Abstract
Type 1 diabetes is an autoimmune disease characterized by T cell responses to beta cell antigens, including insulin. Investigations employing the NOD mouse model of the disease have revealed an essential role for beta cell-specific CD8+ T cells in the pathogenic process. As CD8+ T cells specific for beta cell antigens are also present in patients, these reactivities have the potential to serve as therapeutic targets or markers for autoimmune activity. NOD mice transgenic for human class I MHC molecules have previously been employed to identify T cell epitopes having important relevance to the human disease. However, most studies have focused exclusively on HLA-A*0201. To broaden the reach of epitope-based monitoring and therapeutic strategies, we have looked beyond this allele and developed NOD mice expressing human β2-microglobulin and HLA-A*1101 or HLA-B*0702, which are representative members of the A3 and B7 HLA supertypes, respectively. We have used islet-infiltrating T cells spontaneously arising in these strains to identify beta cell peptides recognized in the context of the transgenic HLA molecules. This work has identified the insulin C-peptide as an abundant source of CD8+ T cell epitopes. Responses to these epitopes should be of considerable utility for immune monitoring, as they cannot reflect an immune reaction to exogenously administered insulin, which lacks the C-peptide. Because the peptides bound by one supertype member were found to bind certain other members also, the epitopes identified here have the potential to result in therapeutic and monitoring tools applicable to large numbers of patients and at-risk individuals.
INTRODUCTION
Type 1 diabetes is an organ-specific autoimmune disease in which T cell-mediated elimination of pancreatic islet beta cells results in insulin insufficiency. While the strongest genetic determinant for disease susceptibility is the expression of predisposing class II MHC molecules (1), a series of studies have also uncovered an association with particular class I MHC alleles, including the common HLA-A*0201 (2–11). This class I MHC association is not merely reflective of linkage disequilibrium with disease-promoting class II genes (4, 6, 9). Consistent with the idea that particular class I MHC molecules can foster diabetes development is the finding that CD8+ T cells specific for beta cell antigens are present in the peripheral blood of type 1 diabetes patients (12). CD8+ T cells are also seen infiltrating the islets of new-onset and graft-recurrent type 1 diabetes patients, suggesting their contribution to beta cell elimination (13–17). In the NOD mouse model of the disease, CD8+ T cells specific for beta cell antigens are required pathogenic effectors (18) that have begun to demonstrate potential as therapeutic targets (19–24).
Peptide-based CD8+ T cell assays are showing promise as tools for the detection of beta cell autoimmunity in recent-onset type 1 diabetes patients and islet transplant recipients, particularly when multiple T cell epitopes are simultaneously examined (25–27). While it is true that the specific epitopes targeted can differ from one individual to another, it is clear from both NOD mouse models (28–30) and type 1 diabetes patients (25–27) that peptides derived from the beta cell antigens insulin (Ins)7 and islet-specific glucose-6-phosphatase catalytic subunit-related protein (IGRP) are recognized by CD8+ T cells in most individuals. For example, in one study, 85% of recent-onset HLA-A*0201-positive patients showed T cell responses to the HLA-A*0201-binding peptide Ins L15-**24, and one quarter showed responses to IGRP 265–273 (27).
Though multiple beta cell peptides have been identified as the antigenic targets of CD8+ T cells in type 1 diabetes patients, nearly all of these are recognized in the context of HLA-A*0201 (12). While this is a common class I MHC molecule expressed in nearly 50% of certain ethnic groups (31), elucidation of the insulin and IGRP peptides recognized in the context of other human class I molecules would allow broader coverage of the patient population in terms of those that could benefit from the development of peptide-based predictive, diagnostic, and therapeutic strategies (32). In the past, we have used HLA-A*0201-transgenic NOD mouse models to identify epitopes of insulin and IGRP that are recognized by islet-infiltrating CD8+ T cells (28, 30, 33), and this strategy successfully identified epitopes (e.g., IGRP 228–236, IGRP 265–273, Ins B5-14, and Ins B10-18) that were also found to be recognized in HLA-A*0201-positive type 1 diabetes patients (25–27, 34–38). In our efforts to look beyond HLA-A*0201, here we have generated NOD mouse strains expressing human β2-microglobulin (β2m) and HLA-A*1101 or HLA-B*0702 and used these mice to identify beta cell peptides recognized in the context of these human class I MHC molecules. Our characterization of these new strains has revealed the insulin C-peptide to be a rich source of CD8+ T cell epitopes. Responses to these epitopes should be of particular utility for immune monitoring of type 1 diabetes patients and islet-transplant recipients, as they cannot reflect an immune reaction to exogenously administered insulin, which lacks the C-peptide. Furthermore, HLA-A*1101 and HLA-B*0702 are representative members of two different HLA supertypes, which are groupings of MHC molecules that have been defined on the basis of structural similarities in the peptide-binding groove (39–41). Members of a supertype show overlap in peptide-binding repertoires (40, 42), and the beta cell peptides we identified using one supertype member were found to also bind certain other members of that supertype, potentially resulting in monitoring and therapeutic reagents relevant to large numbers of patients and at-risk individuals.
MATERIALS AND METHODS
Derivation of NOD.mβ2mnull.hβ2m mice transgenic for HLA-A*1101 or HLA-B*0702
C57BL/6 mice expressing a chimeric HLA-A*1101 heavy chain (α1 and α2 domains of HLA-A*1101, and α3, transmembrane, and cytoplasmic domains from H-2Kb) or a fully human HLA-B*0702 heavy chain were obtained from C. David (Mayo Clinic) and have been described previously (43, 44). Both strains were backcrossed to NOD mice for at least ten generations and fixed to homozygosity for markers of NOD origin delineating known Idd loci. Murine β2m was removed and human β2m introduced by intercrossing with the NOD.mβ2mnull.hβ2m strain (45), yielding the two new strains designated NOD.mβ2mnull.hβ2m.HLA-A11 and NOD.mβ2mnull.hβ2m.HLA-B7.
Derivation of NOD.hCD8 mice
C57BL/6 mice expressing human CD8α and human CD8β under the control of the murine p56lck proximal promoter (line αβ57) were obtained from The Jackson Laboratory (46). They were backcrossed to NOD mice for at least ten generations and fixed to homozygosity for markers of NOD origin delineating known Idd loci, resulting in the NOD.hCD8 strain.
Flow cytometric analysis of splenocytes
Single-cell spleen suspensions were obtained by gentle grinding between frosted slides and passing through a 40-µm cell strainer. Splenocytes from NOD.mβ2mnull.hβ2m.HLA-A11, NOD.mβ2mnull.hβ2m.HLA-B7, and murine β2m-expressing NOD.HLA-A11 mice were analyzed by multicolor flow cytometry after staining with labeled antibodies to class I HLA heavy chains (B9.12.1; Beckman Coulter), human β2m (TÜ99), H-2Kd (SF1-1.1), and H-2Db (KH95). Splenocytes from NOD.hCD8 and NOD mice were analyzed after staining with labeled antibodies specific for murine CD4 (RM4-5), murine CD8α (53-6.7), and human CD8α (RPA-T8). All antibodies for flow cytometry were obtained from BD Biosciences except where indicated.
Assessment of diabetes development
Mice were monitored weekly for glucosuria with Diastix reagent strips for urinalysis (Bayer). Mice were considered diabetic when two positive measurements were obtained. The time of onset of disease was recorded as the date of the first of the two positive readings.
Cyclophosphamide treatment
Female mice (12 to 21 weeks of age) were treated with two injections of 200 mg/kg cyclophosphamide (Sigma) i.p. two weeks apart (47, 48). Diabetes development was monitored weekly after the first injection.
Peptides
Peptide libraries containing all of the 8mer, 9mer, 10mer, and 11mer peptides that can be derived from murine preproinsulin 1, preproinsulin 2, or IGRP were synthesized by Mimotopes using their proprietary Truncated PepSet technology. Each library mixture contained four peptides with a common C-terminus and having a length of 8, 9, 10, or 11 residues. The four peptides in each mixture were present in approximately equimolar amounts. Concentrated peptide stocks (2.75 mM) were prepared in 50% acetonitrile/H2O, and 40 µM (i.e., about 10 µM for each peptide in the mixture) working stocks were obtained by serial dilution in PBS (pH 6.5). Individual peptides, having a purity of ≥ 90%, were obtained from Mimotopes. Concentrated stocks (10 mM) were prepared in DMSO, and 10 µM working stocks were obtained by dilution in PBS.
Islet-infiltrating T cells
Pancreatic islets were isolated from female mice by collagenase perfusion of the common bile duct and islet-infiltrating T cells were cultured as described (49). Briefly, islets were handpicked and cultured for 7 days in 24-well cell culture plates (~50 islets/well) in RPMI 1640 medium supplemented with 10% FBS (Hyclone), 1 mM sodium pyruvate, non-essential amino acids, 28 µM β-mercaptoethanol, and 50 U/ml recombinant human IL-2 (PeproTech).
IFN-γ ELISPOT
IFN-γ ELISPOT was performed as described (49) using 2 × 104 islet-infiltrating T cells as responders and 2 × 104 syngeneic splenocytes pulsed with 1 µM peptide as antigen-presenting cells. Spots were developed after incubation at 37°C for 40 h and were counted using an automated ELISPOT reader system (Autoimmun Diagnostika). Where indicated, CD8+ T cells were first purified by negative selection from cultured islet infiltrates using magnetic separation (Miltenyi Biotec).
Tetramer staining of islet-infiltrating T cells
PE-labeled HLA-A*1101 tetramers were prepared following standard procedures (50) using a chimeric heavy chain (α1 and α2 domains of HLA-A*1101, and α3 domain of H-2Kb) and human β2m. Islet-infiltrating T cells were first stained with the tetramers and then with a labeled antibody to murine CD8α (53-6.7) and analyzed by flow cytometry.
MHC purification and peptide-binding assays
Purification of MHC molecules by affinity chromatography has been detailed elsewhere (51). Briefly, EBV-transformed homozygous cell lines or single MHC allele-transfected 721.221 or C1R lines were utilized as sources of HLA class I MHC molecules. HLA molecules were purified from cell pellet lysates by repeated passage over Protein A Sepharose beads conjugated with the W6/32 (anti-HLA A, B, C) antibody. In some cases, HLA-A molecules were separated from HLA-B and -C molecules by pre-passage over a B1.23.2 (anti-HLA B, C and some A) column. Protein purity, concentration, and the effectiveness of depletion steps were monitored by SDS-PAGE and bicinchoninic acid protein assay.
Assays to quantitatively measure peptide binding to class I MHC molecules were based on the inhibition of binding of a high affinity radiolabeled peptide to purified MHC molecules, and were performed essentially as detailed elsewhere (51, 52). Briefly, 0.1–1 nM of radiolabeled peptide was co-incubated at room temperature with 1 µM to 1 nM of purified MHC in the presence of a cocktail of protease inhibitors and 1 µM β2m. Following a two-day incubation, MHC bound radioactivity was determined by capturing MHC/peptide complexes on W6/32 (anti-class I) antibody coated Lumitrac 600 plates (Greiner Bio-One), and measuring bound cpm using the TopCount (Packard Instrument Co.) microscintillation counter. In the case of competitive assays, the concentration of peptide yielding 50% inhibition of the binding of the radiolabeled peptide was calculated. Under the conditions utilized, where [label] < [MHC] and IC50 ≥ [MHC], the measured IC50 values are reasonable approximations of the true Kd values (53, 54). Each competitor peptide was tested at six different concentrations covering a 100,000-fold dose range, and in three or more independent experiments. As a positive control, the unlabeled version of the radiolabeled probe was also tested in each experiment.
RESULTS
NOD.mβ2mnull.hβ2m mice transgenic for HLA-A11 or HLA-B7 are diabetes-susceptible to varying degrees
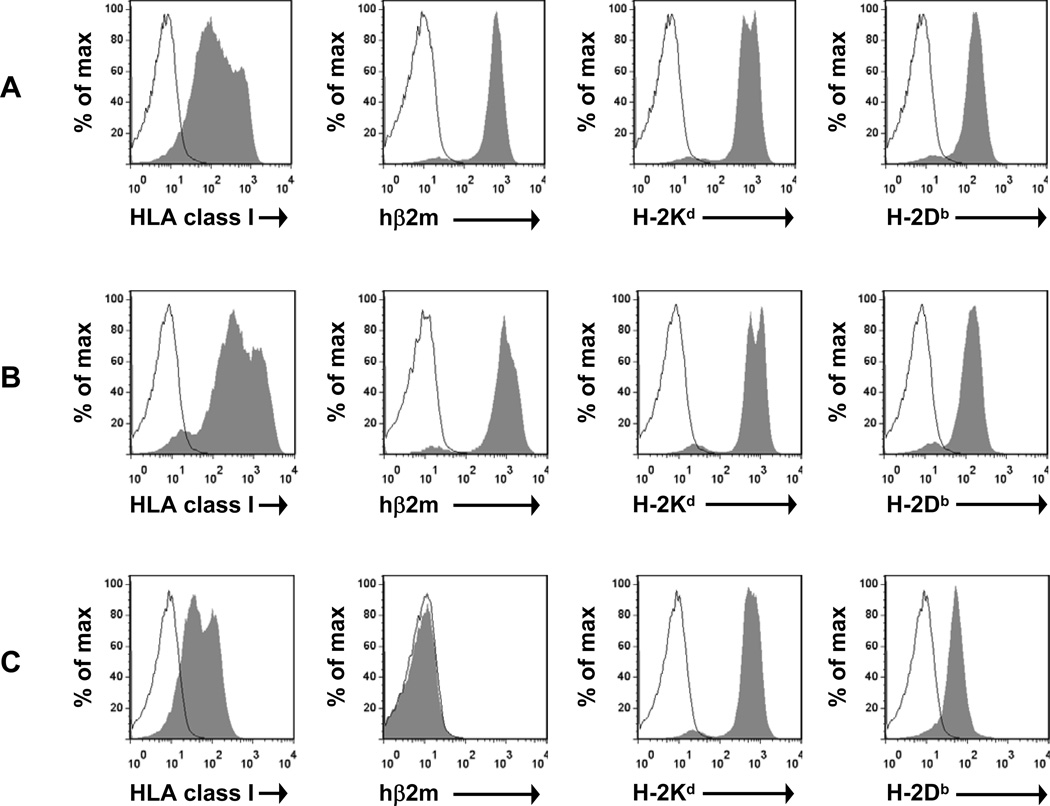
Splenocytes from NOD.mβ2mnull.hβ2m mice transgenic for HLA-A11 or HLA-B7 were analyzed by flow cytometry, which confirmed the cell-surface expression of the human β2m and HLA molecules (Fig. 1, A and B). As expected, expression of the endogenous NOD class I MHC molecules H-2Kd and H-2Db was also observed (Fig. 1, A and B).
FIGURE 1. NOD.mβ2mnull.hβ2m mice transgenic for HLA-A11 or HLA-B7 express the transgenic HLA molecule in addition to the endogenous NOD class I MHC molecules H-2Kd and H-2Db.
Splenocytes from (A) NOD.mβ2mnull.hβ2m.HLA-A11, (B) NOD.mβ2mnull.hβ2m.HLA-B7, or (C) NOD.HLA-A11 mice (expressing murine β2m) were analyzed by flow cytometry for cell-surface expression of the indicated molecules. Open histogram, unstained; filled histogram, stained.
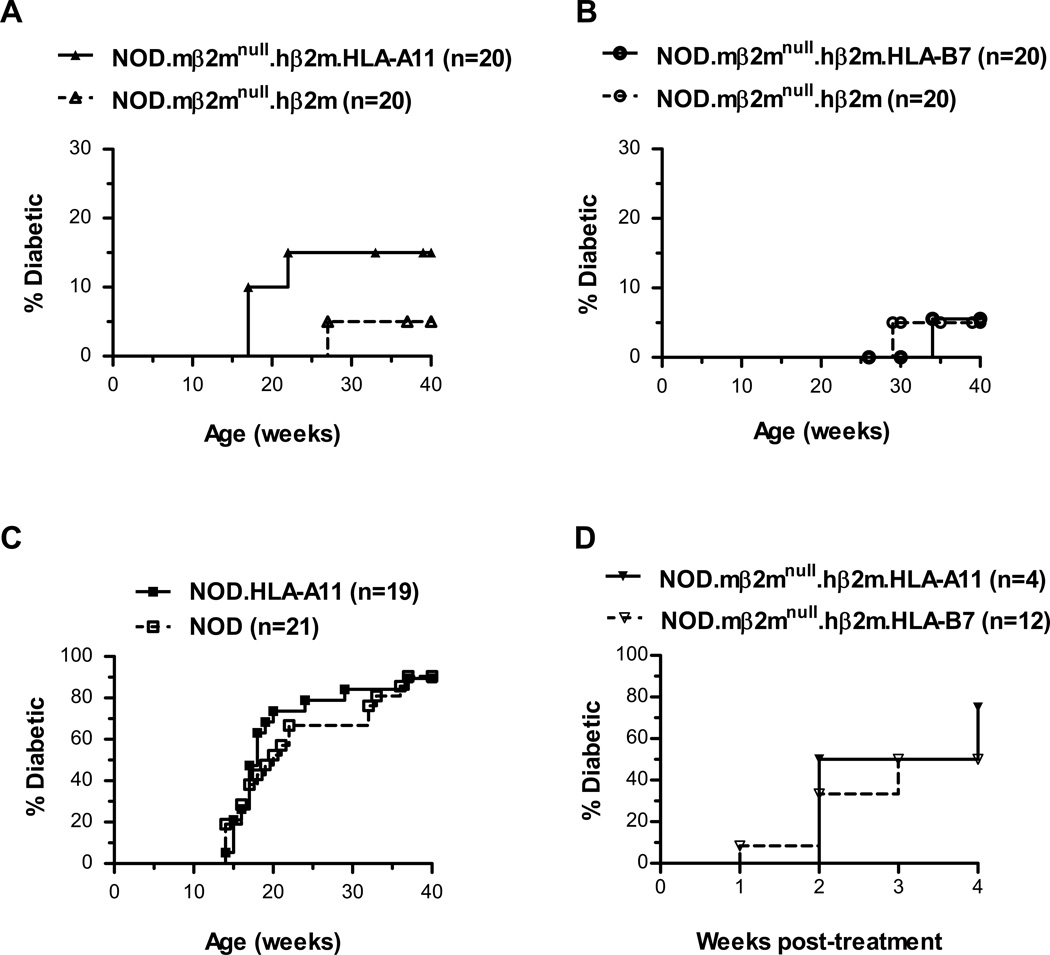
Both the NOD.mβ2mnull.hβ2m.HLA-A11 and NOD.mβ2mnull.hβ2m.HLA-B7 mice were diabetes-susceptible, albeit to varying degrees (Fig. 2, A and B) and far less so than standard NOD mice which had a diabetes incidence of 90% (Fig. 2C). As had been reported previously (45), even non-HLA-transgenic NOD.mβ2mnull.hβ2m mice showed reduced disease compared to standard NOD mice (Fig. 2, A–C). This phenomenon is believed to be due to the adoption of a non-diabetogenic conformation by murine class I MHC molecules containing human β2m (45). NOD mice expressing the endogenous murine β2m (instead of human β2m) along with the transgenic HLA-A11 heavy chain (designated NOD.HLA-A11 mice) still exhibited HLA-A11 expression (Fig. 1C), but showed a diabetes incidence curve indistinguishable from that of NOD mice (Fig. 2C), showing that HLA-A11 expression on its own does not protect from disease. We did not examine NOD.HLA-B7 mice, because prior work showed that HLA-B7 is poorly expressed in the absence of human β2m (55).
FIGURE 2. NOD.mβ2mnull.hβ2m mice transgenic for HLA-A11 or HLA-B7 are diabetes-susceptible to varying degrees.
A–C, Female HLA-transgenic mice of the indicated strains and their corresponding non-transgenic littermates were monitored weekly for diabetes development. D, Female mice of the indicated strains (12 to 21 weeks of age) were treated with two injections of 200 mg/kg cyclophosphamide i.p. two weeks apart. Diabetes incidence was monitored weekly after the first injection. The horizontal axis indicates weeks following the first injection.
To further characterize the NOD.mβ2mnull.hβ2m.HLA-A11 and NOD.mβ2mnull.hβ2m.HLA-B7 mice, we investigated whether cyclophosphamide treatment could accelerate disease as it does in standard NOD mice (48). For these experiments, female mice (12 to 21 weeks of age) were treated with two injections of 200 mg/kg cyclophosphamide i.p. two weeks apart. Diabetes incidence was monitored weekly after the first injection. As depicted in Fig. 2D, cyclophosphamide treatment induced disease in the majority of the treated animals. As cyclophosphamide acceleration of diabetes is associated with a reduction in regulatory T cells (47), these findings suggest that diabetogenic effectors are generated in the NOD.mβ2mnull.hβ2m.HLA-A11 and NOD.mβ2mnull.hβ2m.HLA-B7 mice, but that they are generally kept in check by regulatory mechanisms.
Identification of HLA-A11-restricted epitopes of IGRP and insulin
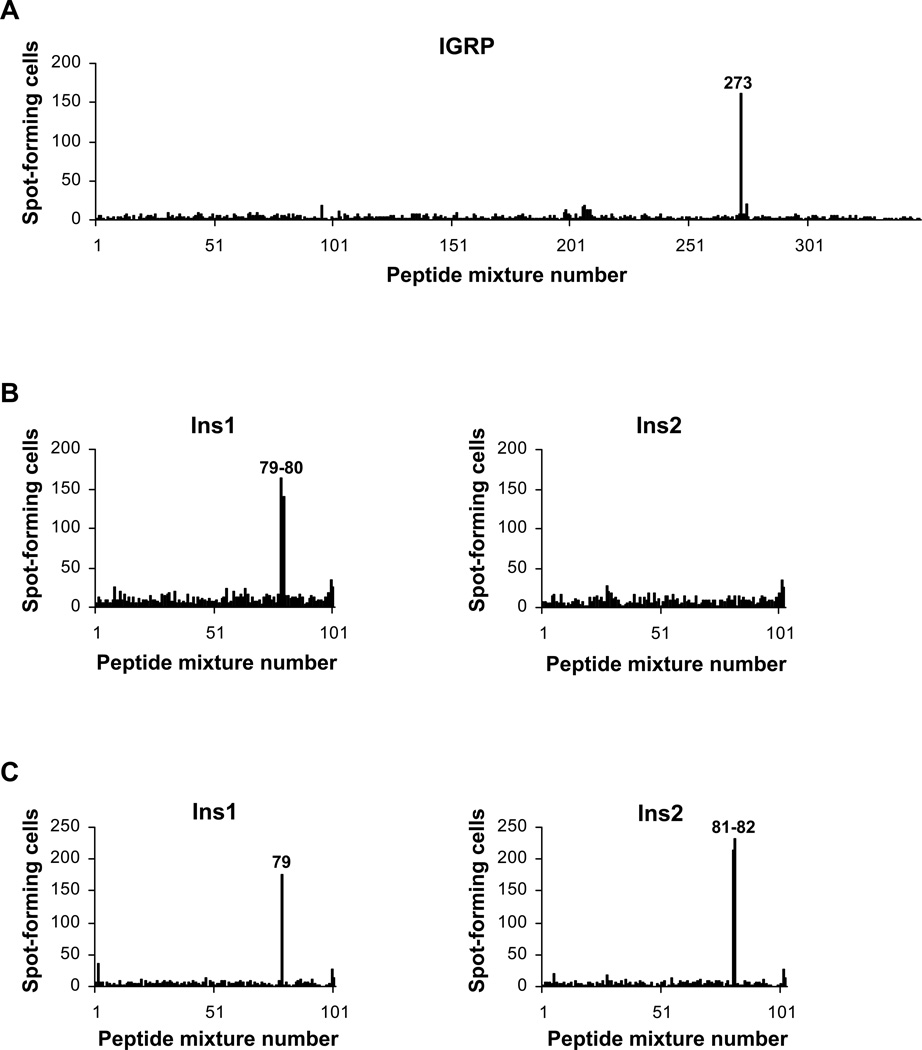
We previously showed that IGRP is an important antigenic target of pathogenic CD8+ T cells in both standard (56) and HLA-A2-transgenic NOD mice (30). To determine whether NOD.mβ2mnull.hβ2m.HLA-A11 mice similarly harbor HLA-A11-restricted T cells specific for this beta cell antigen, we used cultured islet-infiltrating T cells to screen, by IFN-γ ELISPOT assay, a peptide library containing all possible 8 to 11mer sequences that can be derived from murine IGRP. The library was offset by one residue, and the peptide mixtures in the library contained four sequences with a common C-terminus, but having a length of 8, 9, 10, or 11 residues. As shown in Fig. 3A, a strong T cell response was observed to peptide mixture 273. We next synthesized and tested the individual 8mer, 9mer, 10mer, and 11mer peptides comprising mixture 273 and found that the 9mer peptide IGRP 272–280, having the sequence AINSEMFLR, was the minimal epitope recognized by T cells (Fig. 4A). This sequence is consistent with the peptide-binding motif reported for HLA-A11, i.e., L, M, I, V, S, A, T, G, or N at position 2, and K or R at the C terminus (57). Interestingly, the peptide overlaps the HLA-A2-binding epitope IGRP 265–273. It should be noted that recognition of the 10mer and 11mer peptides from mixture 273 (Fig. 4A) most likely reflects proteolytic generation of the 9mer peptide during the assay period. However, it cannot be ruled out that these longer peptides represent epitopes distinct from the 9mer.
FIGURE 3. Islet-infiltrating T cells from NOD.mβ2mnull.hβ2m.HLA-A11 mice recognize IGRP and insulin peptides.
A, Islet-infiltrating T cells from a 17-week-old nondiabetic female NOD.mβ2mnull.hβ2m.HLA-A11 mouse were used to screen a murine IGRP peptide library by γ-IFN ELISPOT using syngeneic splenocytes pulsed with 1 µM peptide as antigen-presenting cells. B–C, Islet-infiltrating T cells from (B) two 15-week-old nondiabetic or (C) five 13- to 27-week-old diabetic female NOD.mβ2mnull.hβ2m.HLA-A11 mice were used to screen Ins1 and Ins2 peptide libraries as in (A). Numbers corresponding to the reactive mixtures are indicated.
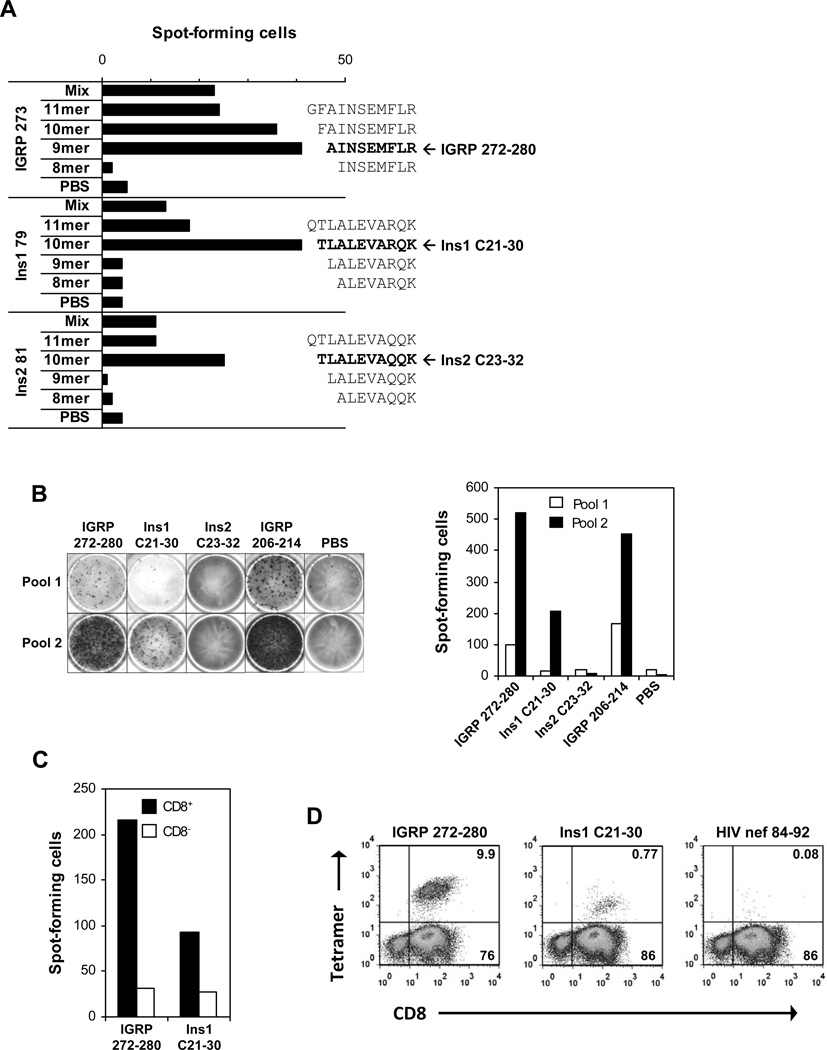
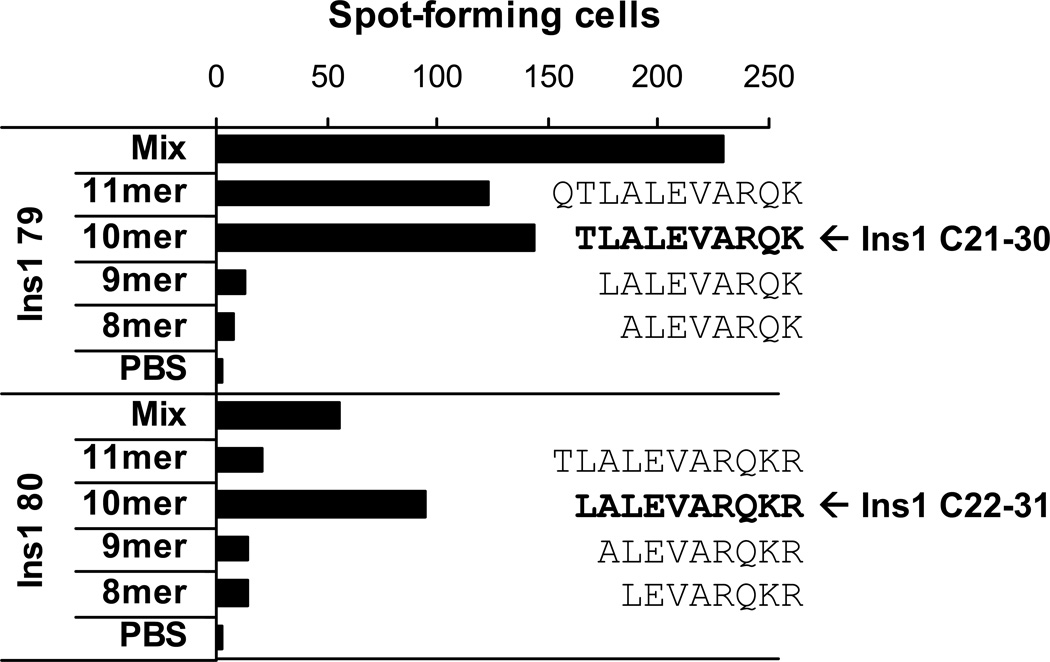
FIGURE 4. Characterization of IGRP and insulin epitopes recognized by islet-infiltrating CD8+ T cells from NOD.mβ2mnull.hβ2m.HLA-A11 mice.
A–C, Islet-infiltrating T cells from female NOD.mβ2mnull.hβ2m.HLA-A11 mice were tested by γ-IFN ELISPOT for reactivity to the indicated peptide mixtures or individual peptides. Independent T cell cultures were used for each of the panels. A, Reactivity to peptide mixtures IGRP 273, Ins1 79, and Ins2 81 as well as the individual peptides making up those mixtures was examined. Diabetic mice were used as the T cell source for the top set of bars, while nondiabetic mice were used for the two lower sets. The peptide sequences are shown next to their corresponding bars, and the minimal epitopes for each mixture are shown in bold. B, Representative ELISPOT wells and a graphic representation of spot numbers for two independent T cell cultures (Pool 1, nondiabetic mice; Pool 2, diabetic mice). C, Islet-infiltrating cells from nondiabetic mice were separated based on CD8 positivity, and the CD8+ and CD8− enriched populations were tested for reactivity to the indicated peptides. D, Islet-infiltrating T cells from diabetic female NOD.mβ2mnull.hβ2m.HLA-A11 mice were stained with anti-CD8 and the indicated peptide/HLA-A11 tetramers and analyzed by flow cytometry. Numbers denote the percentage of cells in the corresponding quadrants.
Peptide libraries representing the two insulin proteins expressed in mice, i.e., Ins1 and Ins2, were screened similarly using islet-infiltrating T cells pooled from two independent sets of NOD.mβ2mnull.hβ2m.HLA-A11 mice (Fig. 3, B and C). Several peptide mixtures elicited positive responses, some of which were observed with only one of the T cell pools (e.g., Ins2 81–82), and some of which were in common to both pools (e.g., Ins1 79). We identified Ins1 C21-30 (TLALEVARQK) as the minimal epitope present in mixture Ins1 79, and Ins2 C23-32 (TLALEVAQQK) was found to be the minimal epitope present in mixture Ins2 81 (Fig. 4A). Though these two peptides differ at only a single position, their status as independent epitopes is suggested by the finding that some T cell pools responded only to mixture Ins1 79, and not to Ins2 81 (Fig. 3B, 4B).
When screening peptide libraries designed as ours were, a doublet of reactivity is sometimes seen. In this case, the true epitope is generally present in the first positive peptide mixture, but reactivity is sometimes observed to the next mixture due to proteolytic generation of the epitope from a longer peptide during the assay period. This likely explains the reactivity observed to Ins2 mixtures 81 and 82, as we did not see reactivity to one but not the other in any of our experiments (Fig. 3C and data not shown). However, careful examination of our peptide library screening results revealed that the doublet of reactivity observed for Ins1 mixtures 79 and 80 (Fig. 3B) likely represents two independent epitopes, as the T cells tested in Fig. 3C responded to mixture 79 but not mixture 80. To confirm that mixture 80 contained an epitope independent from Ins1 C21-30 (the peptide responsible for reactivity to mixture 79), we indentified another T cell pool that showed reactivity to both mixtures, and we screened it against the individual peptides comprising these mixtures. If reactivity to mixture 80 was due to proteolytic cleavage of a peptide generating Ins1 C21-30, we would have expected the 11mer of this mixture to give the strongest response. However, we found instead that the 10mer was the minimal epitope responsible for the reactivity observed to mixture Ins1 80 (Fig. 5). Taken together with our peptide library screening results (Fig. 3, B and C), these findings confirm the 10mer peptide Ins1 C22-31 as an independent epitope.
FIGURE 5. Ins1 C21-30 and Ins1 C22-31 are independent C-peptide-derived T cell epitopes in NOD.mβ2mnull.hβ2m.HLA-A11 mice.
Islet-infiltrating T cells from a diabetic female NOD.mβ2mnull.hβ2m.HLA-A11 mouse were tested by γ-IFN ELISPOT for reactivity to peptide mixtures Ins1 79 and Ins1 80 as well as the individual peptides making up those mixtures. The peptide sequences are shown next to their corresponding bars, and the minimal epitopes for each mixture are shown in bold. Similar results were obtained using islet-infiltrating cells from nondiabetic mice (data not shown).
T cells cultured from islets of NOD.mβ2mnull.hβ2m.HLA-A11 mice according to our protocol generally contained nearly 90% CD8+ T cells (Fig. 4D). Nonetheless, to confirm that CD8+ T cells were indeed responsible for the IFN-γ responses we observed, we magnetically separated CD8+ and CD8− islet-infiltrating cell populations and tested them for reactivity to the predominant epitopes IGRP 272–280 and Ins1 C21-30. We found that reactivity was enriched 3- to 7-fold in the CD8+ population (Fig. 4C). Finally, we wished to verify that these peptides were recognized by CD8+ T cells restricted to the transgenic HLA-A11 molecules rather than to the endogenous NOD class I MHC molecules H-2Kd and H-2Db which are also expressed in the NOD.mβ2mnull.hβ2m.HLA-A11 mice (Fig. 1A). When we stained islet-infiltrating T cells from these mice with peptide/HLA-A11 tetramers (containing the α3 domain from H-2Kb as found in the HLA-A11-transgenic mice), a clear population of CD8+ T cells bound the IGRP 272–280/HLA-A11 or the Ins1 C21-30/HLA-A11 tetramers, while this was not the case for the irrelevant HIV nef/HLA-A11 reagent (Fig. 4D). In addition to confirming MHC restriction, this flow cytometry analysis also confirmed that the CD8+ T cell population was responsible for the peptide reactivities we observed.
Table I provides a summary of the peptides we found to be recognized by HLA-A11-restricted islet-infiltrating T cells in NOD.mβ2mnull.hβ2m.HLA-A11 mice. Importantly, these experiments have identified the insulin C-peptide as a rich source of CD8+ T cell epitopes.
Table I.
MHC binding capacity of mouse peptides recognized by islet-infiltrating HLA-restricted T cells in HLA-transgenic NOD mice and their human equivalents
| A: HLA-A*1101-transgenic NOD mice | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Binding to A3 supertype members (IC50, nM) | |||||||||
| Organism | Position | Sequence | A*1101 | A*0301 | A*3001 | A*3101 | A*3301 | A*6601 | A*6801 |
| Mouse | IGRP 272–280 | AINSEMFLRa | 209 | 428 | 49752 | 67 | 1081 | 4547 | 109 |
| Human | IGRP 272–280 | AINSEMFLL | 2824 | 1258 | 6776 | 1071 | 12784 | 36672 | 14186 |
| Mouse | Ins1 C21-30 | TLALEVARQK | 3327 | 605 | 23280 | 13026 | 25455 | – b | 13432 |
| Mouse | Ins2 C23-32 | TLALEVAQQK | 833 | 856 | – | – | – | – | 7494 |
| Human | Ins C23-32 | PLALEGSLQKc | 37072 | 20873 | – | 39403 | – | 48509 | 41456 |
| Mouse | Ins1 C22-31 | LALEVARQKR | – | 43592 | 42979 | 10808 | 9145 | 12966 | 12582 |
| Human | Ins C24-33 | LALEGSLQKR | 34461 | 17521 | – | 38387 | 3271 | 515 | 66 |
| B: HLA-B*0702-transgenic NOD mice | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Binding to B7 supertype members (IC50, nM) | |||||||||
| Organism | Position | Sequence | B*0702 | B*3501 | B*3503 | B*4201 | B*5101 | B*5301 | B*5401 |
| Mouse | Ins1 C15-24 | SPGDLQTLAL | 4.4 | – | 16115 | 35 | – | 10987 | – |
| Human | Ins C15-26 | GPGAGSLQPLAL | 462 | – | – | 6066 | – | 15456 | – |
bold and underlined letters indicate amino acid identity between murine and human peptides
dash indicates IC50 > 50000 nM
recently reported as an HLA-A3-restricted epitope in humans (26)
Epitope mapping using HLA-B7 transgenic mice
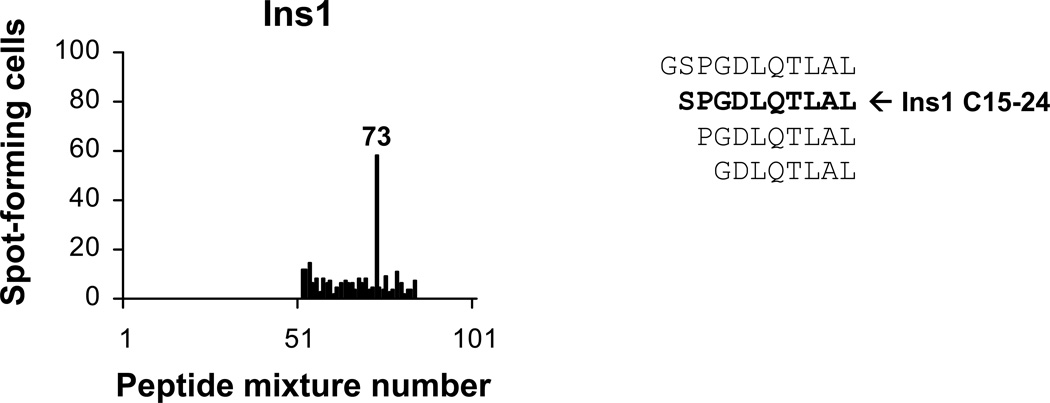
Because the low spontaneous disease incidence observed in the HLA-B7-transgenic NOD.mβ2mnull.hβ2m mice (Fig. 2B) made it difficult to collect sufficient numbers of islet-infiltrating T cells, it was not possible to do the extensive screens and characterizations carried out for the HLA-A11-transgenic mice. However, given our identification of three C-peptide-derived epitopes in the HLA-A11-transgenic mice, we used islet-infiltrating T cells from the HLA-B7-transgenic mice to perform a limited screen of the Ins1 peptide library that was restricted to the C-peptide and its flanking regions. Remarkably, mixture 73 elicited a positive T cell response (Fig. 6). Based on the peptide binding motif described for HLA-B*0702 (P at position 2, and L at the C terminus) (58), the 10mer peptide in this mixture (Ins1 C15-24; SPGDLQTLAL) is most certainly responsible for the activity observed. Consistent with this idea is our finding that the 10mer peptide Ins1 C15-24 bound very well to HLA-B*0702 (IC50 of 4.4 nM in a competitive binding assay; Table I).
FIGURE 6. Islet-infiltrating T cells from NOD.mβ2mnull.hβ2m.HLA-B7 mice recognize a C-peptide-derived insulin epitope.
Islet-infiltrating T cells from four 15-week-old nondiabetic female NOD.mβ2mnull.hβ2m.HLA-B7 mice were used to conduct a partial screen of an Ins1 peptide library (C-peptide and flanking regions; mixtures 52–84) by γ-IFN ELISPOT using syngeneic splenocytes pulsed with 1 µM peptide as antigen-presenting cells. The number of the reactive mixture is indicated, and the individual peptides making up that mixture are shown. The predicted minimal epitope is shown in bold.
The identified epitopes bind multiple members of the corresponding HLA supertype
Members of an HLA supertype show overlap in peptide-binding repertoires (40, 42). To determine whether the epitopes we identified using HLA-A11-transgenic NOD mice were capable of binding other alleles of the A3 supertype, we performed competitive peptide-binding assays under conditions where the measured IC50 is a reasonable approximation of the true Kd (Table I). Murine IGRP 272–280 exhibited strong to intermediate binding (IC50 < 500 nm) not only to HLA-A*1101, but also to three other A3 supertype members (A*0301, A*3101, and A*6801). In addition, binding to other A3 supertype alleles was detectable, albeit with weak affinity (IC50 between 500 nM and 5000 nM; A*3301 and A*6601). Importantly, human IGRP 272–280 also showed binding to A*1101 and to certain other members of the A3 supertype, albeit to varying degrees and generally lower affinity, perhaps reflective of the fact that it bears a less optimal A3 supertype motif. In the case of the murine insulin epitopes we identified and their human equivalents, some of these bound multiple members of the corresponding HLA supertype also (Table I).
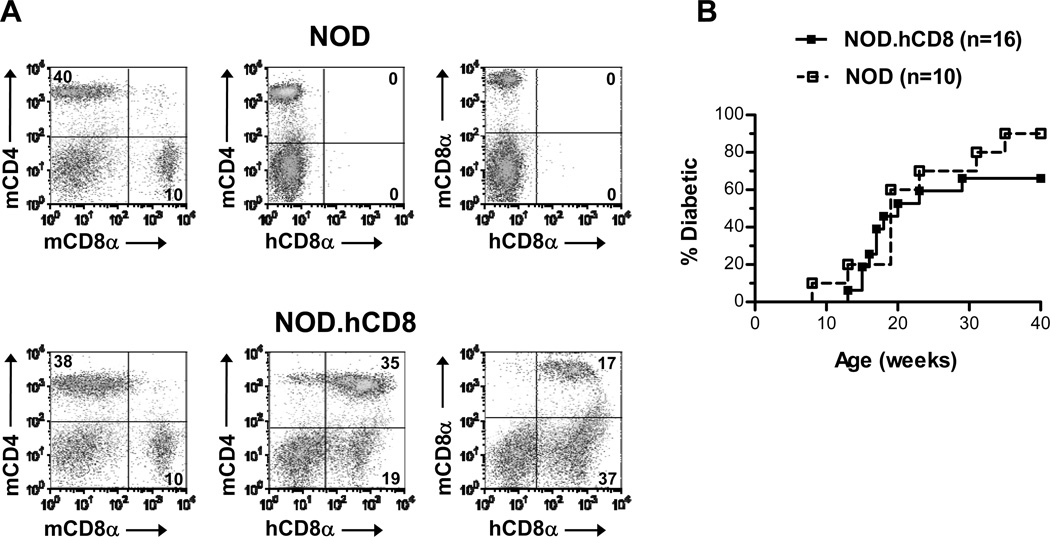
NOD.hCD8 mice are diabetes-susceptible
Our mapping of HLA-A11-restricted epitopes using our HLA-transgenic NOD.mβ2mnull.hβ2m mice was likely aided by the chimeric nature of the transgenic HLA-A11 molecule in which the α3 domain was derived from the murine class I MHC molecule H-2Kb. This would be expected to facilitate HLA-A11-restricted T cell responses, as murine CD8 interacts preferentially with the murine α3 domain compared to the human α3 domain (59, 60). Future epitope mapping studies employing NOD mice transgenic for fully human class I MHC heavy chains would thus likely benefit from the co-expression of human CD8. To this end, we took advantage of a previously described strain of C57BL/6 mice transgenically expressing human CD8 under the control of the murine T cell-specific p56lck proximal promoter (46). We used these mice to introduce human CD8 to NOD mice, backcrossed for at least 10 generations, and then analyzed T cell populations and diabetes incidence in the newly developed NOD.hCD8 strain. As reported for the C56BL/6 mice expressing human CD8 (46), the murine CD4+:murine CD8+ T cell ratio was unaltered by the expression of human CD8, and human CD8 was expressed on both murine CD4+ and murine CD8+ T cells (Fig. 7A). Diabetes development in NOD.hCD8 females was as observed for NOD mice (Fig. 7B). This supports the idea that introduction of hCD8 to NOD models transgenic for fully human class I MHC chains will increase their usefulness for epitope mapping studies. Such work is already in progress in our laboratory.
FIGURE 7. NOD.hCD8 mice exhibit a normal murine CD4+:CD8+ T cell ratio and are diabetes-susceptible.
A, Splenocytes from NOD and NOD.hCD8 mice were analyzed by flow cytometry for cell-surface expression of the indicated markers. Numbers denote the percentage of cells in the corresponding quadrants. B, Female NOD and NOD.hCD8 mice were monitored weekly for diabetes development. The two incidence curves were not statistically different (p = 0.48; log-rank test).
DISCUSSION
While multiple beta cell peptides have been identified as the antigenic targets of CD8+ T cells in type 1 diabetes patients, nearly all of these are recognized in the context of HLA-A*0201 (12). Thus, they are only relevant to a subset of patients (32). While the gene frequency of HLA-A*1101, studied here, is generally lower than that of HLA-A*0201, e.g., 7% and 27% among the Caucasian population in the United States, respectively (61), HLA-A*1101 is a representative member of the A3 supertype, which has a phenotypic frequency of 38–53%, depending on the ethnic group examined (39). This compares favorably to the phenotypic frequency of 39–46% for the A2 supertype (39), of which HLA-A*0201 is a member. In addition to HLA-A*1101, other A3 supertype members include A*0301, A*3101, A*3301, and A*6801 (39). The A3 supertype is characterized by a B-pocket specificity (position 2 of the peptide) for the amino acids A, I, L, M, V, S, or T, and an F-pocket specificity (peptide C-terminus) for R or K (39). Importantly, this supertype has been functionally verified, meaning that it has been established that a peptide that binds one member of the supertype will likely bind other members as well (40). This led us to hypothesize that antigenic beta cell peptides identified using the HLA-A11-transgenic NOD mice would have relevance to humans expressing other members of the A3 supertype. This has now been confirmed by a very recent report which identified the human equivalent of an epitope we mapped using our mice (i.e., human Ins C23-32, and having the sequence PLALEGSLQK; Table I) as being recognized in the context of HLA-A3 in type 1 diabetes patients (26). This finding, coupled with our MHC binding results (Table I), supports the idea that the other epitopes we identified using the HLA-A11-transgenic NOD mice should also be examined for their relevance in patients.
When the transgenic HLA-A11 molecules expressed in NOD mice contained murine β2m, diabetes incidence was much higher than that observed when human β2m was expressed instead (Fig. 1, A and C). Nonetheless, we chose to conduct our epitope mapping studies in the context of human β2m, so that the transgenic HLA molecules would resemble their human counterparts as closely as possible. For example, HLA class I heavy chains associated with murine β2m appear to take on an altered structure (as measured by antibody reactivity) compared to those associated with human β2m (62). This suggests that the peptide-binding repertoire might also be altered. Interestingly, we searched for T cell responses to our newly identified HLA-A11-binding epitopes IGRP 272–280 and Ins1 C21-30 using islet-infiltrating T cells derived from thirteen NOD.HLA-A11 mice (expressing murine β2m), and we were unable to detect reactivity (data not shown). While this might reflect altered peptide binding, it could instead, or in addition, be due to an altered T cell repertoire. Murine class I MHC molecules containing human β2m are apparently non-diabetogenic and fail to support the development of beta cell-specific T cell responses (45). Thus, in the NOD.mβ2mnull.hβ2m.HLA-A11 strain, beta cell-specific T cells restricted to the transgenic HLA molecules may enjoy reduced competition from those restricted to the murine class I MHC molecules.
Despite the diabetes-protective effect of hβ2m in NOD.mβ2mnull.hβ2m mice alluded to immediately above (45), diabetes susceptibility is restored when the HLA-A2 heavy chain is also expressed (63). In contrast, expression of either the HLA-A11 or the HLA-B7 heavy chain in NOD.mβ2mnull.hβ2m mice is insufficient to overcome the protective effect of hβ2m (Fig. 2, A and B). This intriguing phenomenon may be related to the finding that HLA-A2 is a susceptibility allele for type 1 diabetes in humans, while HLA-A11 and HLA-B7 are not (4, 6).
Spontaneous CD8+ T cell responses to only a limited number of epitopes entirely contained within the insulin C-peptide (hIns C20-28 for HLA-A2 and HLA-A3, and hIns C23-32 for HLA-A3) have been reported previously (Fig. 8) (25, 26). Our identification of four such peptides in our work (Ins1 C21-30, Ins2 C23-32, and Ins1 C22-31 for HLA-A11, and Ins1 C15-24 for HLA-B7) (Fig. 8) establishes the C-peptide as a rich source of disease-relevant CD8+ T cell epitopes. In humans, reactivities to C-peptide epitopes may be particularly informative as they cannot represent an immune response to exogenously administered insulin.
FIGURE 8. CD8+ T cell epitopes of insulin contained within the C-peptide and targeted by spontaneous T cell responses.
An alignment of murine insulin 1 and insulin 2 and human insulin is shown. Prohormone convertase cleavage sites are denoted by arrows, and residues trimmed by carboxypeptidase E are depicted in black. C-peptide epitopes identified in the current study are indicated with solid brackets, while those identified in patients and reported elsewhere (25, 26) are marked with dashed brackets. The restricting MHC is noted in each case.
It is possible that the C-termini of some of the peptides identified here (Ins1 C21-30 and Ins2 C23-32) may be generated independently of the proteasome. This is an important point, as proteasomal cleavage is often taken as a prerequisite for the examination of candidate T cell epitopes in human studies. Proteasome-independent generation of the C-terminus of an HLA-A3-restricted viral epitope (ELFSYLIEK) has recently been reported (64). In that study, the peptide C-terminus was instead found to be generated by the cytosolic endopeptidase nardilysin. As nardilysin cleaves before or between dibasic residues, its involvement in the generation of Ins1 C21-30 and Ins2 C23-32 (Fig. 8) should be considered.
Like HLA-A*0201 and A*1101, B*0702 is also a member of a well-characterized and functionally verified HLA supertype, i.e., the B7 supertype (42). While here we were only able to conduct limited epitope mapping studies using the NOD.mβ2mnull.hβ2m.HLA-B7 mice, we did successfully identify Ins1 C15-24 as an antigen (Fig. 6). Importantly, the human counterpart of Ins1 C15-24 (i.e., Ins C15-26) is capable of binding to B*0702 with high affinity (Table I). To our knowledge, only one other HLA-B7-binding epitope derived from a beta cell antigen (Ins L4-13) has been identified to date (26). As the B7 supertype has a phenotypic frequency of 43–57% (39), further investigation is clearly warranted. We anticipate that introduction of human CD8 from our newly developed NOD.hCD8 strain (Fig. 7) to the HLA-B7-transgenic NOD mice will further increase their utility for antigen discovery experiments (59, 60).
Although we have not yet proven directly that the T cell reactivities we have identified here are pathogenic, their presence within the pancreatic islets prior to disease development (Fig. 3, A and B; Fig. 4, A–C; Fig. 6; and data not shown) certainly supports this idea, as does their secretion of IFN-γ in response to antigen stimulation. Also, we have previously shown, using both standard and HLA-A2-transgenic NOD mice, that T cell specificities identified using islet-infiltrating cells and IFN-γ ELISPOT assays do indeed exhibit cytotoxicity in vivo (28). In addition to using islet-infiltrating cells to identify disease-relevant antigens, our MHC binding results suggest that it is also important to look for candidate epitopes in an unbiased way, as we have done, rather than limit candidates to those that bind well to MHC. As seen in Table I, the mouse epitopes we identified bound to MHC with a wide range of affinities. Despite these advantages of our epitope mapping approach, one drawback is that some of the peptides identified may not be relevant to the human disease due to sequence differences between the mouse and human versions. For example, human preproinsulin and IGRP are only approximately 80% identical to their mouse counterparts. Ideally, then, human autoantigens would be introduced into HLA-transgenic NOD mouse models in the future. The establishment of NOD mice transgenically expressing human IGRP in beta cells is an important first step toward this goal (65).
T cell epitope mapping continues to be a major research effort for a number of laboratories, and this interest is due, at least in part, to the potential of such work to identify peptides that could be useful for the development of preventive or therapeutic strategies. As suggested by a recent report (21), it is possible that manipulation of multiple specificities will be beneficial, if not required, so the more that is known about the relevant epitopes, the more successful the field is likely to be. Identification of new epitopes will also increase the utility of T cell assays, which have begun to show promise as tools for immune monitoring in type 1 diabetes, e.g., to identify beta cell autoimmunity in patients (25); to predict islet graft rejection (26, 27); or to confirm the immunological efficacy of intervention therapies regardless of their clinical outcome (66), information that could be used to guide subsequent clinical trials. When the A2, A3, and B7 supertypes are considered together, the population coverage provided ranges from 83–88%, depending on the population examined (39). Thus, increased knowledge of the beta cell peptides recognized in the context of representative supertype members should result in immunological tools relevant to large numbers of individuals.
ACKNOWLEDGMENTS
We thank Ignacio Guerrero Ros for critical reading of the manuscript.
Footnotes
This work was supported by National Institutes of Health grants R01 DK064315 (T.P.D.) and P60 DK020541 (Albert Einstein College of Medicine’s Diabetes Research and Training Center) and by grants from the Juvenile Diabetes Research Foundation (T.P.D.) and the Irma T. Hirschl/Monique Weill-Caulier Trust (T.P.D.). The flow cytometry facility at Albert Einstein College of Medicine is supported by National Institutes of Health Cancer Center grant P30 CA013330. The contributions of Y.Y. and P.S. were supported by grants from the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada, and the Juvenile Diabetes Research Foundation. P.S. is a Juvenile Diabetes Research Foundation Scholar and a Scientist of Alberta Innovates – Health Solutions. The Julia McFarlane Diabetes Research Centre is supported by the Diabetes Association (Foothills) and the Canadian Diabetes Association.
Abbreviations used in this paper: β2m, β2-microglobulin; IGRP, islet-specific glucose-6-phosphatase catalytic subunit-related protein; Ins, insulin.
REFERENCES
- 1.Cucca F, Lampis R, Congia M, Angius E, Nutland S, Bain SC, Barnett AH, Todd JA. A correlation between the relative predisposition of MHC class II alleles to type 1 diabetes and the structure of their proteins. Hum. Mol. Genet. 2001;10:2025–2037. doi: 10.1093/hmg/10.19.2025. [DOI] [PubMed] [Google Scholar]
- 2.Fennessy M, Metcalfe K, Hitman GA, Niven M, Biro PA, Tuomilehto J, Tuomilehto-Wolf E. A gene in the HLA class I region contributes to susceptibility to IDDM in the Finnish population. Childhood Diabetes in Finland (DiMe) Study Group. Diabetologia. 1994;37:937–944. doi: 10.1007/BF00400951. [DOI] [PubMed] [Google Scholar]
- 3.Honeyman MC, Harrison LC, Drummond B, Colman PG, Tait BD. Analysis of families at risk for insulin-dependent diabetes mellitus reveals that HLA antigens influence progression to clinical disease. Mol. Med. 1995;1:576–582. [PMC free article] [PubMed] [Google Scholar]
- 4.Howson JM, Walker NM, Clayton D, Todd JA. Confirmation of HLA class II independent type 1 diabetes associations in the major histocompatibility complex including HLA-B and HLA-A. Diabetes Obes. Metab. 2009;11(Suppl 1):31–45. doi: 10.1111/j.1463-1326.2008.01001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakanishi K, Kobayashi T, Murase T, Naruse T, Nose Y, Inoko H. Human leukocyte antigen-A24 and -DQA1*0301 in Japanese insulin-dependent diabetes mellitus: independent contributions to susceptibility to the disease and additive contributions to acceleration of β-cell destruction. J. Clin. Endocrinol. Metab. 1999;84:3721–3725. doi: 10.1210/jcem.84.10.6045. [DOI] [PubMed] [Google Scholar]
- 6.Nejentsev S, Howson JM, Walker NM, Szeszko J, Field SF, Stevens HE, Reynolds P, Hardy M, King E, Masters J, Hulme J, Maier LM, Smyth D, Bailey R, Cooper JD, Ribas G, Campbell RD, Clayton DG, Todd JA. Localization of type 1 diabetes susceptibility to the MHC class I genes HLA-B and HLA-A. Nature. 2007;450:887–892. doi: 10.1038/nature06406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nejentsev S, Reijonen H, Adojaan B, Kovalchuk L, Sochnevs A, Schwartz EI, Akerblom HK, Ilonen J. The effect of HLA-B allele on the IDDM risk defined by DRB1*04 subtypes and DQB1*0302. Diabetes. 1997;46:1888–1892. doi: 10.2337/diab.46.11.1888. [DOI] [PubMed] [Google Scholar]
- 8.Noble JA, Valdes AM, Bugawan TL, Apple RJ, Thomson G, Erlich HA. The HLA class I A locus affects susceptibility to type 1 diabetes. Hum. Immunol. 2002;63:657–664. doi: 10.1016/s0198-8859(02)00421-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noble JA, Valdes AM, Varney MD, Carlson JA, Moonsamy P, Fear AL, Lane JA, Lavant E, Rappner R, Louey A, Concannon P, Mychaleckyj JC, Erlich HA. HLA class I and genetic susceptibility to type 1 diabetes: results from the Type 1 Diabetes Genetics Consortium. Diabetes. 2010;59:2972–2979. doi: 10.2337/db10-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robles DT, Eisenbarth GS, Wang T, Erlich HA, Bugawan TL, Babu SR, Barriga K, Norris JM, Hoffman M, Klingensmith G, Yu L, Rewers M. Identification of children with early onset and high incidence of anti-islet autoantibodies. Clin. Immunol. 2002;102:217–224. doi: 10.1006/clim.2001.5171. [DOI] [PubMed] [Google Scholar]
- 11.Tait BD, Colman PG, Morahan G, Marchinovska L, Dore E, Gellert S, Honeyman MC, Stephen K, Loth A. HLA genes associated with autoimmunity and progression to disease in type 1 diabetes. Tissue Antigens. 2003;61:146–153. doi: 10.1034/j.1399-0039.2003.00013.x. [DOI] [PubMed] [Google Scholar]
- 12.DiLorenzo TP, Peakman M, Roep BO. Translational mini-review series on type 1 diabetes: Systematic analysis of T cell epitopes in autoimmune diabetes. Clin. Exp. Immunol. 2007;148:1–16. doi: 10.1111/j.1365-2249.2006.03244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bottazzo GF, Dean BM, McNally JM, MacKay EH, Swift PG, Gamble DR. In situ characterization of autoimmune phenomena and expression of HLA molecules in the pancreas in diabetic insulitis. N. Engl. J. Med. 1985;313:353–360. doi: 10.1056/NEJM198508083130604. [DOI] [PubMed] [Google Scholar]
- 14.Coppieters KT, Dotta F, Amirian N, Campbell PD, Kay TW, Atkinson MA, Roep BO, von Herrath MG. Demonstration of islet-autoreactive CD8 T cells in insulitic lesions from recent onset and long-term type 1 diabetes patients. J. Exp. Med. 2012;209:51–60. doi: 10.1084/jem.20111187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Itoh N, Hanafusa T, Miyazaki A, Miyagawa J, Yamagata K, Yamamoto K, Waguri M, Imagawa A, Tamura S, Inada M, Kawata S, Tarui S, Kono N, Matsuzawa Y. Mononuclear cell infiltration and its relation to the expression of major histocompatibility complex antigens and adhesion molecules in pancreas biopsy specimens from newly diagnosed insulin-dependent diabetes mellitus patients. J. Clin. Invest. 1993;92:2313–2322. doi: 10.1172/JCI116835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santamaria P, Lewis C, Jessurun J, Sutherland DE, Barbosa JJ. Skewed T-cell receptor usage and junctional heterogeneity among isletitis αβ and γδ T-cells in human IDDM. Diabetes. 1994;43:599–606. doi: 10.2337/diab.43.4.599. [DOI] [PubMed] [Google Scholar]
- 17.Somoza N, Vargas F, Roura-Mir C, Vives-Pi M, Fernandez-Figueras MT, Ariza A, Gomis R, Bragado R, Marti M, Jaraquemada D, Pujol-Borrell R. Pancreas in recent onset insulin-dependent diabetes mellitus. Changes in HLA, adhesion molecules and autoantigens, restricted T cell receptor Vβ usage, and cytokine profile. J. Immunol. 1994;153:1360–1377. [PubMed] [Google Scholar]
- 18.DiLorenzo TP, Serreze DV. The good turned ugly: immunopathogenic basis for diabetogenic CD8+ T cells in NOD mice. Immunol. Rev. 2005;204:250–263. doi: 10.1111/j.0105-2896.2005.00244.x. [DOI] [PubMed] [Google Scholar]
- 19.Amrani A, Verdaguer J, Serra P, Tafuro S, Tan R, Santamaria P. Progression of autoimmune diabetes driven by avidity maturation of a T-cell population. Nature. 2000;406:739–742. doi: 10.1038/35021081. [DOI] [PubMed] [Google Scholar]
- 20.Han B, Serra P, Amrani A, Yamanouchi J, Maree AF, Edelstein-Keshet L, Santamaria P. Prevention of diabetes by manipulation of anti-IGRP autoimmunity: high efficiency of a low-affinity peptide. Nat. Med. 2005;11:645–652. doi: 10.1038/nm1250. [DOI] [PubMed] [Google Scholar]
- 21.Niens M, Grier AE, Marron M, Kay TW, Greiner DL, Serreze DV. Prevention of "humanized" diabetogenic CD8 T-cell responses in HLA-transgenic NOD mice by a multipeptide coupled-cell approach. Diabetes. 2011;60:1229–1236. doi: 10.2337/db10-1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scott GS, Fishman S, Khai Siew L, Margalit A, Chapman S, Chervonsky AV, Wen L, Gross G, Wong FS. Immunotargeting of insulin reactive CD8 T cells to prevent diabetes. J. Autoimmun. 2010;35:390–397. doi: 10.1016/j.jaut.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 23.Tsai S, Shameli A, Yamanouchi J, Clemente-Casares X, Wang J, Serra P, Yang Y, Medarova Z, Moore A, Santamaria P. Reversal of autoimmunity by boosting memory-like autoregulatory T cells. Immunity. 2010;32:568–580. doi: 10.1016/j.immuni.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 24.Vincent BG, Young EF, Buntzman AS, Stevens R, Kepler TB, Tisch RM, Frelinger JA, Hess PR. Toxin-coupled MHC class I tetramers can specifically ablate autoreactive CD8+ T cells and delay diabetes in nonobese diabetic mice. J. Immunol. 2010;184:4196–4204. doi: 10.4049/jimmunol.0903931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mallone R, Martinuzzi E, Blancou P, Novelli G, Afonso G, Dolz M, Bruno G, Chaillous L, Chatenoud L, Bach J-M, van Endert P. CD8+ T-cell responses identify β-cell autoimmunity in human type 1 diabetes. Diabetes. 2007;56:613–621. doi: 10.2337/db06-1419. [DOI] [PubMed] [Google Scholar]
- 26.Unger WW, Velthuis J, Abreu JR, Laban S, Quinten E, Kester MG, Reker-Hadrup S, Bakker AH, Duinkerken G, Mulder A, Franken KL, Hilbrands R, Keymeulen B, Peakman M, Ossendorp F, Drijfhout JW, Schumacher TN, Roep BO. Discovery of low-affinity preproinsulin epitopes and detection of autoreactive CD8 T-cells using combinatorial MHC multimers. J. Autoimmun. 2011;37:151–159. doi: 10.1016/j.jaut.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 27.Velthuis JH, Unger WW, Abreu JR, Duinkerken G, Franken K, Peakman M, Bakker AH, Reker-Hadrup S, Keymeulen B, Drijfhout JW, Schumacher TN, Roep BO. Simultaneous detection of circulating autoreactive CD8+ T-cells specific for different islet cell-associated epitopes using combinatorial MHC multimers. Diabetes. 2010;59:1721–1730. doi: 10.2337/db09-1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jarchum I, Baker JC, Yamada T, Takaki T, Marron MP, Serreze DV, DiLorenzo TP. In vivo cytotoxicity of insulin-specific CD8+ T cells in HLA-A*0201-transgenic NOD mice. Diabetes. 2007;56:2551–2560. doi: 10.2337/db07-0332. [DOI] [PubMed] [Google Scholar]
- 29.Lieberman SM, Takaki T, Han B, Santamaria P, Serreze DV, DiLorenzo TP. Individual nonobese diabetic mice exhibit unique patterns of CD8+ T cell reactivity to three islet antigens, including the newly identified widely expressed dystrophia myotonica kinase. J. Immunol. 2004;173:6727–6734. doi: 10.4049/jimmunol.173.11.6727. [DOI] [PubMed] [Google Scholar]
- 30.Takaki T, Marron MP, Mathews CE, Guttmann ST, Bottino R, Trucco M, DiLorenzo TP, Serreze DV. HLA-A*0201-restricted T cells from "humanized" NOD mice recognize autoantigens of potential clinical relevance to type 1 diabetes. J. Immunol. 2006;176:3257–3265. doi: 10.4049/jimmunol.176.5.3257. [DOI] [PubMed] [Google Scholar]
- 31.Ellis JM, Henson V, Slack R, Ng J, Hartzman RJ, Katovich Hurley C. Frequencies of HLA-A2 alleles in five U.S. population groups. Predominance of A*02011 and identification of HLA-A*0231. Hum. Immunol. 2000;61:334–340. doi: 10.1016/s0198-8859(99)00155-x. [DOI] [PubMed] [Google Scholar]
- 32.Antal Z, Jarchum I, DiLorenzo TP. HLA class I supertypes in type 1 diabetic children in an urban children's hospital. Ann. N. Y. Acad. Sci. 2008;1150:86–89. doi: 10.1196/annals.1447.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jarchum I, DiLorenzo TP. Ins2 deficiency augments spontaneous HLA-A*0201-restricted T cell responses to insulin. J. Immunol. 2010;185:658–665. doi: 10.4049/jimmunol.0903414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Enee E, Martinuzzi E, Blancou P, Bach JM, Mallone R, van Endert P. Equivalent specificity of peripheral blood and islet-infiltrating CD8+ T lymphocytes in spontaneously diabetic HLA-A2 transgenic NOD mice. J. Immunol. 2008;180:5430–5438. doi: 10.4049/jimmunol.180.8.5430. [DOI] [PubMed] [Google Scholar]
- 35.Jarchum I, Nichol L, Trucco M, Santamaria P, DiLorenzo TP. Identification of novel IGRP epitopes targeted in type 1 diabetes patients. Clin. Immunol. 2008;127:359–365. doi: 10.1016/j.clim.2008.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ouyang Q, Standifer NE, Qin H, Gottlieb P, Verchere CB, Nepom GT, Tan R, Panagiotopoulos C. Recognition of HLA class I-restricted β-cell epitopes in type 1 diabetes. Diabetes. 2006;55:3068–3074. doi: 10.2337/db06-0065. [DOI] [PubMed] [Google Scholar]
- 37.Pinkse GG, Tysma OH, Bergen CA, Kester MG, Ossendorp F, van Veelen PA, Keymeulen B, Pipeleers D, Drijfhout JW, Roep BO. Autoreactive CD8 T cells associated with β cell destruction in type 1 diabetes. Proc. Natl. Acad. Sci. U. S. A. 2005;102:18425–18430. doi: 10.1073/pnas.0508621102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Toma A, Haddouk S, Briand JP, Camoin L, Gahery H, Connan F, Dubois-Laforgue D, Caillat-Zucman S, Guillet JG, Carel JC, Muller S, Choppin J, Boitard C. Recognition of a subregion of human proinsulin by class I-restricted T cells in type 1 diabetic patients. Proc. Natl. Acad. Sci. U. S. A. 2005;102:10581–10586. doi: 10.1073/pnas.0504230102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sette A, Sidney J. Nine major HLA class I supertypes account for the vast preponderance of HLA-A and -B polymorphism. Immunogenetics. 1999;50:201–212. doi: 10.1007/s002510050594. [DOI] [PubMed] [Google Scholar]
- 40.Sidney J, Grey HM, Southwood S, Celis E, Wentworth PA, del Guercio MF, Kubo RT, Chesnut RW, Sette A. Definition of an HLA-A3-like supermotif demonstrates the overlapping peptide-binding repertoires of common HLA molecules. Hum. Immunol. 1996;45:79–93. doi: 10.1016/0198-8859(95)00173-5. [DOI] [PubMed] [Google Scholar]
- 41.Sidney J, Peters B, Frahm N, Brander C, Sette A. HLA class I supertypes: a revised and updated classification. BMC Immunol. 2008;9:1. doi: 10.1186/1471-2172-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sidney J, del Guercio MF, Southwood S, Engelhard VH, Appella E, Rammensee HG, Falk K, Rotzschke O, Takiguchi M, Kubo RT, Grey HM, Sette A. Several HLA alleles share overlapping peptide specificities. J. Immunol. 1995;154:247–259. [PubMed] [Google Scholar]
- 43.Alexander J, Oseroff C, Sidney J, Wentworth P, Keogh E, Hermanson G, Chisari FV, Kubo RT, Grey HM, Sette A. Derivation of HLA-A11/Kb transgenic mice: functional CTL repertoire and recognition of human A11-restricted CTL epitopes. J. Immunol. 1997;159:4753–4761. [PubMed] [Google Scholar]
- 44.Chamberlain JW, Nolan JA, Gromkowski SH, Kelley KA, Eisenstadt JM, Herrup K, Janeway CA, Jr, Weissman SM. Cell surface expression and alloantigenic function of a human class I MHC heavy chain gene (HLA-B7) in transgenic mice. J. Immunol. 1988;140:1285–1292. [PubMed] [Google Scholar]
- 45.Hamilton-Williams EE, Serreze DV, Charlton B, Johnson EA, Marron MP, Mullbacher A, Slattery RM. Transgenic rescue implicates β2-microglobulin as a diabetes susceptibility gene in nonobese diabetic (NOD) mice. Proc. Natl. Acad. Sci. U. S. A. 2001;98:11533–11538. doi: 10.1073/pnas.191383798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.LaFace DM, Vestberg M, Yang Y, Srivastava R, DiSanto J, Flomenberg N, Brown S, Sherman LA, Peterson PA. Human CD8 transgene regulation of HLA recognition by murine T cells. J. Exp. Med. 1995;182:1315–1325. doi: 10.1084/jem.182.5.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brode S, Raine T, Zaccone P, Cooke A. Cyclophosphamide-induced type-1 diabetes in the NOD mouse is associated with a reduction of CD4+CD25+Foxp3+ regulatory T cells. J. Immunol. 2006;177:6603–6612. doi: 10.4049/jimmunol.177.10.6603. [DOI] [PubMed] [Google Scholar]
- 48.Harada M, Makino S. Promotion of spontaneous diabetes in non-obese diabetes-prone mice by cyclophosphamide. Diabetologia. 1984;27:604–606. doi: 10.1007/BF00276978. [DOI] [PubMed] [Google Scholar]
- 49.Jarchum I, Takaki T, DiLorenzo TP. Efficient culture of CD8+ T cells from the islets of NOD mice and their use for the study of autoreactive specificities. J. Immunol. Methods. 2008;339:66–73. doi: 10.1016/j.jim.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Altman JD, Moss PA, Goulder PJ, Barouch DH, McHeyzer-Williams MG, Bell JI, McMichael AJ, Davis MM. Phenotypic analysis of antigen-specific T lymphocytes. Science. 1996;274:94–96. [PubMed] [Google Scholar]
- 51.Sidney J, Southwood S, Oseroff C, del Guercio MF, Sette A, Grey HM. Measurement of MHC/peptide interactions by gel filtration. In: Coligan JE, Kruisbeek AM, Margulies DH, Shevach EM, Strober W, editors. Current Protocols in Immunology. Hoboken: John Wiley & Sons, Inc.; 2001. pp. 18.13.11–18.13.19. [Google Scholar]
- 52.Sidney J, Assarsson E, Moore C, Ngo S, Pinilla C, Sette A, Peters B. Quantitative peptide binding motifs for 19 human and mouse MHC class I molecules derived using positional scanning combinatorial peptide libraries. Immunome Res. 2008;4:2. doi: 10.1186/1745-7580-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cheng Y, Prusoff WH. Relationship between the inhibition constant (K1) and the concentration of inhibitor which causes 50 per cent inhibition (I50) of an enzymatic reaction. Biochem. Pharmacol. 1973;22:3099–3108. doi: 10.1016/0006-2952(73)90196-2. [DOI] [PubMed] [Google Scholar]
- 54.Gulukota K, Sidney J, Sette A, DeLisi C. Two complementary methods for predicting peptides binding major histocompatibility complex molecules. J. Mol. Biol. 1997;267:1258–1267. doi: 10.1006/jmbi.1997.0937. [DOI] [PubMed] [Google Scholar]
- 55.Chamberlain JW, Nolan JA, Conrad PJ, Vasavada HA, Vasavada HH, Ploegh HL, Ganguly S, Janeway CA, Jr, Weissman SM. Tissue-specific and cell surface expression of human major histocompatibility complex class I heavy (HLA-B7) and light (β2-microglobulin) chain genes in transgenic mice. Proc. Natl. Acad. Sci. U. S. A. 1988;85:7690–7694. doi: 10.1073/pnas.85.20.7690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lieberman SM, Evans AM, Han B, Takaki T, Vinnitskaya Y, Caldwell JA, Serreze DV, Shabanowitz J, Hunt DF, Nathenson SG, Santamaria P, DiLorenzo TP. Identification of the β cell antigen targeted by a prevalent population of pathogenic CD8+ T cells in autoimmune diabetes. Proc. Natl. Acad. Sci. U. S. A. 2003;100:8384–8388. doi: 10.1073/pnas.0932778100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kubo RT, Sette A, Grey HM, Appella E, Sakaguchi K, Zhu NZ, Arnott D, Sherman N, Shabanowitz J, Michel H, et al. Definition of specific peptide motifs for four major HLA-A alleles. J. Immunol. 1994;152:3913–3924. [PubMed] [Google Scholar]
- 58.Rammensee H-G, Bachmann J, Stevanovic S. MHC Ligands and Peptide Motifs. Austin: Landes Bioscience; 1997. [Google Scholar]
- 59.Irwin MJ, Heath WR, Sherman LA. Species-restricted interactions between CD8 and the α3 domain of class I influence the magnitude of the xenogeneic response. J. Exp. Med. 1989;170:1091–1101. doi: 10.1084/jem.170.4.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tishon A, LaFace DM, Lewicki H, van Binnendijk RS, Osterhaus A, Oldstone MB. Transgenic mice expressing human HLA and CD8 molecules generate HLA-restricted measles virus cytotoxic T lymphocytes of the same specificity as humans with natural measles virus infection. Virology. 2000;275:286–293. doi: 10.1006/viro.2000.0517. [DOI] [PubMed] [Google Scholar]
- 61.Cao K, Hollenbach J, Shi X, Shi W, Chopek M, Fernandez-Vina MA. Analysis of the frequencies of HLA-A, B, and C alleles and haplotypes in the five major ethnic groups of the United States reveals high levels of diversity in these loci and contrasting distribution patterns in these populations. Hum. Immunol. 2001;62:1009–1030. doi: 10.1016/s0198-8859(01)00298-1. [DOI] [PubMed] [Google Scholar]
- 62.Ferrier P, Fontecilla-Camps JC, Bucchini D, Caillol DH, Jordan BR, Lemonnier FA. Altered structure of HLA class I heavy chains associated with mouse beta-2 microglobulin. Immunogenetics. 1985;21:321–331. doi: 10.1007/BF00430798. [DOI] [PubMed] [Google Scholar]
- 63.Marron MP, Graser RT, Chapman HD, Serreze DV. Functional evidence for the mediation of diabetogenic T cell responses by HLA-A2.1 MHC class I molecules through transgenic expression in NOD mice. Proc. Natl. Acad. Sci. U. S. A. 2002;99:13753–13758. doi: 10.1073/pnas.212221199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kessler JH, Khan S, Seifert U, Le Gall S, Chow KM, Paschen A, Bres-Vloemans SA, de Ru A, van Montfoort N, Franken KL, Benckhuijsen WE, Brooks JM, van Hall T, Ray K, Mulder A, Doxiadis, van Swieten PF, II, Overkleeft HS, Prat A, Tomkinson B, Neefjes J, Kloetzel PM, Rodgers DW, Hersh LB, Drijfhout JW, van Veelen PA, Ossendorp F, Melief CJ. Antigen processing by nardilysin and thimet oligopeptidase generates cytotoxic T cell epitopes. Nat. Immunol. 2011;12:45–53. doi: 10.1038/ni.1974. [DOI] [PubMed] [Google Scholar]
- 65.Shameli A, Yamanouchi J, Thiessen S, Santamaria P. Endoplasmic reticulum stress caused by overexpression of islet-specific glucose-6-phosphatase catalytic subunit-related protein in pancreatic beta cells. Rev. Diabet. Stud. 2007;4:25–32. doi: 10.1900/RDS.2007.4.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fourlanos S, Perry C, Gellert SA, Martinuzzi E, Mallone R, Butler J, Colman PG, Harrison LC. Evidence that nasal insulin induces immune tolerance to insulin in adults with autoimmune diabetes. Diabetes. 2011;60:1237–1245. doi: 10.2337/db10-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]