Abstract
Summary
Background and objectives
Catheter-dependent hemodialysis patients may develop access-related and nonaccess-related infections that may be managed in the outpatient arena or in the hospital. The goal of this study was to quantify infections in such patients, to characterize their clinical presentations, and to evaluate factors determining need for hospitalization.
Design, setting, participants, & measurements
We collected prospective data on the clinical management of catheter-dependent hemodialysis patients with suspected infection at a large dialysis center. We documented the presenting symptoms, type of infection, pathogen, and whether hospitalization occurred.
Results
An infection was suspected in 305 separate cases and confirmed in 88%. The 268 diagnosed infections included catheter-related bacteremia (69%), another access-related infection (19%), and nonaccess-related infection (12%). The overall frequency of infection was 4.62 per 1000 catheter-days. Hospitalization occurred in 37% of all infections, but it varied greatly (72% for nonaccess-related infection, 34% for catheter-related bacteremia, and 4% for exit-site infection). Among patients with catheter-related bacteremia, the likelihood of hospitalization varied by pathogen, being 53% for Staphylococcus aureus, 30% for Enterococcus, 23% for Staphylococcus epidermidis, and 17% for gram-negative rods (P < 0.001). The likelihood of hospitalization was not associated with age, gender, or diabetes. Fever was a presenting symptom in only 47% of cases of catheter-related bacteremia.
Conclusions
Catheter-dependent patients have a high burden of infection. It is important to evaluate patients with suspected infection for various access-related and nonaccess-related infections. A low threshold is indicated for suspecting catheter-related bacteremia because the patients frequently present without fever.
Introduction
Infection is the second most common cause of death and hospitalization among hemodialysis patients (1–3). Previous prospective studies have focused on the subset of infections causing death (4) or requiring hospitalization (2,5) without including infections treated in the outpatient setting. Moreover, many publications have included primarily patients with fistulas or grafts. Catheters are used in approximately 80% of patients initiating hemodialysis and 25% of all prevalent patients as a bridge to a permanent vascular access or because the patient has exhausted all options for a permanent access (6). Catheter-dependent patients are at increased risk for all-cause infection (7,8). When catheter-dependent hemodialysis patients present with symptoms suggesting infection, the assumed diagnosis is catheter-related bacteremia (9). However, other access-related infections or nonaccess-related infections also need to be considered.
There is little published information on the incidence of different types of infections and the likelihood of hospitalization in catheter-dependent hemodialysis patients. A recent Center of Medicare and Medicaid Services (CMS)-sponsored technical expert panel proposed mandatory computerized collection of information on inpatient and outpatient infections in all hemodialysis patients (http://www.cms.gov/CPMProject/), but the feasibility of such comprehensive data collection has not been demonstrated. We performed a prospective study on infections occurring in catheter-dependent patients at a large dialysis center. The goal of our study was to quantify the frequency and type of infections, their clinical presentations, and the factors that determine patient hospitalization.
Materials and Methods
Study Population
Approximately 500 hemodialysis patients receive their medical care at the University of Alabama at Birmingham (UAB). These patients are dialyzed at five in-center hemodialysis units in metropolitan Birmingham. Approximately 20% to 25% of the patients use a dialysis catheter at any time; of these patients, 25% to 30% had a secondary fistula, graft, or peritoneal dialysis catheter. Clinical nephrologists at UAB supervise their medical care, and >95% of their hospitalizations are at UAB hospital. Four experienced transplant surgeons place new vascular accesses and revise them as needed. UAB interventional radiologists perform preoperative vascular mapping and percutaneous access interventions, including placement of tunneled dialysis catheters. Two full-time access coordinators schedule all access procedures performed by the surgeons and radiologists and maintain a prospective, computerized access database (10).
Management of Infections in Catheter-Dependent Hemodialysis Patients
The outpatient dialysis nurses were in-serviced on the recognition and initial approach to suspected infection. An infection was suspected in any patient with fever, rigors, or findings suggesting localized infection. The dialysis nurse performed the initial evaluation of patients with suspected infection when the symptoms manifested at the in-center dialysis unit, and the emergency room physician or nephrologist did so when the patient presented to the hospital. Catheter-related bacteremia was suspected whenever a patient developed fever (temperature ≥ 37.8°C) or rigors (11). Less commonly, it was suspected because of a purulent discharge from the catheter exit site, malaise, altered mental status, or unexplained hypotension (systolic BP < 90 mmHg) (Table 1). If the patient had a secondary vascular access (fistula or graft), the surgical site was inspected for erythema, heat, swelling, or drainage. If the patient had a peritoneal dialysis catheter, the abdominal site was inspected for evidence of peritonitis or an exit-site infection. In addition, the dialysis nurse or physician evaluated the patient for a nonaccess-related infection by a focused history (shortness of breath, productive cough, abdominal pain, lower extremity pain, dysuria, or localized pain). A focused physical examination was guided by the patient's symptoms, such as inspection of the feet for evidence of gangrene or infection, auscultation of the lungs for suspected pneumonia, and inspection of the skin for cellulitis, abscess, or decubitus ulcer. In selected patients, additional studies were performed to define the type of infection, including imaging studies, urine culture, or abscess culture.
Table 1.
Clinical presentation of probable catheter-related bacteremia
| Clinical Presentation | Number of Cases |
|---|---|
| Total cases | 184 |
| Temperature not reported | 3 |
| Temperature ≥ 37.8°C and rigors | 53 |
| Temperature ≥ 37.8°C without rigors | 32 |
| Temperature < 37.8°C with rigors | 59 |
| Temperature < 37.8°C without rigors | 37 |
| altered mental status | 5 |
| malaise | 8 |
| exit-site purulence | 8 |
| hypotension (systolic BP <90 mmHg) | 2 |
| not reported | 14 |
In patients with suspected catheter-related infection (i.e., no localizing symptoms or signs to suggest an alternative source of infection), antibiotics were initiated per dialysis protocol. If the patient had evidence of another source of infection, the dialysis nurse contacted a nephrologist for guidance. If the symptoms were present upon initiation of a dialysis session, the nurse obtained two sets of blood cultures—one from the catheter lumen and a second from the dialysis bloodline (12). Peripheral blood cultures were not obtained because of the paucity of suitable veins and the need to preserve existing veins for future vascular access. If the symptoms manifested after initiation of the dialysis session, two sets of blood cultures (separated by 15 minutes) were obtained from the dialysis bloodline because systemic blood was already circulating through the dialysis catheter. After drawing the blood cultures, the patient was started on empiric antibiotics (vancomycin and ceftazidime) for broad-spectrum coverage of gram-positive cocci and gram-negative rods. This empiric antibiotic regimen was effective against >95% of organisms grown, but it was modified to a more narrow spectrum antibiotic within 2 to 5 days according to the organism grown and its sensitivities. Patients with documented methicillin-resistant Staphylococcus infection and those with Enterococcus infections were continued on vancomycin alone, those with methicillin-sensitive Staphylococcus infection were switched to cefazolin, and those with gram-negative infections were continued on ceftazidime alone or switched to cefazolin or gentamicin on the basis of the sensitivities. Finally, a few (<5%) patients with concurrent gram-positive and gram-negative infections were continued on the initial empiric antibiotic regimen. Many patients were treated as outpatients, but those with severe sepsis (high fever, persistent rigors, or hemodynamic instability) were hospitalized as a direct referral from the outpatient dialysis unit or if they presented to the emergency room with severe infection.
Whenever a dialysis patient was initiated on intravenous antibiotics, the treating nurse filled out a standardized worksheet, providing the patient's temperature, presence or absence of rigors, and other presenting symptoms, as well as the dose of antibiotics administered. This worksheet was faxed to the access coordinators, who placed a computerized entry into the access database. The access coordinators recorded whether the patient required hospitalization, followed up on the culture results, and modified the antibiotic regimen as needed. The nephrology fellow communicated with the access coordinators at the time of discharge about any patients with suspected infection seen in the emergency room or the hospital.
Data and Statistical Analyses
Our local Institutional Review Board provided approval for analyzing these medical records for research purposes. During the 1.5-year study period (January 1, 2009, to June 30, 2010) we averaged 106 catheter-dependent patients at the five dialysis units. There were 305 instances of suspected infection among our catheter-dependent hemodialysis patients. The access coordinators maintained a prospective, computerized database with details of each suspected infection. The study investigators retrospectively reviewed the data for each case of suspected infection and adjudicated the type of infection on the basis of clinical, microbiologic, and imaging information. Access-related infections were categorized by type of vascular access. Probable catheter-related bacteremia required symptoms suggestive of infection, positive blood cultures, and absence of an alternate source of bacteremia. Exit-site infection was diagnosed in patients with a purulent discharge from the exit site and positive exit-site culture but negative blood cultures. A probable graft or fistula infection was diagnosed in patients with localized erythema, heat, swelling, or drainage over the access site. Peritonitis was diagnosed in patients with a peritoneal dialysis catheter, abdominal pain, and positive peritoneal dialysate cultures. Pneumonia was diagnosed in patients with productive cough or shortness of breath and a pulmonary infiltrate on chest radiograph. A urinary tract infection was diagnosed by urine cultures. Lower extremity infection was diagnosed when there was redness, heat, swelling, or drainage from the foot or stump. Cellulitis was diagnosed in patients with painful, warm, red streaks in the extremity. A skin abscess was diagnosed by physical examination and incision and drainage. Osteomyelitis was diagnosed by computerized tomography or magnetic resonance imaging.
The frequency of hospitalization was calculated for different patient subsets. We compared the likelihoods of hospitalization between different subsets using chi-squared analysis and calculated hazard ratios (HR) and their 95% confidence intervals (CI). A P value <0.05 was considered to be statistically significant.
Results
During the 1.5-year study period, there were 305 cases of suspected infection requiring initiation of systemic antibiotics in catheter-dependent hemodialysis patients. These cases occurred in 172 catheter-dependent patients, who had a range of one to seven instances of suspected infection (Table 2). Eighty percent of the patients with suspected infection had only one or two occurrences during the study period. The demographic and clinical features of the study population are summarized in Table 3. Most patients were black, reflecting the racial composition of our dialysis population. Approximately 40% of the patients were women, and nearly half had diabetes. A substantial proportion had vascular disease or congestive heart failure.
Table 2.
Frequency of suspected infection in catheter-dependent hemodialysis patients
| Number of Infections | Number of Patients | Percent of Patients |
|---|---|---|
| 1 | 96 | 56 |
| 2 | 41 | 24 |
| 3 | 21 | 12 |
| 4 | 8 | 5 |
| 5 | 5 | 3 |
| 7 | 1 | 0.5 |
A total of 172 patients had 305 cases of suspected infection.
Table 3.
Clinical features of the study population
| Number of Patients | Percent of Patients | |
|---|---|---|
| Total | 172 | – |
| Age, mean ± SD | 52 ± 15 | – |
| Women | 71 | 41 |
| Blacks | 138 | 80 |
| Diabetes | 79 | 46 |
| Coronary artery disease | 58 | 34 |
| Peripheral vascular disease | 24 | 14 |
| Congestive heart failure | 61 | 35 |
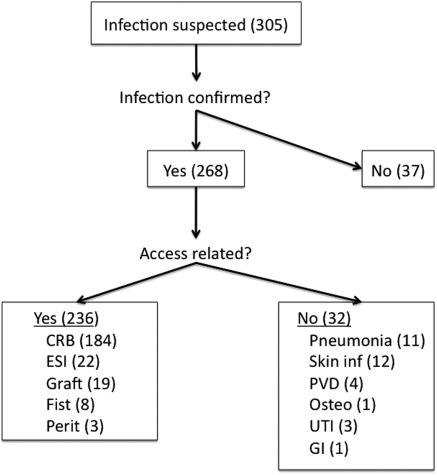
In 37 of 305 (or 12%) cases of suspected infection, the cultures were negative and there were no localizing signs of infection; therefore, an infection was excluded (Figure 1). Thus, infection was confirmed in 268 (or 88%) of cases. Of these, 236 (or 88%) were probable access-related infections because clinical evaluation did not reveal an alternative source of infection. Most (78%) probable access infections were episodes of catheter-related bacteremia. A smaller number of episodes of probable access-related infections were purulent catheter exit-site infections (without concurrent bacteremia), graft infection, fistula infection, or peritonitis related to peritoneal dialysis catheters. Finally, approximately 12% of the cases were nonaccess-related infections, including pneumonia, urinary tract infection, skin infections, lower extremity infection in patients with peripheral vascular disease, and osteomyelitis. Thus, probable catheter-related bacteremia was diagnosed in 184 of 305 (or 60%) cases of catheter-dependent patients with suspected infection.
Figure 1.
The frequency and type of infections in catheter-dependent hemodialysis patients. Note that an infection was confirmed in most patients with suspected infection, but that only 60% had probable catheter-related bacteremia. The remainder had an infection of a secondary-access or a nonaccess-related infection. CRB, catheter-related bacteremia; ESI, exit-site infection; Fist, fistula; Perit, peritonitis; PVD, peripheral vascular disease; Osteo, osteomyelitis; UTI, urinary tract infection; GI, gastrointestinal.
The overall frequency of infection was 4.62 per 1000 catheter-days (Table 4). The frequency of probable catheter-related bacteremia was 3.17 per 1000 catheter-days. Approximately 37% of all infections required hospitalization, whereas 63% were managed as outpatients. The likelihood of hospitalization was highly dependent on the type of infection, being as high as 72% for nonaccess-related infections and as low as 4% for exit-site infections. Access-related infections accounted for 77% of all infection-related hospitalizations. Among the 184 episodes of probable catheter-related bacteremia, 34% required hospitalization, but the likelihood varied greatly by type of organism, being 53% for Staphylococcus aureus, 30% for Enterococcus, 23% for Staphylococcus epidermidis, and only 17% for gram-negative rods (HR for S. aureus versus other organisms 2.32; 95% CI 1.53 to 3.50; P < 0.001) (Table 5). The likelihood of hospitalization for catheter-related bacteremia was not associated with patient age (33% in patients ≥65 years versus 34% in those <65 years of age; HR 0.99; 95% CI 0.58 to 1.68; P = 0.96), gender (41% in women versus 29% in men; HR 1.42; 95% CI 0.95 to 2.12; P = 0.10), or diabetic status (40% in diabetics versus 28% in nondiabetics; HR 1.38; 95% CI 0.92 to 2.08; P = 0.12).
Table 4.
Frequency of infection-related hospitalizations
| Rate of Infectiona | Rate of Infections Requiring Hospitalizationa | Percent of Infections Requiring Hospitalization | |
|---|---|---|---|
| All infections | 4.62 | 1.70 | 36.8 |
| Nonaccess-related infections | 0.55 | 0.39 | 71.9 |
| Access-related infections | 4.07 | 1.31 | 32.2 |
| Catheter-related bacteremia | 3.17 | 1.07 | 33.7 |
| Catheter exit-site infection | 0.38 | 0.02 | 4.3 |
| Graft infection | 0.33 | 0.14 | 42.6 |
| Fistula infection | 0.14 | 0.06 | 48.8 |
| Peritoneal dialysis infection | 0.05 | 0.02 | 31.2 |
Per 1000 catheter-days.
Table 5.
Likelihood of hospitalization for catheter-related bacteremia by pathogen
| Organism | Total | Inpatient | Percent Inpatient |
|---|---|---|---|
| Staphylococcus aureus | 53 | 28 | 53 |
| Enterococcus | 30 | 9 | 30 |
| Staphylococcus epidermidis | 60 | 14 | 23 |
| gram-negative rod | 24 | 4 | 17 |
Excludes 17 cases of polymicrobial bacteremia. P < 0.001 for S. aureus versus other organisms.
Among the subset of 116 cases of infection suspected because of fever, 73% had probable catheter-related bacteremia, 4% had a probable graft or fistula infection, 2% had a purulent catheter exit-site infection, 6% had a nonaccess-related infection, and 15% did not have an infection confirmed. Only 18% (5 of 27) of patients with probable graft or fistula infection had a fever on presentation.
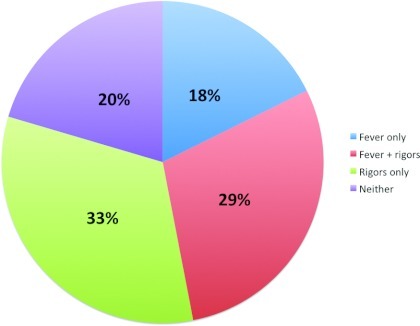
The clinical presentation of patients with probable catheter-related bacteremia was analyzed (Table 1). The patient's temperature was not reported in three cases. Of the remaining 181 episodes, the patient presented with fever and rigors in 53 cases, fever without rigors in 32 cases, and rigors without fever in 59 cases. Finally, 37 cases of catheter-related bacteremia presented with symptoms other than fever or rigors and without clinical findings to suggest an alternative source of bacteremia. The presenting symptom in these patients included altered mental status, malaise, exit-site drainage, or hypotension. The presenting symptom was not reported in 14 cases of catheter-related bacteremia. The frequency of rigors was similar in patients presenting with fever or no fever (62% versus 61%). The frequency of each type of clinical presentation is displayed in Figure 2. Only 47% of patients with probable catheter-related bacteremia had fever at presentation. The likelihood of fever at presentation was higher with catheter-related bacteremia due to S. aureus (77%) as compared with gram-negative rods (46%), S. epidermidis (33%), and Enterococcus (23%) (HR for S. aureus versus other organisms 2.28; 95% CI 1.70 to 3.07; P < 0.001).
Figure 2.
Clinical presentation of patients with probable catheter-related bacteremia. Note that only 47% of patients had fever at presentation.
Discussion
This study demonstrates the high burden of infection in catheter-dependent hemodialysis patients at a frequency of 4.62 per 1000 catheter-days. Remarkably, nearly 90% of cases with suspected infection were confirmed to have an infection. However, probable catheter-related bacteremia was diagnosed in only 60% of cases with suspected infection, emphasizing the importance of considering other sources of infections in catheter-dependent patients. This finding is in agreement with three prior studies that reported a 59% to 81% likelihood of bacteremia in catheter-dependent patients with suspected infection (12–14). The other infections included secondary-access (fistula, graft, or peritoneal dialysis catheter) infection and nonaccess-related infection. A focused history and physical examination by the dialysis nurse or physician in conjunction with selected additional tests in selected patients were able to identify the probable infection type in most cases.
Access-related infections accounted for 77% of infection-related hospitalizations in the study presented here, considerably higher than the 21% rate reported in the Hemodialysis (HEMO) study (2). The HEMO study observed that catheters were present in 32% of patients hospitalized with access-related infection, although catheters accounted for only 7.6% of all vascular accesses in the study. Likewise, Hoen et al. reported that catheters were present in 36% of patients with access-related infections, although only 6% of their dialysis patients were using catheters (15). Thus, the high proportion of access-related infection hospitalizations in the study presented here is likely a direct reflection of catheter use. Alternatively, it may reflect the patients' comorbidities that required catheter use. Of interest, fever was much more likely to be a presenting sign in patients with catheter-related bacteremia than in patients with a graft or fistula infection (18% versus 47%). This observation is consistent with a previous report from the HEMO study (2).
Approximately two thirds of the infections observed in our catheter-dependent patients were managed in the outpatient arena. Thus, studies reporting only infections requiring hospitalization may substantially underestimate the overall frequency of infections. The likelihood of hospitalization was related to the type of infection, with nonaccess-related infections much more likely than access-related infections to require hospitalization. Moreover, among patients with probable catheter-related bacteremia, those with S. aureus infection were much more likely to require hospitalization than those caused by S. epidermidis, Enterococcus, or gram-negative rods. Previous studies have reported that a treatment failure of catheter-related bacteremia is most likely with S. aureus infections, followed by Enterococcus, S. epidermidis, and gram-negative rods (12,14,16–19). This hierarchy is consistent with the relative likelihood of hospitalization for catheter-related bacteremia observed in the study presented here.
The clinical presentations of catheter-related bacteremia provide important new information. Fever has been proposed as an important criterion for diagnosing catheter-related bacteremia (20). Given that only 47% of our patients with probable catheter-related bacteremia had fever as a presenting symptom, this rigid requirement would lead to marked underestimation of the frequency of catheter-related bacteremia. Although it might be argued that use of alternative criteria, such as rigors, may overestimate catheter-related bacteremia, we also required exclusion of alternative sources of infection. This requirement was adhered to, as is evident from the substantial number of nonaccess-related infections and noncatheter-related access infections diagnosed in our study.
The strengths of the study presented here include its prospective data collection, the exclusive focus on catheter-dependent hemodialysis patients, and the inclusion of infections managed in the outpatient arena. Our study does have some limitations. First, it was a single-center study, and the results may not generalize to all centers. For example, the criteria for hospitalizing patients with infection may differ at other institutions, and the rate of catheter-related bacteremia varies considerably among centers. Second, we only included patients who received intravenous antibiotics. However, it is likely that patients treated with oral antibiotics had mild and localized infections. Third, the assessment of infection was performed by many dialysis nurses or physicians who might differ in their diagnostic skills. However, this reflects the “real-world” scenario. Moreover, the investigators adjudicated all suspected cases to classify the likely type of infection.
There is a dearth of comprehensive prospective information on access-related infections among US hemodialysis patients. A recent CMS-sponsored technical expert panel proposed mandatory computerized collection of information on inpatient and outpatient infections in all hemodialysis patients (http://www.cms.gov/CPMProject/). The study presented here demonstrates the feasibility of such data collection when dedicated and experienced nurses are charged with ensuring comprehensive quality control. A national database of dialysis-associated infections would provide a wealth of information on frequency of infection and differences among dialysis units. Such information would be valuable in promoting concerted efforts to reduce infectious complications in the dialysis population. However, CMS would have to fund full-time infection control nurses at the outpatient hemodialysis units to make certain that the collected data are complete and accurate.
Disclosures
None.
Acknowledgments
Part this manuscript was presented in abstract form at the National Kidney Foundation meeting; April 26 through 30, 2011; Las Vegas, NV.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. U.S. Renal Data System: USRDS 1998 Annual Data Report, Bethesda, MD, National Institute of Health, National Institute of Diabetes and Digestive and Kidney Disease, 1998 [Google Scholar]
- 2. Allon M, Depner TA, Radeva M, Bailey J, Beddhu S, Butterly D, Coyne DW, Gassman JJ, Kaufman AM, Kaysen GA, Lewis JA, Schwab SJ: Impact of dialysis dose and membrane on infection-related hospitalization and death: Results of the HEMO study. J Am Soc Nephrol 14: 1863–1870, 2003 [DOI] [PubMed] [Google Scholar]
- 3. Bloembergen WE, Hakim RM, Stannard DC, Held PJ, Wolfe RA, Agodoa LYC, Port FK: Relationship of dialysis membrane and cause-specific mortality. Am J Kidney Dis 33: 1–10, 1999 [DOI] [PubMed] [Google Scholar]
- 4. Sarnak MJ, Jaber BL: Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidney Int 58: 1758–1764, 2000 [DOI] [PubMed] [Google Scholar]
- 5. Powe NR, Jaar B, Furth SL, Hermann J, Briggs W: Septicemia in dialysis patients: Incidence, risk factors, and prognosis. Kidney Int 55: 1081–1090, 1999 [DOI] [PubMed] [Google Scholar]
- 6. Collins AJ, Foley RN, Gilbertson DT, Chen SC: The state of chronic kidney disease, ESRD, and morbidity and mortality in the first year of dialysis. Clin J Am Soc Nephrol 4[Suppl 1]: S5–S11, 2009 [DOI] [PubMed] [Google Scholar]
- 7. Allon M, Daugirdas JT, Depner TA, Greene T, Ornt D, Schwab SJ: Effect of change in vascular access on patient mortality in hemodialysis patients. Am J Kidney Dis 47: 469–477, 2006 [DOI] [PubMed] [Google Scholar]
- 8. Lacson E, Jr, Wang W, Lazarus JM, Hakim RM: Change in vascular access and mortality in maintenance hemodialysis patients. Am J Kidney Dis 54: 912–921, 2009 [DOI] [PubMed] [Google Scholar]
- 9. Allon M: Dialysis catheter-related bacteremia: Treatment and prophylaxis. Am J Kidney Dis 44: 779–791, 2004 [PubMed] [Google Scholar]
- 10. Allon M, Bailey R, Ballard R, Deierhoi MH, Hamrick K, Oser R, Rhynes VK, Robbin ML, Saddekni S, Zeigler ST: A multidisciplinary approach to hemodialysis access: Prospective evaluation. Kidney Int 53: 473–479, 1998 [DOI] [PubMed] [Google Scholar]
- 11. Allon M: Treatment guidelines for dialysis catheter-related bacteremia: An update. Am J Kidney Dis 54: 13–17, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Poole CV, Carlton D, Bimbo L, Allon M: Treatment of catheter-related bacteremia with an antibiotic lock protocol: Effect of bacterial pathogen. Nephrol Dial Transplant 19: 1237–1244, 2004 [DOI] [PubMed] [Google Scholar]
- 13. Krishnasami Z, Carlton D, Bimbo L, Taylor ME, Balkovetz DF, Barker J, Allon M: Management of hemodialysis catheter related bacteremia with an adjunctive antibiotic lock solution. Kidney Int 61: 1136–1142, 2002 [DOI] [PubMed] [Google Scholar]
- 14. Vardhan A, Davies J, Daryanani I, Crowe A, McClelland P: Treatment of haemodialysis catheter-related infections. Nephrol Dial Transplant 17: 1149–1150, 2002 [DOI] [PubMed] [Google Scholar]
- 15. Hoen B, Paul-Dauphin A, Hestin D, Kessler M: EPIBACDIAL: A multicenter prospective study of risk factors for bacteremia in chronic hemodialysis patients. J Am Soc Nephrol 9: 869–876, 1998 [DOI] [PubMed] [Google Scholar]
- 16. Fernandez-Hidalgo N, Almirante B, Calleja R, Ruiz I, Planes AM, Rodriguez D, Pigrau C, Pahissa A: Antibiotic-lock therapy for long-term intravascular catheter-related bacteremia: Results of an open, non-comparative study. J Antimicrob Chemother 57: 1172–1180, 2006 [DOI] [PubMed] [Google Scholar]
- 17. Maya ID, Carlton D, Estrada E, Allon M: Treatment of dialysis catheter-related Staphylococcus aureus bacteremia with an antibiotic lock: A quality improvement report. Am J Kidney Dis 50: 289–295, 2007 [DOI] [PubMed] [Google Scholar]
- 18. Mokrzycki MH, Zhang M, Cohen H, Golestaneh L, Laut JM, Rosenberg SO: Tunnelled hemodialysis catheter bacteraemia: Risk factors for bacteraemia recurrence, infectious complications and mortality. Nephrol Dial Transplant 21: 1024–1031, 2006 [DOI] [PubMed] [Google Scholar]
- 19. Peterson WJ, Maya ID, Carlton D, Estrada E, Allon M: Treatment of dialysis catheter-related Enterococcus bacteremia with an antibiotic lock: A quality improvement report. Am J Kidney Dis 53: 107–111, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK: Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 49: 1–45, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]