Abstract
Objectives
To assess the behavioural and weight status outcomes in English children in a feasibility study of a novel primary school-based obesity prevention programme.
Design
Exploratory cluster randomised controlled trial of the Healthy Lifestyles Programme.
Setting
Four city primary schools (two control and two intervention) in the South West of England.
Participants
202 children aged 9–10 years, of whom 193 and 188 were followed up at 18 and 24 months, respectively. No child was excluded from the study; however, to be eligible, schools were required to have at least one single Year 5 class.
Intervention
Four-phase multicomponent programme using a range of school-based activities including lessons, assemblies, parents' evenings, interactive drama workshops and goal setting to engage and support schools, children and their families in healthy lifestyle behaviours. It runs over the spring and summer term of Year 5 and the autumn term of Year 6.
Primary and secondary outcomes
Weight status outcomes were body mass index, waist circumference and body fat standard deviation scores (SDS) at 18 and 24 months, and behavioural outcomes were physical activity, television (TV) viewing/screen time and food intake at 18 months.
Results
At 18 months of follow-up, intervention children consumed less energy-dense snacks and more healthy snacks; had less ‘negative food markers’, more ‘positive food markers’, lower mean TV/screen time and spent more time doing moderate-vigorous physical activity each day than those in the control schools. Intervention children had lower anthropometric measures at 18 and 24 months than control children, with larger differences at 24 months than at 18 months for nearly all measures.
Conclusions
Results from this exploratory trial show consistent positive changes in favour of the intervention across all targeted behaviours, which, in turn, appear to affect weight status and body shape. A definitive trial is now justified.
Article summary
Article focus
To present behavioural and weight status outcomes from an exploratory cluster randomised controlled trial of a novel school-based obesity prevention programme with English primary school children.
To present sample size estimates required for a definitive trial of the programme based on outcome results, attrition rates and estimates of the intraclass correlations of the outcome measures.
Key messages
The Healthy Lifestyles Programme (HeLP) has been developed using behaviour change theory and extensive stakeholder involvement to engage and support children and their families in healthy lifestyles.
Behavioural and weight status outcomes at 18 and 24 months from this exploratory trial (Phase 3 pilot) show consistency in the direction of effects, all in favour of the intervention, demonstrating ‘proof of concept’.
Results from the exploratory trial have provided sufficient evidence to support the evaluation of HeLP in a full-scale trial.
Strengths and limitations of this study
The HeLP intervention has undergone a systematic development process using research evidence, behavioural theory, stakeholder consultation and piloting. This has enabled the researchers to gain a deeper understanding of the context in which the intervention was to be delivered in order to maximise engagement at all levels. The exploratory trial presented in this paper (Phase 3 pilot) has demonstrated not only that the design of the trial is feasible, with outcome data obtained from 92% of the original cohort at 24 months after transition to secondary school, but also that behavioural and weight status outcome measures at 18 and 24 months show consistency in the direction of effects (although the differences are relatively small), all in favour of the intervention, demonstrating ‘proof of concept’. This shows that a definitive trial of HeLP is both feasible and justified.
The study was conducted in the South West of England, where the population is predominantly white, and although there are areas of deprivation, none of the four schools had ≥25% of children eligible for free school meals (the national average of proportion of children eligible for free school meals). However, the intervention has been developed to allow the flexibility and adaptation to ensure that it is recognising and responding to the local needs of children and families from different socioeconomic and ethnic groups while still maintaining fidelity. Food intake and television (TV) viewing/screen time were self-reported, and although children were asked to sit in their literacy tables so that appropriate support could be provided to each child during completion, the information children are able to provide is limited. We did, however, go to great lengths to ensure that the questionnaires were simple and presented in such a way so as to trigger recall.
Introduction
During the past 3 decades, the prevalence of obesity in children in Europe has risen dramatically.1 In the UK, the Health Survey for England reported that 19% of girls and 18% of boys aged 11–15 years were obese and 34% of girls and 33% of boys were overweight or obese.2 The National Child Measurement Programme in England reported that by age 10–11 years, one in three children were either overweight or obese.3 Being overweight in childhood is associated with adverse consequences, including metabolic abnormalities, increased risk of type II diabetes and musculoskeletal and psychological problems.4 A recent systematic review showed that the risk of overweight children becoming overweight adults was at least twice as high as for normal weight children,5 and more contemporary data, from a large prospective cohort of children born in the South West of England in 1991/1992 (Avon Longitudinal Study of Parents and Children), showed that the 4-year incidence of obesity was higher between the ages of 7 and 11 years than between 11 and 15 years, suggesting that mid- to late childhood (around 7–11 years) may merit greater attention in future obesity prevention interventions.6
Obesity results from an imbalance between consumption and expenditure of energy. Epidemiological studies suggest a number of risk factors, the strongest of which is having one or more overweight parents.7 There are also strong associations between the risk of overweight and socioeconomic status, diet, physical activity levels and other lifestyle factors.8 At a population level, the consumption of processed and fast food, including sweetened fizzy drinks, has increased while that of fruit and vegetables has declined and portion size in prepackaged food has increased substantially.9 In addition, the National Travel Survey10 has shown that, since the 1970s, children's transport activity (eg, walking or cycling to school) has been in decline.
Evidence about the relationship between physical activity, sedentary behaviours and childhood obesity is scarce with reviews of physical activity and obesity prevention reporting inconsistent results.11 12 Using data from the Avon Longitudinal Study of Parents and Children, Riddoch and colleagues13 found strong associations between children's fat mass at age 14 and their physical activity at age 12. Compared with previous generations, children in the UK spend more time participating in sedentary activities, with research suggesting that children spend an average of 4.5 h a day looking at a screen.14 Some studies have reported an association between time spent watching TV and obesity.15 Not only is TV viewing a sedentary activity, but it is also positively correlated with total calorific intake16 and the consumption of snack foods.17
Schools have the potential to play a critical role in the prevention of overweight and obesity, and the more recent development of community-wide multisite approaches often use school-based interventions as part of the overall programme of events.18 19 Schools' existing organisational, social and communication structures provide opportunities for regular health education and for the creation of a health-enhancing environment and, if school-based interventions are developed in a systematic way involving stakeholders and appropriate piloting phases, they have the potential to reach children and their families across the social spectrum. The most recent systematic review (2008) of controlled trials of school-based interventions concluded that interventions that aim to increase activity and reduce sedentary behaviour and affect diet may be more effective in preventing children becoming overweight in the long term.20
The Healthy Lifestyles Programme (HeLP) is an innovative school-based intervention that aims to deliver a general healthy lifestyle message encouraging a healthy energy balance. The programme takes a population approach, seeking to change behaviour at a family as well as at an individual and school level. The development of HeLP followed the MRC guidance for the development and evaluation of complex interventions21 involving careful theoretical derivation of behaviour change techniques (BCTs)22 and three phases of iterative pilot work.23 Phase 3 was the exploratory randomised controlled trial (RCT) to assess, for schools, children and their families: recruitment and retention in control and intervention schools; feasibility and acceptability of the intervention and of future trial outcomes measures and facilitators and barriers to uptake of the intervention. In addition, data from this trial would help us in calculating the sample size required for a full-scale trial. Here we present the behavioural and weight status outcomes from the exploratory RCT and the estimation of the sample size required for a definitive evaluation of the programme.
Methods
Study design
This is an exploratory cluster RCT of the HeLP intervention, in Exeter (a city in the South West of England), involving 202 children aged 9–10 years. There is little ethnic mix in the South West, with the majority of the population being ‘white’. Although overall socioeconomic status for the area is higher than average; within Exeter, there are some areas with quite severe deprivation. All state primary and junior schools in Exeter were eligible to take part if they had at least one single age Year 5 class (9–10-year-olds) (ie, not mixed classes, 8–10- or 9–11-year-olds). Schools were recruited via the local network of primary school head teachers. Of the 11 eligible schools in Exeter, eight expressed an interest from which four schools (with a total of seven Year 5 classes) were randomly selected to participate and randomly allocated to intervention or control using a telephone-based randomisation service involving a statistician independent of the research. All parents of children were sent an information pack with an opportunity to opt-out of the study. If the opt-out form was not returned within 2 weeks, consent was inferred. The class teacher gave daily oral reminders to the children over this 2-week period to ensure that they and their parents had read the information sheet. Baseline measures were taken prior to schools being randomised to control or intervention groups.
Intervention
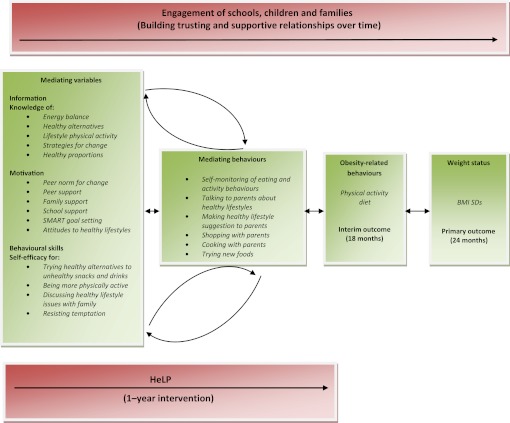
HeLP is a multicomponent four-phase programme delivered to 9–10-year-olds over three school terms (spring and summer term of Year 5 and autumn term of Year 6). The programme is based on the Information, Motivation and Behavioural Skills Model,24 which proposes that adequate information, motivation and behavioural skills are essential to behaviour change. Information, Motivation and Behavioural Skills Model has been demonstrated to provide an effective basis for behaviour change interventions in other domains25 26 and aims to deliver a general healthy lifestyle message encouraging a healthy energy balance. Within this context, three key behaviours are emphasised: a decrease in the consumption of sweetened fizzy drinks, an increase in the proportion of healthy snacks (HS) to unhealthy snacks consumed and a reduction in television (TV) viewing and other screen-based activities. These messages are consistent with the strategies suggested in the UK National Institute for Clinical Excellence (NICE) guidance on the prevention of overweight and obesity in adults and children.27 We hypothesise that targeting information, motivation and behavioural skills will lead to the adoption of mediating behaviours, which will, in turn, lead to improvements in diet and physical activity thus preventing excessive weight gain. These mediating variables and behaviours will interact to strengthen the engagement of children and their parents throughout the course of the intervention. Figure 1 provides a representation of this process indicating the feedback loops.
Figure 1.
The Healthy Lifestyles Programme (HeLP) process model. BMI, body mass index.
An Intervention Mapping approach,28 involving considerable stakeholder consultation and pilot work, was undertaken to link theory to specific BCTs29 30 and methods of delivery22 that were suitably engaging and compatible with the existing school curriculum. Table 1 shows each phase of HeLP, the targets of change, the BCTs used and the method and agent of delivery. Key to engaging and motivating the children are the highly inclusive and interactive drama activities, which are built around four characters (Disorganised Duncan, Football Freddie, Snacky Sam and Active Amy) with whom the children identify. During the Healthy Lifestyles Week (Phase 2), children work closely with the character most like them to help them to change their behaviours. In Phase 3, the children reflect on their own lifestyle behaviours around diet and activity and set simple goals with their parents. The programme has been specifically designed so that the function of each phase is clearly defined and delivered appropriately, while the precise content can be adapted to relate to children from differing ethnic and social backgrounds. During the drama workshops, children co-create scenes with the actors and provide their own ideas and solutions to problems faced by the characters.
Table 1.
Intervention phases, change targets, BCTs and the method and agent of delivery
| Intervention phase | Change targets | BCTs | Method (frequency and duration) | Agent of delivery |
| Phase 1 | Establish relationships with schools, children and families | Provide information on behaviour–health link |
|
HeLP coordinators |
| Creating a supportive context | Raise awareness and increase knowledge | Provide information on health–behaviour link | Newsletter articles (3) (over the spring term) | HeLP coordinators |
| Spring term (Year 5) | Promote positive attitudes and norms towards healthy eating and physical activity |
|
Activity workshops (2) (parents observe) (1.5 h) | Professional sportsmen/dancers |
| Skill building | Parents' evening (1) involving child performances; (1 h) | Class teachers/HeLP coordinator/drama group | ||
| Increase self-efficacy for behaviour change | ||||
| Phase 2 | Strengthen relationships with schools, children and families | Provide information on health–behaviour link | *PSHE lessons (5) (morning) (1 h) | Class teacher |
| Intensive healthy lifestyles week—1 week |
|
Problem solving/barrier identification modelling/demonstrating behaviour | §Drama (5) (afternoon) (forum theatre; role play; food tasting, discussions, games, etc) (2 h) | Drama group |
| Summer term (Year 5) |
|
|
||
| Phase 3 | Increase awareness of own behaviour | Self-monitoring | Self-reflection questionnaire (1) (40 mins) | HeLP coordinator/class teacher |
| Personal goal setting with parental support—goals set during week following drama |
|
|
Goal setting sheet to go home to parents to complete with child (1) (10 mins) | HeLP coordinator/parents |
| Agree behavioural contract | 1:1 goal setting interview (1) (goals sent home to parents) (10 mins) | HeLP coordinator | ||
| Summer term (Year 5) | Prompt identification as a role model | Parent's evening (1) (child involvement—Forum Theatre) (1 h) | HeLP coordinator/drama group | |
| Phase 4 | Increase self-awareness and prioritise healthy goals. Consolidate social support | Provide information on health–behaviour link | Newsletter articles (2) (over the autumn term) |
|
| Reinforcement activities | ||||
| Develop monitoring and coping skills |
|
|
|
|
| Autumn term (Year 6) | Increase parental support |
|
|
|
|
1-to-1 goal supporting interview to discuss facilitators/barriers and to plan new coping strategies (1) (10 mins) (renewed goals sent home to parents) | HeLP coordinator |
PSHE – Personal, Social and Health Education
The drama framework includes 4 characters, each represented by one of the actors, whose attributes related to the three key behaviours. Children choose which of the characters they most resemble then work with that actor to help the character learn to change their behaviour.
Outcome measures
Baseline height, weight, waist circumference, % body fat, food intake, TV viewing/screen-based activity and physical activity were collected at the start of the school year, in the autumn term (October/November 2008) prior to randomisation of schools. These same measures were then collected 18 months post-baseline (June/July 2009), and anthropometric measures only were collected 24 months post-baseline (October/November 2010), after the children had moved to secondary school.
Anthropometric
All anthropometric measures were taken by an independent assessor who was blinded to each child's allocated group. For the anthropometric measures, children were asked to remove their shoes and socks. Height was measured using a portable SECA stadiometer (Hamburg, Germany) and recorded to an accuracy of 1 mm. Weight and body fatness was measured using the Tanita SC330 portable body composition analyser (UK Ltd, Middlesex, UK). Weight was recorded to within 0.1 kg. Body fatness was estimated from leg-to-leg bioelectrical impedance. Waist circumference was measured using a non-elastic flexible tape 4 cm above the umbilicus.
Behavioural
Food intake was assessed using an adapted version of the validated Food Intake Questionnaire,31 a recall method that asks whether specific foods were consumed the previous day. Children completed the Food Intake Questionnaire twice, during school hours, in order to obtain a weekday and weekend food intake. These results were then combined and weighted to calculate the mean number of different HS, energy-dense snacks (EDS), positive (PM) and negative (NM) foods markers consumed each day. TV viewing/screen-based usage was assessed using an adapted version of the validated Children's TV Viewing Habits Questionnaire.32 Participants were asked to record the time (in minutes) they usually spent watching TV or doing other leisure time screen-based activities on weekdays before school, before tea and after tea and on the weekend (Saturday and Sunday morning, afternoon and evening). The results were then combined and weighted to calculate the mean time spent watching TV/doing leisure time screen-based activities each day. Additional information on the number and location of TV sets and rules in the home regarding TV viewing and screen-based usage was also collected.
Questionnaires were completed during class time, where children were asked to sit in their literacy groups (table groupings based on their ability in literacy). JJL instructed the class on how to complete the questionnaires and, with the class teacher, learning support assistant, and an additional researcher assisted individual children where necessary. Physical activity was measured in one randomly selected class per school using a GT1M Actigraph (Actigraph LLC, Pensacola, Florida, USA: http://www.theactigraph.com), attached to a flexible elastic belt fastened securely round the waist, which children were asked to wear during waking hours over seven consecutive days (five weekdays and two weekend days). As the device is not waterproof, children were instructed to remove it for water-based activities and record on their log sheet the reason for removal and the duration of this non-wear time.
Data management
Anthropometric and questionnaire data were entered into a specifically designed database. Ten per cent of entries (using a random number generator) were subsequently checked by a second researcher revealing only two data entry errors.
The raw accelerometry data from the pre- and post-time points were processed using kinesoft software (V.3.3.55) and quality control checks carried out. To be included in the analysis, participants had to have at least 10 h of wear time a day on three weekdays and one weekend day. Days were counted if participants accrued 10 h of wear time during the day. Periods of non-wear time were classified as 30 min of zero counts. Those who failed to meet the inclusion criteria were excluded from subsequent analysis. Usable accelerometry data were obtained for 104/111 (95%) and 95/111 (85%) participants at baseline and 18 months of follow-up, respectively.
Eligible days of data were organised into time spent in each activity intensity per day. Activity intensity categories were classified using the following previously published cut points (sedentary: 0–299; light: 300–3580; moderate: 3581–6129; vigorous: ≥6130).33
Statistical analysis
As this was an exploratory study, we sought to use the results, including the attrition rates and estimates of the intraclass correlations of the outcome measures, to help us plan a definitive cluster RCT, including estimating the sample size needed for such a definitive trial.
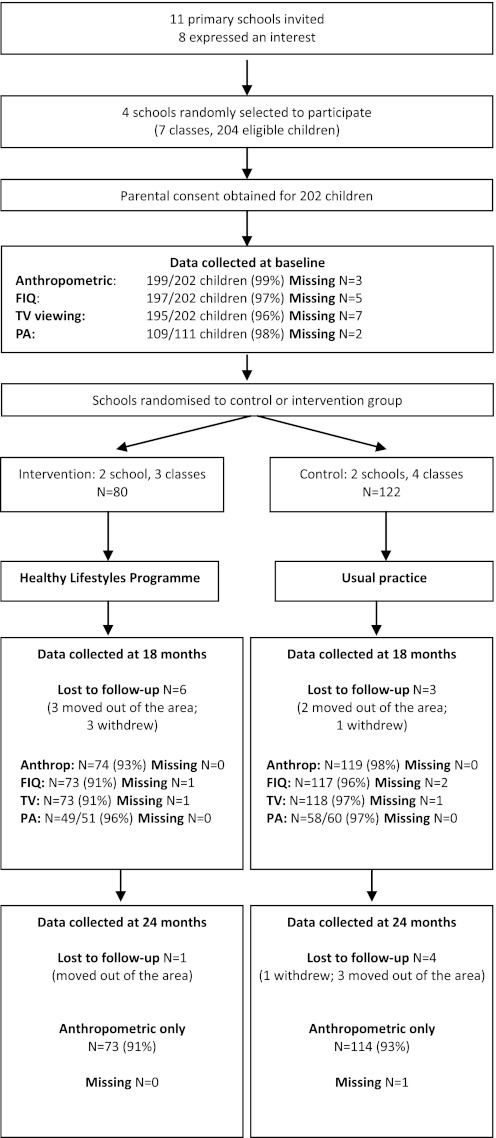
The main analysis of the effect of the exploratory trial was undertaken on an intention-to-treat basis. As there was only a small number of missing data for some of the outcomes (see figure 2), the analysis was based on all the available data, with no imputation for missing data. As this was an exploratory trial involving only four schools, only cluster-level analyses were undertaken34 35; this meant that the analyses could not be adjusted for individual-level covariates (eg, baseline measures). As there were varying numbers of children in each school, the analyses were weighted by cluster size35 36; inverse variance weighting was not used, given the uncertainties in estimating the intraclass correlation coefficients (ICCs).
Figure 2.
Flow chart of participants through the trial and numbers of children from whom measures were collected. Anthrop, anthropometric; FIQ, Food Intake Questionnaire; PA, physical activity.
Differences between the intervention and control groups are presented, together with 95% CIs. Unadjusted results (ie, without clustering being taken into account) are also presented, in order to allow comparison of the precision of the estimates of the effect of the intervention. ICCs (and 95% CIs) were calculated for selected outcomes. All analyses were undertaken in STATA V.11.1.
Results
Recruitment and participant characteristics at baseline
Figure 2 shows the flow of participants through the trial37 and follow-up of anthropometric measures at 18 and 24 months. The intervention group consisted of two primary schools, one with 170 children on the school roll (13% eligible for free school meals (FSM) and one larger primary school with 384 children on the roll (2.6% FSM). The control group consisted of two primary schools, one with 317 on roll (14% FSM) and the other with 364 on roll (6% FSM).
Table 2 shows that the intervention and control groups were generally comparable at baseline with the percentages of children overweight/obese being 24% and 26%, respectively.38 While there was higher percentage of obese and a higher percentage body fat (≥85th and <95th centile) in the control schools, the continuous measurements had very similar means and ranges. Food intake on all categories was similar for both control and intervention groups, with an approximate ratio for HS:EDS and PM:NM of 1:1. Children's mean TV viewing/screen time was 2.6 h a day, which mirrors national data for 4–15-year-olds.16 The percentage of children who had TVs in their bedrooms was higher in the control group compared with the intervention group; however, the percentage of children who had no rules regarding screen time was higher in the intervention group compared with the control group. Both groups spent a similar amount of time per day in sedentary activities but differed slightly in time spent in moderate-vigorous physical activity; however, this varied greatly between children (range: 13.7–104 min). Mean sedentary time (including sleep time) for all children was 16.2 h/day.
Table 2.
Baseline characteristics of children allocated to the intervention and control
| Intervention (n=80) | Control (n=122) | Total (n=202) | |
| Demographics | |||
| Age, years, mean (SD) | 9.69 (0.3) | 9.69 (0.3) | 9.69 (0.3) |
| Sex, % (n) | |||
| Male | 50.0 (40) | 50.0 (61) | 50.0 (101) |
| Female | 50.0 (40) | 50.0 (61) | 50.0 (101) |
| Total % of all children in the schools eligible for free school meals | 5.7 | 9.7 | 7.9 |
| Anthropometric measures | |||
| Overweight (≥85th and <95th centile), % (n)* | 10.5 (8) | 7.6 (9) | 8.7 (17) |
| Obese (≥95th centile), % (n) | 13.2 (10) | 18.5 (22) | 16.4 (32) |
| Underweight (≤2nd centile), % (n) | 1.3 (1) | 0.0 (0) | 0.5 (1) |
| Body fat (≥85th and <95th centile), % (n)† | 5.3 (4) | 11.8 (14) | 9.2 (18) |
| Body fat (≥95th centile), % (n) | 11.8 (9) | 10.1 (12) | 10.8 (21) |
| Body fat (≤2nd centile), % (n) | 19.7 (15) | 14.3 (17) | 16.4 (32) |
| Waist circumference (≥85th and <95th centile), % (n)‡ | 21.3 (17) | 21.3 (26) | 21.3 (43) |
| Waist circumference (≥95th centile), % (n) | 21.3 (17) | 21.3 (26) | 21.3 (43) |
| BMI, mean (SD) (range) | 17.4 (2.6) (13.3 to 25.4) | 17.8 (2.8) (13.7 to 25.1) | 17.6 (2.7) (13.3 to 25.4) |
| BMI SDS, mean (SD) (range) | 0.3 (1.1) (−2.3 to 2.5) | 0.4 (1.1) (−2.0 to 2.9) | 0.3 (1.1) (−2.3 to 2.9) |
| % Body fat, mean (SD) (range) | 19.3 (6.8) (3.0 to 37.4) | 20.0 (6.7) (7.6 to 36.8) | 19.71 (6.8) (3.0 to 37.4) |
| % Body fat SDS, mean (SD) (range) | −0.9 (3.4) (−25.8 to 2.3) | −0.5 (1.7) (−6.5 to 2.4) | −0.6 (2.5) (−25.8 to 2.4) |
| Waist circumference (cm), mean (SD) (range) | 62.0 (6.5) (50 to 81) | 62.6 (7.0) (52 to 83) | 62.3 (6.8) (50 to 83) |
| Waist circumference SDS, mean (SD) (range) | 0.8 (1.0) (−1.9 to 3.0) | 0.91 (1.0) (−1.2 to 3.2) | 0.9 (1.0) (−1.9 to 3.2) |
| Food intake§ (SD) | |||
| EDS, mean (SD) (range) | 4.2 (2.2) (0.0 to 10.7) | 4.1 (2.1) (0.3 to 11.2) | 4.2 (2.1) (0.0 to 11.2) |
| HS, mean (SD) (range) | 3.2 (1.6) (0.3 to 8.4) | 3.4 (1.7) (0.0 to 8.0) | 3.4 (1.7) (0.0 to 8.4) |
| PM, mean (SD) (range) | 7.3 (2.9) (2.6 to 15.0) | 7.6 (3.3) (2.3 to 20.3) | 7.5 (3.1) (2.3 to 20.3) |
| NM, mean (SD) (range) | 6.8 (3.3) (1.4 to 16.6) | 6.8 (3.2) (0.3 to 20.2) | 6.8 (3.2) (0.3 to 20.2) |
| TV/screen viewing | |||
| TV/screen viewing (hours/day), mean (SD) (range) | 2.5 (1.7) (0.1 to 7.9) | 2.7 (1.7) (0.3 to 8.4) | 2.6 (1.7) (0.1 to 8.4) |
| TV in bedroom, % (n) | 45.6 (36) | 59.8 (73) | 54.2 (109) |
| No rules for TV/screen time, % (n) | 39.2 (31) | 33.9 (40) | 36.0 (71) |
| Physical activity (PA) | |||
| Moderate-vigorous PA (mins/day), mean (SD) (range) | 36.7 (12.0) (13.7 to 70.0) | 49.5 (20.0) (18.1 to 104.4) | 43.6 (17.9) (13.7 to 104.4) |
| Sedentary activities (hours/day), mean (SD) (range) | 16.2 (1.6) (9.8 to 18.7) | 16.4 (1.9) (10.6 to 19.2) | 16.2 (1.9) (9.3 to 19.2) |
Intervention and control group comparisons at follow-up
Anthropometric
Anthropometric follow-up data were collected for 193 and 187 participants at 18 and 24 months, respectively (94% and 92% of the original cohort of 202 children). Table 3 shows the comparisons of the main outcomes at 18- and 24-month follow-ups between the children in the intervention schools and control schools. Children in the intervention schools typically fared better than those in the control schools having, on average, lower anthropometric measures at 18 and 24 months with larger differences at 24 months than at 18 months for all measures except percentage body fat standard deviations (SDs). At 18 months, the proportion of overweight and obese children had increased by 6% in the control schools (from 26% (31/122) to 32% (38/119)), while remaining at baseline levels in the intervention schools (24% (18/74)). At 24 months, the proportion of overweight/obese children remained at 32% (36/114) in the control schools and decreased slightly to 22% (16/73) in the intervention schools. The waist circumference data show similar proportions at baseline (≥85th centile) shifting to an 8.7% difference in favour of the intervention at 24 months.
Table 3.
Difference in outcomes at 18 and 24 months of follow-up of children allocated to the intervention and control groups
| Mean difference (intervention minus control) (95% CI) |
||||
| 18 months |
24 months |
|||
| Outcome | Unadjusted | Adjusted for clustering | Unadjusted | Adjusted for clustering |
| BMI | −0.95 (−1.88 to −0.02) | −0.95 (−3.79 to 1.90) | −1.16 (−2.15 to −0.18) | −1.16 (−3.82 to 1.49) |
| BMI SDs | −0.38 (−0.74 to −0.02) | −0.38 (−1.65 to 0.89) | −0.45 (−0.82 to −0.08) | −0.45 (−1.71 to 0.81) |
| % Body fat | −0.83 (−3.01 to 1.36) | −0.83 (−6.26 to 4.60) | −1.28 (−3.60 to 1.05) | −1.28 (−8.69 to 6.14) |
| % Body fat SDs | −0.33 (−1.04 to 0.38) | −0.33 (−2.52 to 1.85) | −0.21 (−0.85 to 0.42) | −0.21 (−2.45 to 2.03) |
| Waist circumference (cm) | −2.01 (−4.23 to 0.21) | −2.01 (−9.54 to 5.52) | −2.97 (−5.36 to −0.59) | −2.97 (−10.30 to 4.35) |
| Waist circumference SDs | −0.32 (−0.63 to −0.01) | −0.32 (−1.52 to 0.87) | −0.46 (−0.79 to −0.13) | −0.46 (−1.72 to 0.80) |
| Per cent with BMI ≥85th centile | −7.6 (−20.5 to 5.3) | −7.6 (−49.4 to 34.2) | −9.7 (−22.4 to 3.1) | −9.7 (−27.8 to 8.5) |
| Per cent with % body fat ≥85th centile obese | −5.5 (−15.6 to 4.6) | −5.5 (−31.8 to 20.9) | −6.4 (−17.8 to 5.1) | −6.4 (−34.9 to 22.1) |
| Per cent with waist circumference ≥85th centile | −5.9 (−20.1 to 8.3) | −5.9 (−50.7 to 39.0) | −8.7 (−22.9 to 5.4) | −8.7 (−58.9 to 41.4) |
| Energy-dense snacks | −0.28 (−0.83 to 0.27) | −0.28 (−0.83 to 0.27) | – | – |
| Healthy snacks | 0.47 (0.02 to 0.92) | 0.47 (−1.29 to 2.23) | – | – |
| Positive food markers | 0.38 (−0.37 to 1.13) | 0.38 (−1.55 to 2.31) | – | – |
| Negative food markers | −0.69 (−1.52 to 0.15) | −0.69 (−1.70 to 0.33) | – | – |
| Duration of TV viewing (hours/day) | −0.41 (−0.91 to 0.09) | −0.41 (−1.28 to 0.46) | – | – |
| Sedentary activities (hours/day) | −0.04 (−1.09 to 1.01) | −0.04 (−1.91 to 1.84) | – | – |
| Moderate-vigorous PA (mins/day) | 5.67 (0.20 to 11.15) | 5.67 (−12.59 to 23.93) | – | – |
BMI, body mass index; PA, physical activity.
Behavioural
At 18 months of follow-up, children in the intervention schools had less ‘negative food markers’, consumed less EDS and more HS, had more ‘positive food markers’, had lower mean TV/screen time and on average spent more time doing moderate-vigorous physical activity each day than children in the control schools.
As expected, the 95% CIs were narrower for all outcomes in the unadjusted results when the clustering within schools was (incorrectly) not accounted for in the analyses.
Estimation of ICCs
The ICC for body mass index (BMI) at 24 months for this exploratory trial was estimated to be 0.04 (95% CI 0.00 to 0.15) and for BMI SDs at 24 months was 0.06 (0.00 to 0.19). As four clusters are insufficient to precisely estimate the ICCs, we have looked at the effect of using a range of ICCs, based on both our pilot data and other published data in this field,41–43 in our sample size calculations for a definitive RCT (see table 4).
Table 4.
Sample size calculations for a definite RCT with primary outcome of BMI SDs at 24 months under different assumptions
| 80% power |
90% power |
|||||
| Minimum difference detectable |
Minimum difference detectable |
|||||
| ICC | 0.25 | 0.30 | 0.50 | 0.25 | 0.30 | 0.50 |
| 0.01 | 571 | 397 | 145 | 764 | 531 | 193 |
| 0.03 | 947 | 658 | 240 | 1267 | 880 | 320 |
| 0.06 | 1511 | 1050 | 383 | 2021 | 1404 | 511 |
| 0.10 | 2262 | 1572 | 573 | 3027 | 2103 | 765 |
All numbers are the total number of children required to be recruited, assuming 50 children per school and a loss to follow-up at 24 months of 20%.
The calculations take into account the reduction in variability associated with adjusting for baseline BMI SDs, conservatively assuming the correlation between baseline and 24 months data to be 0.8 (in our pilot study, this correlation was 0.93).
This is the sample size required to detect a true minimal difference in BMI SDs of 0.25, 0.3 or 0.5, assuming the SD is 1.3 (based on our pilot data).
BMI, body mass index; ICC, intraclass correlation coefficient; RCT, randomised controlled trial.
Estimation of sample size required for definitive trial
Statistical efficiency will be maximised in a full trial by analysing BMI SDs and adjusting for baseline values, which will reduce the SE of the estimates of the difference between intervention and control. In this exploratory trial, the correlation between baseline and 24-month BMI SDs was 0.93 (95% CI 0.92 to 0.96).
The sample size estimates shown are based on recruiting 26 schools, each with an average of 50 children. Using BMI SDs as the primary outcome measure at 24 months of follow-up, table 4 shows possible sample sizes required for a definitive trial, for a number of possible scenarios (varying possible effect sizes and ICCs). All sample size calculations are two-sided, significance level of 5%, with an adjustment for a more conservative reduction in variability (assuming a correlation between baseline and 24-month measures of 0.8) and assuming a loss to follow-up of 20%.
A difference in BMI SDs of 0.25 has been shown to be a meaningful change, impacting on improvement on adiposity and metabolic health.44 Using a significance level of 5%, we would need to recruit 1267 children from 26 schools to be able to detect a true difference of at least 0.25, with 90% power, allowing for a conservative attrition rate of 20%, assuming an ICC of 0.03.
Discussion
We have shown over three phases of piloting that HeLP is feasible and acceptable to schools, children and their families23 and that the study design is feasible for a definitive evaluation. We were able to recruit and retain schools and children throughout the study, obtaining follow-up data from 92% of the original cohort at 24 months, after the children had moved on to secondary school. In addition, we obtained usable accelerometry data from 85% of the children at 18 months. We are aware that with a sample size of 202 children and only four schools, the trial was not powered to be able to provide precise estimates of the effect of the intervention. Analyses were undertaken at cluster-level only, thus unable to be adjusted for individual-level covariates (such as measures at baseline); however, both behavioural and anthropometric outcome measures at 18 and 24 months showed consistency in the direction of effects, all in favour of the intervention, demonstrating ‘proof of concept’.
Although estimates of the differences between intervention and control schools were imprecise, it is encouraging to see that there was a consistent positive impact on the behaviours targeted (snacking, screen time and physical activity) and on anthropometric values. When we began the development of this programme back in 2005, we believed that the cumulative effect of making small sustainable changes in multiple behaviours related to the energy balance had the potential to significantly impact on weight status. Interestingly, there were larger differences at 24 months than at 18 months for all measures except percentage body fat SDs, which is encouraging, suggesting the potential of the programme to support children and their families to sustain these lifestyle changes in the longer term.
Further evidence of ‘proof of concept’ is shown by looking at the weight status proportions. While the proportion of overweight and obese were similar at baseline in both groups, in the control schools, this increased to 32% at 18 months (matching our national data for children of the same age) but remained at baseline levels in the intervention schools at both the 18 and 24 months of follow-up, suggesting that the intervention may have the effect of preventing the shift from normal to overweight or overweight to obese that occurs during this time. These results are supported by recent tracking data from England showing that the greatest increases in weight in a non-obese sample are between the ages of 7 and 11 years.6 Our waist circumference data are particularly striking, showing a reduction of almost 10% in those with a waist circumference greater than the 85th centile in the intervention group at 24 months, while remaining at baseline levels in the control group.
In the planned definitive RCT, more sophisticated statistical analyses will be able to be undertaken at the individual level and, by incorporating individual-level covariates, the precision of effect of the intervention will be further improved. Despite being unable to do this for the current study, the data obtained from this study have enabled us to calculate a likely sample size required for the definitive evaluation.
Conclusions
Situating an intervention within a school is not sufficient within itself to generate sustained behaviour change. It is critical to engage and motivate children and to generate a supportive social context involving the whole school as well as children's parents.45 HeLP is unique in that it uses highly inclusive and interactive delivery methods for a range of BCTs to encourage identification with and ownership of the key messages, ensuring that children have the information, motivation, behavioural skills and support necessary to initiate and sustain change. Results from this exploratory trial show positive changes in favour of the intervention across all targeted behaviours (snacking, screen time and physical activity). Furthermore, these changes appear to have a sustained effect on children's weight status and body shape. We have now secured funding from the NIHR Public Health Research programme to carry out the definitive trial of HeLP starting in March 2012.
Supplementary Material
Acknowledgments
We are very grateful to the staff, pupils and parents of the four participating schools, who gave up their time for the study. We also acknowledge Sandy Akerman (Headbangers Theatre Company) who supported the design of the drama component of the intervention and Stuart Logan who helped design the study and secure funding.
Footnotes
To cite: Lloyd JJ, Wyatt KM, Creanor S. Behavioural and weight status outcomes from an exploratory trial of the Healthy Lifestyles Programme (HeLP): a novel school-based obesity prevention programme. BMJ Open 2012;2:e000390. doi:10.1136/bmjopen-2011-000390
Contributors: JJL drafted the manuscript with KMW and SC providing critical revision. SC carried out the statistical analysis and drafted this section of the manuscript. JJL developed and supported the design and production of the intervention materials, coordinated the implementation of the intervention and the collection of measurements at baseline, 18 and 24 months. JLL, KMW and SL designed the study and obtained funding. JLL will act as guarantor of the paper. All authors approved the final version of the manuscript to be published.
Funding: The Exploratory Trial was funded by the National Institute for Health Research (NIHR) Research for Patient Benefit Programme. JLL and KMW were partially supported by PenCLAHRC, the NIHR CLAHRC for the Southwest Peninsula. This paper presents independent research commissioned by the NIHR. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Competing interests: None.
Ethics approval: Ethical approval was granted from the Peninsula College of Medicine and Dentistry Ethics Committee in 2008.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No data are available.
References
- 1.Jackson-Leach R, Lobstein T. Estimated burden of paediatric obesity and co-morbidities in Europe. Part 1. The increase in the prevalence of child obesity in Europe is itself increasing. Int J Pediatr Obes 2006;1:26–32 [DOI] [PubMed] [Google Scholar]
- 2.The NHS Information Centre Health Survey for England—2008 Trend Tables. London: The NHS Information Centre, 2009 [Google Scholar]
- 3.National Child Measurement Programme Results from the School Year 2009/10. Oxford: National Child Measurement Programme, 2010 [Google Scholar]
- 4.Gunnell DJ, Frankel SJ, Nanchahal K, et al. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr 1998;67:1111–18 [DOI] [PubMed] [Google Scholar]
- 5.Singh AS, Mulder C, Twisk JW, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474–88 [DOI] [PubMed] [Google Scholar]
- 6.Hughes AR, Sherriff A, Lawlor DA, et al. Incidence of obesity during childhood and adolescence in a large contemporary cohort. Prev Med 2011;52:300–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lake JK, Power C, Cole TJ. Child to adult body mass index in the 1958 British birth cohort: associations with parental obesity. Arch Dis Child 1997;77:376–80 [DOI] [PubMed] [Google Scholar]
- 8.Li L, Law C, Lo Conte R, et al. Intergenerational influences on childhood body mass index: the effect of parental body mass index trajectories. Am J Clin Nutr 2009;89:551–7 [DOI] [PubMed] [Google Scholar]
- 9.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977-1998. JAMA 2003;289:450–3 [DOI] [PubMed] [Google Scholar]
- 10.National Travel Survey Trends in Personal Travel Trips, Distance Travelled and Time Taken Per Person Per Year: Great Britain, Since 1972/73. London: National Travel Survey, 2010 [Google Scholar]
- 11.Molnár D, Livingstone B. Physical activity in relation to overweight and obesity in children and adolescents. Eur J Pediatr 2000;159(Suppl 1):S45–55 [DOI] [PubMed] [Google Scholar]
- 12.Wareham N. Physical activity and obesity prevention. Obes Rev 2007;8(Suppl 1):109–14 [DOI] [PubMed] [Google Scholar]
- 13.Riddoch CJ, Leary SD, Ness AR, et al. Prospective associations between objective measures of physical activity and fat mass in 12-14 year old children: the Avon Longitudinal Study of Parents and Children (ALSPAC). BMJ 2009;339:b4544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Childwise The Childwise Monitor Trends Report 2010/11. Norwich: Childwise, 2011 [Google Scholar]
- 15.Marshall SJ, Biddle SJ, Gorely T, et al. Relationships between media use, body fatness and physical activity in children and youth: a meta-analysis. Int J Obes Relat Metab Disord 2004;28:1238–46 [DOI] [PubMed] [Google Scholar]
- 16.Wiecha JL, Peterson KE, Ludwig DS, et al. When children eat what they watch: impact of television viewing on dietary intake in youth. Arch Pediatr Adolesc Med 2006;160:436–42 [DOI] [PubMed] [Google Scholar]
- 17.Halford JC, Gillespie J, Brown V, et al. Effect of television advertisements for foods on food consumption in children. Appetite 2004;42:221–5 [DOI] [PubMed] [Google Scholar]
- 18.de Silva-Sanigorski A, Bolton K, Haby M, et al. Scaling up community-based obesity prevention in Australia: Background and evaluation design of the Health Promoting Communities: Being Active Eating Well initiative. BMC Public Health 2010;10:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr 2010;91:831–40 [DOI] [PubMed] [Google Scholar]
- 20.Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev 2009;10:110–41 [DOI] [PubMed] [Google Scholar]
- 21.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lloyd JJ, Logan S, Greaves CJ, et al. Evidence, Theory and Context - Using intervention mapping to develop a school-based intervention to prevent obesity in children. Int J Behav Nutr Phys Act 2011;8:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wyatt KM, Lloyd JJ, Creanor S, et al. The development, feasibility and acceptability of a school-based obesity prevention programme: results from three phases of piloting. BMJ Open 2011. http://bmjopen.bmj.com/content/early/2011/05/23/bmjopen-2010-000026.abstract (accessed 13 Sep 2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fisher JD, Fisher WA. The information-motivation-behavioral skills model. In: DiClemente R, Crosby R, Kegler M, eds. Emerging Theories in Health Promotion Practice and Research. San Fransisco: Jossy-Bass, 2002:40–70 [Google Scholar]
- 25.Fisher JD, Fisher WA, Amico KR, et al. An information-motivation-behavioral skills model of Adherence to Antiretroviral Therapy. Health Psych 2006;25:462–73 [DOI] [PubMed] [Google Scholar]
- 26.Fisher JD, Fisher WA, Williams SS, et al. Empirical Tests of an information-motivation-behavioral skills model of AIDS-Preventive behavior with Gay Men and Heterosexual University Students. Health Psych 1994;13:238–50 [DOI] [PubMed] [Google Scholar]
- 27.NICE Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. London: NICE, 2006 [PubMed] [Google Scholar]
- 28.Bartholomew LK. Planning Health Promotion Programs: An Intervention Mapping Approach. San Francisco: Jossey-Bass, 2006:171–459 [Google Scholar]
- 29.Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26:1479–98 [DOI] [PubMed] [Google Scholar]
- 30.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379–87 [DOI] [PubMed] [Google Scholar]
- 31.Johnson B, Hackett AF. Eating habits of 11–14-year-old schoolchildren living in less affluent areas of Liverpool, UK. J Hum Nutr Diet 1997;10:135–44 [Google Scholar]
- 32.Owens J, Maxim R, McGuinn M, et al. Television-viewing habits and sleep disturbance in school children. Pediatrics 1999;104:e27. [DOI] [PubMed] [Google Scholar]
- 33.Stone MR, Rowlands AV, Eston RG. Characteristics of the activity pattern in normal weight and overweight boys. Prev Med 2009;49:205–8 [DOI] [PubMed] [Google Scholar]
- 34.Kerry SM, Bland JM. Trials which randomize practices I: how should they be analysed? Fam Pract 1998;15:80–3 [DOI] [PubMed] [Google Scholar]
- 35.Donner A, Klar N. Design and Analysis of Cluster Randomization Trials in Health Research. London: Arnold, 2000:1–178 [Google Scholar]
- 36.Bland JM, Kerry SM. Weighted comparison of means. BMJ 1998;316:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Campbell M, Elbourne D, Altman D. CONSORT statement: extension to cluster randomised trials. BMJ 2004;328:702–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCarthy HD, Cole TJ, Fry T, et al. Body fat reference curves for children. Int J Obes 2006;30:598–602 [DOI] [PubMed] [Google Scholar]
- 40.McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0-16.9 y. Eur J Clin Nutr 2001;55:902–7 [DOI] [PubMed] [Google Scholar]
- 41.Taylor RW, McAuley KA, Barbezat W, et al. APPLE Project: 2-y findings of a community-based obesity prevention program in primary school age children. Am J Clin Nutr 2007;86:735–42 [DOI] [PubMed] [Google Scholar]
- 42.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 1999;153:409–18 [DOI] [PubMed] [Google Scholar]
- 43.Caballero B, Clay T, Davis SM, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr 2003;78:1030–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ford AL, Hunt LP, Cooper A, et al. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child 2010;95:256–61 [DOI] [PubMed] [Google Scholar]
- 45.Foresight Tackling Obesities: Future Choices-Project Report. London: The Stationery Office, 2007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.