Abstract
Arteriovenous malformation (AVM) of the scalp is an uncommon entity. Its management is difficult because of its high shunt flow, complex vascular anatomy, and possible cosmetic complications. The etiology of scalp AVMs may be spontaneous or traumatic. Clinical symptoms frequently include pulsatile mass, headache, local pain, tinnitus; and less frequently, hemorrhage and necrosis. Selective angiography is the most significant diagnosis method. Surgical excision is especially effective in AVMs and the most frequently used treatment method. In this article, we discussed the clinical features and surgical management of scalp AVMs.
Keywords: Arteriovenous malformation, diagnosis, scalp, treatment
Introduction
An arteriovenous malformation (AVM) of the scalp is an abnormal fistulous connection between the feeding arteries and draining veins, without an intervening capillary bed within the subcutaneous layer.[1,2] AVM of the scalp is a rare lesion.[2,3] Its management is difficult because of its high shunt flow, complex vascular anatomy, and possible cosmetic complications.[3,4] The origin of AVM of the scalp is still uncertain, but trauma is an important factor in most of the patients.[3,4 Clinical symptoms frequently include pulsatile mass, headache, local pain, tinnitus; and less frequently, hemorrhage and necrosis.[3,5,6] Surgical treatment is particularly indicated in order to rule out bleeding and for the resolution of cosmetic problems, and in case of tinnitus and headache.[4,6,7]
Case Report
A 60-year-old man was admitted with a huge pulsating mass localized in the left frontotemporal region of the scalp that had been present over a 7-month period, with subcutaneous enlarged vessels. A bruit was also demonstrated over the swelling. He reported no history of scalp trauma. There was no other systemic abnormality. A vascular mass under the scalp in the left temporoparietal region, demonstrating high contrast, was detected on magnetic resonance imaging (MRI) [Figure 1]. Angiography showed multiple AVMs of the scalp. The feeding arteries were the left superficial temporal artery (STA) and the left facial artery, while the draining vein was the left external jugular vein [Figure 2]. There was no evidence of communication with intracranial circulation. As the patient did not present with any systemic problems, he was operated. Surgical excision was performed without complications, with complete excision of the AVM, including the feeding artery and draining vein [Figure 3]. The pathological diagnosis of the patient was consistent with AVM. The histopathological specimen contained various well-developed arteries and dilated veins in the connecting tissue. Endothelial cells and perivascular cells in capillary arteries were positive with immunohistological staining for vascular endothelial growth factor (VEGF); the major feeding arteries and draining vein were VEGF-negative [Figure 4]. The patient was discharged with no postoperative problems.
Figure 1.
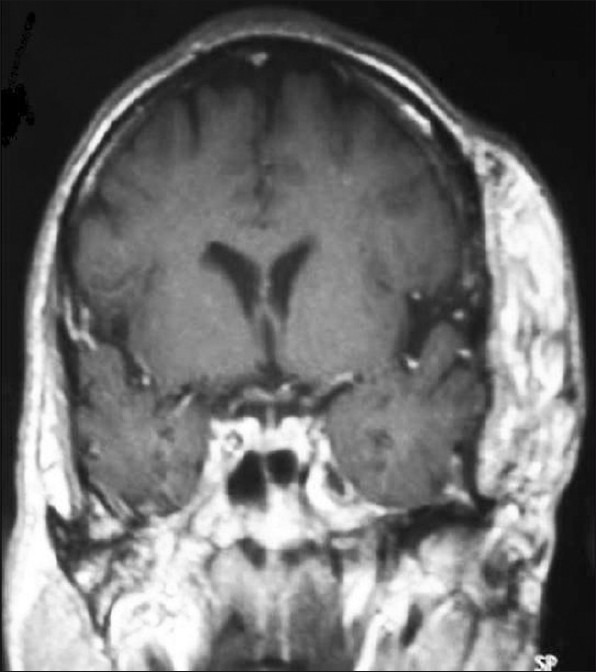
T1-weighted images show a mass lesion under the scalp of the left temporoparietal region
Figure 2.
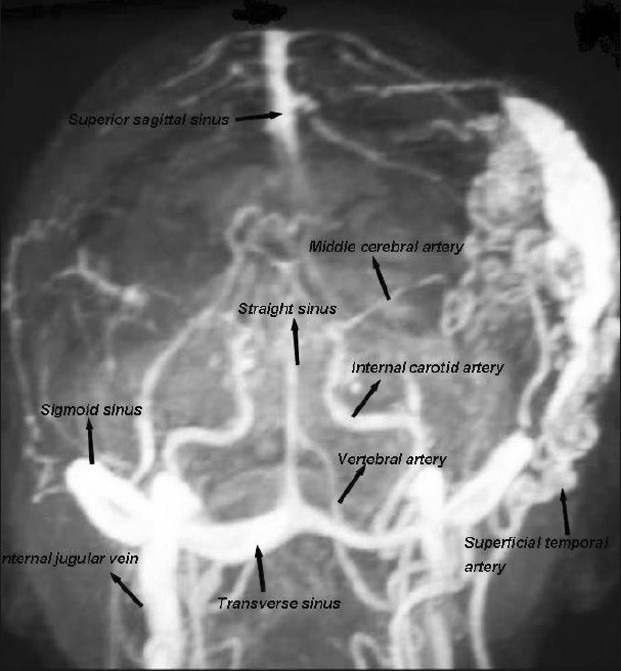
Carotid angiography demonstrates large, tortuous dilated venous structures as well as large AVM
Figure 3.
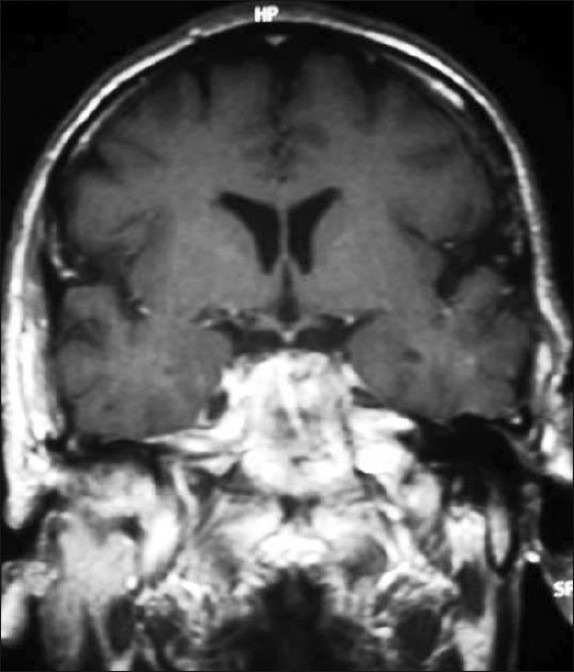
AVM is seen to be removed totally on the postoperative T1-weighted magnetic resonance images
Figure 4.
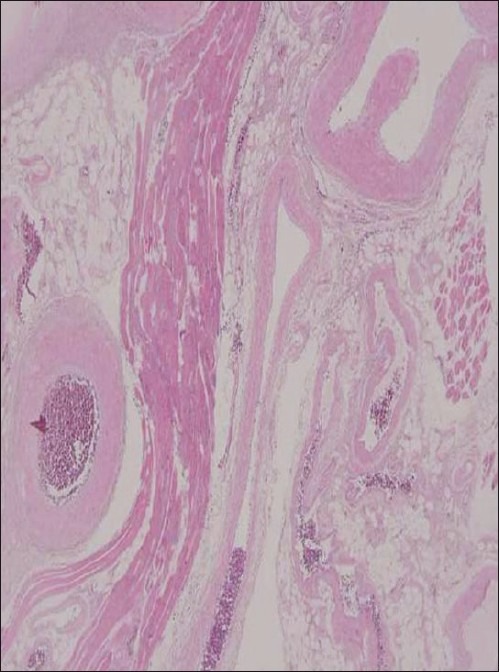
Various sized vessels are seen between fat and muscle tissue (H and E ×40)
Discussion
AVM of the scalp is an uncommon entity.[1,2] Various names are used to describe the vascular malformations of the scalp, including aneurysm cirsoides, aneurysma serpentinum, plexiform angioma, arteriovenous fistula, and AVM.[3–5] The most frequent sites of involvement are frontal, temporal, and parietal regions.[3,5,6] The origin of the main feeder is in the subcutaneous tissue of the scalp. The origin of these main feeders, most frequently, arises from the external carotid, occipital, and supraorbital arteries. The STA is frequently involved in traumatic cirsoid aneurysm.[5–7] The etiology of these lesions remains controversial. The etiology of scalp AVMs may be spontaneous or traumatic.[4,8] They generally develop in the trauma background and in patients over 30 years old. Spontaneous AVM of the scalp may present at birth, but in most patients, it is asymptomatic until adulthood.[3,8,9] Trauma, pregnancy, or hormonal change causes deterioration of the symptoms. Traumatic AVM of the scalp develops months or years after the scalp trauma. About 10 to 20% of scalp AVMs develop following penetrating or non-penetrating trauma to the scalp.[7,8,10] Their clinical signs are associated with the size of the AVM. The patients may present with headache, numbness, and/or hemorrhage. Others may present with severe symptoms such as scalp lesions. Hemorrhage is generally uncommon and may develop in the event of large vascular malformations. Recurrent hemorrhage, which rapidly deteriorates the neurological table, may be seen in some of the patients.[1,3,8] The quality of the diagnosis is important for the surgical procedure to be performed, and cranial angiography is of great significance for diagnosis and treatment selection. It is particularly employed for the determination of cranial feeders. Selective angiography should be carried out for the differential diagnosis of the vascular lesions, such as aneurysms, sinus pericranii, venous malformation, and cavernous hemangioma.[2 8,10] Brain MRI is also of significance for establishing a diagnosis. Scalp AVMs are most frequently confused with hemangioma and cavernomas. No arteriovenous shunt is present in such pathologies, and they are seen as well-demarcated lesions. AVMs show flow void signs on MRI due to the rapid flow in the lesions.[1,8,10] Surgical excision is especially effective in AVMs, and is the most frequently used treatment method.[4,7,11] AVM is generally located in the periosteal and temporal fascia or under the galea. Thus, the preoperative radiological evaluation should be used for the assessment of feeding arteries, drainage vessels, numbers of fistulas, connected vascular structures, and shunt flow volume in order to prevent any possible complications.[3,5,7] One of the substantial complications during the operation is hemorrhage. Hemorrhage may be prevented with preoperative embolization, clamping, and suturing of feeding vessels. Scalp flap is removed with pericranium, which particularly prevents rupture.[5,7,11] The AVM may not always be related to the cranium. Infection and sepsis as well as hemorrhage and necrosis may be seen as complications.[1,5,10] Endovascular treatment may be applied in order to decrease the hemorrhage and facilitate the surgical treatment or in the direct treatment of AVMs.[4,7,11] Embolization of preoperative nidus and feeders especially prevents massive hemorrhage. Embolization and endovascular treatment may not be sufficient in the treatment of large scalp AVMs. Incomplete surgical resection is also insufficient for the treatment. This may cause scalp hemorrhage and necrosis in elderly patients.[7,8,10] Therefore, a large scalp flap should initially be in use for the surgery, as was done in the present case. Despite these treatments, recurrence due to feeding collaterals may develop. The most important step is total surgical excision without causing scalp necrosis and excessive blood loss. Furthermore, a better cosmetic result may be obtained.[1,3,10]
Conclusion
The objective of scalp AVM treatment is to eliminate the clinical complaints affecting the patient′s comfort. Treatment options include surgery, endovascular/percutaneous embolization, electrothrombosis, and combined approaches. Definitive treatment may be provided with embolization in those patients with appropriate angiographic characteristics. In the event of scalp necrosis and excessive blood loss, total excision is the fundamental treatment selection.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Senoglu M, Yasim A, Gokce M, Senoglu N. Nontraumatic scalp arteriovenous fistula in an adult: Technical report on an illustrative case. Surg Neurol. 2008;70:194–7. doi: 10.1016/j.surneu.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Muthukumar N, Rajagopal V, Manoharan AV, Durairaj N. Surgical management of cirsoid aneurysms. Acta Neurochir (Wien) 2002;144:349–56. doi: 10.1007/s007010200048. [DOI] [PubMed] [Google Scholar]
- 3.Shenoy SN, Raja A. Scalp arteriovenous malformations. Neurol India. 2004;52:478–81. [PubMed] [Google Scholar]
- 4.Massimi L, De Bonis P, Esposito G, Novegno F, Pettorini B, Tamburrini G, et al. Vertex scalp mass as presenting sign of a complex intracranial vascular malformation. J Neurosurg Pediatr. 2009;3:307–10. doi: 10.3171/2008.12.PEDS08408. [DOI] [PubMed] [Google Scholar]
- 5.Heilman CB, Kwan ES, Klucznik RP, Cohen AR. Elimination of a cirsoid aneurysm of the scalp by direct percutaneous embolization with thrombogenic coils.Case report. J Neurosurg. 1990;73:296–300. doi: 10.3171/jns.1990.73.2.0296. [DOI] [PubMed] [Google Scholar]
- 6.Burrus TM, Miller GM, Flynn LP, Fulgham JR, Lanzino G. NeuroImages.Symptomatic left temporal arteriovenous traumatic fistula. Neurology. 2009;73:570. doi: 10.1212/WNL.0b013e3181b2a6f1. [DOI] [PubMed] [Google Scholar]
- 7.Gupta AK, Purkayastha S, Bodhey NK, Kapilamoorthy TR, Krishnamoorthy T, Kesavadas C, et al. Endovascular treatment of scalp cirsoid aneurysms. Neurol India. 2008;56:167–72. doi: 10.4103/0028-3886.41995. [DOI] [PubMed] [Google Scholar]
- 8.Fisher-Jeffes ND, Domingo Z, Madden M, de Villiers JC. Arteriovenous malformations of the scalp. Neurosurgery. 1995;36:656–60. doi: 10.1227/00006123-199504000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Li F, Zhu S, Liu Y, Chen Y, Chi L, Chen G, et al. Traumatic arteriovenous fistula of the superficial temporal artery. J Clin Neurosci. 2007;14:595–600. doi: 10.1016/j.jocn.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Matsushige T, Kiya K, Satoh H, Mizoue T, Kagawa K, Araki H. Arteriovenous malformation of the scalp: Case report and review of the literature. Surg Neurol. 2004;62:253–9. doi: 10.1016/j.surneu.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 11.Tiwary SK, Khanna R, Khanna AK. Craniofacial cirsoid aneurysm: 2-stage treatment. J Oral Maxillofac Surg. 2007;65:523–5. doi: 10.1016/j.joms.2005.10.066. [DOI] [PubMed] [Google Scholar]


