Healthcare Accommodation
Within the 13 focus groups, multiple items were noted as a top-three healthcare accommodation. The most common healthcare accommodations were: (1) Gender-concordant care, (2) Halal food and (3) Neutral space for prayer. (Table 1) Gender-concordance was discussed in the context of both inpatient and outpatient settings, while halal food and a neutral prayer space were requested in the hospital. (additional quotes in Table 3)
-
Gender-concordant care
Gender-concordant care was amongst the top-three accommodations requested in nearly every focus group (N = 11). Our participants affirmed the importance of modesty in cross-gender interactions and attributed this value to Islamic teachings around gender relations, dress code, and family values. While variably understood and practiced, our respondents mentioned how this value influences healthcare choices for men and women and presents them with challenges during clinical encounters.
In regards to choice of physician, a female participant expressed, “I look for females for (me and) my daughters, so the gender issue is really high on my list. It is not necessary that my doctor(s) … be…Muslim, but they do have to be female.” Participants also noted how a lack of gender-concordant care may negatively influence their healthcare seeking patterns. “I would not even walk into a clinic (in which) I didn’t have a choice of the gender,” said another participant.
Recognizing that gender-concordant care is not always possible, participants discussed other accommodations that would allow patients to maintain their modesty, such as private rooms or curtained enclosures, as well as more modest patient gowns. Both men and women identified this need. “I want to have clothing, gowns that cover us…—so you worry about those things” said one man, while another participant added, “change the hospital gown (and) make it more suitable (for)…our religious dress code.”
To display respect for patient modesty, participants suggested healthcare providers should “say excuse me to open the curtain” and ask for permission prior to entering patient rooms. One man said, “sometimes…we insist for them to put something (on) the door so …they cannot see.. (my wife)… from outside…They have to knock the door before they (come in)… (in case)….she’s not ready (dressed properly).”
-
Halal food
Halal food is food that adheres to Islamic dietary regulations that prohibit the consumption of pork and prescribe guidelines for ritual slaughter. Dietary guidelines also extend to non-food items such as medications. In most focus groups (N = 10), the provision of halal food was noted within the top-three accommodations requested.
Participants described halal food as “good for health” and better in quality. One nurse offered her perspective, “I've heard it from patients. I've heard it from families…when you don’t eat because of (not having) halal food, it's definitely going to affect (your health).” Thus, participants stressed that “nutrition is a major part (of) healing,” and that the lack of access to halal food in healthcare settings may impede healing and place undue burden on patient families to address their loved one’s nutritional needs. Participants recounted negative experiences when halal food was not available during their hospital stays, describing these hospitals as “the worst.”
-
Neutral space for prayer
Muslims are obligated to pray five times a day. Comprised of physical movements, litanies, and recitation from the Quran, ritual prayer also requires a clean and quiet space. Participants across focus groups (N = 11) considered a religiously neutral prayer space to be an important aspect of cultural accommodation.
Prayer is a central part of the healing process for many Muslim patients. A respondent noted that “a prayer room is a form of healing on its own.” Participants noted that patients who prayed in their own rooms sometimes faced interruptions from healthcare staff. One woman recounted, “I said, ok, before…they have to hook up the wires on (me)…I must do my last prayer. They gave me (only) three seconds…and start(ed) interfering.” Additionally, participants noted that sometimes when Muslim patients and their visitors prayed, hospital staff became suspicious. As one man shared, “so we were praying but… nurses and …. security [came] and asked if everything was ok…Doctors were (thereafter)… hesitant to come back in the room and…everybody came by after that and kind of looked in the door [gawking].” Further reflecting on an unwelcoming hospital environment, the participant continued “It's just like, you know, if they see a nun walking through the hospital, they say … hi sister, but they see a Muslim woman in a hijab…they might be thinking they need to keep security on hand.”
Participants also discussed how health systems might adapt existing prayer spaces to accommodate the needs of Muslim consumers by removing iconography to make the space a neutral one. As one participant explained, “at (a local Hospital) they have a meditation room. Other hospital(s)…take a section of the church, which you feel…(is) not good.” Other suggestions included making prayer rugs available for patients to use in their rooms and marking the direction towards Mecca so Muslims can face that direction while praying.
Table 3.
Illustrative Quotes relating to Healthcare Accommodations
| Healthcare Accommodation Requested | Theme | Quotes |
|---|---|---|
| Gender-concordant care | Influences healthcare-seeking patterns | Then they are hesitant or they have to think twice about their medical care because there is no privacy for them (when gender-concordant care is not possible) |
| When I had my children…I had a terrible experience…where I was just constantly yelling at people to get out (opposite gender) but the second one was much better because the nurses actually respected me and they put a sign on the door (stating) please knock (before you enter) | ||
| If somebody gets put in that position where there isn’t privacy to make them comfortable, when they get sick they are hesitant to be put in the same spot where they were violated. They have to try to…heal themselves or… they try to postpone (going to the doctor) | ||
| Is part of a concern for maintaining privacy | (There is) unnecessary walking in and out of patient rooms by staff. Especially those who have no business you know | |
| …you keep your privacy at a maximum. And sometimes I like (a) sign (that says), please knock before you enter, please no male doctor, no male nurses | ||
| Is related to modesty | If we have the gowns and we’re not wearing hijab (Muslim headscarf) and laying down on the bed and… the male nurses come in to check you, where is the gown…they put the IV or check your stomach or something so the gown goes up | |
| I said, don’t open the curtain, speak to me from behind the curtain and I could feel his (the doctor’s) tone so angry… I said, you can talk to me, I can talk to you, you don’t need to see me. I don’t want any male in here. I'm all exposed | ||
| Halal food | Is better for health | It has to be slaughtered halal…that’s got to be the best food source |
| A lack of access to halal food causes frustration | I asked them to bring me something to eat. They brought me some gelatin …. I was just asking (for something else), and they were rude | |
| Every time I ask for halal food, oh, we have vegetarian…It would be nice to have a halal steak or chicken….I mean everybody else gets meat. Except us. We always get vegetarian | ||
| Neutral space for prayer | A lack of space causes discomfort | Sometimes, they make you sit in the room for a long time waiting, right? So I pray, but I was hoping that they would understand, so even if they walked in they should know why—what I'm doing |
| One thing I say is that [we go] to the chapel or we don’t feel comfortable praying in there | ||
| At (local hospital) they have a prayer room, a chapel room. It was originally for Christians, then they made it accessible for everybody else. But it wasn’t established (with)…a qibla (an marking/ornament pointing towards Mecca to indicate direction of prayer for Muslims) |
DISCUSSION
American Muslims are a fast-growing, under-studied, and underserved minority. While ethnically and racially diverse, their shared faith brings forth common concerns and challenges within the healthcare setting. Our focus group participants from African American, Arab American and South Asian American Muslims in Metro Detroit provide a consistent message: Providers need to be aware of Islamic values and should work toward cultural competence by accommodating these values when possible. When asked to offer specific recommendations of how healthcare systems can improve the Muslim healthcare experience, participants prioritized three items: (1) allowing for gender-concordant care providers as much as possible; (2) providing halal food in the hospital; and (3) allocating a neutral space for prayer. The preference for gender-concordant care stems from Islamic conceptions of modesty and was noted to influence healthcare seeking patterns. Halal food was believed to be health-promoting and integral to convalescence. The need for a neutral prayer space was advanced given the discomfort patients felt and challenges they faced while praying in the hospital. Thus, our participants addressed specific ways in which healthcare systems can improve the quality of American Muslim healthcare experiences, and to our knowledge is the first account where a multi-ethnic and multi-racial group of American Muslims were asked to identify and prioritize healthcare accommodations.
Our respondents mentioned how cultural accommodations may influence healthcare-seeking behaviors, particularly in discussions of gender-concordant care, as some participants choose providers—and delay healthcare-seeking—based on availability of same-sex providers. Discussions of gender relations were most prominent in our female focus groups; however, both men and women noted these challenges, confirming findings from Afghan, Somali, South Asian and other Muslim groups.18–22 Our findings reinforce prior research demonstrating that lack of provision for some type of gender-concordant care leads to delayed healthcare-seeking within this community.19,22–24 While in the outpatient and non-urgent setting, it may be possible to choose a physician based on a gender preference, in the hospital setting, or for urgent and specialized medical conditions, greater challenges exist. It is unclear how healthcare systems and individual providers respond to patient requests for gender concordant care. A few hospitals have responded to modesty concerns by implementing knock, wait, and enter policies, and by providing more modest patient gowns.25,26However, some Muslim women note that providers may misinterpret their concern for modesty as shame for their bodies.21 Thus, the extent to which gender preferences and modesty concerns influence Muslim patient behaviors, as well as how healthcare providers can best respond to these needs, merit further investigation.
Hospitals have a long-standing history of accommodating patient preferences for food and allocating space to meet the spiritual needs of patients. The absence of such accommodations for Muslim patients within hospitals is multi-factorial, and our work suggests several possible reasons. One reason may be that Muslim patients are reticent to voice or advocate for their needs. Our focus group participants felt burdened at times in having to constantly educate healthcare providers about their values, and noted that cultural competency was a shared responsibility between the patient and the provider. The reservation against advocating for religious accommodations may further be compounded by uneasiness in drawing attention to their faith and mistrust of providers in the post-9/11 social climate.27 The healthcare administration may consider existing food services such as Kosher or vegetarian, and hospital chapels, to be sufficient for Muslim patient needs. Yet research notes that tailored food services and spiritual care delivery are gaps within hospital-based cultural accommodations common to many different groups.21,28 Thus, a need exists for dialogue between hospital administrators and community leaders. Such initiatives will allow for a better assessment of community needs and preferences, identify gaps in current healthcare delivery, and enhance trust and communication. Future studies should aim to assess the influence of such initiatives and established hospital-based cultural accommodations upon healthcare-seeking patterns.
Our findings are strengthened by our use of a community-based approach to recruitment, sampling from multiple segments of the American Muslim community, using languages preferred by participants in focus groups, and a qualitative research design. However, there are some clear limitations. Our data represent the voices of those members of the Greater Detroit Muslim community that attend mosques. This community is notable in that it is large and well-established with significant social capital. Yet a mosque-based recruitment strategy introduces selection bias toward members of the American Muslim community who have a stronger or more formal religious framework. As such, our work may not be generalizable across the breadth of American Muslim community and in particular to less religious segments of the population. However, precisely due to the long-history and large number of the Greater Detroit Muslim community, this work represents a first approximation to better understand American Muslim values and needs.
Lastly, our work suggests the need for further empirical and normative research. Developing and validating Islam-based measures of religiosity is integral to exploring associations between religion and health behaviors, and these efforts are still in preliminary stages.29 To gauge the generalizability of our findings, next steps should include gaining views from multiple Muslim communities and from Muslims with varying levels of religious adherence.
Enhancing cultural competency and providing patient-centered care are means by which healthcare inequities may be ameliorated. These efforts aim to inculcate attitudes at the provider-level that facilitate cross-cultural communication and respond to patient needs by tailoring healthcare. The same ethos applies at the healthcare system level where community needs are better understood and met by culturally sensitive healthcare accommodations and structural modifications in healthcare delivery. While we report on American Muslim values and preferences for healthcare accommodation, our work may have greater implications for minority health in general. The study of one underserved community may yield generalizable knowledge applicable to a larger group of minority populations, and a targeted intervention for one group may lead to benefits for people outside of this group. For example, understanding the need for culturally appropriate food provision within the hospital for Muslim patients may shine light on this unmet need of other communities. Similarly, developing more modest patient gowns sensitive to Muslim patient concerns may benefit others who feel patient gowns are too revealing.
In conclusion, our study informs efforts to deliver high-quality healthcare to American Muslims in several ways. Understanding the values underlying these requests for healthcare improvement and the challenges stemming from lack of accommodations will inform efforts at improving cultural competence and providing culturally sensitive healthcare.
Acknowledgements
We thank our respondents for sharing their insights with us, and our community partners for their invaluable recruitment assistance and support: Muzammil Ahmed MD, Hamada Hamid DO MPH from the Institute for Social Policy & Understanding, Adnan Hammad PhD from the Arab Community Center for Economic & Social Services, Mouhib Ayyas MD from the Islamic Shura Council of Michigan, and Ghalib Begg from the Council of Islamic Organizations of Michigan. We also thank Sonia Duffy RN and Michael D. Fetters MD MPH MA for assistance with study design, qualitative methods, and intellectual support. Lastly, a note of thanks to our troupe of research assistants, Heather Tidrick, Afrah Raza, Shoaib Rasheed, Ali Beydoun, Nadia Samaha, David Krass, Imen Alem, and Samia Arshad for their invaluable assistance.This project and the time-effort of AIP, AK, and KG was supported by the Robert Wood Johnson Foundation Clinical Scholars Program and additional project funding was provided by the Institute for Social Policy & Understanding.
Conflicts of Interest
None disclosed.
References
- 1.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Anonymous Poor communications, cultural barriers impacting quality of health care for minorities. Qual Lett Healthc Lead. 2002;14(4):11–13. [PubMed] [Google Scholar]
- 3.Cross TL, Bazron BJ, Dennis KW, Isaacs MR. Toward a culturally competent system of care. Georgetown University Child Development Center. 1989.
- 4.United States Department of Health and Human Services, Office of Minority Health. What Is Cultural Competency? Available at: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlid=11. Accessed December 6, 2011.
- 5.Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Culturally competent healthcare systems: a systematic review. Am J Prev Med. 2003;24(3 Suppl 1):68–79. doi: 10.1016/S0749-3797(02)00657-8. [DOI] [PubMed] [Google Scholar]
- 6.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(Suppl 1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller T. Mapping the Global Muslim Population: A Report on the Size and Distribution of the World’s Muslim Population. Pew Research Center; 2010.
- 8.Ba-Yunus I. Muslims of Illinois, a demographic report. Chicago: East-West University; 1997. [Google Scholar]
- 9.Obama B. Remarks by the President on a New Beginning. Available at: http://www.whitehouse.gov/the-press-office/remarks-president-cairo-university-6-04-09. Accessed December 6, 2011.
- 10.Allied Media Corp. Muslims American Demographic Facts. Available at: http://www.allied-media.com/AM/. Accessed December 6, 2011.
- 11.Hassoun RJ. Arab Americans in Michigan. Lansing: Michigan State University Press; 2005. [Google Scholar]
- 12.Numan FH. The Muslim Population in the United States. American Muslim Council; 1992; Available at: http://www.uga.edu/islam/muslimpop_usa.html. Accessed December 6, 2011.
- 13.Arab American Institute Foundation. Michigan; 20011. Available at: http://www.aaiusa.org/index_ee.php/pages/state-profiles. Accessed December 6, 2011.
- 14.Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88(2):251–258. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 15.Wehbe-Alamah H. Bridging generic and professional care practices for Muslim patients through use of Leininger's culture care modes. Contemp Nurse. 2008;28(1–2):83–97. doi: 10.5172/conu.673.28.1-2.83. [DOI] [PubMed] [Google Scholar]
- 16.Smedley BD, Smith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Care. Washington, DC: The National Academies Press; 2002. [PMC free article] [PubMed] [Google Scholar]
- 17.Israel BA. Methods in Community-Based Participatory Research for Health. 1. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- 18.Beine K, Fullerton J, Palinkas L, Anders B. Conceptions of prenatal care among Somali women in San Diego. J Nurse Midwifery. 1995;40(4):376–381. doi: 10.1016/0091-2182(95)00024-E. [DOI] [PubMed] [Google Scholar]
- 19.Simpson J, Carter K. Muslim women's experiences with health care providers in a rural area of the United States. J Transcult Nurs. 2008;19(1):16–23. doi: 10.1177/1043659607309146. [DOI] [PubMed] [Google Scholar]
- 20.Morioka-Douglas N, Sacks T, Yeo G. Issues in caring for Afghan American elders: insights from literature and a focus group. J Cross Cult Gerontol. 2004;19(1):27–40. doi: 10.1023/B:JCCG.0000015015.63501.db. [DOI] [PubMed] [Google Scholar]
- 21.Reitmanova S, Gustafson D. "They can't understand it": maternity health and care needs of immigrant Muslim women in St. John's, Newfoundland. Matern Child Health J. 2008;12(1):101–111. doi: 10.1007/s10995-007-0213-4. [DOI] [PubMed] [Google Scholar]
- 22.Matin M, LeBaron S. Attitudes toward cervical cancer screening among Muslim women: a pilot study. Women Health. 2004;39(3):63–77. doi: 10.1300/J013v39n03_05. [DOI] [PubMed] [Google Scholar]
- 23.Luna L. Care and cultural context of Lebanese Muslim immigrants: using Leininger's theory. J Transcult Nurs. 1994;5(2):12–20. doi: 10.1177/104365969400500203. [DOI] [PubMed] [Google Scholar]
- 24.DeShaw P. Use of the emergency department by Somali immigrants and refugees. Minn Med. 2006;89(8):42–45. [PubMed] [Google Scholar]
- 25.Zezima K. The Muslim patient will see you now, Doctor. New York Times. 2004 Sept 1;Sect. Health. Available at: http://www.nytimes.com/2004/09/01/national/01muslim.html. Accessed December 6, 2011.
- 26.Modesty gowns for female patients. British Broadcasting Company. 2006 September 5;Sect. News. Available at: http://news.bbc.co.uk/2/hi/uk_news/england/lancashire/5315306.stm. Accessed December 6, 2011.
- 27.Cainkar L. The Impact of 9/11 on Muslims and Arabs in the United States. In: Tirman J, editor. The maze of fear: security and migration after September 11. New York: The New Press; 2004. [Google Scholar]
- 28.Davidson J, Boyer ML, Casey D, Matzel SC, Walden D. Gap analysis of cultural and religious needs of hospitalized patients. Crit Care Nurs Q. 2008;31(2):119–126. doi: 10.1097/01.CNQ.0000314472.33883.d4. [DOI] [PubMed] [Google Scholar]
- 29.Amer MM, Hood RW. Special issue: part II. Islamic religiosity: measures and mental health. J Muslim Ment Health. 2008;3(1):1–5. doi: 10.1080/15564900802156544. [DOI] [Google Scholar]