Abstract
Surgical resections of large-to-giant pituitary adenomas (PA) are technically challenging procedures. Tumors with a fibrous consistency or ‘hour-glass’ configurations are particularly difficult to remove completely and safely through the transsphenoidal route alone. Although the transcranial approach can facilitate the removal of a large suprasellar mass, it may be associated with significant bleeding within the intradural space. A simultaneous microscopic transcranial and transsphenoidal approach has been described as an alternative surgical strategy. We have further modified this ‘above and below’ approach by adopting endoscopic techniques for the transsphenoidal part of the procedure. This modified approach has the advantages of requiring only one operating microscope, and permitting freer maneuvers and easier orientation for both surgical teams. We present two patients successfully treated with this approach. Complete tumor removal was achieved and both patients achieved satisfactory functional recovery.
Keywords: Pituitary adenoma, Endoscopy, Transsphenoidal, Craniotomy, Skull base, Surgical approach
Introduction
Surgical resections of large-to-giant pituitary adenomas (PAs) are technically challenging procedures. Tumors with a fibrous consistency or ‘hour-glass’ configurations are particularly difficult to remove completely and safely through the transsphenoidal route alone. Although the transcranial approach can facilitate the removal of a large suprasellar mass, it may be associated with significant bleeding within the intradural space [1]. Other approaches such as the staged transsphenoidal approach [2] and the staged transcranial-transsphenoidal approach [3] are potentially effective strategies but have the disadvantage of requiring multiple operations.
An alternative technique of simultaneous ‘above and below’ resection of large PAs has been described [3–5]. It combines a microscopic transsphenoidal approach with a craniotomy in a single setting. We have further modified this approach by adopting endonasal endoscopic techniques for the transsphenoidal part of the procedure. We present here two patients treated with this technique and discuss its applications and limitations.
Surgical procedure
The tumor was approached both transcranially and transsphenoidally by two surgical teams under a single setting of general anesthesia. The transsphenoidal surgeon stood on the right side of the patient while the transcranial surgeon was seated at the head end (Fig. 1) . The transcranial surgeon approached the tumor through a pterional craniotomy under the operating microscope. But unlike the combined approach previously described [3, 4] our transsphenoidal surgeon approached the sella using standard endonasal endoscopic techniques [6].
Fig. 1.
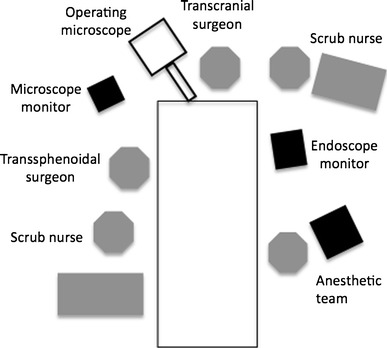
A schematic diagram illustrating the arrangement in the operating theatre
The tumor was first exposed on the cranial side but every effort was made to avoid breaching the tumor capsule to minimize bleeding within the intradural space. The cranial surgeon’s role was to dissect the tumor capsule from adjacent structures, to protect the latter against the transsphenoidal surgeon’s manipulations, and to deliver the tumor towards the sphenoidal sinus. The tumor capsule was first opened on the transsphenoidal side, followed by tumor debulking. The subsequent skull base defect was repaired with abdominal fat graft. Again, the cranial surgeon served to prevent against over-enthusiastic packing by the transsphenoidal surgeon. Wound closure was performed in the standard manner. A subgaleal suction drain was inserted on the cranial side, and the nasal passages were packed for 1 day. No lumbar drain was used.
Illustrative case 1
A 61-year-old man presented with 2 months’ history of blurring of vision. On examination, he had a left temporal hemianopia. His visual acuity was 0.3 (right) and 0.1 (left). Basal pituitary function evaluation revealed a serum prolactin (PRL) level of 154 mU/l (normal values 70–417 mU/l) and panhypopituitarism. There was no clinical evidence of diabetes insipidus (DI). Hydrocortisone and thyroxine replacement was commenced. Magnetic resonance imaging (MRI) revealed a 3.8 × 4.2 × 4.5 cm (transverse (TR) × anterior-posterior (AP) × longitudinal (L)) sellar mass with optic chiasmal compression and third ventricular extension. The findings were compatible with a Hardy Grade II Stage B lesion [7] (Fig. 2a, b). The patient underwent tumor removal with the procedure described above. Pathological examination confirmed a non-functioning PA. His visual acuity improved post-operatively to 0.4 (right) and 0.7 (left) after surgery. The visual field recovered except for a residual rim of peripheral loss. He developed permanent DI and required full pituitary hormone replacement therapy. Post-operative MRI performed 3 months afterwards showed no residual tumor (Fig. 2c, d)
Fig. 2.
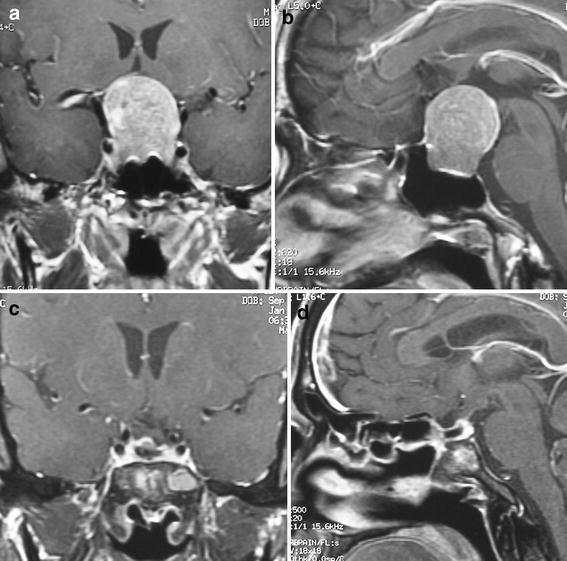
Contrasted T1-weighted magnetic resonance images of Patient Case 1. a Pre-operative coronal; b pre-operative sagittal; c post-operative coronal; d post-operative sagittal
Illustrative case 2
A 60-year-old man presented with 1 week’s history of blurring of vision and headache. On examination, he had significant bitemporal hemianopia. Laboratory investigations revealed hyponatremia of 118 mmol/l (normal values 136–148 mmol/l). The random spot serum cortisol was less than 22 nmol/l. The serum PRL level was 628 mU/l (normal values 70–417 mU/l). Other anterior pituitary hormones levels were subnormal. There was no clinical evidence of DI. MRI revealed a suprasellar tumor measuring 3.8 × 4.2 × 4.5 cm (TR × AP × L) with heterogeneous contrast enhancement, optic chiasm compression and third ventricular extension. The findings were compatible with a Hardy Grade III Stage B lesion [7] (Fig. 3a, b). The patient was commenced on hydrocortisone and thyroxine replacement, and underwent a gross total tumor removal 1 week later. The pathology was a non-functioning PA, with focal immuno-staining positivity with TSH and FSH/LH. The patient’s visual field recovered completely. He developed permanent DI. MRI performed 9 months later demonstrated complete removal of the tumor mass (Fig. 3c, d)
Fig. 3.
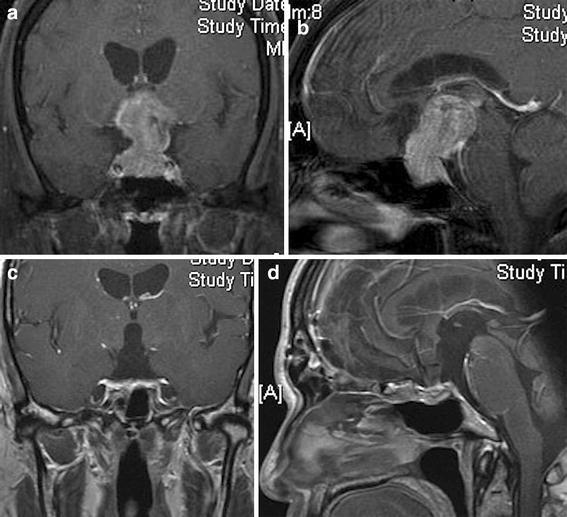
Contrasted T1-weighted magnetic resonance images of Patient Case 2. a Pre-operative coronal; b pre-operative sagittal; c post-operative coronal; d post-operative sagittal
Discussion
Surgery is the treatment of choice for non-functioning large-to-giant PAs. But complete tumor removal can be difficult to accomplish and the procedure may be associated with significant morbidities or even mortalities. Historically, the operative mortality rates were as high as 14% for transsphenoidal and 25% for transcranial resections [8]. More recent series have reported better outcomes [9–11]. In Mortini’s series of 111 patients with huge PA, the treatment mortality rate was 2.7% [10]. Sinha et al. similarly reported mortality and morbidity rates of 4.4 and 14%, respectively [9]. The introduction of endoscopic pituitary surgery has further revolutionized the treatment of these difficult lesions [12, 13]. The extended endoscopic transsphenoidal technique, in particular, has been shown to facilitate the safe removal of large tumors which previously were not amendable to complete resection through a single route alone [14, 15]. However, considerable experiences and technical expertise are needed before this technique can be used to its full advantages [6].
One of the difficulties encountered during transsphenoidal resection of giant PAs is that the suprasellar tumor portion may ‘refuse’ to descend into the sella. Several techniques have been described to address this problem, including the use of Valsalva’s maneuvers, intraspinal saline infusion, and staged removals [2]. A simultaneous ‘above and below’ technique has been described which combines a transsphenoidal approach with a craniotomy. With this approach, Alleyne et al. achieved a gross total resection rate of 40% in a cohort of 10 patients. More than half of the patients who had pre-operative visual field defects experienced complete improvement. Permanent DI occurred in 20% of patients [3]. In D’Ambrosio’s series, gross total resection was achieved in six out of 11 patients. Seven patients (64%) experienced visual improvement. Panhypopituitarism occurred in four and persistent DI in two patients [4]. The technique described by these two groups required one operating microscope for each of the transsphenoidal and transcranial teams. In our experience, this may create difficulties with positioning as the two microscopes tended to clash over the patient’s head. Furthermore, not all centres can have two microscopes readily available. The head rotation required for the pterional craniotomy may also disorientate the transsphenoidal surgeon who tried to approach the sella sublabially.
Our modified technique thus takes advantages of the ‘above and below’ approach as well as that of endoscopic surgery. It requires only one operating microscope. It also permits freer movement by both surgical teams since the endoscope and the microscope occupy different air-spaces above the patient’s body. The endonasal endoscopeic method provides excellent visualization and illumination of the operative field, and is associated with minimal soft tissue damage within the nose. The monitors of the microscope and the endoscope can be positioned to allow both teams to see each other’s operative fields. The transcranial surgeon serves to deliver the tumor bulk and to protect intradural structures. There is minimal tumor bleeding within the subarachnoid space. Safe and complete tumor removal can be achieved in selected cases.
The use of endoscopes for the simultaneous ‘above and below’ approach has been described previously [16–18]. These authorities combined the use of endonasal with transventricular endoscopes. The technique was particularly suitable for tumors with third ventricular extension and ventricular dilatation. Our modified approach, on the other hand, is applicable also for PAs which are not causing hydrocephalus but for which a combined approach is still potentially useful. Zada et al. recently reviewed 250 transsphenoidal operations and identified 13 complex sellar lesions which would have benefited more from transcranial attack instead. Based on these lesions, eight factors were found to limit the extent or safety of transsphenoidal resections. These included significant suprasellar extension, lateral extension, retrosellar extension, brain invasion with edema, firm tumor consistency, involvement or vasospasm of the arteries of the circle of Willis, and encasement of the optic apparatus or invasion of the optic foramina [19]. It is our opinion that some of these lesions may also benefit from our ‘above and below’ approach. The factors identified by Zada et al. may be used as relative indications for an ‘above and below’ approach.
It must be emphasized, however, that the optimal treatment of huge PAs requires a tailored approach based on individual patients’ conditions and the surgeons’ experiences and abilities. Our technique therefore represents only one of the many available strategies; it may be considered as a safe alternative when expertise in a single-route endonasal endoscopic removal is unavailable. For a complex lesion that obviously requires a transcranial attack, an additional simultaneous transsphenoidal approach may be considered when the sellar tumor component is large or when significant bleeding is anticipated.
It is regrettable that both of our patients developed permanent DI after surgery which, given their large tumors, may not have been preventable. It is reasonable to assume that at least some of the vasopressinergic neurons would have been destroyed prior to surgery despite the absence of clinical DI. Cortisol insufficiency, present in both patients pre-operatively, is known to lessen the degree of polyuria in those with combined anterior and posterior pituitary diseases by reducing renal perfusion and increasing endogenous anti-diuretic hormone release [20]. Further damage sustained intra-operatively (e.g. due to axonal shock) may then lead to clinically apparent permanent DI. Moreover, the administration of cortisol during the peri-operative period would also lead to the rapid onset of polyuria [21]. We speculate that both of these mechanisms (i.e. cumulatively pituitary insult and correction of cortisol insufficiency) played a part in the pathogenesis of DI in our patients.
Conclusion
The simultaneous ‘above and below’ technique is a safe and feasible approach for large-to-giant PAs. The adoption of the endonasal endoscopic transsphenoidal method obviates the need for two operating microscopes, permits freer maneuvers and better orientation for both surgical teams, and is associated with minimal soft tissue injury within the nose. It may be considered as an alternative surgical approach for a carefully selected group of patients.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Musleh W, Sonabend AM, Lesniak MS. Role of craniotomy in the management of pituitary adenomas and sellar/parasellar tumors. Expert Rev Anticancer Ther. 2006;6(Suppl 9):S79–S83. doi: 10.1586/14737140.6.9s.S79. [DOI] [PubMed] [Google Scholar]
- 2.Abe T, Iwata T, Kawamura N, Izumiyama H, Ikeda H, Matsumoto K. Staged transsphenoidal surgery for fibrous nonfunctioning pituitary adenomas with suprasellar extension. Neurol Med Chir (Tokyo) 1997;37:830–835. doi: 10.2176/nmc.37.830. [DOI] [PubMed] [Google Scholar]
- 3.Alleyne CH, Jr, Barrow DL, Oyesiku NM. Combined transsphenoidal and pterional craniotomy approach to giant pituitary tumors. Surg Neurol. 2002;57:380–390. doi: 10.1016/S0090-3019(02)00705-X. [DOI] [PubMed] [Google Scholar]
- 4.D’Ambrosio AL, Syed ON, Grobelny BT, Freda PU, Wardlaw S, Bruce JN. Simultaneous above and below approach to giant pituitary adenomas: surgical strategies and long-term follow-up. Pituitary. 2009;12:217–225. doi: 10.1007/s11102-009-0171-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loyo M, Kleriga E, Mateos H, de Leo R, Delgado A. Combined supra-infrasellar approach for large pituitary tumors. Neurosurgery. 1984;14:485–488. doi: 10.1227/00006123-198404000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Cappabianca P, Cavallo LM, de Divitiis E. Endoscopic endonasal transsphenoidal surgery. Neurosurgery. 2004;55:933–940. doi: 10.1227/01.NEU.0000137330.02549.0D. [DOI] [PubMed] [Google Scholar]
- 7.Wilson CB. A decade of pituitary microsurgery. The Herbert Olivecrona lecture. J Neurosurg. 1984;61:814–833. doi: 10.3171/jns.1984.61.5.0814. [DOI] [PubMed] [Google Scholar]
- 8.Takakura K, Teramoto A. Management of huge pituitary adenomas. Acta Neurochir Suppl. 1996;65:13–15. doi: 10.1007/978-3-7091-9450-8_5. [DOI] [PubMed] [Google Scholar]
- 9.Sinha S, Sharma BS. Giant pituitary adenomas—an enigma revisited. Microsurgical treatment strategies and outcome in a series of 250 patients. Br J Neurosurg. 2010;24:31–39. doi: 10.3109/02688690903370305. [DOI] [PubMed] [Google Scholar]
- 10.Mortini P, Barzaghi R, Losa M, Boari N, Giovanelli M. Surgical treatment of giant pituitary adenomas: strategies and results in a series of 95 consecutive patients. Neurosurgery. 2007;60:993–1002. doi: 10.1227/01.NEU.0000255459.14764.BA. [DOI] [PubMed] [Google Scholar]
- 11.Sanai N, Quinones-Hinojosa A, Narvid J, Kunwar S. Safety and efficacy of the direct endonasal transsphenoidal approach for challenging sellar tumors. J Neurooncol. 2008;87:317–325. doi: 10.1007/s11060-007-9512-2. [DOI] [PubMed] [Google Scholar]
- 12.Jane JA, Jr, Han J, Prevedello DM, Jagannathan J, Dumont AS, Laws ER., Jr Perspectives on endoscopic transsphenoidal surgery. Neurosurg Focus. 2005;19:E2. doi: 10.3171/foc.2005.19.6.3. [DOI] [PubMed] [Google Scholar]
- 13.Nakao N, Itakura T. Surgical outcome of the endoscopic endonasal approach for non-functioning giant pituitary adenoma. J Clin Neurosci. 2011;18:71–75. doi: 10.1016/j.jocn.2010.04.049. [DOI] [PubMed] [Google Scholar]
- 14.Laufer I, Anand VK, Schwartz TH. Endoscopic, endonasal extended transsphenoidal, transplanum transtuberculum approach for resection of suprasellar lesions. J Neurosurg. 2007;106:400–406. doi: 10.3171/jns.2007.106.3.400. [DOI] [PubMed] [Google Scholar]
- 15.Wang RZ, Yin J, Su CB, Ren ZY, Yao Y, Tao W. Extended transsphenoidal operation for giant and invasive pituitary adenomas. Zhonghua Wai Ke Za Zhi. 2006;44:1548–1550. [PubMed] [Google Scholar]
- 16.Greenfield JP, Leng LZ, Chaudhry U, Brown S, Anand VK, Souweidane MM, Schwartz TH. Combined simultaneous endoscopic transsphenoidal and endoscopic transventricular resection of a giant pituitary macroadenoma. Minim Invasive Neurosurg. 2008;51:306–309. doi: 10.1055/s-0028-1082323. [DOI] [PubMed] [Google Scholar]
- 17.Ojha BK, Husain M, Rastogi M, Chandra A, Chugh A, Husain N. Combined trans-sphenoidal and simultaneous trans-ventricular-endoscopic decompression of a giant pituitary adenoma: case report. Acta Neurochir (Wien) 2009;151:843–847. doi: 10.1007/s00701-009-0336-z. [DOI] [PubMed] [Google Scholar]
- 18.Romano A, Chibbaro S, Marsella M, Oretti G, Spiriev T, Iaccarino C, Servadei F. Combined endoscopic transsphenoidal-transventricular approach for resection of a giant pituitary macroadenoma. World Neurosurg. 2010;74:161–164. doi: 10.1016/j.wneu.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 19.Zada G, Du R, Laws ER., Jr Defining the “edge of the envelope”: patient selection in treating complex sellar-based neoplasms via transsphenoidal versus open craniotomy. J Neurosurg. 2011;114:286–300. doi: 10.3171/2010.8.JNS10520. [DOI] [PubMed] [Google Scholar]
- 20.Martin MM. Coexisting anterior pituitary and neurohypophyseal insufficiency. A syndrome with diagnostic implication. Arch Intern Med. 1969;123:409–416. doi: 10.1001/archinte.1969.00300140055013. [DOI] [PubMed] [Google Scholar]
- 21.Garrett P, Langan C, Egan J, Mulloy E, O’Donnell J. Sarcoidosis, anterior pituitary failure, and diabetes insipidus. Ir J Med Sci. 1983;152:136–138. doi: 10.1007/BF02960054. [DOI] [PubMed] [Google Scholar]


