Abstract
Objectives
This study assessed the impact of cardiac risk assessment using gated single-photon emission computed tomography (SPECT) on cardiac events in end-stage renal disease (ESRD) patients.
Methods
We evaluated 215 asymptomatic patients who began dialysis between January 2005 and April 2009. Baseline electrocardiography and echocardiography were performed in all the patients. The subjects were stratified into low- and high-risk groups according to the baseline cardiac status, and gated SPECT was additionally recommended for the high-risk patients.
Results
The study population consisted of 50 low- and 165 high-risk patients undergoing SPECT. Among the high-risk patients, 75 (45.5%) showed perfusion defects on SPECT and their overall cardiac-event rate per person-year of follow-up was 15.0%, significantly higher than 4.5% in high-risk group without perfusion defect and 1.2% in low-risk group. The presence of perfusion defect was a significant independent predictor of adverse cardiac events [hazard ratio (HR) 2.11; 95% confidence interval (CI) 1.05-4.24; P = .035]. When gated SPECT was added to the clinical and the echocardiographic variables, the prognostic stratification significantly improved (P < .001). However, coronary revascularization was not associated with improved cardiac event-free survival (HR 0.62; 95% CI 0.26-1.52; P = .296).
Conclusions
Gated SPECT may provide additional prognostic information for cardiac risk stratification, particularly among high-risk patients starting dialysis.
Electronic supplementary material
The online version of this article (doi:10.1007/s12350-011-9497-2) contains supplementary material, which is available to authorized users.
Keywords: Cardiac outcome, end-stage renal disease, risk stratification, single-photon emission computed tomography (SPECT)
Introduction
Cardiovascular disease is the leading cause of death in patients with end-stage renal disease (ESRD),1 and nearly 20% of these mortalities can be attributed to coronary artery disease (CAD).2,3 As a large number of ESRD patients are asymptomatic despite having significant CAD, cardiac risk assessment in these patients is an important issue. However, no accurate screening strategy is available for these asymptomatic patients, although symptomatic high-risk patients are generally screened for CAD. The National Kidney Foundation advises routine CAD screening only in high-risk renal transplant candidates, such as patients with diabetes, patients with a prior history of ischemic heart disease or an abnormal electrocardiogram, or patients over 50 years of age.4 There is insufficient evidence to support the benefit of routine screening and treatment in asymptomatic dialysis patients, regardless of their cardiac risk status. In addition, the traditional clinical risk assessment model using Framingham risk scores5 has limited value in dialysis patients, as it does not include renal function as a significant predictor for cardiovascular mortality.6 Therefore, global consensus on a screening strategy and an effective risk stratification method are needed in asymptomatic hemodialysis patients.
Although coronary angiography (CAG) remains the gold standard for the detection of occult CAD, it is difficult to use CAG in asymptomatic individuals owing to the risks associated with exposure to nephrotoxic contrast agents or procedure-related complications. In contrast, single-photon emission computed tomography (SPECT) is a non-invasive pharmacological stress test suitable for patients who are unable to exercise or patients who display abnormal baseline electrocardiography (ECG) such as chronic kidney disease (CKD) and dialysis patients.
Since 2005, we have conducted an independent CAD screening program to detect occult CAD in asymptomatic ESRD patients at the start of dialysis. Our previous data showed that the prevalence of CAD was 27.4% in asymptomatic ESRD patients and that the diagnostic accuracy of SPECT was acceptable.7 Screening for the presence of significant CAD may lead to the identification of patients whose prognosis could be improved with medical therapy and/or coronary revascularization. The purpose of this study was to evaluate the prognostic value of the stress/rest gated SPECT imaging analysis for baseline cardiac risk stratification, and to investigate the benefit of coronary revascularization in asymptomatic high-risk ESRD patients with significant coronary stenosis.
Methods
Patients and Study design
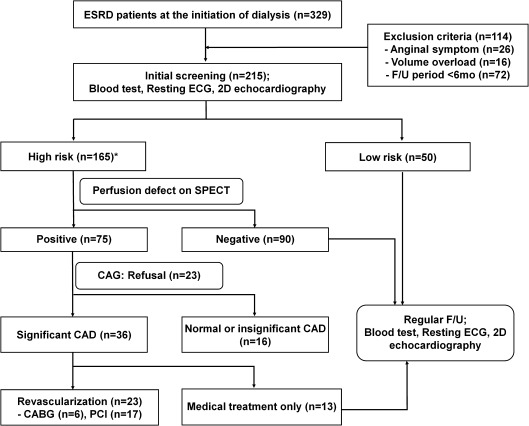
We evaluated asymptomatic ESRD patients who began dialysis between January 2005 and April 2009 at the Hallym University Sacred Heart Hospital in Korea. This study was designed such that baseline resting ECG and two-dimensional (2D) echocardiography tests were performed in all the patients, as recommended by the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines.4 Subjects with typical anginal pain or anginal equivalents (n = 26) were not invited to participate. Patients presenting with significant volume overload (n = 16) and those with a total follow-up duration of <6 months (n = 72) were also excluded (Figure 1). This study was approved by the institutional ethics committee and was conducted according to the Declaration of Helsinki.
Figure 1.
Study flow diagram. From January 2005 to April 2009, 329 ESRD patients started dialysis and 215 included in our study. *High-risk group was defined as patients >50 years of age, diabetes >10 years, a prior history of CAD or an abnormal electrocardiogram (excluding LV hypertrophy and electrolyte imbalance), decreased LV ejection fraction (LVEF) <40% or regional wall motion abnormality (RWMA) on echocardiography, and having 2 or more traditional CAD risk factors. ESRD, end-stage renal disease; F/U, follow-up; ECG, electrocardiography; CAG, coronary angiography; CAD, coronary artery disease; CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention
Based on the results of initial screening tests, the patients were classified into low- and high-risk groups. Patients in the high-risk group were >50 years of age; had diabetes for more than 10 years; had a prior history of CAD or an abnormal electrocardiogram [excluding left ventricular (LV) hypertrophy and electrolyte imbalance], a decreased LV ejection fraction (LVEF) of <40%, or a regional wall motion abnormality (RWMA) on echocardiography; and had two or more traditional CAD risk factors such as hypertension, dyslipidemia, smoking, LV hypertrophy, or family history of premature CAD.5 A stress/rest gated SPECT analysis was performed on the high-risk patients, and after consultation with a cardiologist, CAG was further recommended for those displaying a positive stress test on SPECT.
Diagnostic Work-up
When a patient was considered euvolemic, comprehensive echocardiographic measurements were performed following several sessions of dialysis. LVEF, LV RWMA, and LV geometric pattern data were collected using 2D echocardiography in M-mode with color Doppler. The LVEFs were calculated from the apical four- and two-chamber views using Simpson’s methods. Based on the LV mass index (LVMI) (normal values >115 g/m2 in men, >95 g/m2 in women) and relative wall thickness (RWT) (normal 0.42), echocardiographic LV hypertrophy (LVH) was categorized into four LV geometry groups: concentric hypertrophy (increased LVMI and increased RWT), eccentric hypertrophy (increased LVMI and normal RWT), concentric remodeling (normal LVMI and increased RWT), and normal geometry (normal LVMI and normal RWT).
Gated SPECT analyses were acquired using 99mTc-tetrofosmin (Myoview; Siemens Medical Systems, Inc., USA) and a pharmacological vasodilator (adenosine, 0.14 mg · kg−1 · min−1) with a 1-day protocol. For stress and rest images, 30 and 10 mCi of 99mTc-tetrofosmin were administered, respectively. Quantitative analyses of SPECT data were performed with the SPECT software packages Quantitative Gated SPECT (QGS) and 4DM-SPECT (4DM) by a standard processing method. A reversible perfusion defect was defined as a perfusion defect on stress images that partially or completely resolved on rest images in two or more contiguous segments. A fixed perfusion defect was defined as a perfusion defect on stress images in two or more contiguous segments that persisted on rest images. The summed stress score (SSS) and summed rest score (SRS) were obtained using 17-segment defect scores graded on a 5-point scale, and the summed difference score (SDS) was calculated as the difference between the SSS and SRS. The severity of myocardial perfusion defects was graded as normal (SSS <4), mild (SSS 4-8), moderate (SSS 9-13), and severe (SSS ≥14). An abnormal perfusion scan was taken to indicate the presence of a perfusion defect or elevated SSS ≥4. One experienced nuclear cardiologist in our institution, who was unaware of the clinical data, reviewed the SPECT images. Patient gender was revealed only on request.
CAD was considered to be present when any of the major coronary arteries showed luminal diameter narrowing of ≥50% (visual assessment). A reduction of <50% in luminal diameter was regarded as insignificant CAD. CAG images were analyzed by two different readers who were blinded to the clinical information, SPECT analysis results, and clinical outcomes.
Follow-Up and Endpoints
Patients were followed by periodic examinations in an outpatient setting. For patients not followed at our center, information was obtained during telephone interviews. For patients who were not reached by telephone, the Korean Society of Nephrology Demographic Registry was queried. The end of follow-up was determined by a cardiac event, or by the last patient contact in the hospital for those without events. Cardiac events were defined as cardiac death, non-fatal acute coronary syndrome (ACS), and acute decompensated heart failure requiring hospitalization. Cardiac death was defined as death with documentation of a significant arrhythmia, cardiac arrest, or both, or death attributable to congestive heart failure or myocardial infarction in the absence of any other precipitating factors. A sudden unexpected death outside of the hospital and without an autopsy was attributed to a cardiac cause. ACS (unstable angina, acute myocardial infarction) was defined using the standard criteria of history, ECG, and cardiac enzyme levels. In cases of multiple cardiac events, only the first event was used as the end point of follow-up. Elective revascularization procedures during follow-up were not considered to be cardiac events because the decision for coronary angioplasty might have been subjective.
Statistical Analyses
Continuous variables with normal distributions are expressed as means ± SD. The low- and high-risk groups were compared using the independent t test and chi-squared test. Survival curves were derived by the Kaplan-Meier method, and the differences between survival curves were compared using the log-rank test. The multivariate Cox proportional hazard model was used to evaluate independent predictors for adverse cardiac outcomes. A sequential Cox model analysis was performed to assess the incremental prognostic value of abnormal SPECT results over baseline, clinical variables, and echocardiographic findings. The incremental prognostic value was defined by a significant increase in the global chi-square, using the following variables in the global chi-squared test: age, gender, diabetes, smoking, prior history of CAD (baseline model), EF, LVH (baseline plus 2D echocardiography model), perfusion defect, SSS, and SDS (baseline plus 2D echocardiography plus SPECT model). The angiographic extent of CAD was not included because only a subgroup of patients (n = 52) underwent CAG. With the probability data generated by logistic regression analysis, the methods of Hanley and McNeil were used to generate the areas under the receiver operating characteristics (ROC) curves for the baseline clinical model, the baseline plus 2D echocardiography model, and the baseline plus 2D echocardiography plus SPECT model. The pre- and post-test odds for cardiac events were calculated using the following formula: post-test odds = pre-test odds × likelihood ratio, where odds = probability/(1 − probability), and likelihood ratio = sensitivity/(1 − sensitivity). All data were analyzed using SPSS 18.0 software. Statistical significance was defined as P < .05.
Results
Baseline Characteristics
The study population consisted of 215 ESRD patients with a mean (±SD) age of 57.1 (±14.3) years (range 21-88 years). Among these, 75 were high-risk patients with perfusion defects on SPECT, 90 were high-risk patients without perfusion defects, and 50 were low-risk patients (Figure 1). Of the 75 high-risk patients with perfusion defects, 52 (69.3%) underwent CAG, and 36 of these showed significant CAD with the presence of one-vessel, two-vessel, three-vessel, and left main CAD in 11 (30.6%), 14 (38.9%), 9 (25.0%), and 2 (5.6%) patients, respectively. For the 23 (30.7%) high-risk patients with perfusion defects patients who did not undergo CAG, 10 cases were according to the physician’s decision, and 13 cases were due to the patient’s refusal (poor socioeconomic status, n = 6; deprived of family support, n = 7).
The demographic characteristics and risk factors for CAD are summarized in Table 1. Patients in the high-risk group were significantly older and had higher prevalence of smoking, diabetes, and hypertension (P < .001) compared with the low-risk patients. A significantly elevated serum C-reactive protein level was also observed in the high-risk group (P = .012). In contrast, except for a history of ischemic heart disease (IHD), the demographic and risk factor characteristics were similar between the high-risk patients with and without perfusion defects. The baseline electrocardiographic and echocardiographic characteristics of both the groups are shown in Table 2. Compared with subjects in the low-risk group, the high-risk patients had significantly higher rates of LVH, RWMA, and increased pulmonary pressure, whereas LV systolic function was lower in the high-risk patients (LVEF 53.7% ± 10.9% vs 58.8% ± 8.4%, low vs high risk; P = .002). Among the high-risk patients, those with perfusion defects showed significantly lower LVEF, a higher rate of RWMA, and increased SSS, SRS, and SDS compared with those without perfusion defects.
Table 1.
Baseline characteristics of patients (n = 215)
| Total | Low risk | High risk | ||
|---|---|---|---|---|
| Perfusion defect (−) | Perfusion defect (+) | |||
| Patients, number | 215 | 50 | 90 (54.5%) | 75 (45.5%) |
| Age (years)* | 57.1 ± 14.3 | 44.1 ± 11.6 | 59.7 ± 13.1 | 62.6 ± 12.1 |
| Gender, male, n (%) | 113 (52.6) | 22 (44.0) | 54 (60.0) | 37 (49.3) |
| Smoking, n (%)* | 93 (43.2) | 10 (20.0) | 48 (53.3) | 35 (46.7) |
| BMI (kg/m2) | 23.1 ± 3.6 | 22.5 ± 3.4 | 23.5 ± 3.5 | 23.2 ± 3.8 |
| Diabetes, n (%)* | 123 (57.2) | 10 (20.0) | 58 (64.4) | 55 (73.3) |
| Hypertension, n (%)* | 124 (57.7) | 18 (36.0) | 59 (65.6) | 47 (62.7) |
| MAP (mm Hg) | 97.5 ± 13.4 | 96.5 ± 11.1 | 99.1 ± 15.2 | 96.5 ± 11.1 |
| Type of dialysis | ||||
| Hemodialysis | 151 (70.2) | 31 (62.0) | 70 (77.8) | 50 (66.7) |
| Peritoneal dialysis | 64 (29.8) | 19 (38.0) | 20 (22.2) | 23 (33.3) |
| Cause of ESRD* | ||||
| Diabetic | 122 (56.7) | 15 (30.0) | 57 (63.3) | 50 (66.7) |
| Hypertensive | 38 (17.7) | 9 (18.0) | 17 (18.9) | 12 (16.0) |
| Glomerulonephritis | 26 (12.1) | 17 (34.0) | 6 (6.7) | 3 (4.0) |
| Others | 29 (13.5) | 9 (14.0) | 10 (11.0) | 10 (13.3) |
| Previous heart disease*,† | ||||
| IHD with angioplasty | 14 (6.5) | 0 (0.0) | 5 (5.5) | 9 (12.0) |
| IHD with bypass surgery | 3 (1.4) | 0 (0.0) | 0 (0.0) | 3 (4.0) |
| IHD with medical therapy | 9 (4.3) | 0 (0.0) | 3 (3.4) | 6 (7.9) |
| Congestive heart failure | 6 (2.8) | 1 (2.0) | 2 (2.2) | 3 (4.0) |
| CRP (mg/L)* | 5.1 (1.0–37.10) | 3.2 (1.0–27.7) | 5.6 (1.0–26.10) | 6.1 (1.0–37.10) |
| Medications, n (%) | ||||
| Aspirin* | 119 (55.3) | 10 (20.0) | 51 (56.7) | 58 (77.3) |
| ACEi/ARBs* | 165 (76.7) | 31 (62.0) | 72 (80.0) | 62 (82.7) |
| β-Blockers | 103 (47.9) | 25 (50.0) | 38 (42.2) | 40 (53.3) |
| Statins* | 87 (40.5) | 16 (32.0) | 36 (40.0) | 35 (46.7) |
BMI, Body mass index; MAP, mean arterial pressure; ESRD, end-stage renal disease; IHD, ischemic heart disease; CRP, C-reactive protein; ACEi, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker.
* P < .05 between the high- and the low-risk groups.
† P < .05 between patients without and with perfusion defect among the high-risk patients.
Table 2.
Assessment of baseline cardiac status and clinical outcomes
| Total (n = 215) | Low risk (n = 50) | High risk | ||
|---|---|---|---|---|
| Perfusion defect (−) (n = 90) | Perfusion defect (+) (n = 75) | |||
| Electrocardiography, n (%) | ||||
| LVH* | 140 (65.1) | 22 (44.0) | 64 (71.1) | 54 (72.0) |
| Pathologic Q wave*,† | 29 (13.5) | 3 (6.0) | 10 (11.1) | 16 (21.3) |
| ST wave abnormality | 121 (56.3) | 25 (50.0) | 52 (57.8) | 44 (58.7) |
| Echocardiography | ||||
| LVEF*,† | 55.0 ± 10.6 | 58.8 ± 8.4 | 56.7 ± 9.6 | 50.1 ± 11.4 |
| RWMA, n (%)*,† | 37 (17.2) | 0 (0.0) | 14 (15.6) | 23 (30.6) |
| LV geometry* | ||||
| Normal | 72 (33.5) | 27 (34.0) | 25 (27.8) | 20 (26.7) |
| Concentric hypertrophy | 113 (52.6) | 17 (34.0) | 52 (57.8) | 44 (58.7) |
| Eccentric hypertrophy | 25 (11.6) | 6 (12.0) | 9 (10.0) | 10 (13.3) |
| Concentric remodeling | 5 (2.3) | 0 (0.0) | 4 (4.4) | 1 (1.3) |
| Pulmonary hypertension*,† | ||||
| None | 177 (82.3) | 46 (92.0) | 80 (88.9) | 51 (68.0) |
| Mild | 16 (7.4) | 2 (4.0) | 3 (3.3) | 11 (14.7) |
| Moderate to severe | 22 (10.2) | 2 (4.0) | 7 (7.8) | 13 (17.3) |
| SPECT | ||||
| EF at stress† | – | – | 55.9 ± 11.5 | 49.0 ± 9.7 |
| TID | – | – | 1.04 (0.68–1.35) | 1.08 (0.22–1.64) |
| SSS† | – | – | 0 (0–8) | 4 (0–33) |
| Normal (0–4), n (%) | 81 (90.0) | 47 (62.7) | ||
| Mild (4–8), n (%) | 6 (6.7) | 12 (16.0) | ||
| Moderate–severe (≥9), n (%) | 3 (3.3) | 16 (21.3) | ||
| SRS† | – | – | 0 (0–3) | 2 (0–21) |
| SDS† | – | – | 0 (0–4) | 2 (0–12) |
| Cardiac events*,†, n (%) | ||||
| Total | 53 (24.7) | 2 (4.0) | 15 (16.7) | 36 (48.0) |
| Nonfatal ACS | 30 (14.0) | 1 (2.0) | 7 (7.8) | 22 (29.3) |
| Cardiac death | 19 (8.8) | 1 (2.0) | 7 (7.8) | 11 (14.7) |
| ADHF | 4 (1.9) | 0 (0.0) | 1 (1.1) | 3 (4.0) |
LVH, Left ventricular hypertrophy; LVEF, left ventricular ejection fraction; RWMA, regional wall motion abnormality; SPECT, single-photon emission computed tomography; TID, transient ischemic dilatation; SSS, summed stress score; SRS, summed rest score; SDS, summed difference score; ACS, acute coronary syndrome; ADHF, acute decompensated heart failure.
* P < .05 between the high- and the low-risk groups.
† P < .05 between patients without and with perfusion defect among the high-risk patients.
Cardiac Events and Survival Analysis
During the follow-up period (mean 50.1 ± 20.9 months; median 47.1 months; range 15.0-87.3 months), 51 patients (30.9%) in the high-risk group experienced adverse cardiac events, whereas only 2 (4.0%) in the low-risk group experienced cardiac events, at 10.0 and 34.5 months, respectively. The overall rate of cardiac events per person-year of follow-up was 15.0% in the high-risk group with perfusion defects, 4.5% in the high-risk group without perfusion defects, and 1.2% in the low-risk group. More detailed cardiac event rates according to CAG in high-risk patients with perfusion defects are described in Supplemental Table 1.
As shown in Table 3, increasing age (P = .006), female gender (P = .016), diabetes (P = .005), RWMA (P = .003), LVEF (P < .001), and abnormal perfusion defect (P < .001) predicted cardiac events in the univariate analysis. In the multivariate Cox analysis, diabetes [hazard ratio (HR) 2.29; 95% confidence interval (CI) 1.02-5.17; P = .045], a reversible perfusion defect (HR 2.24; 95% CI 1.19-4.22; P = .012), and LVEF (HR 0.96; 95% CI 0.94-0.99; P = .013) were independent predictors. Replacing the reversible perfusion defect with any perfusion defect (reversible, fixed, and mixed) gave similar results (HR 2.11; 95% CI 1.05-4.24; P = .035). And a 1% increase of LVEF was associated with 4% reduction of cardiac event rate
Table 3.
Significant predictors for cardiac events
| Variables | Univariate analysis | Multivariate analysis* | Multivariate analysis** | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | |
| Age (per 1 year) | 1.03 (1.01–1.06) | .006 | 1.03 (0.99–1.05) | .065 | 1.02 (0.99–1.05) | .070 |
| Male (vs female) | 0.50 (0.30–0.88) | .016 | 0.64 (0.36–1.15) | .134 | 0.62 (0.35–1.12) | .115 |
| Diabetes (vs non–diabetes) | 3.14 (1.41–6.97) | .005 | 2.29 (1.02–5.17) | .045 | 2.31 (1.02–5.22) | .044 |
| Prior IHD | 2.43 (1.33–4.45) | .004 | – | – | – | – |
| hs-CRP (per 1 mg/L) | 1.05 (1.01–1.09) | .010 | – | – | – | – |
| RWMA (vs normal) | 2.32 (1.32–4.08) | .003 | – | – | – | – |
| LVH (vs normal) | 1.64 (0.85–3.16) | .140 | – | – | – | – |
| LVEF (per 1%) | 0.95 (0.93–0.98) | <.001 | 0.96 (0.94–0.99) | .013 | 0.97 (0.94–0.99) | .025 |
| Perfusion defect (vs normal) | 3.28 (1.79–6.00) | <.001 | 2.24 (1.19–4.22) | .012 | 2.11(1.05–4.24) | .035 |
| SSS ≥4 (vs <4) | 1.68 (0.92–3.10) | .081 | – | – | – | – |
HR, Hazard ratio; CI, confidence intervals; IHD, ischemic heart disease; hs-CRP, high-sensitivity C-reactive protein; RWMA, regional wall motion abnormality; LVH, left ventricular hypertrophy; LVEF, left ventricular ejection fraction; SSS, summed stress score.
* Adjusted with age, gender, diabetes, LV ejection fraction, and reversible perfusion defect.
** Adjusted with age, gender, diabetes, LV ejection fraction, and any type of perfusion defect (reversible, fixed, and mixed).
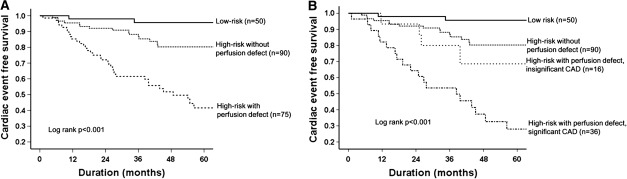
Figure 2A shows the Kaplan-Meier estimates for the occurrence of cardiac events in each group. The risk for adverse cardiac events was significantly higher in high-risk patients with perfusion defects than in high-risk patients without perfusion defects (HR 3.28; 95% CI 1.79-5.99; P < .001) and low-risk patients (HR 17.56; 95% CI 4.20-73.55; P < .001), emphasizing the importance of identifying a perfusion defect on SPECT analysis. As shown in Figure 2B, the presence of significant CAD was associated with increased risk for cardiac events in high-risk patients (HR 1.94; 95% CI 1.38-2.71; P < .001).
Figure 2.
Kaplan-Meier estimates for the occurrence of cardiac events in low (n = 50)- and high (n = 165)-risk patients. Among high-risk patients, the presence of perfusion defect was closely associated with adverse cardiac outcomes (HR 3.16; 95% CI 1.65-6.04, P = .001) (A) and the presence of CAD significantly increased the risk of cardiac events (HR 1.94 95% CI 1.38-2.71, P < .001) (B)
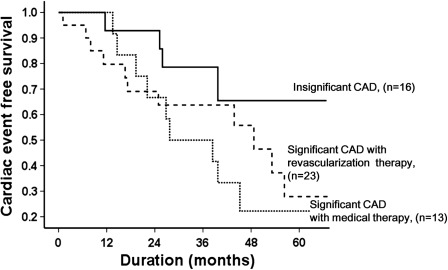
Among the 36 patients with significant CAD, 23 (63.9%) were treated with coronary revascularization therapy (6 by coronary artery bypass graft surgery, 17 by percutaneous coronary interventions), whereas 13 patients (36.1%) refused coronary revascularization therapy and were treated medically only. Of the 23 subjects with revascularization, 11 (47.8%) experienced adverse cardiac events within a mean duration of 38.2 ± 23.1 months, and there were 4 (17.4%) cardiac deaths. Of the 13 patients who refused coronary revascularization therapy, 9 (69.2%) developed adverse cardiac events within 31.7 ± 19.1 months, and 3 (23.1%) died. As presented in Figure 3, patients who had significant CAD had a significantly higher rate of cardiac events compared with patients having insignificant or normal CAD (55.6% vs 31.2%, P < .001). Although patients who received only medical treatment appeared to have a higher rate of cardiac events, revascularization therapy did not improve the cardiac event-free survival rate (HR 0.62; 95% CI 0.26-1.52; P = .296).
Figure 3.
Kaplan-Meier analysis of the cardiac event rate in high-risk patients with significant CAD. Revascularization therapy did not improve cardiac events-free survival (HR 0.62, 95% CI 0.26-1.52; P = .296)
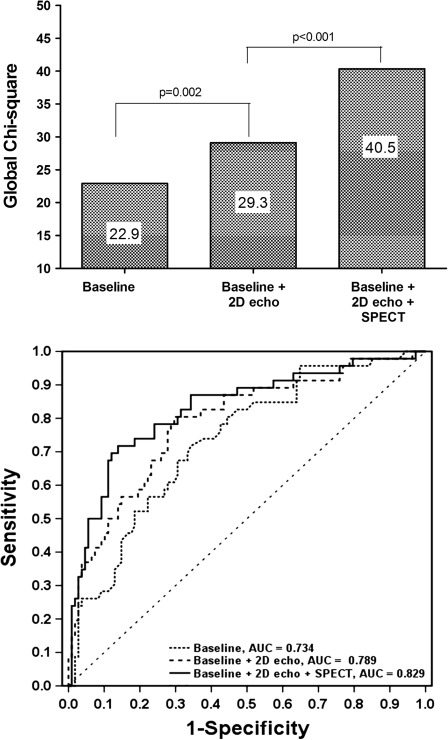
The Incremental Value of SPECT in High-Risk Group
Further analyses assessed the incremental value of the SPECT in the high-risk group. For prediction of cardiac events, three analyses were performed: (1) baseline (clinical data only), (2) baseline plus 2D echocardiography, and (3) baseline plus 2D echocardiography plus SPECT. Figure 4 shows the incremental prognostic values from the global chi-square (upper) and ROC (lower) analyses. Compared with the baseline model, the addition of 2D echocardiography data significantly improved the prediction of cardiac events (global chi-square = 29.3, P = .002), and the inclusion of SPECT data further improved the prognostic value, increasing the global chi-square value to 40.5 (P < .001). Similarly, the area under the ROC curve (AUC) of baseline plus 2D echocardiography plus SPECT data (AUC = 0.829) was significantly larger than that of baseline (AUC = 0.734, P = .001) or baseline plus 2D echocardiography (AUC = 0.789, P = .048). The addition of SPECT data provided the most accurate outcome prediction. The likelihood ratio of cardiac events for a positive 2D echocardiography and SPECT was 5.17; the post-test odds was 4.34 with the mean pre-test probability of CAD was 45.8%.
Figure 4.
Incremental prognostic value of SPECT over baseline (clinical only) and baseline plus 2D echocardiographic variables; upper global chi-square, lower ROC curve analysis
Discussion
In this study, we found that (1) more than 75% of ESRD patients could be classified in a high-risk group based on clinical and echocardiographic findings at the start of dialysis; (2) among the high-risk patients, 45.5% showed perfusion defects on gated SPECT, and it was a strong predictor of adverse cardiac mortality; and (3) coronary revascularization therapy in asymptomatic ESRD patients was not significantly associated with an improved cardiac event-free survival rate. Gated SPECT analysis may be a useful tool in selecting patients at high risk for adverse cardiac outcomes and in choosing a therapeutic option.
SPECT, with its high diagnostic and prognostic accuracy,8,9 is one of the most extensively validated and commonly employed methods in various subsets of populations, including patients with diabetes,10 patients after myocardial infarction and revascularization therapy,9,11,12 patients with CKD,13-15 patients with ESRD,16-18 and renal transplantation candidates.19-21 However, the role of SPECT is less defined in asymptomatic patients than in those with active symptoms. The 2003 ACC/AHA/ASNC guidelines for the clinical use of cardiac radionucleotide imaging suggested that SPECT may be helpful in some asymptomatic high-risk patients.22 According to the most recent 2009 guidelines, the use of SPECT is considered to be appropriate and necessary in asymptomatic patients at high-risk for CAD.23
Here, we determined the level of cardiac risk based on traditional CAD risk factors, including electrocardiographic and echocardiographic features, and based on the result of stress/rest gated SPECT, especially for high-risk patients. Consistent with previous data,10,13,15 our study found that patients with perfusion defects and increased SSS (≥4) had a 3.3- and 2.1-fold increase in relative risk for cardiac events compared with patients without perfusion defects, even in the same high-risk group. Considering that there were minimal differences in baseline clinical parameters between patients with and without perfusion defects, abnormal SPECT findings may have significant implications in cardiac risk stratification. Multivariate Cox analysis also demonstrated the importance of determining perfusion defects, as well as reversible perfusion defect, for the prediction of long-term cardiac risk. Furthermore, this study confirmed the benefit of SPECT over clinical and echocardiographic variables; adding the SPECT results to clinical and/or echocardiographic data provided significant incremental prognostic value for the prediction of adverse cardiac outcomes. These findings support the widely accepted idea that the diagnostic and prognostic accuracy of SPECT is greater than that of clinical or echocardiographic data, and even that of CAG in risk stratification of CAD. In 2009, Gimelli et al8 evaluated the efficacy of stress/rest gated SPECT and demonstrated that myocardial perfusion abnormalities identified by gated SPECT may be the best predictor of cardiac event-free survival, even when compared with an extensive diagnostic CAD work-up that included clinical, echocardiographic, and angiographic analyses.
On the other hand, compared with our results, a recently published study from the Netherlands reported seemingly contradictory results with renal transplant patients.24 Aalten et al reported that the incidence of significant cardiac ischemia was low (6.6%) and significant benefit could not be observed with a preoperative cardiac assessment program for adverse cardiac outcomes, especially early cardiac events (≤30 days of transplantation). However, there are important differences between these two studies. Aalten et al evaluated the benefit of a cardiac screening test in subjects limited to renal transplant candidates among a relatively young and healthy population. Their patient group had a younger mean age (50.8 vs 61.0 years), a lower percentage of diabetes (8.8% vs 68.5%), and a lower rate of cardiac disease history (11.2% vs 17.5%) compared with our patients. This may explain the relatively low rate of significant ischemia on a non-invasive stress test (3.6%) and low rate of perioperative cardiac events observed in their study. Furthermore, our study evaluated the long-term cardiac event rate (over 4 years), whereas their study evaluated short-term cardiac events (≤30 days of transplantation) and did not address long-term benefits. Similar results were also shown by Hage et al in 2007.25 With 3,698 kidney transplant candidate, they evaluated all-cause mortality during a mean follow-up of 2.5 years and reported that the presence and the severity of CAD was not predictor for survival, but LV ejection fraction was the best predictor for death. However, their patients were at relatively lower risk and had more favorable baseline characteristics, too. Thus, the incidence of abnormal findings on MPI was only 19%, and three-vessel CAD was found only in 2% of patients, while 52.7% and 25.0% of our patients showed abnormal MPI results and three-vessel CAD, respectively. Nevertheless, the significant role of LV ejection fraction for predicting mortality was in good accordance with our data.
Our study did not demonstrate a reduced risk for cardiac events in asymptomatic patients with significant CAD after coronary revascularization, compared with those who received optimal medical therapy alone (HR 0.62; 95% CI 0.26-1.52; P = .296). However, this finding should be interpreted with caution because the analysis of this subpopulation was limited by a small sample size. Nevertheless, the optimal CAD therapy in this population remains uncertain and the benefit of pre-emptive coronary revascularization therapy (percutaneous coronary intervention or coronary artery bypass graft) at the start of dialysis on the long-term outcome is unclear.26,27 Previously, clinicians were reluctant to perform early revascularization therapy in this population for fear of the complete loss of residual renal function as a result of contrast nephropathy or a higher rate of procedure-related complications.26 Moreover, according to the limited data available, ESRD is associated with a higher rate of stent restenosis following percutaneous coronary intervention.28 However, recent advances in surgery and percutaneous coronary intervention as well as additional adjunctive medical therapies have lowered the complication rate and stent restenosis rate in this population.27,29 Reddan et al30 reported that revascularization therapy using percutaneous coronary intervention or coronary artery bypass graft improved the survival of CKD patients. Moroi et al31 also evaluated the effects of revascularization in patients with stable IHD and showed a benefit for patients with moderate to severe ischemia. Nevertheless, the optimal timing for revascularization therapy has not yet been established. In some ways, coronary revascularization performed at the initiation of dialysis may already be too late to improve cardiac outcomes. However, considering the risk for contrast nephropathy in non-dialysis CKD patients,14 cardiac revascularization at the initiation of dialysis may be optimal. Additional long-term, well-designed, large-scale comparative trials are needed.
This study has several limitations. First, the predictive role of SPECT was evaluated in only a selected high-risk group of ESRD patients at baseline. SPECT imaging has been shown to be inappropriate for low-risk patients, as no proven clinical value of SPECT has been demonstrated in these patients.23 However, in our study, two patients in the low-risk group experienced cardiac events. The usefulness of gated SPECT in low-risk patients should be further evaluated in a larger cohort. Second, this study was a non-randomized and non-comparative study, and thus we could not demonstrate the benefit of our cardiac risk assessment protocol on cardiovascular mortality, compared with the routine screening test recommended by KDOQI guidelines. Third, a substantial portion of the patients (13/36, 36.1%) did not undergo CAG, despite reversible perfusion defects on SPECT. In practice, it was impossible to perform CAG in these patients because the patients or their families refused to provide the required signed consent. At last, about 10% of patients (n = 23) lost to follow-up during study period. Therefore, we could not predict future cardiac event rate more accurately.
In conclusion, baseline cardiac risk stratification based on gated SPECT analysis may be useful for the prediction of cardiac mortality in asymptomatic ESRD patients. It may also provide prognostic information, in addition to clinical and echocardiographic data, for cardiac risk stratification, particularly among high-risk patients starting dialysis. More detailed cardiac risk assessment methods using non-invasive imaging parameters such as coronary calcium scores, carotid intima-media thicknesses, or ankle brachial indexes are needed for further stratification of high-risk patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
None to declare.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Baig SZ, Coats WC, Aggarwal KB, Alpert MA. Assessing cardiovascular disease in the dialysis patient. Adv Perit Dial. 2009;25:147–154. [PubMed] [Google Scholar]
- 2.Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, et al. Chronic kidney disease and mortality risk: A systematic review. J Am Soc Nephrol. 2006;17:2034–2047. doi: 10.1681/ASN.2005101085. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 4.KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Chronic Kidney Disease. Am J Kidney Dis. 2007;49:S12–S154. doi: 10.1053/j.ajkd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Ruilope LM. The Framingham risk score is valuable in Europeans. Nat Rev Nephrol. 2010;6:14–15. doi: 10.1038/nrneph.2009.205. [DOI] [PubMed] [Google Scholar]
- 6.Weiner DE, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS, et al. The Framingham predictive instrument in chronic kidney disease. J Am Coll Cardiol. 2007;50:217–224. doi: 10.1016/j.jacc.2007.03.037. [DOI] [PubMed] [Google Scholar]
- 7.Song YR, Kim SG, Kim EJ, Kim SJ, Park TJ, Song YS, et al. The prevalence of coronary artery disease in patients with end stage renal disease at the initiation of dialysis and the accuracy of noninvasive tests. Korean J Nephrol. 2007;26:327–333. [Google Scholar]
- 8.Gimelli A, Rossi G, Landi P, Marzullo P, Iervasi G, L’Abbate A, et al. Stress/rest myocardial perfusion abnormalities by gated SPECT: Still the best predictor of cardiac events in stable ischemic heart disease. J Nucl Med. 2009;50:546–553. doi: 10.2967/jnumed.108.055954. [DOI] [PubMed] [Google Scholar]
- 9.Piccini JP, Horton JR, Shaw LK, Al-Khatib SM, Lee KL, Iskandrian AE, et al. Single-photon emission computed tomography myocardial perfusion defects are associated with an increased risk of all-cause death, cardiovascular death, and sudden cardiac death. Circ Cardiovasc Imaging. 2008;1:180–188. doi: 10.1161/CIRCIMAGING.108.776484. [DOI] [PubMed] [Google Scholar]
- 10.Kato M, Matsumoto N, Nakano Y, Suzuki Y, Yoda S, Sato Y, et al. Combined assessment of myocardial perfusion and function by ECG-gated myocardial perfusion single-photon emission computed tomography for the prediction of future cardiac events in patients with type 2 diabetes mellitus. Circ J. 2011;75:376–382. doi: 10.1253/circj.CJ-10-0794. [DOI] [PubMed] [Google Scholar]
- 11.Giri S, Shaw LJ, Murthy DR, Travin MI, Miller DD, Hachamovitch R, et al. Impact of diabetes on the risk stratification using stress single-photon emission computed tomography myocardial perfusion imaging in patients with symptoms suggestive of coronary artery disease. Circulation. 2002;105:32–40. doi: 10.1161/hc5001.100528. [DOI] [PubMed] [Google Scholar]
- 12.Zellweger MJ, Lewin HC, Lai S, Dubois EA, Friedman JD, Germano G, et al. When to stress patients after coronary artery bypass surgery? Risk stratification in patients early and late post-CABG using stress myocardial perfusion SPECT: Implications of appropriate clinical strategies. J Am Coll Cardiol. 2001;37:144–152. doi: 10.1016/S0735-1097(00)01104-9. [DOI] [PubMed] [Google Scholar]
- 13.Hatta T, Nishimura S, Nishimura T. Prognostic risk stratification of myocardial ischaemia evaluated by gated myocardial perfusion SPECT in patients with chronic kidney disease. Eur J Nucl Med Mol Imaging. 2009;36:1835–1841. doi: 10.1007/s00259-009-1165-2. [DOI] [PubMed] [Google Scholar]
- 14.Hakeem A, Bhatti S, Trevino AR, Samad Z, Chang SM. Non-invasive risk assessment in patients with chronic kidney disease. J Nucl Cardiol. 2011;18:472–485. doi: 10.1007/s12350-011-9359-y. [DOI] [PubMed] [Google Scholar]
- 15.Al-Mallah MH, Hachamovitch R, Dorbala S, Di Carli MF. Incremental prognostic value of myocardial perfusion imaging in patients referred to stress single-photon emission computed tomography with renal dysfunction. Circ Cardiovasc Imaging. 2009;2:429–436. doi: 10.1161/CIRCIMAGING.108.831164. [DOI] [PubMed] [Google Scholar]
- 16.Hase H, Joki N, Ishikawa H, Fukuda H, Imamura Y, Saijyo T, et al. Prognostic value of stress myocardial perfusion imaging using adenosine triphosphate at the beginning of haemodialysis treatment in patients with end-stage renal disease. Nephrol Dial Transplant. 2004;19:1161–1167. doi: 10.1093/ndt/gfh037. [DOI] [PubMed] [Google Scholar]
- 17.Momose M, Babazono T, Kondo C, Kobayashi H, Nakajima T, Kusakabe K. Prognostic significance of stress myocardial ECG-gated perfusion imaging in asymptomatic patients with diabetic chronic kidney disease on initiation of haemodialysis. Eur J Nucl Med Mol Imaging. 2009;36:1315–1321. doi: 10.1007/s00259-009-1110-4. [DOI] [PubMed] [Google Scholar]
- 18.Venkataraman R, Hage FG, Dorfman T, Heo J, Aqel RA, de Mattos AM, et al. Role of myocardial perfusion imaging in patients with end-stage renal disease undergoing coronary angiography. Am J Cardiol. 2008;102:1451–1456. doi: 10.1016/j.amjcard.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 19.Patel AD, Abo-Auda WS, Davis JM, Zoghbi GJ, Deierhoi MH, Heo J, et al. Prognostic value of myocardial perfusion imaging in predicting outcome after renal transplantation. Am J Cardiol. 2003;92:146–151. doi: 10.1016/S0002-9149(03)00529-0. [DOI] [PubMed] [Google Scholar]
- 20.De Lima JJ, Wolff Gowdak LH, de Paula FJ, Ianhez LE, Franchini Ramires JA, Krieger EM. Validation of a strategy to diagnose coronary artery disease and predict cardiac events in high-risk renal transplant candidates. Coron Artery Dis. 2010;21:164–167. doi: 10.1097/MCA.0b013e328332ee5e. [DOI] [PubMed] [Google Scholar]
- 21.Wang JH, Kasiske BL. Screening and management of pretransplant cardiovascular disease. Curr Opin Nephrol Hypertens. 2010;19:586–591. doi: 10.1097/MNH.0b013e32833e034e. [DOI] [PubMed] [Google Scholar]
- 22.Klocke FJ, Baird MG, Lorell BH, Bateman TM, Messer JV, Berman DS, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging—executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging) Circulation. 2003;108:1404–1418. doi: 10.1161/01.CIR.0000080946.42225.4D. [DOI] [PubMed] [Google Scholar]
- 23.Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol. 2009;53:2201–2229. doi: 10.1016/j.jacc.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 24.Aalten J, Peeters SA, van der Vlugt MJ, Hoitsma AJ. Is standardized cardiac assessment of asymptomatic high-risk renal transplant candidates beneficial? Nephrol Dial Transplant. 2011;26:3006–3012. doi: 10.1093/ndt/gfq822. [DOI] [PubMed] [Google Scholar]
- 25.Hage FG, Smalheiser S, Zoghbi GJ, Perry GJ, Deierhoi M, Warnock D, et al. Predictors of survival in patients with end-stage renal disease evaluated for kidney transplantation. Am J Cardiol. 2007;100:1020–1025. doi: 10.1016/j.amjcard.2007.04.045. [DOI] [PubMed] [Google Scholar]
- 26.Williams ME. Coronary revascularization in diabetic chronic kidney disease/end-stage renal disease: A nephrologist’s perspective. Clin J Am Soc Nephrol. 2006;1:209–220. doi: 10.2215/CJN.00510705. [DOI] [PubMed] [Google Scholar]
- 27.Singh M, Arora R, Kodumuri V, Khosla S, Jawad E. Coronary revascularization in diabetic patients: Current state of evidence. Exp Clin Cardiol. 2011;16:16–22. [PMC free article] [PubMed] [Google Scholar]
- 28.de Lemos JA, Hillis LD. Diagnosis and management of coronary artery disease in patients with end-stage renal disease on hemodialysis. J Am Soc Nephrol. 1996;7:2044–2054. doi: 10.1681/ASN.V7102044. [DOI] [PubMed] [Google Scholar]
- 29.Daemen J, Lemos P, Aoki J, Arampatzis C, Hoye A, McFadden E, et al. Treatment of coronary artery disease in dialysis patients with sirolimus-eluting stents: 1-year clinical follow-up of a consecutive series of cases. J Invasive Cardiol. 2004;16:685–687. [PubMed] [Google Scholar]
- 30.Reddan DN, Szczech LA, Tuttle RH, Shaw LK, Jones RH, Schwab SJ, et al. Chronic kidney disease, mortality, and treatment strategies among patients with clinically significant coronary artery disease. J Am Soc Nephrol. 2003;14:2373–2380. doi: 10.1097/01.ASN.0000083900.92829.F5. [DOI] [PubMed] [Google Scholar]
- 31.Moroi M, Yamashina A, Tsukamoto K, Nishimura T. Coronary revascularization does not decrease cardiac events in patients with stable ischemic heart disease but might do in those who showed moderate to severe ischemia. Int J Cardiol 2011. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.