ABSTRACT
BACKGROUND
In patients with diabetes, delays in controlling blood pressure are common, but the harms of delays have not been quantified.
OBJECTIVE
To estimate the harms of delays in controlling systolic blood pressure in middle-aged adults with newly diagnosed Type 2 diabetes.
DESIGN
Decision analysis using diabetes complication equations from the United Kingdom Prospective Diabetes Study (UKPDS).
PARTICIPANTS
Hypothetical population of adults aged 50 to 59 years old with newly diagnosed Type 2 diabetes based on characteristics from the National Health and Nutrition Examination Surveys.
INTERVENTION
Delays in lowering systolic blood pressure from 150 (uncontrolled) to 130 mmHg (controlled).
MAIN MEASURES
Lifetime complication rates (amputation, congestive heart failure, end-stage renal disease, ischemic heart disease, myocardial infarction, and stroke), average life expectancy and quality-adjusted life expectancy (QALE).
KEY RESULTS
Compared to a lifetime of controlled blood pressure, a lifetime of uncontrolled blood pressure increased complications by 1855 events per 10,000 patients and decreased QALE by 332 days. A 1-year delay increased complications by 14 events per 10,000 patients and decreased QALE by 2 days. A 10-year delay increased complications by 428 events per 10,000 patients and decreased QALE by 145 days. Among complications, rates of stroke and myocardial infarction increased to the greatest extent due to delays. With a 20-year delay in achieving controlled blood pressure, a baseline blood pressure of 160 mmHg decreased QALE by 477 days, whereas a baseline of 140 mmHg decreased QALE by 142 days.
CONCLUSIONS
Among middle-aged adults with diabetes, the harms of a 1-year delay in controlling blood pressure may be small; however, delays of ten years or more are expected to lower QALE to the same extent as smoking in patients with cardiovascular disease.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1951-y) contains supplementary material, which is available to authorized users.
KEY WORDS: diabetes mellitus, delays, hypertension, decision analysis
Blood pressure control is integral to diabetes treatment for adults with diabetes.1–4 In the United Kingdom Prospective Diabetes Study (UKPDS), tight blood pressure control (average blood pressure 144/82 mmHg) reduced the risk of mortality by 32% in patients with newly diagnosed Type 2 diabetes compared to usual care (average blood pressure 154/87 mmHg).5 Long-term follow-up of UKPDS revealed that the majority of benefits from tight blood pressure control are sustained only if control is maintained.6
While the health benefits of tight blood pressure control are well-accepted, blood pressure control is not consistently attained in clinical practice.7–10 Failure to attain tight blood pressure can be tied to critical junctures in the health care experience. Poor access to health care has been implicated as a barrier to achieving recommended blood pressure goals.11 Among patients who have access to health care, many experience clinical inertia in blood pressure management,7,12–16 which can be due in part to a patient’s unwillingness to take additional blood pressure medications.17 After medications are prescribed, at least one in five patients with diabetes is nonadherent to their prescribed medications.18–21
Multiple ongoing public health efforts are designed to overcome the barriers at these critical junctures in order to reduce delays in attaining blood pressure control. To improve access to health care, American health policy efforts have expanded insurance coverage for uninsured middle-aged adults.22 To address clinical inertia, researchers have made calls to reduce delays in blood pressure intensification.7,12,15,16,23,24 These calls are supported by specific recommendations in diabetes care guidelines. The American Diabetes Association recommends a medication-free lifestyle therapy trial of 3 months for patients whose blood pressure is <10 mmHg above goal and immediate initiation of medication for patients with blood pressure levels ≥10 mmHg above goal.25 While public health efforts to hasten the lowering of blood pressure have proliferated, the actual harms of delays in achieving tight blood pressure control have, surprisingly, never been quantified.
Quantifying the harms of delays in control of any intermediate clinical outcome is challenging with classical research methods. A randomized control trial of different delays in blood pressure control would be impractical due to the large number of possible delay periods and could be considered unethical due to the known benefits of blood pressure control. Observational studies would produce findings that are likely biased by treatment selection issues. Decision analysis does not have these limitations and provides an opportunity to quantify the risks of delays in controlling risk factors. Using decision analytic modeling, we estimate the harms of different delays in controlling blood pressure on health outcomes in middle-aged adults with newly diagnosed Type 2 diabetes.
METHODS
Overview
We constructed a Monte Carlo simulation model based on published equations from a diabetes complications model based on the UKPDS trial.26 The UKPDS equations simulate disease progression through seven individual diabetes complications and mortality. This model has been validated both internally and externally with data from cardiovascular trials.27 The diabetes complications include amputation, blindness, congestive heart failure, end-stage renal disease, ischemic heart disease, myocardial infarction, and stroke. UKPDS equations were used as published. The racial composition of the UKPDS population was significantly different from that of the current U.S. population. As a result, we did not account for any influence of race beyond differences in risk factor distributions.
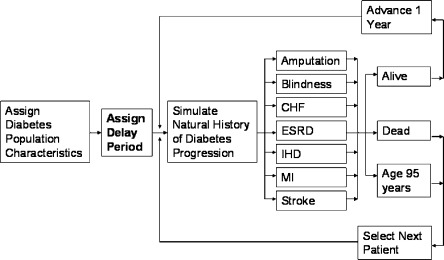
We specified hypothetical patients who can remain healthy or progressively develop diabetes complications until death or age 95, whichever comes first. Because of the structure of the UKPDS equations, each patient can experience multiple different complications during their lifetime, but each complication can only occur once per patient lifetime. To achieve stable estimates of model results, the model was run for a population of 10,000 hypothetical patients (iterations) for each delay period (Fig. 1). (Microsoft Excel 2000, Microsoft, Seattle, WA and @Risk 5.5, Palisades, Inc., Newfield, NY).
Figure 1.
Model framework. Abbreviations: CHF, congestive heart failure; ESRD, end-stage renal disease; IHD, ischemic heart disease; MI, myocardial infarction.
Population of Interest
The main population of interest was U.S. adults aged 50 to 59 years old with newly diagnosed Type 2 diabetes. The hypothetical population was assumed to have the demographic and clinical characteristics of pre-diabetes patients found in the National Health and Nutrition Examination Surveys (NHANES) (1999–2008). Patients were defined as having pre-diabetes based on reporting that they did not have a diagnosis of diabetes and any of three criteria: 1) hemoglobin A1c levels 5.7-6.4%, 2) fasting blood sugar levels 100–125 mg/dl (5.6-6.9 mmol/l), or 3) oral glucose tolerance test results 140–199 mg/dl (7.8-11.0 mmol/l).25
For each age and gender, population-level characteristics were used including current smoking rates, total and high-density lipoprotein cholesterol levels, body mass index, and history of congestive heart failure (Online Appendix Table 1). We assumed that the hemoglobin A1C at diagnosis was 6.5%.25 We also assumed that their duration of diabetes was 0 years. Since history of atrial fibrillation is not available in NHANES, we used rates from a large United States managed care population.28
Comparison Groups
To quantify the harms of delays, we compared a population with newly diagnosed diabetes who had a lifetime of controlled systolic blood pressure (130 mmHg) to populations who delay lowering systolic blood pressure from 150 to 130 mm Hg (delay populations). Based on diabetes care guidelines, we chose a conservative goal of 130 mmHg to represent controlled systolic blood pressure.25 An uncontrolled blood pressure of 150 mmHg was chosen to closely match the blood pressure of the control arm of the UKPDS.5 Separate delay populations were modeled to have delays ranging from 1 to 20 years (Fig. 1). A population was also modeled to experience a lifetime of uncontrolled systolic blood pressure (i.e. a lifetime systolic blood pressure of 150 mmHg) to estimate the maximum expected harm of delays. Apart from systolic blood pressure, the comparison groups were identical in terms of all population-level variables (baseline and current smoking rates, total and high-density lipoprotein levels, hemoglobin A1c, body mass index, and history of congestive heart failure and atrial fibrillation).
Outcomes of Interest
Outcomes of interest included lifetime complication rates (amputation, congestive heart failure, end-stage renal disease, ischemic heart disease, myocardial infarction, and stroke), average life expectancy, and average quality-adjusted life expectancy (QALE). The risk of blindness is not affected by blood pressure levels in the UKPDS equations, so we do not report blindness rates.26 We report the difference in lifetime overall and individual complication rates, average life expectancy, and average QALE between the population with a lifetime of controlled systolic blood pressure and each of the populations with delays in controlling systolic blood pressure. QALE was calculated based on utilities directly elicited from a racially/ethnically diverse sample of U.S. patients with Type 2 diabetes (Online Appendix Table 2).29 UKPDS utility values were used for myocardial infarction and congestive heart failure, since directly elicited values were not available.30 When multiple health states occurred during a cycle, the lowest utility value was used (minimum health state method). Delays in controlling systolic blood pressure were assumed to have no additional disutility.31
Sensitivity Analyses
In sensitivity analyses, we explored the effects of both higher (160 mmHg) and lower baseline systolic blood pressure (140 mmHg). We also quantified the harms of delays based on utility values previously used in the UKPDS diabetes complications model and other prominent diabetes models, since utility values may differ based on collection methods.29,32,33
To evaluate the effects of delays in blood pressure control in other diabetes populations, we repeated the analysis using the U.S. adult prevalent diabetes population. We defined prevalent diabetes by having any of the following criteria: 1) self-reported diagnosis, 2) hemoglobin A1C levels ≥6.5%, 3) fasting blood sugar levels ≥126 mg/dl (7.0 mmol/l), or 4) oral glucose tolerance test results ≥200 mg/dl (11.0 mmol/l). We used data from NHANES 1999–2008 to provide prevalent diabetes population-level characteristics for current smoking rates, smoking rates at diabetes diagnosis, total and high-density lipoprotein cholesterol levels, body mass index, history of congestive heart failure, duration of diabetes, and hemoglobin A1c. We used atrial fibrillation rates from a large United States managed care population, since these rates are not available in NHANES.28
RESULTS
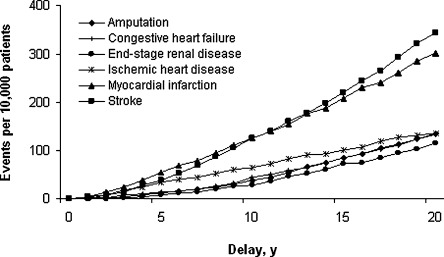
A lifetime of controlled systolic blood pressure led to 6296 complications per 10,000 patients, an average life expectancy of 22.10 years, and an average QALE of 20.39 years (Table 1). With a lifetime of uncontrolled systolic blood pressure (the maximum expected harm of delays), complications increased by 1855 events per 10,000 patients, average life expectancy decreased by 209 days, and average QALE decreased by 332 days. The average rates of stroke and myocardial infarction increased to the greatest extent compared to other complications (Fig. 2 and Online Appendix Table 3).
Table 1.
Harm of Delays in Controlling Systolic Blood Pressure on Overall Diabetes Complication Rates, Life Expectancy and Quality-Adjusted Life Expectancy*
| Delay, y | Overall diabetes complication rates† | Life expectancy | Quality-adjusted life expectancy | |||
|---|---|---|---|---|---|---|
| Events (95% CI) | Difference‡ | Years (95% CI) | Days lost | Years (95% CI) | Days lost | |
| 0 | 6296 (6138–6454) | -- | 22.10 (21.94–22.26) | -- | 20.39 (20.24–20.54) | -- |
| 1 | 6310 (6152–6468) | 14 | 22.10 (21.94–22.26) | 0 | 20.39 (20.23–20.54) | 2 |
| 5 | 6460 (6301–6619) | 164 | 22.01 (21.85–22.18) | 30 | 20.24 (20.08–20.39) | 55 |
| 10 | 6724 (6562–6886) | 428 | 21.86 (21.69–22.02) | 89 | 19.99 (19.84–20.15) | 145 |
| 15 | 7071 (6906–7236) | 775 | 21.70 (21.53–21.86) | 146 | 19.76 (19.61–19.92) | 229 |
| 20 | 7464 (7294–7634) | 1168 | 21.59 (21.43–21.76) | 184 | 19.60 (19.45–19.76) | 287 |
| Lifetime | 8151 (7971–8331) | 1855 | 21.53 (21.36–21.69) | 209 | 19.48 (19.33–19.63) | 332 |
*Delays were modeled for a hypothetical population of adults aged 50–59 year old with newly diagnosed Type 2 diabetes. During delays, hypothetical patients were assumed to have uncontrolled systolic blood pressure (150 mmHg)
†Complications included amputation, congestive heart failure, end-stage renal disease, ischemic heart disease, myocardial infarction, and stroke. Rates reported as events per 10,000 patients (95% Cl)
‡Difference in events between population with controlled blood pressure and populations with delays in controlling blood pressure
Figure 2.
Harm of delays in controlling systolic blood pressure on individual diabetes complication rates.
A 1-year delay in controlling systolic blood pressure increased lifetime complications by 14 events per 10,000 patients with a range between 0 (end-stage renal disease) and five events (myocardial infarction) per 10,000 patients for specific complications. A 1-year delay did not affect average life expectancy but decreased QALE by 2 days. A 5-year delay increased lifetime complications by 164 events with individual complications increasing between 9 and 55 events per 10,000 patients. Average life expectancy decreased by 30 days (14% of maximum expected harm) and QALE decreased by 55 days (16% of maximum expected harm). A 10-year delay increased lifetime complications by 428 events per 10,000 patients and increased individual complications between 29 and 125 events per 10,000 patients. The average life expectancy decreased by 89 days (43% of the maximum expected harm) and QALE decreased by 145 days (44% of the maximum expected harm). A 20-year delay increased lifetime complications by 1168 events per 10,000 patients and individual complications increased between 115 and 343 events. Average life expectancy decreased by 184 days (88% of the maximum expected harm) and QALE decreased by 287 days (86% of the maximum expected harm).
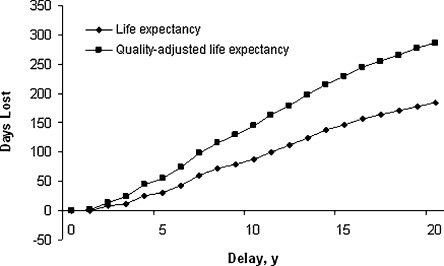
For delays between 2 and 20 years, lifetime complication rates increased (Fig. 2) and average life expectancy and average QALE decreased steadily with each additional year of delay (Fig. 3). For each additional year of delay, lifetime diabetes complications increased by an average of 61 events per 10,000 patients (Range, 23–86). Additionally, life expectancy decreased by an average of 10 days per year (Range, 3–17) and QALE decreased by an average of 15 days per year (Range, 9–24).
Figure 3.
Harm of delays in controlling systolic blood pressure on life expectancy and quality-adjusted life expectancy.
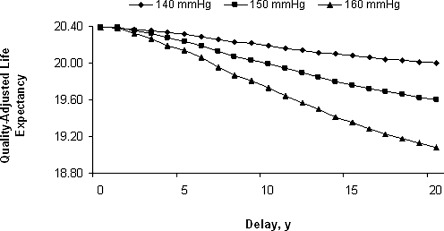
Sensitivity Analyses
The level of baseline systolic blood pressure affected the degree to which delays in controlling blood pressure affected health outcomes (Fig. 4). A lifetime systolic blood pressure level of 160 mmHg decreased average QALE by 544 days, compared to a lifetime systolic blood pressure level of 140 mmHg which decreased QALE by 163 days. With a 1-year delay in achieving control, a baseline systolic blood pressure level of 160 mmHg decreased average QALE by 5 days, whereas a baseline systolic blood pressure level of 140 mmHg decreased QALE by 2 days. With a 20-year delay, a baseline blood pressure of 160 mmHg decreased QALE by 477 days and a baseline blood pressure of 140 mmHg decreased QALE by 142 days. For delays between 2 and 20 years, each additional year of delay decreased average QALE by an average of 25 days per year (baseline systolic blood pressure 160 mmHg) and 7 days per year (baseline systolic blood pressure 140 mmHg).
Figure 4.
Harm of delays in controlling systolic blood pressure on quality-adjusted life expectancy with different starting systolic blood pressure levels.
Incorporating utility values used in other diabetes models modified the degree of harm caused by delays but did not alter the overall patterns of results. A lifetime of uncontrolled systolic blood pressure decreased average QALE by 254 days (vs. 332 days). A 1-year delay in controlling systolic blood pressure decreased average QALE by 1 day (vs. 2 days). For delays between 2 and 20 years, average QALE decreased by an average of 12 days (vs. 15 days) per year of delay.
For the prevalent diabetes population, delays in controlling systolic blood affected complications, life expectancy, and QALE to a lesser degree than the newly diagnosed population (Online Appendix Tables 4 and 5). Immediately controlled systolic blood pressure led to 4384 overall complications (vs. 6296 overall complications), an average life expectancy of 16.70 years (vs. 22.10 years), and an average QALE of 15.93 years (vs. 20.39 years). A lifetime of uncontrolled blood pressure led to an additional 1354 overall complications (vs. 1855 overall complications), an average life expectancy of 16.21 years (vs. 21.53 years), and an average QALE of 15.23 years (vs. 19.48 years). A 1 year delay in blood pressure control increased complications by 37 events and decreased average life expectancy by 5 days and average QALE by 11 days. Each delay between 2 and 20 years increased complications by 59 events and decreased average life expectancy by 9 days and average QALE by 12 days.
DISCUSSION
To our knowledge, this study provides some of the first insights into the expected magnitude of harm of different delays in controlling blood pressure in patients with diabetes. A 1-year delay in controlling systolic blood pressure is expected to lead to small declines in health outcomes. However, multiple years of delay, especially above 10 years, are expected to lead to significant declines in health outcomes. Among diabetes-related complications, rates of stroke and myocardial infarction are projected to increase to the greatest degree with delays in controlling blood pressure. Additionally, the harms of delays are greater when the baseline systolic blood pressure is higher.
The clinical significance of delays in controlling systolic blood pressure can be better understood by comparing their effects with those of other interventions. Delays in achieving blood pressure control of 10 years or less are expected to produce harms that are generally smaller than the harms of not addressing other risk factors of cardiovascular disease.34 For example, a patient with diabetes and a baseline blood pressure level of 150 mmHg, who delays blood pressure control for 10 years, is expected to lose 145 quality-adjusted days of life; whereas, the same patient is expected to lose 398 quality-adjusted days if they do not achieve a LDL cholesterol <100 mg/dL. On the other hand, delays in achieving blood pressure control that are above 10 years are expected to produce harms that are comparable to those of unmanaged cardiovascular risk factors. A 15 year delay in controlling systolic blood pressure is expected to lower QALE to the same degree as a lifetime of smoking in patients with cardiovascular disease (a loss of 237 quality-adjusted days).34
Given the current size of the diabetes population, our results suggest that achieving and maintaining tight blood pressure control earlier among U.S. middle-aged adults with diabetes has the potential to generate substantial population-level health benefits. Eliminating a 5-year delay in systolic blood pressure control for the U.S. population of middle-aged adults with newly diagnosed diabetes is expected to save 86,000 years of life. Achieving and maintaining tight blood pressure control requires that U.S. middle-aged adults with diabetes have early and stable access to health care throughout their disease course. Access to health care services for the middle-aged population may be easier to achieve through expanded health insurance coverage expected to occur in 2014 due to the Affordable Care Act.22
While many years of delays in controlling blood pressure are quite harmful, there may only be small harm from a single year of delay. This contrast between long-term and short-term delays has important implications for the timing of initiation of drug therapy for blood pressure control. Current diabetes care guidelines recommend that patients with new onset hypertension undergo at most a 3-month period of medication-free lifestyle therapy.25 This short period of lifestyle therapy is undoubtedly motivated by a desire to minimize patients’ exposure to hypertension. However, our study results suggest that health care providers may have more time, at least up to 1-year, to focus on diabetes self-management and lifestyle modification. This prolonged focus on lifestyle modification, at the time of diagnosis, could have lifelong benefits for patients with diabetes, since self-management increases diabetes knowledge and improves outcomes.25,35–39 From the patient perspective, extending the period of lifestyle therapy without introducing medications may be in line with their preferences, since many patients prefer to control blood pressure through diet and exercise rather than with antihypertensive medications.29 At the same time, these preferences cannot be the indefinite arbiter of treatment decisions as extensive delays in initiating medical therapy for uncontrolled hypertension have negative consequences.
There are several limitations to our findings. Since this study is based on a decision analytic model, our results are contingent on the model assumptions. We specified delay periods to start after diabetes diagnosis and to run continuously, which may limit generalizability to other patterns of delays. We also focused on one comparison of systolic blood pressure levels in order to provide a model clinical scenario for delays in control. As our sensitivity analysis suggests, there are a countless number of blood pressure comparisons and the exact impact of delays in control will vary with each of them. In addition, our analysis focuses on the health effects of traditional diabetes-related complications and does not account for the potential adverse effects of intensive blood pressure control therapies. Intensive blood pressure control therapies may increase adverse drug events due to polypharmacy,40 and intensive therapies may not be preferred by individual patients over conventional therapy.29 Interestingly, clinical trials such as UKPDS have not clearly found a quality of life effect of intensive blood pressure control therapies when using standard quality of life instruments.31
Our results suggest that the harms of delays in controlling systolic blood pressure depend on the duration of the delays in middle-aged adults with newly diagnosed and prevalent Type 2 diabetes. A 1-year delay in controlling systolic blood pressure may lead to only small declines in life expectancy and quality-adjusted life expectancy. However, delays over 10 years may lead to large declines in health. Discussions with patients about initiating intensive blood pressure control could be enhanced by including information on how postponing blood pressure control can affect their lifelong outcomes. This must be balanced with honest conversation regarding the challenges of adopting lifestyle therapy and complex medical therapies. Though our study focused on delays in systolic blood pressure control in middle-aged adults with diabetes, our results may have implications for the management of other chronic diseases. Future studies are needed to confirm these findings in clinical practice and to evaluate whether delays in attaining other intermediate clinical outcomes have similar relationships with lifetime outcomes.
Electronic supplementary material
(DOC 151 kb)
Acknowledgments
Funders
The authors are supported by an NIDDK Ruth L. Kirschstein National Research Service Award (F32 DK089973 [Dr. Laiteerapong]), a NIDDK Diabetes Research and Training Center (P60 DK20595 [Dr. Laiteerapong, Ms. John, Dr. Meltzer, and Dr. Huang]), a NIDDK Chicago Center for Diabetes Translational Research (P30 DK092949 [Dr. Laiteerapong, Ms. John, Dr. Meltzer, and Dr. Huang]), a NIA Midcareer Investigator Award in Patient-Oriented Research (K24 AG031326 [Dr. Meltzer]), and an AHRQ Hospital Medicine and Economics Center for Education and Research in Therapeutics (U18 HS016967-01 [Dr. Meltzer]).
Prior Presentations
This work was presented in part at the Society of General Internal Medicine (SGIM) 34th Annual Meeting, Phoenix, AZ, May 2011.
Conflict of Interest
None disclosed.
REFERENCES
- 1.Anderson RJ, Bahn GD, Moritz TE, Kaufman D, Abraira C, Duckworth W. Blood pressure and cardiovascular disease risk in the Veterans Affairs Diabetes Trial. Diabetes Care. 2011;34:34–38. doi: 10.2337/dc10-1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vijan S, Hayward RA. Treatment of hypertension in type 2 diabetes mellitus: blood pressure goals, choice of agents, and setting priorities in diabetes care. Ann Intern Med. 2003;138:593–602. doi: 10.7326/0003-4819-138-7-200304010-00018. [DOI] [PubMed] [Google Scholar]
- 3.Boer IH, Rue TC, Cleary PA, et al. Long-term Renal Outcomes of Patients With Type 1 Diabetes Mellitus and Microalbuminuria: An Analysis of the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Cohort. Arch Intern Med. 2011;171:412–420. doi: 10.1001/archinternmed.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pogach L, Aron DC. Sudden acceleration of diabetes quality measures. JAMA. 2011;305:709–710. doi: 10.1001/jama.2011.153. [DOI] [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–713. doi: 10.1136/bmj.317.7160.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med. 2008;359:1565–1576. doi: 10.1056/NEJMoa0806359. [DOI] [PubMed] [Google Scholar]
- 7.Grant RW, Cagliero E, Dubey AK, et al. Clinical inertia in the management of Type 2 diabetes metabolic risk factors. Diabet Med. 2004;21:150–155. doi: 10.1111/j.1464-5491.2004.01095.x. [DOI] [PubMed] [Google Scholar]
- 8.Triad Study Group Health systems, patients factors, and quality of care for diabetes: a synthesis of findings from the TRIAD study. Diabetes Care. 2010;33:940–947. doi: 10.2337/dc09-1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141:272–281. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 10.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–574. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 11.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med. 2009;150:505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 12.Gil-Guillen V, Orozco-Beltran D, Perez RP, et al. Clinical inertia in diagnosis and treatment of hypertension in primary care: quantification and associated factors. Blood Press. 2010;19:3–10. doi: 10.3109/08037050903350762. [DOI] [PubMed] [Google Scholar]
- 13.Kerr EA, Zikmund-Fisher BJ, Klamerus ML, Subramanian U, Hogan MM, Hofer TP. The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Ann Intern Med. 2008;148:717–727. doi: 10.7326/0003-4819-148-10-200805200-00004. [DOI] [PubMed] [Google Scholar]
- 14.Roumie CL, Elasy TA, Wallston KA, et al. Clinical inertia: a common barrier to changing provider prescribing behavior. Jt Comm J Qual Patient Saf. 2007;33:277–285. doi: 10.1016/s1553-7250(07)33032-8. [DOI] [PubMed] [Google Scholar]
- 15.O’Connor PJ. Overcome clinical inertia to control systolic blood pressure. Arch Intern Med. 2003;163:2677–2678. doi: 10.1001/archinte.163.22.2677. [DOI] [PubMed] [Google Scholar]
- 16.Viera AJ, Schmid D, Bostrom S, Yow A, Lawrence W, Dubard CA. Level of blood pressure above goal and clinical inertia in a Medicaid population. J Am Soc Hypertens. 2010;4:244–254. doi: 10.1016/j.jash.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zikmund-Fisher BJ, Hofer TP, Klamerus ML, Kerr EA. First things first: difficulty with current medications is associated with patient willingness to add new ones. Patient. 2009;2:221–231. doi: 10.2165/11313850-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27:2800–2805. doi: 10.2337/diacare.27.12.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katon W, Russo J, Lin EH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medication adherence or lack of treatment intensification? Psychosom Med. 2009;71:965–972. doi: 10.1097/PSY.0b013e3181bd8f55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 21.Bruggen R, Gorter K, Stolk RP, Zuithoff P, Klungel OH, Rutten GE. Refill adherence and polypharmacy among patients with type 2 diabetes in general practice. Pharmacoepidemiol Drug Saf. 2009;18:983–991. doi: 10.1002/pds.1810. [DOI] [PubMed] [Google Scholar]
- 22.Laiteerapong N, Huang ES. Health care reform and chronic diseases: anticipating the health consequences. JAMA. 2010;304:899–900. doi: 10.1001/jama.2010.1209. [DOI] [PubMed] [Google Scholar]
- 23.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135:825–834. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 24.Phillips LS, Twombly JG. It’s time to overcome clinical inertia. Ann Intern Med. 2008;148:783–785. doi: 10.7326/0003-4819-148-10-200805200-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Diabetes Association Standards of medical care in diabetes--2011. Diabetes Care. 2011;34(Suppl 1):S11–61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clarke PM, Gray AM, Briggs A, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68) Diabetologia. 2004;47:1747–1759. doi: 10.1007/s00125-004-1527-z. [DOI] [PubMed] [Google Scholar]
- 27.Mount Hood 4 Modeling Group Computer modeling of diabetes and its complications: a report on the Fourth Mount Hood Challenge Meeting. Diabetes Care. 2007;30:1638–1646. doi: 10.2337/dc07-9919. [DOI] [PubMed] [Google Scholar]
- 28.Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 29.Huang ES, Brown SE, Ewigman BG, Foley EC, Meltzer DO. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care. 2007;30:2478–2483. doi: 10.2337/dc07-0499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62) Med Decis Making. 2002;22:340–349. doi: 10.1177/0272989X0202200412. [DOI] [PubMed] [Google Scholar]
- 31.U.K. Prospective Diabetes Study Group Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37) Diabetes Care. 1999;22:1125–1136. doi: 10.2337/diacare.22.7.1125. [DOI] [PubMed] [Google Scholar]
- 32.CDC Diabetes Cost-effectiveness Group Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA. 2002;287:2542–2551. doi: 10.1001/jama.287.19.2542. [DOI] [PubMed] [Google Scholar]
- 33.The Diabetes Control and Complications Trial Research Group Lifetime benefits and costs of intensive therapy as practiced in the diabetes control and complications trial. JAMA. 1996;276:1409–1415. doi: 10.1001/jama.1996.03540170053032. [DOI] [PubMed] [Google Scholar]
- 34.Kahn R, Robertson RM, Smith R, Eddy D. The impact of prevention on reducing the burden of cardiovascular disease. Diabetes Care. 2008;31:1686–1696. doi: 10.2337/dc08-9022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 36.Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 2003;29:488–501. doi: 10.1177/014572170302900313. [DOI] [PubMed] [Google Scholar]
- 37.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 38.Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: a meta-analysis and meta-regression. Patient Educ Couns. 2004;52:97–105. doi: 10.1016/S0738-3991(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 39.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164:1641–1649. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 40.Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 151 kb)